Abstract
Purpose of review
Henoch-Schönlein purpura nephritis (HSPN), known currently as nephritis associated with IgA vasculitis (IgAVN), and IgA nephropathy (IgAN) share pathogenetic mechanisms and almost indistinguishable histology, but have peculiar clinical behavior and outcome. Recent classifications, clinical trials, and discussions lead to critical revision of old and new treatments.
Recent findings
In recent years, the histological classification of IgAN Oxford-MEST allowed the identification of histological and clinical risk factors for progression of IgAN and encouraged new studies to explore the value of different treatments, allowing a more standardized classification of enrolled patients. For HSPN, large clinical studies are lacking, and the old histological classifications available do not allow such a precise standardization. However, new efforts are made to follow the IgAN pipeline. Personalized therapies are being forecast, tailored according to histological and clinical risk factors implemented by more innovative biomarkers. The aim is to efficaciously treat both diseases in the earlier phases. The inflammatory process can be completely extinguished if treated adequately without delay, with a high percentage of permanent complete remission in children.
Summary
The state-of-the-art knowledge of the elements useful to choose the appropriate treatment in HSPN/IgAVN and IgAN in children is reviewed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
IgA nephropathy and Henoch-Schönlein purpura nephritis/IgA vasculitis: one or two diseases?
IgA nephropathy, the most diffuse glomerulonephritis in the young, has a relatively recent history due to the definition of its characteristic mesangial intercapillary deposits only in 1968 [1], when IgG- and IgA-specific antisera became available [2]. Previously it was described as benign recurrent hematuria, with a histology of focal segmental nephritis and a clinical behavior strictly related to infections but without hypocomplementemia. For some years, the finding of Berger was not confirmed by other authors and was considered as a non-specific incidental staining due to poor quality of the antiserum, and only in 1973, the group of Habib was able to join idiopathic recurrent macroscopic hematuria with the presence of IgG and IgA mesangial deposits [3].
Henoch-Schönlein purpura, the most common vasculitis in childhood, has instead a much older history, being known since the previous century, and often associated to food allergy and frequently complicated by nephritis.
These two independent stories converged in 1973, when dominant IgA deposits were described in the vessel walls and in mesangium of 4 cases of Henoch-Schönlein purpura nephritis (HSPN) and of 4 cases of recurrent macroscopic hematuria. The presence of IgA, IgG, and C3 raised the hypothesis of a common pathomechanism for the two diseases [4], possibly driven by the IgA itself, identified also in the vessel wall of unaffected skin [5].
Since the 1970s, the two diseases have run a parallel pathway: it became rapidly evident that IgA nephropathy was the most common glomerulonephritis worldwide and that HSPN in contrast was a rare disease, with distinct epidemiological and clinical characteristics between them, but with an almost indistinguishable histology, suggesting common immunological aspects but some peculiar differences [6•].
After 50 years of parallel journey, the pathogenic mechanisms of both diseases remain elusive: histology, biochemistry, immunology, and some clinical aspects are completely superimposable but HSPN has a widespread tendency to regress and completely recover in most of the cases, while IgAN more commonly has a chronic progressive course and a much less explosive onset [7].
Henoch Schönlein purpura
HSPN/IgA vasculitis: which disease are we talking about?
Henoch-Schönlein purpura is the most common vasculitis in childhood, involving the skin, the gastrointestinal tract, the joints and less frequently kidneys, testes, and brain.
The true incidence is widely variable from 3 to 30/100.000 children, owing to both possible under-reporting but also different classification criteria used over the years. The American College of Rheumatology classification of 1990 is exclusively clinical and without consideration for IgA, whereas the EULAR PRINTO/PRES classification of 2010 requires the presence of palpable purpura but without the need for a histological criterion. In the most recent “Chapel Hill conference revised nomenclature of systemic vasculitis” of 2012, HSP is re-named “IgA vasculitis” (IgAV) for the mandatory presence of dominant IgA1 deposits in small vessels of the skin or gastrointestinal tract, frequently associated with arthritis and possibly to nephritis (IgAVN), histologically indistinguishable from IgA Nephropathy. The vasculitic involvement may be systemic or limited to a single organ.
IgAV has a peculiar epidemiology, involving mainly children, with a peak incidence at primary school age but being present in all ages, with seasonal trend [8, 9] and a trend towards a lower incidence over decades all over the world [10], supporting the hypothesis of a pathogenic role of infections [11] of bacterial, viral, and protozoal origin.
Renal involvement occurs in about one-third of patients. In a recent metanalysis, some predictive risk elements were identified as age over 8 years, male gender, severe persistent abdominal involvement, recurrent persistent purpura, and laboratory parameters like C3 consumption, leukocytosis, and thrombocytosis [12].
Timing of nephritis appearance is widely variable from the onset of purpura, from 1 day to over 1 year, but primarily within the first month. In a recent European pediatric cohort [13], the median time of renal involvement appearance was 13 days after purpura onset (IQR 0–45 days), with presentation differing from microscopic hematuria to nephrotic or nephritic syndrome, and in a small percentage with rapidly progressive evolution. Adults frequently receive a delayed diagnosis of the nephritis due to milder, misdiagnosed, or under-detected purpura [14].
Timing of renal biopsy policy may vary according to the clinical presentation: the idea of a generally favorable disease in childhood often leads to a delayed biopsy, frequently after a tentative therapeutic approach with steroids. Histology is mainly evaluated in patients’ unresponsive to treatment or with nephrotic syndrome and avoided in milder cases with isolated microscopic hematuria or rapidly resolving disease.
Timing of biopsy after the onset of nephritis in a recent German study [15] was found to influence histology, particularly when considering crescents and sclerotic lesions. Crescents were progressively less frequent when the biopsy was delayed, giving way to increased incidence of chronic lesions such as glomerular sclerosis and interstitial fibrosis/tubular atrophy after awaiting months. Chronic lesions, often associated to non-nephrotic smoldering proteinuria, in this cohort represented an unfavorable prognostic factor for progression.
In an Italian cohort including 83 children [14], the presentations were isolated urinary abnormalities or nephrotic range proteinuria associated in some cases with moderate renal failure. Main histological findings were class II and III according to Emancipator classification. Lower histological classes were also the most common finding in a recent survey within European centers [13] and in the German cohort [15].
Is there anything to do to prevent HSPN/IgAVN?
The unfavorable long-term renal outcome in a significant percent of cases [16] accounts for the main complication for HSPN/IgAV, especially in younger age. Pediatricians therefore are often tempted to provide a preemptive treatment aimed at avoiding nephritis occurrence, mainly with steroids.
Several schemes of preemptive treatment, mainly based on short-term courses of oral corticosteroids, have been employed but without a significantly positive effect in avoiding nephritis occurrence, as demonstrated in a systematic review in 2009 [17, 18].
KDIGO guidelines published in 2012 (Chapter 11, recommendation 11.3.1) included 5 RCTs with 789 children and did not find any protection induced by 2–4 weeks of oral steroids from the development of persistent kidney involvement (microscopic hematuria, proteinuria, hypertension, reduced kidney function) at 6 and 12 months. The recommendation therefore is not to use corticosteroids to prevent HSPN/IgAV with high grade (1B) of evidence [19••].
A recent randomized placebo controlled trial [20] further demonstrates that there is no conclusive evidence of the benefit of steroid systematic treatment in avoiding nephritis occurrence [21].
Histology can help in deciding the therapeutic strategy in HSPN/IgAVN?
HSPN/IgAVN in most cases has an acute although extremely variable presentation, from minimal microscopic hematuria to rapidly progressive renal failure. Therefore, the treatment options should be tailored and balanced according to both histology and clinical presentation.
Although the International Study of Kidney Disease in Children (ISKDC) classified the risk of progression based on the extent of crescents, the predictive value of long-term outcome of this classification, which takes into account mainly acute lesions, is questioned. Extracapillary proliferation is a dominant histologic feature of HSPN, extremely variable upon timing of biopsy and highly susceptible to healing upon treatment, even in higher classes, while on the other side, lower grade lesions can also lead to chronic kidney disease when underestimated and under-treated (Table 1).
A recent French study [22] including 92 children with ISKDC, class II and variable clinical presentation reported that 25% of the children remaining proteinuric along follow-up, had higher risk of progression to chronic kidney diseases as previously demonstrated [16] (see Table 1). The same study pointed out that ISKDC classification, which does not take into account morphologic lesions such as interstitial and glomerular inflammation, tubular atrophy, interstitial fibrosis (IFTA), segmental sclerosis, and vascular lesions like arteriosclerosis, may be scarcely predictive of long-term outcome and of limited value in guiding therapeutic choice. Several studies in recent years have attempted to extend the Oxford MEST classification [23, 24], validated for primary IgAN [25••], to selected cohorts of HSPN/IgAVN either in adults [26] and in children [13, 27] (Table 1). The need for an updated HSPN/IgAVN histological classification that is predictive, reliable, and helpful to establish treatment strategies is presently being addressed by a Global IGAV histological classification study including both children and adults (ongoing study with unpublished results).
HSP/IgAVN: once nephritis occurs, steroids or non-steroids?
The extremely heterogeneous clinical presentation of HSPN/IgAV requires therapeutic choices to be based not only on histology but also on renal function and evolution. In milder cases, with sub nephrotic proteinuria, nephritic syndrome, or isolated urinary abnormalities, the value of histology in driving therapeutic choices is debated and the available studies are mainly small cohort studies or underpowered randomized controlled trials (RCTs), with questionable outcomes and enrollment criteria. A systematic review [28] pointed out that “further adequately powered Randomized Controlled Trials (RCT) of short term prednisone therapy compared with placebo should be considered in children, who have or develop kidney disease with HSP or have risk factors for developing kidney disease including older age…..with clearly defined end points for kidney function (GFR), proteinuria (protein/creatinine ratios or timed urine collections), microscopic and macroscopic hematuria and hypertension. However recruitment to a placebo controlled RCT may be difficult”.
KDIGO guidelines released in 2012 [19••] produced three recommendations for the treatment of HSPN in children which were quite debated in Europe and Asia, particularly for the tendency to assimilate HSPN to IgAN, which by contrast is usually characterized by a milder, less fulminant, and chronic behavior. The first recommendation in KDIGO guideline suggests that children with persistent proteinuria below 1 g/d/1.73 m2 are treated with ACE or ARBS for at least 6 months. Even if proteinuria is increasing along time, the recommendation (evidence grade 2D) is still to treat with ACE/ARBS for 6 months. In the event of persistent proteinuria, it was suggested to treat these cases with a 6-month course of steroids as in IgAN. This recommendation was highly debated, particularly in Europe, where there is a long dating tradition of treatment with intravenous steroid pulses and immunosuppression in children [29••], aiming at the complete resolution of crescents and glomerular endocapillary infiltration, although without controlled ad hoc studies. Delaying a strong anti-inflammatory treatment may allow the spontaneous evolution of crescents to sclerotic lesions and potentially favor progression toward chronic kidney disease. This idea is further supported by a retrospective study which evidenced the persistence of proteinuria in 25% of children with ISKDC class II nephritis which was not treated with steroids according to benign histology and low-grade proteinuria compared with those with nephrotic proteinuria and analogous histology treated with steroids, without significant difference between pulse intravenous and oral [22] steroid therapy.
The acute explosive onset of HSPN/IgAV is in many cases accompanied by a rapidly deteriorating kidney function associated with crescents in a high percentage of glomeruli: these cases can be assimilated to rapidly progressive IgAN or to vasculitis and the treatments suggested by KDIGO recommendation 11.2 [19••] and usual clinical practice are derived accordingly.
The advantage of pulse steroids over oral administration has been investigated in IgAN in an older retrospective cohort [30], which evidenced a positive effect of pulses over renal function survival compared with oral steroids or supportive treatment. No specific trial has addressed this issue in HSPN/IgAV where the tendency to use pulse steroids is widespread in clinically aggressive cases aiming at a rapid anti-inflammatory effect. The clinical indication to use pulse steroids in children is usually anticipated to a lower percentage than the 50% crescents threshold suggested in KDIGO 2012. In the last release of KDIGO in 2019 [31••, 32], IgAV is not specifically considered; however, the need for discussion and update on the schemes of use of ACE inhibitors and steroids in IgAN is stated.
Immunosuppressive agents in HSPN/IgAVN: when are they necessary? Which options?
According to retrospective series, as the recent CureGN study [33], including 285 children (112 IgAVN and 173 IgAN) and 382 adults (49 IgAVN and 333 IgAN), the use of immunosuppressive drugs at diagnosis is widespread in both children and adults. In IgAVN, cyclophosphamide was used in 16.3% of adults versus 8% of children, which were more frequently treated with mycophenolate mofetil (20.5% in children vs 10.2% in adults). Azathioprine was used to a similar degree in both in children and in adults (8.9% vs 6.1%). In this cohort, adults affected by IgAVN were more severely affected than children, with lower GFR, and thus more aggressively treated than children also with steroids (85.7% in adults vs 73.2% in children).
Conclusive data on cyclophosphamide efficacy on the survival of renal function, however, are not available: in children a randomized controlled trial was not conclusive on long-term protection against chronic renal disease progression, although a beneficial anti-proteinuric effect was demonstrated [34]. Similar findings have also been observed in adults [35]. KDIGO 2012 guidelines included immunosuppressive drugs with a low evidence of efficacy (grade 2D) even in case of deteriorating renal function [19••] and a systematic review was not conclusive on indications in 2015 [28].
In clinical practice, however, particularly in rapidly progressive cases or with persistent steroid resistant nephrotic syndrome, some sort of immunosuppression is widely used, including cyclosporine [36, 37], tacrolimus [38], and mycophenolate mofetil. Moreover, due to minor side effects and clinical application to other nephritis types, the use of mycophenolate mofetil is increasing, and is reported as a successful alternative to other immunosuppressants as an adjunctive therapy to steroids, in several case series or cohorts either in both adults [39, 40] and children [41,42,43,44].
In a recent study [42], mycophenolate mofetil (MMF) was introduced in 18 children as an early second-line therapy within 3 months after diagnosis of HSP and 1 month after nephritis onset, after steroid pulses with incomplete response (33.8 ± 47.6 days after the diagnosis of HSPN, and 21.9 ± 17.5 days after initiation of pulsed methylprednisolone), at an initial dose of MMF of 800–1200 mg/m2 BSA/day, obtaining proteinuria remission within 3 months without significant side effects.
These authors in accordance with the position already expressed in [29••] believe that HSPN/IgAV in children is a highly inflammatory and explosive disease. In such patients, a rapid intervention during the acute inflammatory phase may allow to completely switch off the process, favoring complete and permanent healing, avoiding the possible spontaneous resolution of crescents and endocapillary infiltrate toward sclerosis.
Is there a space for rituximab?
The majority of children affected by HSPN/IgAVN respond to steroids and, as discussed in the previous paragraphs, only in a small percentage is an immunosuppressive drug required, reserved for aggressive cases, steroid resistant or relapsing disease.
Another option, extrapolated from the positive experience in other types of vasculitis, is B lymphocyte depleting treatment with rituximab (RTX). After initial case reports either in adults [45,46,47,48,49,50] and children [51], small cohorts are appearing in recent years reporting a positive effect of RTX in inducing remission in multidrug-resistant or refractory cases and in steroid dependent [52] cases, without significant side effects. Proteinuria remission, renal function stabilization, and absence of further relapses were observed in over 90% of cases. The adopted schemes were variable from 2 pulses of 750–1000 mg/m2 to 4 pulses of 375 mg/m2.
Ofatumumab was described as equivalently effective in one case of IgAV [53].
IgA nephropathy
IgAN: a wide variety of clinical pictures
Primary IgAN in childhood, even more than in adults, has an extremely variable clinical presentation: occasional finding of isolated microscopic hematuria, recurrent macroscopic hematuria, and rare cases of rapidly progressive renal failure, with accordingly different history and outcome [54].
Some Asian countries like Japan have longstanding urinary screening policies in schools, with timely biopsy of persistent microscopic hematuria [55, 56] allowing early diagnosis of IgAN, in most cases with initial histological lesion, facilitating expeditious follow-up. This policy was demonstrated in high IgAN incidence countries to offer sustained advantages in terms of long-term prevention of chronic kidney disease [55, 57].
Biopsy timing and policy strictly influence the histological findings, subsequent history, and outcome: in a recent Japanese work, 201 children received a renal biopsy after school screening in 65% of the cases within 10 months from first observation. Active histological lesions were negatively correlated with time from clinical onset to biopsy, with endocapillary hypercellularity and crescents significantly more frequent in early biopsies, while biopsies delayed for over 3 years had significantly more sclerotic lesions and a lower percentage of proliferative active lesions [58, 59••]. The Oxford classification [60••], validated also in children in different cohorts [24, 61, 62], has allowed the identification of histological risk factors for renal outcome, defining sclerotic and tubular-interstitial lesions as the prominent risk factors for progression independent from clinical presentation (Table 1).
In children, the most frequent clinical presentation is recurrent macroscopic hematuria with sub-nephrotic proteinuria, with only slightly reduced renal function and mild hypertension in the majority of the cases. In such cases, the dominant lesions have proliferative characteristics—mesangial, endocapillary, and extracapillary—with formation of crescents.
These highly inflammatory lesions are responsive to treatment with an elevated possibility to completely reverse the clinical picture at onset.
Indeed, active inflammatory lesions, namely endocapillary proliferation, were prognostically negative only when no immunosuppressive treatment was used, in a recent adult cohort [63].
In a large recent study combining the Oxford, VALIGA, and Asian individual cohorts to more than 3000 patients, crescents were associated with progression only in untreated cases while any type of therapy was able to reduce the progression risk. The same pattern was revealed in cases with no crescents [64].
Additionally, another study demonstrated with serial biopsies that endocapillary hypercellularity, crescents, and necrosis are reversible with the use of immunosuppression in parallel with clinical improvement defined as proteinuria remission, reduction of macroscopic hematuria episodes, and renal function improvement or stabilization [65].
A convincing amount of clinical evidence supports, therefore, the need for timely biopsies, to identify active proliferative and inflammatory lesions, potentially responsive to treatment with a positive effect on long-term outcome. On the other hand, particularly in children with mild clinical and histological features, IgAN may undergo spontaneous remission: in a Japanese cohort, 55.7% and 74% reached spontaneous remission after 5 and 10 years, respectively, with a recurrence rate of urinary abnormalities in 20% and 32% at 5- and 10-year follow-up [66].
Between the fulminant and histologically active cases deserving and in most cases receiving some type of immunosuppressive treatment and the milder cases possibly evolving to spontaneous remission, another subpopulation of children was revealed to maintain milder urinary abnormalities and a smoldering disease through years, with a relentless progression to renal failure over decades.
Even today, almost 50% of IgAN patients will reach end stage renal failure before the age of 50 and it is conceivable that the most important part of the inflammatory damage occurs during childhood or young adulthood.
Generally, IgAN in children has a progression trend significantly more benign than in adults. However, considering the long life expectancy of pediatric cases, the prognostic value of histological lesions and even minor clinical signs should be considered so as not to delay or avoid an effective and potentially corrective treatment.
The rational basis for treatment of IgAN in children: IgAN is an autoimmune and inflammatory disease
The pathogenesis of IgAN is complex and the most accredited hypothesis is based on a multihit model. Under the presence of a predisposing genetic background, the 1st hit is the production of galactose deficient IgA1 (GdIgA1), able to induce an immunological response with the production of anti-glycan antibodies (2nd hit) and the resulting formation of circulating IgA1 immune complexes (3rd hit), which will deposit on mesangial cells (4th hit) inducing the activation of the local inflammatory cascade, involving also complement [67,68,69].
In this multi-step model, therapeutic intervention could be addressed at these crucial steps, controlling causal infections and antigens as primary stimuli leading to GdIgA1, abort the immunological mechanisms leading to the formation of anti-glycan antibodies and immune complexes through immunosuppression and finally acting on the inflammatory and anti-fibrogenic/sclerogenic pathways [70].
IgAN in children is different from adults
Considering the long natural history of IgAN with childhood onset, most frequently caught in a highly proliferative phase, there is a wide consensus on the need for immunosuppressive therapy more often than in adults, which are instead frequently observed in the sclerogenic and post-inflammatory phase.
This important difference between children and adults with IgAN should be taken into due account in interpreting the therapeutic indications in guidelines [19••, 32] and in different position papers published in the last several years, after the large steroid trials performed in adults (the STOPIgAN [71••] and the TESTING trials [72]).
These trials observed an excess of steroid side effects which brought to debate the value of sustained supportive therapy against steroids in adult IgAN, although demonstrating a good efficacy of steroids in reducing proteinuria, which is the undiscussed greatest clinical risk factor for progression [73,74,75,76].
The KDIGO guidelines of 2012 suggest also for children to start supportive therapy with RAS blockers if proteinuria is below 1 g/day/1.73 m2. Cases with proteinuria above 1 g/day/1.73 m2 should be treated with a 3–6-month course of RASB if eGFR is stable and above 50 ml/min/1.73 m2, and only in cases with proteinuria persistently > 1 g/day/1.73 m2, a course of steroids should be attempted.
These suggestions were based only on proteinuria, without considering histology and other risk factors for progression and are therefore questionable at least for children, where the risk of delaying a potentially disease-modifying treatment, as steroids, is consistent.
These recommendations in the last controversy of the KDIGO working group of 2018 [31••] are indicated as requiring revision, which will be possibly released in the next years taking into account the trend toward personalized treatments basing upon modifiable risk factors.
Personalized treatment in IgAN in children: which parameters to consider to decide?
Although serological, immunological, and genetic biomarkers have strong rationale and a promising future, at present, the lack of standardization and wide availability leaves the clinician to rely substantially on only clinical and histological risk factors. Being strictly interconnected, the critical combined evaluation of both elements is necessary, taking into particular consideration the potential reversibility of both parameters.
Histology: M1 and S1
The VALIGA study, as previously stated, validated the MEST score as independent predictor of outcome in both adults [27] and children [26]. A specific sub-analysis exploring the effect of steroids/immunosuppression evidenced that patients paired with the same MEST score treated with steroids and ACE/ARB inhibitor compared with those treated with ACE/ARB inhibitor alone had better outcome [77].
Interestingly, the effect was particularly significant in cases with mesangial hypercellularity (Oxford MEST M1) versus non-proliferative (Oxford MEST M0): in the cohort of children and young adults aged < 23 years, M1 resulted a risk factor but the reduction of proteinuria below < 0.5 g/day by steroids/immunosuppressive agents blunted the risk. These data strongly suggest that M1 histology score in children and young adults represents a risk factor for progression, and that these subjects are those who mostly may benefit of such agents [78].
These data are further confirmed by a Japanese RCT [79] which demonstrated, over a long follow-up, that the 10-year probability of renal survival of children receiving steroids and azathioprine for 24 months was 97.1% vs 84.8% of those receiving only supportive therapy, with a probability of reaching proteinuria remission after 2 years of 100% vs 84% with supportive therapy. This RCT enrolled only children with severe mesangial hypercellularity giving further strength to the value of this histology risk factor, which can confidently be considered to decide for a steroids/immunosuppressive in children.
Another histology parameter recently critically re-evaluated is glomerular sclerosis (Oxford MEST S1) [80], with particular attention to podocyte lesions. Podocyte hypertrophy and/or tip lesions were associated with higher grades of proteinuria and higher rate of progression if untreated, and any type of steroid/immunosuppressive treatment significantly improved the outcome at 5 years, compared with no treatment.
These data, confirmed also by a small recent pediatric study [81], introduce the concept that podocyte lesions may be somehow reversible upon treatment; therefore, when dealing with children, thorough evaluation of these lesions and a course of treatment are highly recommendable.
On the other side, a recent retrospective study considered the outcome of an untreated cohort, including also children, selected for endocapillary proliferation (Oxford MEST E1): the renal survival at 15 years was less than 20%, significantly lower than in cases without endocapillary hypercellularity (E0) [63].
The side effects of corticosteroids in children in all studies were globally less severe compared with adults. Considering the long life expectancy, potentially effective and curative agents should not be denied from children, particularly when facing with potentially reversible lesions.
Clinical risk factors: blood pressure, proteinuria, and glomerular filtration rate
Hypertension in children is a very strong risk factor
Hypertension is an unanimously considered strong risk factor for progression in all renal diseases, particularly in children [82] and often underestimated in its value by general pediatricians.
In the pediatric cohort of the VALIGA study, mean arterial pressure (MAP) proved as a risk factor for GFR declines [78] stronger than proteinuria.
Referring back to the KDIGO guidelines [19••] and to the results of the STOP trial [71••], intensive supportive therapy and blood pressure optimization with RAS blockers are recommended, with an add-on approach to reach target MAP normalization and modify this risk factor.
Proteinuria but also hematuria
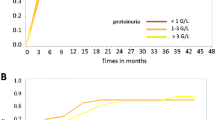
Proteinuria at onset and at time of biopsy in children has a moderate predictive value, being possible expression of an acute, reversible inflammatory damage. A higher weight was given in adults and children to persisting proteinuria, expressed as time-averaged proteinuria [83] or to hypoalbuminemia [84].
To which level proteinuria can be considered satisfactory allowing for positive prognosis is a matter of debate: a recent Japanese work [85] demonstrated in children that proteinuria < 1 g/day/1.73 m2 with normal serum albumin in a long-term follow-up of 25 years is protective over the decline of renal function, provided a good blood pressure control. Children with persisting proteinuria over 1 g/d/1.73 m2 and serum albumin < 3 g/dl had instead at 20 years renal survival lower than 20%.
The pediatric cohort of the VALIGA study [82] allowed to discriminate further lower proteinuria levels indicating as a protective target urine protein excretion of < 0.5 g/d/1.73 m2.
Hematuria is, amongst children, the dominant index parameter for referral for renal biopsy demonstrating IgAN: its prognostic value, however, is debated. Recurrent macroscopic hematuria has a recognized proinflammatory and prooxidant effect, but the difficulty to standardize the measurement unit produced contradictory results.
In a Spanish cohort [86], the deleterious effect of protracted hematuria on the decline of renal function was demonstrated but other studies have been unable to confirm the value of hematuria as an independent risk factor.
Although the harming effect of hematuria persistence is not clearly demonstrated, important attention must be payed to this parameter, taking into account the co-existence of other risk factors to consider a treatment, especially in children.
Immunosuppressants: when are they necessary?
The use of steroid-sparing immunosuppressants in IgAN with persistent proteinuria has been explored primarily with small scale underpowered RCT; therefore, the largely negative results have led to the widespread opinion, expressed also by the KDIGO, that unless facing rapidly deteriorating renal function, the use of immunosuppressants is not recommended, particularly at GFR of below 30 ml/min.
However, the pediatric nephrology community has gathered substantial good results upon their use [87] and the Guidelines of The Japanese Society of Nephrology released in 2016 [88] include specific recommendations addressing children. They[LP1] recommend with grade B the use of immunosuppressive drugs in cases with persistent proteinuria > 1 g/day/1.73 m2 and severe histology (Oxford MEST M1, S1 or C1), as a combination therapy for 2 years, indicating azathioprine as the drug of choice.
Mycophenolate mofetil
The increasing use of MMF in different clinical settings also in children led to an opening toward its use in the last KDIGO revision [31••] while data on some RCT are gathered and summated in a recent metanalysis [89].
The global limit of the studies done so far was the observation period of only 6 months, when none of the enrolled children/young adults was able to reach complete remission of proteinuria [90]. In a single center study in 33 children [91], MMF resistance was correlated to fibrosis and tubular atrophy, while cases with milder lesions had a beneficial effect on proteinuria reduction.
The main favorable responses were observed in the Asian population. Although not supported by strong data, the use of MMF as alternative to azathioprine in children may be explored in cases of steroid-resistant proteinuria, due to a minor side effect profile in comparison with cyclophosphamide.
Is there a space for new drugs in IgAN?
Beyond immunosuppressive therapy, new strategies are being explored, addressing different steps of the pathogenic cascade and possibly based on informative biomarkers. From a practical point of view, renal histology is still unavoidable and therapeutic decisions are still primarily tailored upon histological and clinical data; however, wider availability of pathobiological biomarkers could allow a hit-addressed therapy targeting earlier steps in the pathogenesis (Fig. 1).
The multihit model for the pathogenesis of IgA nephropathy with hit addressed therapy with old and new drugs. TLR, toll-like receptors; APRIL, a proliferation inducing ligand; BAFF, B cell-activating factor; TK inhibitors, tyrosine kinase inhibitors; GdA1, galactose-deficient immunoglobulin A; IgG anti-GdIgA, immunoglobulin G anti-galactose deficient immunoglobulin A; PAF inhibitor, platelet-activating factor inhibitor; C3, complement protein 3; C5, complement protein 5; anti-B, anti-complement factor B.
Mucosal response and B cells priming could be addressed by intestinal targeted-release steroids as budesonide [92, 93•] and drugs able to modify toll-like receptor recognition as hydroxychloroquine.
The production and deposition of galactose-deficient iga1 is an interesting experimental field with direct targeting of the altered glycan step [94], while several other approaches are being explored to target B cells to limit the production of anti-IgA IgG antibodies with rituximab, proteasome inhibitors, anti-B cell activating factor B (BAFF) blisibimod, and spleen tyrosine kinase inhibitors (fostamatinib) [93•, 95, 96].
A new and promising field is complement inhibition and several complement-targeting drugs are currently under clinical trial, addressed at both complement activation, inhibition, and receptor-binding interference (Table 2).
Other interesting approaches are targeting endothelin (Sparsentan) [97], limiting mesangial matrix production, and exploring podocyte effective drugs as bortezomib, amiloride, and platelet-activating factor inhibitors [98].
Conclusions
The understanding of the pathogenic steps of primary IgAN and HSPN/IgAVN, timely biopsy and thorough evaluation of individual risk factors, particularly in children, is of key importance for tailoring the most appropriate therapy.
The prevalence of proliferative and inflammatory lesions in children indicates the potential benefit of treatments geared towards the complete remission of the disease.
New therapeutic approaches are being explored acting from the earlier phases of the pathogenic cascade to the final effectors offering a wide catalog of options for precise personalized treatment.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Berger J, Hinglais N. Intercapillary deposits of IgA-IgG. J Urol Nephrol (Paris). 1968;74(9):694–5.
Feehally J, Cameron JS. IgA nephropathy: progress before and since Berger. Am J Kidney Dis. 2011;58 (2):310–9.
Levy M, Beaufils H, Gubler MC, Habib R. Idiopathic recurrent macroscopic hematuria and mesangial IgA-IgG deposits in children (Berger’s disease). Clin Nephrol. 1973;1(2):63–9.
Baart De La Faille-Kuyper EH, Kater L, Kooiker CJ, Mees EJD. IgA-deposits in cutaneous bloodvessel walls and mesangium in Henoch Schoenlein syndrome. Lancet. 1973;301(7808):892–3.
Faille-Kuyper EH, Kater L, Kuijten RH, Kooiker CJ, Wagenaar SS, van der Zouwen P, et al. Occurrence of vascular IgA deposits in clinically normal skin of patients with renal disease. Kidney Int. 1976;9(5):424–9.
• Davin J-C, Ten Berge IJ, Weening JJ. What is the difference between IgA nephropathy and Henoch-Schö nlein purpura nephritis? Kidney Int. 2001;59:823–34 Detailed discussion on differences and similarities of the two diseases.
Komatsu H, Fujimoto S, Yoshikawa N, Kitamura H, Sugiyama H, Yokoyama H. Clinical manifestations of Henoch–Schönlein purpura nephritis and IgA nephropathy: comparative analysis of data from the Japan Renal Biopsy Registry (J-RBR). Clin Exp Nephrol. 2016;20(4):552–60.
Hwang HH, Lim IS, Choi BS, Yi DY. Analysis of seasonal tendencies in pediatric Henoch-Schönlein purpura and comparison with outbreak of infectious diseases. Medicine (Baltimore). 2018;97(36):e12217.
Singh S, Aulakh R. Kawasaki disease and Henoch Schonlein purpura: changing trends at a tertiary care hospital in north India (1993–2008). Rheumatol Int. 2010;30(6):771–4.
Okubo Y, Nochioka K, Sakakibara H, Hataya H, Terakawa T, Testa M, et al. Nationwide epidemiological survey of childhood IgA vasculitis associated hospitalization in the USA. Clin Rheumatol. 2016;35(11):2749–56.
Heineke MH, Ballering AV, Jamin A, Ben Mkaddem S, Monteiro RC, Van Egmond M. New insights in the pathogenesis of immunoglobulin A vasculitis (Henoch-Schönlein purpura). Autoimmun Rev. 2017;16(12):1246–53.
Chan H, Tang YL, Lv XH, Zhang GF, Wang M, Yang HP, et al. Risk factors associated with renal involvement in childhood Henoch-Schönlein purpura: a meta-analysis. PLoS One. 2016;11(11):e0167346. https://doi.org/10.1371/journal.pone.0167346.
Coppo R, Lugani F, Jankauskiene A, Pecoraro C, Alessandrella A, Murer L, et al. TO044A European registry of Henoch Schoenlein purpura nephritis in children to detect risk factors for progression. Nephrol Dial Transplant. 2017;31(suppl_1):i80.
Coppo R, Mazzucco G, Cagnoli L, Lupo A, Schena FP. Long-term prognosis of Henoch-Schonlein nephritis in adults and children. Nephrol Dial Transplant. 1997;12(11):2277–83.
Hennies I, Gimpel C, Gellermann J, Möller K, Mayer B, Dittrich K, et al. Presentation of pediatric Henoch–Schönlein purpura nephritis changes with age and renal histology depends on biopsy timing. Pediatr Nephrol. 2018;33(2):277–86.
Coppo R, Andrulli S, Amore A, Gianoglio B, Conti G, Peruzzi L, et al. Predictors of outcome in Henoch-Schönlein nephritis in children and adults. Am J kidney Dis Off J Natl Kidney Found. 2006;47(6):993–1003.
Chartapisak W, Opastiraku SL, Willis NS, Craig JC, Hodson EM. Prevention and treatment of renal disease in Henoch-Schönlein purpura: a systematic review. Arch Dis Child. 2009;94(2):132–7.
Szemenyei C, Hahn D. Prevention of nephritis in Henoch-Schönlein purpura. J Paediatr Child Health. 2015;51(2):236–9.
•• Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group. KDIGO clinical practice guideline for glomerulonephritis. Kidnet Int Suppl. 2012;2(2):1–274 Worldwide adopted guideline of treatment of glomerulonephritis.
Dudley J, Smith G, Llewelyn-Edwards A, Bayliss K, Pike K, Tizard J. Randomised, double-blind, placebo-controlled trial to determine whether steroids reduce the incidence and severity of nephropathy in Henoch-Schonlein purpura (hsp). Arch Dis Child. 2013;98(10):756–63.
Hoyer PF. Prevention of renal disease in Henoch-Schönlein purpura: clear evidence against steroids. Arch Dis Child. 2013;98(10):750–1.
Delbet JD, Hogan J, Aoun B, Stoica I, Salomon R, Decramer S, et al. Clinical outcomes in children with Henoch–Schönlein purpura nephritis without crescents. Pediatr Nephrol. 2017;32(7):1193–9.
Cattran DC, Coppo R, Cook HT, Feehally J, Roberts ISD, Troyanov S, et al. The Oxford classification of IgA nephropathy: rationale, clinicopathological correlations, and classification. Kidney Int. 2009;76(5):534–45.
Coppo R, Troyanov S, Camilla R, Hogg RJ, Cattran DC, Cook HT, et al. The Oxford IgA nephropathy clinicopathological classification is valid for children as well as adults. Kidney Int. 2010;77(10):921–7.
•• Coppo R, Troyanov S, Bellur S, Cattran D, Cook HT, Feehally J, et al. Validation of the Oxford classification of IgA nephropathy in cohorts with different presentations and treatments. Kidney Int. 2014;86(4):828–36 The European validation study of the Oxford MEST classification of IgAN.
Ho Kim C, Jin Lim B, Sung Bae Y, Eun Kwon Y, Ly Kim Y, Heon Nam K, et al. Using the Oxford classification of IgA nephropathy to predict long-term outcomes of Henoch-Schönlein purpura nephritis in adults. Mod Pathol. 2014;27(7):972–82.
Xu K, Zhang L, Ding J, Wang S, Su B, Xiao H, et al. Value of the Oxford classification of IgA nephropathy in children with Henoch–Schönlein purpura nephritis. J Nephrol. 2018;31(2):279–86.
Hahn D, Hodson EM, Willis NS, Craig JC. Interventions for preventing and treating kidney disease in Henoch-Schönlein Purpura (HSP). Cochrane Database Syst Rev. 2015;(8):CD005128. https://doi.org/10.1002/14651858.
•• Davin J-C, Coppo R. Pitfalls in recommending evidence-based guidelines for a protean disease like Henoch–Schönlein purpura nephritis. Pediatr Nephrol. 2013;28(10):1897–903 Critical discussion of KDIGO guidelines for treatment of HSPN in children.
Katafuchi R, Ninomiya T, Mizumasa T, Ikeda K, Kumagai H, Nagata M, et al. The improvement of renal survival with steroid pulse therapy in IgA nephropathy. Nephrol Dial Transplant. 2008;23(12):3915–20.
•• Floege J, Barbour SJ, Cattran DC, Hogan JJ, Nachman PH, Tang SCW, et al. Management and treatment of glomerular diseases (part 1): conclusions from a Kidney Disease: improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019;95(2):268–80 Premises for the new KDIGO guidelines action.
Rovin BH, Caster DJ, Cattran DC, Gibson KL, Hogan JJ, Moeller MJ, et al. Management and treatment of glomerular diseases (part 2): conclusions from a Kidney Disease: improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019;95:281–95.
Selewski DT, Ambruzs JM, Appel GB, Bomback AS, Matar RB, Cai Y, et al. Clinical characteristics and treatment patterns of children and adults with IgA nephropathy or IgA vasculitis: findings from the CureGN study. Kidney Int Rep. 2018;3:1373–84.
Tarshish P, Bernstein J, Edelmann CM. Henoch-Schönlein purpura nephritis: course of disease and efficacy of cyclophosphamide. Pediatr Nephrol. 2004;19(1):51–6.
Pillebout E, Alberti C, Guillevin L, Ouslimani A, Thervet E. Addition of cyclophosphamide to steroids provides no benefit compared with steroids alone in treating adult patients with severe Henoch Schönlein Purpura. Kidney Int. 2010;78(5):495–502.
Ronkainen J, Autio-Harmainen H, Nuutinen M. Cyclosporin A for the treatment of severe Henoch-Schönlein glomerulonephritis. Pediatr Nephrol. 2003;18(11):1138–42.
Ohara S, Kawasaki Y, Miyazaki K, Ono A, Suzuki Y, Suyama K, et al. Efficacy of cyclosporine A for steroid-resistant severe Henoch-Schönlein purpura nephritis. Fukushima J Med Sci. 2013;59(2):102–7.
Andersen RF, Rubak S, Jespersen B, Rittig S. Early high-dose immunosuppression in HenochSchnlein nephrotic syndrome may improve outcome. Scand J Urol Nephrol. 2009;43(5):409–15.
Han F, Chen L-L, Ren P-P, Le J-Y, Choong P-J, Wang H-J, et al. Mycophenolate mofetil plus prednisone for inducing remission of Henoch-Schönlein purpura nephritis: a retrospective study*. J Zhejiang Univ-Sci B (Biomed Biotechnol). 2015;16(9):772–9.
Dede F, Onec B, Ayli D, Gonul II, Onec K. Mycophenolate mofetil treatment of crescentic Henoch-Schönlein nephritis with IgA depositions. Scand J Urol Nephrol. 2008;42(2):178–80.
Du Y, Hou L, Zhao C, Han M, Wu Y. Treatment of children with Henoch-Schönlein purpura nephritis with mycophenolate mofetil. Pediatr Nephrol. 2012;27(5):765–71.
Hackl A, Becker JU, Körner LM, Ehren R, Habbig S, Nüsken E, et al. Mycophenolate mofetil following glucocorticoid treatment in Henoch-Schönlein purpura nephritis: the role of early initiation and therapeutic drug monitoring. Pediatr Nephrol. 2018;33(4):619–29.
Nikibakhsh AA, Mahmoodzadeh H, Karamyyar M, Hejazi S, Noroozi M, Macooie AA. Treatment of severe Henoch-Schönlein purpura nephritis with mycophenolate mofetil. Saudi J Kidney Dis Transpl. 2014;25(4):858–63.
Lu Z, Song J, Mao J, Xia Y, Wang C. Evaluation of mycophenolate mofetil and low-dose steroid combined therapy in moderately severe Henoch-Schönlein purpura nephritis. Med Sci Monit. 2017;23:2333–39.
Fenoglio R, Naretto C, Basolo B, Quattrocchio G, Ferro M, Mesiano P, et al. Rituximab therapy for IgA-vasculitis with nephritis: a case series and review of the literature. Immunol Res. 2017;65(1):186–92.
Pindi Sala T, Michot J-M, Snanoudj R, Dollat M, Estève E, Marie B, et al. Successful outcome of a cortico dependent Henoch-Schönlein purpura adult with rituximab. Case Rep Med. 2014;2014:1–4.
Pillebout E, Rocha F, Fardet L, Rybojad M, Verine J, Glotz D. Successful outcome using rituximab as the only immunomodulation in Henoch-Schonlein purpura: case report. Nephrol Dial Transplant. 2011;26(6):2044–6.
El-Husseini A, Ahmed A, Sabucedo A, Fabulo E. Refractory Henoch Schoenlein purpura: atypical aetiology and management. J Ren Care. 2013;39(2):77–81.
Thomas SR, Mohr DSR. Nitric oxide inhibits indoleamine 2,3-dioxygenase activity in interferon-gamma primed mononuclear phagocytes. J Biol Chem. 1994;269:14457–64.
Ishiguro H, Hashimoto T, Akata M, Suzuki S, Azushima K, Kobayashi Y, et al. Rituximab treatment for adult purpura nephritis with nephrotic syndrome. Intern Med. 2013;52(10):1079–83.
Crayne CB, Eloseily E, Mannion ML, Azerf SP, Weiser P, Beukelman T, et al. Rituximab treatment for chronic steroid-dependent Henoch-Schonlein purpura: 8 cases and a review of the literature. Pediatr Rheumatol Online J. 2018;16(1);71. https://doi.org/10.1186/s12969-018-0285-2.
Maritati F, Fenoglio R, Pillebout E, Emmi G, Urban ML, Rocco R, et al. Brief report: rituximab for the treatment of adult-onset IgA vasculitis (Henoch-Schönlein). Arthritis Rheum. 2018;70(1):109–14.
Lundberg S, Westergren E, Smolander J, Bruchfeld A. B cell depleting therapy with rituximab or ofatumumab in immunoglobulin A nephropathy or vasculitis with nephritis. Clin Kidney J. 2017;10(1):20–6.
Coppo R. Pediatric IgA nephropathy: clinical and therapeutic perspectives. Semin Nephrol. 2008;28(1):18–26.
Yanagihara T, Kuroda N, Hayakawa M, Yoshida J, Tsuchiya M, Yamauchi K, et al. Epidemiology of school urinary screening over a 30 year period in Tokyo. Pediatr Int. 2007;49(5):570–6.
Iwasaki C, Moriyama T, Tanaka K, Takei T, Nitta K. Effect of hematuria on the outcome of immunoglobulin A nephropathy with proteinuria. J Nephropathol. 2016;5(2):72–8.
Yang H, Wang Q, Luo J, Li Q, Wang L, Li C-C, et al. Ultrasound of urinary system and urinary screening in 14,256 asymptomatic children in China. Nephrology (Carlton). 2010;15(3):362–7.
Shima Y, Nakanishi K, Hama T, Sato M, Mukaiyama H, Togawa H, et al. Biopsy timing and Oxford classification variables in childhood/adolescent IgA nephropathy. Pediatr Nephrol. 2015;30(2):293–9.
•• Coppo R, Davin JC. The difficulty in considering modifiable pathology risk factors in children with IgA nephropathy: crescents and timing of renal biopsy. Pediatr Nephrol. 2014;30(2):189–92 Discussion on the value of timely biopsy in children.
•• Roberts ISD, Cook HT, Troyanov S, Alpers CE, Amore A, Barratt J, et al. The Oxford classification of IgA nephropathy: pathology definitions, correlations, and reproducibility. Kidney Int. 2009;76(5):546–56 The histological details of Oxford MEST classification for IgAN.
Shima Y, Nakanishi K, Hama T, Mukaiyama H, Togawa H, Hashimura Y, et al. Validity of the Oxford classification of IgA nephropathy in children. Pediatr Nephrol. 2012;27(5):783–92.
Le W, Zeng C-H, Liu Z, Liu D, Yang Q, Lin R-X, et al. Validation of the Oxford classification of IgA nephropathy for pediatric patients from China. BMC Nephrol. 2012.
Chakera A, MacEwen C, Bellur SS, Chompuk LO, Lunn D, Roberts ISD. Prognostic value of endocapillary hypercellularity in IgA nephropathy patients with no immunosuppression. J Nephrol. 2016.
Haas M, Verhave JC, Liu Z-H, Alpers CE, Barratt J, Becker JU, et al. A multicenter study of the predictive value of crescents in IgA nephropathy. J Am Soc Nephrol. 2017;28(2):691–701.
Shen XH, Liang SS, Chen HM, Le WB, Jiang S, Zeng CH, et al. Reversal of active glomerular lesions after immunosuppressive therapy in patients with IgA nephropathy: a repeat-biopsy based observation. J Nephrol. 2015;28:441–9. https://doi.org/10.1007/s40620-014-0165-x.
Shima Y, Nakanishi K, Hama T, Mukaiyama H, Togawa H, Sako M, et al. Spontaneous remission in children with IgA nephropathy. Pediatr Nephrol. 2013;28:71–6. https://doi.org/10.1007/s00467-012-2294-6.
Suzuki H, Kiryluk K, Novak J, Moldoveanu Z, Herr AB, Renfrow MB, et al. The pathophysiology of IgA nephropathy. J Am Soc Nephrol. 2011;22(10):1795–803.
Al Hussain T, Hussein MH, Al Mana H, Akhtar M. Pathophysiology of IgA nephropathy. Adv Anat Pathol. 2017;24:56–62.
Daha MR, van Kooten C. Role of complement in IgA nephropathy. J Nephrol. 2016;29(1):1–4.
Rauen T, Floege J. Inflammation in IgA nephropathy. Pediatr Nephrol. 2017;32(12):2215–24.
•• Rauen T, Eitner F, Fitzner C, Sommerer C, Zeier M, Otte B, et al. Intensive supportive care plus immunosuppression in IgA nephropathy. N Engl J Med. 2015;373(23):2225–36 STOPIgAN trial on the questioned use of steroids in adults.
Lv J, Zhang H, Wong MG, Jardine MJ, Hladunewich M, Jha V, et al. Effect of oral methylprednisolone on clinical outcomes in patients with IgA nephropathy: The TESTING randomized clinical trial. JAMA - J Am Med Assoc. 2017;318(5):432–42.
Glassock RJ. Moderator’s view: treatment of IgA nephropathy - getting comfortable with uncertainty. Nephrol Dial Transplant. 2016;31(11):1776–80.
Pozzi C. Pro: STOP immunosuppression in IgA nephropathy? Nephrol Dial Transplant. 2016;31:1766–70.
Locatelli F, Del Vecchio L, Ponticelli C. Should we really STOP treating patients with IgA nephropathy with steroids? Physiol Int. 2018;105:101–9. https://doi.org/10.1556/2060.105.2018.2.10.
Rauen T, Eitner F, Fitzner C, Floege J. Con: STOP immunosuppression in IgA nephropathy. Nephrol Dial Transplant. 2016;31:1771.
Tesar V, Troyanov S, Bellur S, Verhave JC, Cook HT, Feehally J, et al. Corticosteroids in IgA nephropathy: a retrospective analysis from the VALIGA study. J Am Soc Nephrol. 2015;26(9):2248–58.
Coppo R, Lofaro D, Camilla RR, Bellur S, Cattran D, Cook HT et al Risk factors for progression in children and young adults with IgA nephropathy: an analysis of 261 cases from the VALIGA European cohort. Pediatr Nephrol. 2017;32:139–50.
Kamei K, Nakanishi K, Ito S, Saito M, Sako M, Ishikura K, et al. Long-term results of a randomized controlled trial in childhood IgA nephropathy. Clin J Am Soc Nephrol. 2011;6(6):1301–7.
Bellur SS, Lepeytre F, Vorobyeva O, Troyanov S, Cook HT, Roberts IS, et al. Evidence from the Oxford Classification cohort supports the clinical value of subclassification of focal segmental glomerulosclerosis in IgA nephropathy. Kidney Int. 2016;91(1):235–43.
Cambier A, Rabant M, Peuchmaur M, Hertig A, Deschenes G, Couchoud C, et al. Immunosuppressive treatment in children with IgA nephropathy and the clinical value of podocytopathic features. Kidney Int Rep. 2018;3(4):916–25.
Wühl E, Trivelli A, Picca S, Litwin M, Peco-Antic A, Zurowska A, et al. Strict blood-pressure control and progression of renal failure in children. N Engl J Med. 2009;361(17):1639–50.
Barbour SJ, Cattran DC, Espino-Hernandez G, Hladunewich MA, Reich HN. Identifying the ideal metric of proteinuria as a predictor of renal outcome in idiopathic glomerulonephritis. Kidney Int. 2015;88(6):1392–401.
Xie J, Kiryluk K, Wang W, Wang Z, Guo S, Shen P, et al. Predicting progression of IgA nephropathy: new clinical progression risk score. PLoS One. 2012;7(6):e38904.
Kamei K, Harada R, Hamada R, Sakai T, Hamasaki Y, Hataya H, et al. Proteinuria during follow-up period and long-term renal survival of childhood IgA nephropathy. PLoS One. 2016;11(3):1–11.
Sevillano AM, Gutiérrez E, Yuste C, Cavero T, Mérida E, Rodríguez P, et al. Remission of hematuria improves renal survival in IgA nephropathy. J Am Soc Nephrol. 2017;28(10):3089–99.
Coppo R. IgA nephropathy: a European perspective in the corticosteroid treatment. Kidney Dis (Basel, Switzerland). 2018;4(2):58–64.
Yuzawa Y, Yamamoto R, Takahashi K, Katafuchi R, Tomita M, Fujigaki Y, et al. Evidence-based clinical practice guidelines for IgA nephropathy 2014. Clin Exp Nephrol. 2016;20(4):511–35.
Du B, Jia Y, Zhou W, Min X, Miao L, Cui W. Efficacy and safety of mycophenolate mofetil in patients with IgA nephropathy: an update meta-analysis. BMC Nephrol. 2017;18(1):245.
Hogg RJ, Bay RC, Jennette JC, Sibley R, Kumar S, Fervenza FC, et al. Randomized controlled trial of mycophenolate mofetil in children, adolescents, and adults with IgA nephropathy. Am J Kidney Dis. 2015;66(5):783–91.
Li Z, Duan C, He J, Wu T, Xun M, Zhang Y, et al. Mycophenolate mofetil therapy for children with steroid-resistant nephrotic syndrome. Pediatr Nephrol. 2010;25(5):883–8.
Fellström BC, Barratt J, Cook H, Coppo R, Feehally J, de Fijter JW, et al. Targeted-release budesonide versus placebo in patients with IgA nephropathy (NEFIGAN): a double-blind, randomised, placebo-controlled phase 2b trial. Lancet. 2017;389(10084):2117–27.
Coppo R. The gut–kidney axis in IgA nephropathy: role of microbiota and diet on genetic predisposition. Pediatr Nephrol. 2018; Review on the role of gut in the pathogenesis of IgAN.
Xie LS, Huang J, Qin W, Fan JM. Immunoglobulin A1 protease: a new therapeutic candidate for immunoglobulin A nephropathy. Nephrology. 2010;15(5):584–6.
Coppo R. Biomarkers and targeted new therapies for IgA nephropathy. Pediatr Nephrol. 2017;32:725–31.
Coppo R. Treatment of IgA nephropathy: recent advances and prospects. Nephrol Ther. 2018;Suppl 1:S13–S21.
Davenport AP, Kuc RE, Southan C, Maguire JJ. New drugs and emerging therapeutic targets in the endothelin signaling pathway and prospects for personalized precision medicine. Physiol Res. 2018;67(Supplement 1):S37–S54.
Trimarchi H, Coppo R. Podocytopathy in the mesangial proliferative immunoglobulin A nephropathy: new insights into the mechanisms of damage and progression. Nephrol Dial Transplant. 2019. https://doi.org/10.1093/ndt/gfy413.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Licia Peruzzi, Enrico Cocchi, and Flavio Tarizzo declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Nephrology
Rights and permissions
About this article
Cite this article
Peruzzi, L., Cocchi, E. & Tarizzo, F. Old and New Treatment Options in IgA Nephropathy and Henoch Schönlein Purpura Nephritis/IgA Vasculitis in Children. Curr Treat Options Peds 5, 236–254 (2019). https://doi.org/10.1007/s40746-019-00168-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40746-019-00168-1