Abstract
Purpose of review
Autoimmune encephalitis (AE) is an increasingly recognized etiology for neuropsychiatric deficits that are highly responsive to immunotherapy. As a result, rheumatologists are often called upon to help with the diagnosis and treatment of these conditions. The purpose of this review is to provide an update on the pharmacologic treatment of AE.
Recent findings
To date, there are no prospective randomized placebo-controlled trials to guide treatment recommendations for AE. First-line therapies include corticosteroids, intravenous immunoglobulin, and plasma exchange. Second-line therapies include rituximab and cyclophosphamide (CYC), as well as mycophenolate mofetil and azathioprine. For patients refractory to both first- and second-line therapy, there is emerging evidence for the interleukin-6 (IL-6) inhibitor tocilizumab, the proteasome inhibitor bortezomib, and low-dose IL-2. Early treatment initiation and treatment escalation in patients with refractory disease improve outcomes. Given the delayed time between dosing and treatment effects of second-line agents, continuing first-line treatment until the patients shows improvement is recommended.
Summary
Although AE can present with dramatic, life-threatening neuropsychiatric deficits, the potential for recovery with prompt treatment is remarkable. First- and second-line therapies for AE lead to clinical improvement in the majority of patients, including full recoveries in many. Early treatment and escalation to second-line therapy in those with refractory disease improves patient outcomes. Novel treatments including IL-6 blockade and proteasome inhibitors have shown promising results in patients with refractory disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autoimmune encephalitis (AE) is an increasingly recognized etiology of acute neuropsychiatric decline in adults and children. The clinical manifestations of AE are broad and include seizures, movement disorders, behavior and mood changes, psychosis, memory/cognitive impairment, autonomic dysfunction, and altered level of consciousness [1,2,3]. Recently proposed diagnostic criteria provide a framework for making a diagnosis of AE [4]. However, the substantial variability in presenting symptoms, severity, and progression of disease both within and across subtypes of AE, along with the lack of clear treatment recommendations, complicates management. Currently, there are no randomized trials for the treatment of AE and evidence for treatment comes primarily from case reports and cohort studies.
AE starts as an immune response triggered by infection, neoplasm, or unknown genetic and environmental triggers, which ultimately results in an autoimmune process targeting the brain [2, 5]. The immune reaction can be cell mediated, antibody mediated, or both, resulting in a spectrum of neurologic and psychiatric manifestations. While historically considered a paraneoplastic condition primarily in adults, the discovery of anti-neuronal antibodies targeting cell surface receptors has changed the framework and therapeutic approach of AE. Paraneoplastic AE results from neuronal injury and death due to T cell-mediated immunity [6]. The associated autoantibodies are not directly pathogenic and there is minimal reversibility with immunotherapy. In contrast, antibodies that target cell surface receptors are themselves pathogenic. They bind receptors and directly alter neuronal function without causing neuronal death [1, 7]. As a result, these conditions are remarkably sensitive to immunotherapy. It is important to note, however, that a chronically inflamed brain is more likely to sustain injury and long-term damage, highlighting the importance of early treatment and prompt escalation of therapy if children are not responding to initial treatment [8, 9].
Recently published diagnostic criteria for adult AE emphasize recognition of probable AE and initiation of treatment early to maximize potential recovery [4]. It is agreed in both adult and pediatric literature that patients treated early have improved outcomes. While work to modify and validate these diagnostic classifications for pediatric patients is currently in progress, the conceptual framework of these criteria is helpful to guide when to initiate treatment. A diagnosis of possible AE is made when patients present with acute to subacute onset (rapid progression of less than 3 months) of working memory deficits, altered mental status, or psychiatric symptoms, with at least one additional defined abnormality on evaluation (Table 1). Subsequent diagnostic criteria are presented for the various AE subtypes, including definite limbic encephalitis, acute disseminated encephalomyelitis, anti-NMDA receptor encephalitis, Hashimoto’s encephalopathy, and autoantibody-negative but probable AE [4]. While there is significant overlap in the presentations of adults and children, there are also important differences. Pediatric specific diagnostic criteria are currently in development to account for these differences.
Currently, there are no prospective trials for immunomodulatory treatments for AE. The majority of the evidence for treatment comes from a few larger retrospective observational cohort studies and numerous small case series and case reports [10]. The first neuronal surface autoantibody reported was anti-N-Methyl-D-aspartate (NMDA) and it is currently the most prevalent in children [11]. As a result, the most robust data for clinical findings and treatment recommendations for AE in children are from patients with anti-NMDA receptor (NMDAR) encephalitis. The principles of treatment of NMDAR encephalitis are considered by experts in the field to apply more generally to other forms of AE as well. The general framework for treatment may be divided into first-line, second-line, and maintenance therapy [12]. First-line therapies include steroids, intravenous immunoglobulin, and plasma exchange, all of which have a rapid onset of action and relatively low associated risks. If patients respond promptly to these therapies, the use of prolonged immunosuppressant therapy, or second-line agents, is not necessarily needed. However, if patients are not showing improvement or are worsening, escalation to second-line therapy is warranted. Second-line therapy, including rituximab and cyclophosphamide, are considered higher risk medications given their longer duration of action and increased immunosuppressive nature. The timing of when to escalate is not established. For those requiring inpatient care, many escalate to second-line therapy if the child is not improving within 10–14 days of initiating first-line therapy [13]. The data for those managed in the outpatient setting is less clear and likely varies depending on physician assessment of symptom severity and AE subtype. Our standard practice is to give at least 1 to 2 months to assess response to first-line therapy, escalating sooner if the patient worsens.
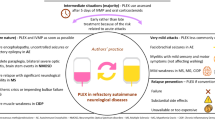
Children with refractory disease may benefit from more novel treatments as well. Expert opinion in both adults and children is that treatment should be initiated once a diagnosis of AE is suspected, as autoantibody testing can take weeks to result, and many patients who meet the clinical criteria for AE will not have a detectable known anti-neuronal antibody. Given diagnostic criteria for adult anti-neuronal antibody-negative AE was just recently proposed and no pediatric criteria exist, the percentage of children with seronegative disease is unknown. In our clinical experience, up to a quarter of the children we care for have antibody-negative disease. While the identification of novel surface anti-neuronal antibodies continues to expand, the absence of an autoantibody should not dissuade treatment of children who meet the clinical diagnosis of AE [2, 11].The purpose of this review is to report current treatments for pediatric AE. We will highlight the stepwise approach to immunotherapy (Fig. 1) currently used in practice with a focus on both the physiologic and practical rationale for selecting various treatment options.
Probable autoimmune encephalitis. PE = Plasma exchange, IV steroids = IV methylprednisolone or dexamethasone. Second-line agents include rituximab, mycophenolate mofetil, azathioprine. *Depending on severity and results of evaluation consider IV steroids alone vs adding IVIG. Recommend 3–6 months of sustained treatment before tapering. †Continue first-line therapy with IVIG and IV steroids while giving time for second-line therapy to take effect, then slowly taper off to ensure no recurrence of symptoms.
Treatment
First-line
The preponderance of studies to date demonstrates the efficacy of corticosteroids and IVIG, which are widely considered first-line medications for the treatment of suspected AE. Plasma exchange is also considered first-line therapy, though many in pediatrics reserve it for those with more severe disease, such as those requiring ICU level care [12]. Compared with other agents discussed in this paper, first-line therapies generally have a shorter latency to effect, proving them more useful in the immediate setting. These medications are often administered concurrently with or shortly after a thorough workup of the patient once AE is suspected, as patients treated earlier in the course of their disease had improved outcomes compared to those treated later [9]. New recommendations encourage the initiation of first-line therapy once criteria for probable AE are met, prior to detection of a specific anti-neuronal antibody [4]. These first-line therapies (Table 2) are broad in their mechanisms of action and can therefore be utilized empirically. To illustrate this point, children with antibody-negative AE have similar response to first-line therapies compared with those who have a confirmed autoantibody [14]. Even children with a “missed” diagnosis who have had symptoms for months to years can show dramatic responses to immunotherapy. Therefore, regardless of antibody status or duration of symptoms, once a diagnosis of possible or definite AE is made, initiating therapy as soon as possible is indicated. While not discussed in detail in this paper, tumor removal in anti-NMDAR encephalitis and paraneoplastic diseases is an essential component of treatment [1, 14,15,16].
Steroids
Intravenous corticosteroids have long been the mainstay of first-line treatment in patients with acute exacerbation of a variety of autoimmune diseases. They have numerous effects on the immune system, including reduced leukocyte trafficking into tissues, reduced production of inflammatory cytokines, inhibition of interleukin-2, and T cell depletion. They are useful for CNS-involving disease because they have good penetration into the brain and modulate the blood-brain barrier. However, their use for AE is largely based on retrospective case reports in adult patients or extrapolated from data for other neurologic autoimmune diseases. Steroids do appear to increase the likelihood of good outcomes in patients across the spectrum of AE [1, 17, 18].
While corticosteroid regimens vary by provider, we generally start with intravenous(IV) methylprednisolone at 30 mg/kg (maximum dose of 1000 mg) once daily for 3 to 5 days. Dosing can be repeated depending on response and results of initial evaluation. There are no clear guidelines on how frequently to give repeat dosing. Our practice varies by severity of disease and response to steroids. We consider standard dosing of one infusion every 4 weeks for 3 months in the outpatient setting, but will commonly use dosing every 2 weeks or weekly in those with more severe disease, such as those requiring ICU-level care. We typically avoid oral steroid tapers as we find fewer side effects with intermittent IV dosing compared to prolonged oral steroid use, with reduced complications from mood/behavior changes, sleep disturbances, hypertension, hyperglycemia, and weight gain. If a patient has a good response to steroids but is unable to tolerate decreased dosing or extended dosing intervals, this indicates a more prolonged, ongoing inflammatory state that warrants an additional agent. However, we recommend additive therapy, such that additional agents are combined with continued steroids until the disease becomes well controlled. Only once the patient has demonstrated stability will we decrease the dose of steroids or space the infusions.
Some patients appear to improve with an initial course of IV corticosteroids (3–5 days in a row) but relapse quickly, making it difficult to ascertain whether they were truly steroid responsive. In patients with either antibody-positive or antibody-negative disease where the risks vs benefits of escalating immunotherapy are questioned, it is reasonable to stack steroid doses, giving weekly infusions (one dose weekly) for 4 weeks to establish if they have clinical improvement. A similar approach has been used in autoimmune epilepsy to help establish reversibility with immunotherapy prior to escalating immunotherapy [19]. In addition, we have used dexamethasone with good effect in rare cases when patients with severe disease have minimal response to IV methylprednisolone [20, 21].
IVIG
Intravenous immunoglobulin (IVIG) is commonly given in conjunction with IV corticosteroids in the acute treatment of AE, although there are reports of its use alone. Its mechanism of action in suppressing the autoimmune response is broad, impacting both innate and adaptive immunity. This includes increasing B cell apoptosis and decreasing B cell proliferation, inhibiting complement activation, neutralizing cytokines, inhibiting dendritic cell differentiation, modulating regulatory T cells, and improving clearance of the pathogenic antibody by saturation of the FcRn receptor [22]. There are randomized trials showing evidence of efficacy of IVIG in non-encephalitic inflammatory neurologic diseases [23]. However, its use for AE is based on case reports and retrospective case series. Several retrospective studies in children specifically have shown improvement in functional outcome with the use of IVIG [2, 14, 24]. A randomized trial in children with encephalitis comparing IVIG with placebo is now ongoing [25].
While many providers report the administration of 2 g/kg IVIG divided over the course of 5 days, we have found that our pediatric patients tolerate a condensed 2-day administration quite well. The optimal dosing of IVIG for AE is not known; however, data from Kawasaki disease suggests higher dose IVIG given over a shorter duration is maximally effective at reducing inflammation quickly. Given the risks of infusion reactions, aseptic meningitis, and other complications of high dose IVIG, induction with 2 g/kg is usually given over 2 days, with monthly maintenance infusions of 1 g/kg over 1 day. Similar to IV steroids, if a patient is unable to taper off IVIG ± steroids by 6 months from initiation, or relapses during this time, we will add an additional disease-modifying agent.
Plasma exchange/plasmapheresis
Plasma exchange (PE), which involves removal and replacement of host plasma with human albumin or fresh frozen plasma, can be an effective adjunctive therapy in combination with steroids and/or IVIG. It is rarely used as monotherapy, but rather in those patients who have responded incompletely to steroids or IVIG and remain hospitalized [13]. Several retrospective studies have shown that PE plus steroids provides significant improvement in modified Rankin scores (mRS) compared with steroids alone [1, 26]. One prospective case control study showed improvement in mRS score (irrespective of prior immunotherapy) with both PE. PE appeared more effective for patients with cell surface autoantibodies (NMDA, LGI1, CASPR, mGluR5) compared with intracellular (Hu, GAD) antigens, consistent with the differences in disease pathogenesis previously discussed. Additionally, greater efficacy was seen in younger patients [27]. However, PE is associated with more adverse events compared with the aforementioned therapies and is therefore not favored as first-line [12]. The most common complications include infection, hypotension, and electrolyte imbalances due to fluid shifts. Additionally, PE is more invasive as it necessitates a central catheter in children, and generally requires at least five sessions to sufficiently remove the offending antibodies. Protocols differ by institution with some receiving daily PE and others spaced to 2–3 per week. One must also be mindful of using PE shortly after IVIG or rituximab, as it will effectively remove these therapeutic antibodies. Studies have demonstrated significant clearance of rituximab if given within 3 days prior to plasmapheresis [28]. Our protocol is to give at least 5 days between rituximab infusion and the next cycle of plasmapheresis and to give IVIG once PE is complete, bridging with IV steroids after each PE cycle.
While there are a handful of prospective studies and small randomized trials demonstrating the efficacy of PE in adults with AE, studies in children are lacking. Because of this and the potential complications, we rarely utilize PE unless the child is severely affected in an ICU setting (due to seizures, dysautonomia, or coma), and steroids and IVIG have not been effective.
Second-line
Second-line therapy classically consists of rituximab and cyclophosphamide (CYC), though oral anti-metabolite agents such as mycophenolate mofetil (MMF) and azathioprine (AZA) may also be considered. In surveys of neurologists and rheumatologists, European providers were more likely to treat with oral anti-metabolites than their US counterparts [13]. Current expert opinion is to start second-line therapy in hospitalized patients if they are not showing signs of improvement within 10–14 days of first-line therapy [11]. While it is important to give adequate time for first-line therapy to take effect, one must not delay escalation of therapy if the patient is not improving. Significantly more patients with NMDAR encephalitis had a good outcome when treated early compared to those with delayed escalation of therapy [8, 29].
Given that AE is classically considered an antibody-mediated disease, we will first review antibody production. B cells are essential to antibody production through their differentiation into short lived plasma cells, or plasmablasts, and long-lived plasma cells. Plasmablasts are active, rapidly cycling cells which are the source of early antibody production and may be the primary cell type responsible for autoantibody production. This finding helps explain the rapid decline in autoantibody titers compared to overall immunoglobulin levels or protective anti-microbial antibodies with medications that target plasmablasts over long-lived plasma cells, such as rituximab. Ongoing autoantibody production in chronic autoimmune diseases requires continual development of plasmablasts from B cells, or their progression into long-lived plasma cells [30]. Long-lived plasma cells develop under the influence of follicular T helper cells in germinal centers [31]. While plasmablasts are rapidly cycling cells, plasma cells are post-mitotic, having silenced their cell cycle programming. They are therefore not susceptible to medications targeting the cell cycle/proliferation. Though these plasma cells have the potential to be long-lived antibody producers, their survival appears to depend on their microenvironment and continued stimulation from cytokines and other factors, including interleukin 6 (IL-6) and tumor necrosis factor (TNF). If the antibody is primarily produced by plasmablasts, one would expect more susceptibility to medications that target cell division. However, long-lived plasma cells will not be as susceptible to these treatments and may preferentially respond to medications targeting cytokines or factors necessary to maintain plasma cell longevity.
Rituximab
Rituximab is a monoclonal, chimeric anti-CD20 antibody which acts to deplete B cells and CD20 expressing plasmablasts through both cell-meditated and complement-mediated cytotoxicity. It is important to note that rituximab does not target plasma cells. Though rituximab is classically considered a B cell treatment, ongoing studies have demonstrated more broad anti-inflammatory effects. Rituximab depletes B cells, preventing their development into antibody-producing plasma cells, and directly depletes plasmablasts [32]. In addition, it reduces production of cytokines that stimulate plasma cells and pro-inflammatory CD4 and CD8 T cell responses [33].
Rituximab can be used alone or in combination with CYC for those who require second-line treatment. A large survey of adult neurologists, pediatric neurologists, and pediatric rheumatologists revealed that the majority agreed with the choice of rituximab alone as second-line treatment (60% of US responses vs 53% of other countries) [13]. Studies in both adults and children demonstrate the efficacy of rituximab [20, 34,35,36]. Several large cohort studies of pediatric patients with NMDAR encephalitis have highlighted that over half of children will require second-line therapy with rituximab chosen most often. Overall outcomes even in children requiring second-line treatments are excellent with the majority having minimal residual disease [3]. The largest cohort study of NMDAR encephalitis to date demonstrated that patients who received second-line therapy with rituximab ± CYC had improved outcomes compared to those who did not [2]. While treatment with rituximab has been suggested to reduce relapse risk, there is insufficient data to make this assessment currently [36].
Common protocols include either weekly dosing for 4 weeks at 375 mg/m2 per dose, or 750 mg/m2 for two doses 2 weeks apart, with a maximum of 1000 mg per dose in both protocols. We prefer to use the latter in our practice. We also recommend continuing first-line therapy while waiting for the immunomodulatory effects of rituximab which typically takes several weeks to months to take effect. The ideal dosing of rituximab has not been determined. One small study of 10 patients with NMDAR encephalitis used low dose rituximab (100 mg IV weekly for 4 weeks), resulting in 30% of their patients with a full recovery, 5 with partial response and 1 who failed to improve [37]. While peripheral depletion of B cells is seen at lower doses, higher doses and serum levels are needed for depletion in extravascular sites [38]. Additionally, higher doses are associated with higher CNS concentrations, though the ideal dosing and necessary CNS concentration for efficacy are not known. Given the limited CNS bioavailability of rituximab, if the patient has significant intrathecal antibody production and fails to respond to treatment, other agents should be considered.
The safety of rituximab in pediatric neurologic disease was reviewed in a study of 144 children with a variety of autoimmune neurologic diseases, including 39 children with NMDAR encephalitis. Rituximab was found to be well tolerated overall. Infusion reactions occurred in 12% but responded to treatment with anti-histamines and steroids. Only one patient was unable to tolerate re-dosing of rituximab. Eight percent of children developed serious infections that were at least in part attributed to rituximab, and only one patient had neutropenia [8]. Progressive multifocal leukoencephalopathy has not been reported in the NMDAR encephalitis literature in the > 130 patients treated with rituximab alone or in combination with other immunomodulatory agents [8, 10]. Similar rates of side effects to rituximab have been reported in pediatric cohorts with NMDAR encephalitis [3]. Additionally, rituximab has been used safely in children with post-herpes simplex NMDAR encephalitis [39]. Monitoring of blood counts, lymphocyte panel, and immunoglobulins is necessary as children can develop cytopenias, persistent B cell depletion, and prolonged hypogammaglobulinemia.
Cyclophosphamide
CYC is classified as an alkylating agent with antimitotic and anti-replicative effects through inhibition of DNA synthesis [40, 41]. CYC has broad effects on the immune system, suppressing cell-mediated and humoral immunity through its actions on T cells and B cells, but may be less efficacious with long-lived plasma cells [42]. CYC has an advantage in CNS autoimmunity due to its bioavailability within the CNS. Consequently, it may induce local immunomodulation and immunosuppression even after the formation of lymphatic tissues in the CNS, stabilizing the disease and preventing further progression. Evidence of the direct intrathecal and intracerebral actions of CYC on compartmentalized immune cells was provided in studies of both multiple sclerosis and in anti-glutamic acid decarboxylase (GAD) antibody associated epilepsy. In GAD-associated refractory status epilepticus, treatment with CYC resulted in cessation of seizures and intrathecal production of anti-GAD antibody [43].
CYC has been reported as part of the treatment armamentarium for anti-NMDAR encephalitis for a decade [12, 44] and more recently for AE in general [45]. There are no clinical trials supporting the use of CYC in AE or defining optimal dosing recommendations. Though CYC is clearly considered a second-line therapy, it is used less frequently than rituximab in pediatric AE due to its side effect profile [13]. In our practice, we reserve CYC for refractory disease. Duration of therapy varies from two doses in conjunction with rituximab, to more chronic therapy from 3 to 24 months depending on severity and response to treatment. There are numerous potential severe adverse effects including infertility, infection, and malignancy that likely explain the preference for other immunomodulatory therapy.
Mycophenolate mofetil and azathioprine
Though rituximab and CYC are the most frequently used second-line agents, oral agents (MMF or AZA) may have utility as well. Their use is more prevalent in Europe compared to the USA (15 vs 5%), but there are inadequate data to make conclusions about their efficacy in AE [10, 13, 36, 46]. In our experience, these medications can be helpful for patients who have had significant benefits from first-line therapy but are unable to taper IV steroids and/or IVIG without relapse. Conceptually, they are beneficial in antibody-negative disease where the role of antibodies vs cellular immunity is less clear. We preferentially utilize MMF based on its apparent efficacy over AZA in primary CNS vasculitis [47]. However, in patients who have been unable to tolerate MMF, we have seen good response to AZA as well, with both enabling a taper off IVIG and steroids. Additionally, we have used these agents in patients who respond well to rituximab, but have early B cell repopulation, as a strategy to provide added coverage.
Tocilizumab
There are also several novel medications for the treatment of refractory AE. Interleukin-6 (IL-6) is a pro-inflammatory cytokine with pleotrophic effects on a broad range of cells including neutrophils, T cells, B cells, and plasma cells [48]. IL-6 is a key mediator in plasmablast and plasma cell survival. Plasmablasts produce high levels of IL-6, which is essential for inducing follicular T helper cells. These in turn are essential for production of long-lived plasma cells. IL-6 is therefore a key cytokine for the differentiation and survival of plasma cells [49]. Tocilizumab, an IL-6 inhibitor, was found to be effective for the treatment of refractory neuromyelitis optica spectrum disorder (NMOSD), and a trial is in progress [50,51,52]. A retrospective cohort study in patients meeting criteria for probable AE who failed to respond to first-line therapy plus at least 4 weeks of rituximab compared treatment with tocilizumab (8 mg/kg IV monthly) vs repeat rituximab dosing vs no additional treatment. At all time points, the tocilizumab group had significantly more patients with a mRS of ≤ 2 than the other two groups. By month 2 of tocilizumab treatment, 60% of patients had a mRS of ≤ 2, which was similar to the last follow-up time point in the tocilizumab group and significantly improved compared to the rituximab group at 2 months (19.4%) and last follow-up (22%) [53]. We have seen remarkable responses in three children with prolonged disease refractory to steroids, IVIG, rituximab, and anti-metabolites, and promising results in two others after 1 month. Tocilizumab has been shown to be well tolerated in children, though adverse effects include infusion reactions, infections, neutropenia, transaminitis, and gastrointestinal perforations. Monitoring of cell counts, liver enzymes, and lipids is important to prevent toxicity.
Bortezomib
The ubiquitin-proteasome system is important for maintenance of cellular homeostasis by controlling intracellular protein degradation. Proteasome inhibitors have a broad range of effects on many cells in the immune system but are particularly potent against plasma cells [54]. Several proteasome inhibitors are approved, but to date, only bortezomib has been used to treat AE refractory to first- and second-line therapy. Two case reports have demonstrated improvements with bortezomib in patients with severe NMDA encephalitis [55, 56]. A separate case series of five patients with NMDA encephalitis treated with between one and six doses of bortezomib demonstrated responses from mild improvement in neurocognitive deficits to complete clinical remission. A partial list of the adverse effects of bortezomib includes infections, gastrointestinal intolerance, peripheral neuropathies, and cytopenias [57].
Interleukin-2
Low doses of interleukin-2 (IL-2) preferentially activate T regulatory cells whereas high doses preferentially activate CD8+ effector T cells [58]. There is growing interest in using low-dose IL-2 to treat a wide range of autoimmune diseases including AE [59,60,61]. Ten patients were treated with low-dose IL-2 due to treatment-refractory AE [62]. After four treatment cycles, symptoms improved in 60% and no patients worsened. Adverse effects included eosinophilia, subclinical hyperthyroidism, neutropenia, GI intolerance, and flu-like symptoms [62].
Adjunct therapy
In addition to immunotherapy, ongoing symptomatic treatment with anti-epileptic drugs (AEDs) and psychiatric medications are often necessary to maximize functionality and minimize suffering. Benzodiazepines, often at high doses, are frequently used early in the course of disease for agitation, seizures, and catatonia. Catatonia is a prominent feature in many children with AE and differentiating it from psychosis and avoiding antipsychotic medications in those cases can avoid precipitating neuroleptic malignant syndrome [1, 63, 64]. In our experience, with careful assessment to differentiate catatonia from psychosis, anti-psychotics can be used safely and effectively to manage psychosis in AE patients, especially once immunotherapy has been initiated [65]. Recovery is often protracted and adjusting to both transient and permanent deficits can be challenging. Being proactive with physical, occupational, and speech therapy along with mental health services can greatly improve patient outcomes and re-entry into their communities.
Conclusion
There is growing evidence to support first- and second-line therapies for AE but prospective, randomized, placebo-controlled studies are lacking. Corticosteroids, IVIG, and plasma exchange are considered first-line therapies. If there is no improvement within 10–14 days of first-line therapy initiation, escalation to a second-line therapy of rituximab or CYC should not be delayed. First-line therapy should be continued when escalating to a second-line therapy. Current practice for pediatric patients shows a preference for rituximab over CYC due to a better side effect profile. There is growing evidence for novel agents including tocilizumab and bortezomib for treatment-refractory disease.
References and Recommended Reading
Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 2008;7:1091–8.
Titulaer MJ, McCracken L, Gabilondo I, Armangue T, Glaser C, Iizuka T, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 2013;12:157–65.
Armangue T, Titulaer MJ, Málaga I, Bataller L, Gabilondo I, Graus F, et al. Pediatric anti-N-methyl-D-aspartate receptor encephalitis-clinical analysis and novel findings in a series of 20 patients. J Pediatr. 2013;162:850–2.
Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15:391–404.
Armangue T, Leypoldt F, Málaga I, Raspall-Chaure M, Marti I, Nichter C, et al. Herpes simplex virus encephalitis is a trigger of brain autoimmunity. Ann Neurol. 2014;75:317–23.
Bien CG, Vincent A, Barnett MH, Becker AJ, Blumcke I, Graus F, et al. Immunopathology of autoantibody-associated encephalitides: clues for pathogenesis. Brain. 2012;135:1622–38.
Hughes EG, Peng X, Gleichman AJ, Lai M, Zhou L, Tsou R, et al. Cellular and synaptic mechanisms of anti-NMDA receptor encephalitis. J Neurosci. Society for Neuroscience. 2010;30:5866–75.
Dale RC, Brilot F, Duffy LV, Twilt M, Waldman AT, Narula S, et al. Utility and safety of rituximab in pediatric autoimmune and inflammatory CNS disease. Neurology. 2014;83:142–50.
Byrne S, Walsh C, Hacohen Y, Muscal E, Jankovic J, Stocco A, et al. Earlier treatment of NMDAR antibody encephalitis in children results in a better outcome. Neurol Neuroimmunol Neuroinflamm. 2015;2:e130.
Gastaldi M, Thouin A, Vincent A. Antibody-Mediated Autoimmune Encephalopathies and Immunotherapies. Neurotherapeutics. 2016;13:147–62.
Barbagallo M, Vitaliti G, Pavone P, Romano C, Lubrano R, Falsaperla R. Pediatric Autoimmune Encephalitis. J Pediatr Neurosci. 2017;12:130–4.
Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011;10:63–74.
Bartolini L, Muscal E. Differences in treatment of anti-NMDA receptor encephalitis: results of a worldwide survey. J Neurol. 2017;264:647–53.
Hacohen Y, Wright S, Waters P, Agrawal S, Carr L, Cross H, et al. Pediatric autoimmune encephalopathies: clinical features, laboratory investigations and outcomes in patients with or without antibodies to known central nervous system autoantigens. J Neurol Neurosurg Psychiatr. 2013;84:748–55.
Brenton JN, Kim J, Schwartz RH. Approach to the Management of Pediatric-Onset Anti- N-Methyl- d-Aspartate (Anti-NMDA) Receptor Encephalitis. J Child Neurol. 2016;31:1150–5.
Dale RC, Gorman MP, Lim M. Autoimmune encephalitis in children: clinical phenomenology, therapeutics, and emerging challenges. Curr Opin Neurol. 2017;30:334–44.
Lancaster E, Lai M, Peng X, Hughes E, Constantinescu R, Raizer J, et al. Antibodies to the GABA(B) receptor in limbic encephalitis with seizures: case series and characterization of the antigen. Lancet Neurol. 2010;9:67–76.
Wingfield T, McHugh C, Vas A, Richardson A, Wilkins E, Bonington A, et al. Autoimmune encephalitis: a case series and comprehensive review of the literature. QJM. 2011;104:921–31.
Toledano M, Britton JW, McKeon A, Shin C, Lennon VA, Quek AML, et al. Utility of an immunotherapy trial in evaluating patients with presumed autoimmune epilepsy. Neurology Lippincott Williams Wilkins. 2014;82:1578–86.
Goldberg EM, Titulaer M, de Blank PM, Sievert A, Ryan N. Anti-N-methyl-D-aspartate receptor-mediated encephalitis in infants and toddlers: case report and review of the literature. Pediatr Neurol. 2014;50:181–4.
Sinha A, Bagga A. Pulse steroid therapy. Indian J Pediatr. 2008;75:1057–66.
Maddur MS, Lacroix-Desmazes S, Bayry J, Kaveri SV. Intravenous polyclonal immunoglobulin in autoimmune diseases: clinical indications and mechanisms of action. Drug Discovery Today Therapeutic Strategies. 2009;6:5–11.
Hughes RAC, Dalakas MC, Cornblath DR, Latov N, Weksler ME, Relkin N. Clinical applications of intravenous immunoglobulins in neurology. Clin Exp Immunol. 2009;158(Suppl 1):34–42.
Byrne S, McCoy B, Lynch B, Webb D, King MD. Does early treatment improve outcomes in N-methyl- d-aspartate receptor encephalitis? Dev Med Child Neurol. 2014;56:794–6.
Iro MA, Sadarangani M, Absoud M, Chong WK, Clark CA, Easton A, et al. ImmunoglobuliN in the Treatment of Encephalitis (IgNiTE): protocol for a multicentre randomized controlled trial. BMJ Open. British Medical Journal Publishing Group. 2016;6:e012356.
De Sena AD, Noland DK, Matevosyan K, King K, Phillips L, Qureshi SS, et al. Intravenous methylprednisolone versus therapeutic plasma exchange for treatment of anti-N-methyl-D-aspartate receptor antibody encephalitis: A retrospective review. J Clin Apher. 2015;30:212–6.
Heine J, Ly L-T, Lieker I, Slowinski T, Finke C, Prüss H, et al. Immunoadsorption or plasma exchange in the treatment of autoimmune encephalitis: a pilot study. J Neurol. 2016;263:2395–402.
Puisset F, White-Koning M, Kamar N, Huart A, Haberer F, Blasco H, et al. Population pharmacokinetics of rituximab with or without plasmapheresis in kidney patients with antibody-mediated disease. Br J Clin Pharmacol. 2013;76:734–40.
Sartori S, Nosadini M, Cesaroni E, Falsaperla R, Capovilla G, Beccaria F, et al. Pediatric anti-N-methyl-D-aspartate receptor encephalitis: The first Italian multicenter case series. Eur J Paediatr Neurol. 2015;19:453–63.
Huang H, Benoist C, Mathis D. Rituximab specifically depletes short-lived autoreactive plasma cells in a mouse model of inflammatory arthritis. Proc Natl Acad Sci. 2010;107:4658–63.
Nutt SL, Hodgkin PD, Tarlinton DM, Corcoran LM. The generation of antibody-secreting plasma cells. Nat Rev Immunol. 2015;15:160–71.
Hachiya Y, Uruha A, Kasai-Yoshida E, Shimoda K, Satoh-Shirai I, Kumada S, et al. Rituximab ameliorates anti-N-methyl-D-aspartate receptor encephalitis by removal of short-lived plasmablasts. J Neuroimmunol. 2013;265:128–30.
Bar-Or A, Fawaz L, Fan B, Darlington PJ, Rieger A, Ghorayeb C, et al. Abnormal B-cell cytokine responses a trigger of T-cell-mediated disease in MS? Ann Neurol. Wiley Subscription Services, Inc., A Wiley Company. 2010;67:452–61.
Goenka A, Jain V, Nariai H, Spiro A, Steinschneider M. Extended Clinical Spectrum of Anti-N-Methyl-d-Aspartate Receptor Encephalitis in Children: A Case Series. Pediatr Neurol. 2017;72:51–5.
Wang Y, Zhang W, Yin J, Lu Q, Yin F, He F, et al. Anti-N-methyl-d-aspartate receptor encephalitis in children of Central South China: Clinical features, treatment, influencing factors, and outcomes. J Neuroimmunol. 2017;312:59–65.
Zekeridou A, Karantoni E, Viaccoz A, Ducray F, Gitiaux C, Villega F, et al. Treatment and outcome of children and adolescents with N-methyl-D-aspartate receptor encephalitis. J Neurol. 2015;262:1859–66.
Wang B-J, Wang C-J, Zeng Z-L, Yang Y, Guo S-G. Lower dosages of rituximab used successfully in the treatment of anti-NMDA receptor encephalitis without tumor. J Neurolog Sci. 2017;377:127–32.
Leandro MJ. B-cell subpopulations in humans and their differential susceptibility to depletion with anti-CD20 monoclonal antibodies. Arthritis Res Ther BioMed Central. 2013;15(Suppl 1):S3.
Strippel C, Mönig C, Golombeck KS, Dik A, Bönte K, Kovac S, et al. Treating refractory post-herpetic anti-N-methyl-d-aspartate receptor encephalitis with rituximab. Oxf Med Case Rep. 2017;2017:omx034.
Emadi A, Jones RJ, Brodsky RA. Cyclophosphamide and cancer: golden anniversary. Nat Rev Clin Oncol Nature Publishing Group. 2009;6:638–47.
Brenner GM, PhD CWS. Pharamcology. Pharmacology. 4th edn. Philadelphia; pp 462–79.
Kim YH, Choi BK, Oh HS, Kang WJ, Mittler RS, Kwon BS. Mechanisms involved in synergistic anticancer effects of anti-4-1BB and cyclophosphamide therapy. Mol Cancer Ther. American Association for Cancer Research. 2009;8:469–78.
Kanter IC, Huttner HB, Staykov D, Biermann T, Struffert T, Kerling F, et al. Cyclophosphamide for anti-GAD antibody-positive refractory status epilepticus. Epilepsia. 2008;49:914–20.
Sansing LH, Tüzün E, Ko MW, Baccon J, Lynch DR, Dalmau J. A patient with encephalitis associated with NMDA receptor antibodies. Nat Clin Pract NeurolNature Publishing Group. 2007;3:291–6.
Suleiman J, Dale RC. The recognition and treatment of autoimmune epilepsy in children. Dev Med Child Neurol. 2014;n/a–n/a.
Salvucci A, Devine IM, Hammond D, Sheth RD. Pediatric anti-NMDA (N-methyl D-aspartate) receptor encephalitis. Pediatr Neurol. 2014;50:507–10.
Hutchinson C, Elbers J, Halliday W, Branson H, Laughlin S, Armstrong D, et al. Treatment of small vessel primary CNS vasculitis in children: an open-label cohort study. Lancet Neurol. Elsevier Ltd. 2010;9:1078–84.
Kishimoto T. IL-6: from its discovery to clinical applications. INTIMM. 2010;22:347–52.
Chavele K-M, Merry E, Ehrenstein MR. Cutting edge: circulating plasmablasts induce the differentiation of human T follicular helper cells via IL-6 production. J Immunol American Association of Immunologists. 2015;194:2482–5.
Lauenstein A-S, Stettner M, Kieseier BC, Lensch E. Treating neuromyelitis optica with the interleukin-6 receptor antagonist tocilizumab. Case Rep. BMJ Publishing Group Ltd. 2014;2014:bcr2013202939.
Marino A, Narula S, Lerman MA. First Pediatric Patient With Neuromyelitis Optica and Sjögren Syndrome Successfully Treated With Tocilizumab. Pediatr Neurol. 2017;73:e5–6.
Araki M, Aranami T, Matsuoka T, Nakamura M, Miyake S, Yamamura T. Clinical improvement in a patient with neuromyelitis optica following therapy with the anti-IL-6 receptor monoclonal antibody tocilizumab. Mod Rheumatol Taylor & Francis. 2013;23:827–31.
Lee W-J, Lee S-T, Moon J, Sunwoo J-S, Byun J-I, Lim J-A, et al. Tocilizumab in Autoimmune Encephalitis Refractory to Rituximab: An Institutional Cohort Study. Neurotherapeutics. 2016;13:1–9.
Verbrugge SE, Scheper RJ, Lems WF, de Gruijl TD, Jansen G. Proteasome inhibitors as experimental therapeutics of autoimmune diseases. Arthritis Res Ther. BioMed Central. 2015;17:17.
Titulaer MJ, Kayser MS, Dalmau J. Authors’ reply. Lancet Neurol. 2013;12:425–6.
Sveinsson O, Granqvist M, Forslin Y, Blennow K, Zetterberg H, Piehl F. Successful combined targeting of B- and plasma cells in treatment refractory anti-NMDAR encephalitis. J Neuroimmunol. 2017;312:15–8.
Scheibe F, Prüss H, Mengel AM, Kohler S, Nümann A, Köhnlein M, et al. Bortezomib for treatment of therapy-refractory anti-NMDA receptor encephalitis. Neurology. 2017;88:366–70.
Arenas-Ramirez N, Woytschak J, Boyman O. Interleukin-2: Biology, Design and Application. Trends Immunol. Elsevier Ltd. 2015;36:1–16.
Hartemann A, Bensimon G, Payan CA, Jacqueminet S, Bourron O, Nicolas N, et al. Low-dose interleukin 2 in patients with type 1 diabetes: a phase 1/2 randomized, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2013;1:295–305.
He J, Zhang X, Wei Y, Sun X, Chen Y, Deng J, et al. Low-dose interleukin-2 treatment selectively modulates CD4(+) T cell subsets in patients with systemic lupus erythematosus. Nat Med. 2016;22:991–3.
von Spee-Mayer C, Siegert E, Abdirama D, Rose A, Klaus A, Alexander T, et al. Low-dose interleukin-2 selectively corrects regulatory T cell defects in patients with systemic lupus erythematosus. Ann Rheum Dis. 2016;75:1407–15.
Lim J-A, Lee S-T, Moon J, Jun J-S, Park B-S, Byun J-I, et al. New feasible treatment for refractory autoimmune encephalitis: Low-dose interleukin-2. J Neuroimmunol. 2016;299:107–11.
Sienaert P, Dhossche DM, Vancampfort D, De Hert M, Gazdag G. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
Gulyayeva NA, Massie MJ, Duhamel KN. Anti-NMDA receptor encephalitis: psychiatric presentation and diagnostic challenges from psychosomatic medicine perspective. Palliat Support Care. vCambridge University Press. 2014;12:159–63.
Mooneyham GC, Gallentine W, Van Mater H. Evaluation and Management of Autoimmune Encephalitis: A Clinical Overview for the Practicing Child Psychiatrist. Child Adolesc Psychiatr Clin N Am. 2018;27:37–52.
Funding
NIH T32 Training Grant: National Human Genome Research Institute/Genomic Medicine (Grant 1T32HG008955-01).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Cory Stingl declares that he has no conflict of interest. Kathleen Cardinale declares that she has no conflict of interest. Heather Van Mater declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatric Rheumatology
Rights and permissions
About this article
Cite this article
Stingl, C., Cardinale, K. & Van Mater, H. An Update on the Treatment of Pediatric Autoimmune Encephalitis. Curr Treat Options in Rheum 4, 14–28 (2018). https://doi.org/10.1007/s40674-018-0089-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40674-018-0089-z