Abstract
This longitudinal study aimed to assess the factors associated with motivation in 303 Brazilian medical students after a 30-month follow-up. Their demographics, study habits, sleep quality, motivation (Brazilian version of the Academic Motivation Scale-BAMS), learning approaches (R-SPQ-2F scale), and stressors (MSSF-Medical Student Stress Factor scale) were examined. We found an increase in amotivation and extrinsic motivation through external regulation (e.g., “I come to school to earn a degree”) and a decrease in intrinsic motivation and extrinsic motivation through integrated regulation (e.g., “because studying broadens our horizons”) in medical students after the 30-month follow-up. Students in earlier stages of medical training showed greater increases in amotivation. Factors such as the learning approach, hours spent studying, sex, stressors, studying just before examinations, and sleep problems were predictors of the different dimensions of motivation. Medical students’ motivation changed negatively as medical training progressed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ongoing search for an effective teaching–learning process in medical schools has led to the need to better understand student motivation as a major determinant of behavior and academic performance [1].
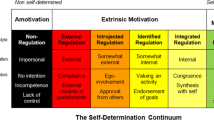
Many aspects that can be developed during medical training (e.g., autonomy, competence, relationship, and performance) as well as non-modifiable factors (e.g., age, sex, and ethnicity) seem to affect medical students’ motivation [2]. In the search for a motivation framework, several learning theories such as behaviorism, cognitivism, and humanism have been proposed. However, the Self-Determination Theory (SDT) remains one of the most recognized theories because of its important educational and clinical implications. This theory highlights that a person’s motivation is a function not only of their immediate social context but also of their inner resources that have developed over time [3], assuming that all students have inherent growth tendencies (curiosity, motivation, and psychological needs) that promote motivation for classroom engagement and functioning [4]. Based on this theory, social environments can either facilitate or disrupt this process, and individuals differ in the intensity of and the reasons underlying their motivation [3].
In the past few decades, several authors have used SDT to understand the complex construct of motivation. This theory is grounded in an established continuum starting from amotivation, followed by a steady increase in extrinsic forms of motivation (e.g., introjected regulation, integrated regulation) and, finally, the attainment of intrinsic motivation [5]. These different types of motivation are influenced by the ways in which individuals manage their drive and whether they are more dependent on external or intrinsic factors to achieve personal satisfaction. These regulatory processes play a pivotal role in motivation [3, 4]. Based on this framework, the Academic Motivation Scale (AMS) was developed to evaluate motivation according to the precepts of SDT and has become one of the most widely used instruments to assess motivation in medical education [6].
In the scientific literature, authors have identified several factors associated with motivation in medical students, namely, grade expectations, level of interest in the content, having a good quality of life, future examinations, and sex differences [7]. Likewise, decreases in motivation are associated with different outcomes such as professional commitment [8], family relationships [9], and academic achievement [10]. In this context, motivation is a multidimensional construct, involving issues related to the individual and their social situation and educational aspects [11]. Therefore, students’ learning approach and stressors should be considered to understand motivation throughout the duration of a medical degree course.
Learning approaches, according to Biggs, are distinguishable by the type of motivation and strategy used by the student, whether deep or surface [12]. In the deep approach, students are really interested in learning about the topic, reading and integrating new information with their previous knowledge. In contrast, in the surface approach, students tend to choose the quickest way to accomplish the task, studying the material in a linear manner and prioritizing memory over comprehension. Approaches can differ for the same student according to the workload, topics, and learning environment [13, 14].
Motivational factors associated with an individual include stress, which constitutes a major mental health problem among medical students [15]. Stress can be associated with numerous factors, such as an unsuitable learning environment [16], high workload [17,18,19], lack of time [18], competition among colleagues [17, 19], financial concerns [17,18,19], health issues [19], and peer/faculty relationships [17]. According to the SDT, pressures can trigger regulatory processes that induce more controlled motivations. Investigating stressors is therefore important in motivation studies.
Although the scientific literature on motivation has made significant strides in the recent decades, demonstrating that motivation is associated with differences in study behavior and student performance [1, 20, 21], few studies have investigated motivational changes throughout the medical school curriculum. Most of the studies available are cross-sectional [22], precluding the analysis of cause–effect relationships. Longitudinal studies in the literature are scarce, with those available involving short follow-ups and limited samples [23, 24].
Longitudinal studies allow the changes in student motivation throughout medical training to be mapped and the associated factors elucidated. This evidence can help raise the awareness of managers and educators about their students and help them redesign curricula, instruction, methods, strategies, resources, culture, learning environment, and climate toward a more effective educational process. To bridge the gap in the literature regarding such evidence, this study aimed to assess the factors associated with motivation in Brazilian medical students after a 30-month follow-up.
Methods
Study Design
A longitudinal, observational 30-month follow-up study was conducted for medical students from a Brazilian public university. The project was approved by the University Teaching Hospital/UFJF’s Research Ethics Committee under Permit No. 2.742.787. All study participants signed a consent form.
Study Participants and Venue
This study was conducted at the School of Medicine of the Federal University of Juiz de Fora. The institution has a traditional curriculum incorporating active strategies such as problem-based learning, flipped classroom, and team-based learning. A total of 80–90 students are enrolled per semester in each class. The duration of the program is 6 years, and the curriculum is divided into three stages of training: preclinical (first and second years—studying most of the basic sciences: anatomy, histology, and physiology; with almost exclusively classroom-based activities and little patient exposure); clinical (third and fourth years—studying disciplines such as cardiology, gastroenterology, and surgery; involving mostly classroom activities but with increasing patient exposure); and clerkship (fifth and sixth years—mostly inpatient or outpatient care and few classroom activities).
For this study, we invited all students enrolled in the first to fourth years of medical school who were present at the time of data collection to participate; approximately 640 medical students were invited. The students who agreed to participate in the survey answered the questionnaire at two different times (waves): at the baseline (first semester, 2016) and after 30 months of follow-up (second semester, 2018). Only those students who answered in the first wave were included in the second wave (that is, the original first-year medical students were in their third year).
Eligibility Criteria
All students who were followed up with for the entirety of 30 months, who were present at the time of data collection, and who agreed voluntarily to participate in the study were included. We excluded students who failed to fill out the questionnaires for the two waves (that is, those concluding their medical degree before the study’s endpoint, those admitted to the university after the first wave, or those who had not completed the questionnaire for one or both waves).
Instruments
We used a self-report, in-person questionnaire as follows: (All instruments used in this questionnaire are freely available to be used for research purposes with appropriate citation).
-
Sociodemographic data: sex, ethnicity, age, and family income;
-
Studying patterns: The following two questions were used: “How many hours per week do you dedicate to your studies (outside classroom activities)?” (six response options, ranging from 1–2 h to > 10 h); and “How often do you leave studying the material until just before examinations?” (five response options, ranging from never to always);
-
Sleep quality: “Over the past month, how would you rate the overall quality of your sleep?” (four response options, ranging from very good to very poor);
-
Motivation: Motivation was measured using the Brazilian Adapted version of the Academic Motivation Scale (BAMS) [25]. The original AMS was devised by Vallerand et al. [6] and is used to evaluate students’ motivation toward learning using 28 items. This scale was subsequently translated, validated, and adapted for use in Brazilian Portuguese after expert meetings and factorial analyses [25,26,27]. The final Brazilian Portuguese version comprised 30 items [25] scored on Likert scales similar to the original AMS, ranging from 1 to 7 (1 = does not correspond at all, 2–3 = corresponds a little, 4 = corresponds moderately, 5–6 = corresponds a lot, and 7 = corresponds exactly). The scale is divided into seven subscales:
-
(a)
Amotivation—6 items (e.g., “Honestly, I don’t know why I come to school,” “I don’t see why I should come to school”);
-
(b)
Intrinsic motivation—3 items (e.g., “because coming to the university is a pleasure for me,” “because I really like going to school”);
-
(c)
Extrinsic motivation through social regulations—4 items (e.g., “I come to school to get out of the house,” “to see my friends is the main reason I come to the university”);
-
(d)
Extrinsic motivation through identified regulation—2 items ( “I come because attending classes is necessary for learning,” “because I think that requiring attendance is needed so that students will take the medical training seriously”);
-
(e)
Extrinsic motivation through integrated regulation—4 items (e.g., “because education is a privilege,” “because studying broadens our horizons”);
-
(f)
Extrinsic motivation through introjected regulation—6 items (e.g., “I come because it is what’s expected of me,” “to show myself that I am an intelligent person”); and
-
(g)
Extrinsic motivation through external regulation—5 items (e.g., “I come to school to not get marked absent,” “I come to school to earn a degree”).
-
Surface and deep learning approaches: We used the R-SPQ-2F questionnaire developed by Biggs et al. [12] because learning approaches are key to the framework of motivation, as described in the “Introduction” section, and the R-SPQ-2F is one of the most widely used evidence-based instruments for assessing it. This instrument comprises two scales (the deep approach and surface approach, respectively) containing 10 items scored on a Likert scale (5 items from never to always or almost always). Each scale has two subscales with five questions, comprising two on motivation and two on strategy: deep motivation, surface motivation, deep strategy, and surface strategy;
-
Stress factors of medical students were measured using the Medical Students Stress Factor (MSSF) scale. This scale was chosen because it includes the most important stressors available in this context, as the validation of this instrument was conducted at our medical school [28]. This instrument rates the most common stressors experienced by medical students for 28 situations on a scale from 1 (not at all) to 7 (extremely distressing). It evaluates five different domains [28]: “Learning environment and academic performance” (e.g., grades, attaining lower academic grades than peers, examinations and evaluations, fear of failing any discipline, extensive learning content, lack of time to study, family pressure); “Relationship” (e.g., family relationships, faculty relationships); “Health” (e.g., physical health, mental health); “Lack of time” (e.g., lack of leisure time, lack of time with friends and family); and “Learning issues” (e.g., inability to answer patients’ questions, difficulty in understanding the entire content) [28].
Procedures
Students completed the questionnaires during class time (before or after educational activities). Scale application took approximately 20 min and was done exclusively by the researchers to guarantee data confidentiality.
Statistical Analyses
Descriptive statistics were expressed in terms of absolute and relative frequencies for categorical variables and mean and standard deviation for continuous measures.
Inferential analyses were performed for the total sample and the following subgroups based on the stage of medical training: first/second years and third/fourth years. The main reason for using such an approach is that the medical school curriculum was fragmented and had distinct stages: preclinical (first/second years), clinical (third/fourth years), and clerkship (fifth/sixth years). Therefore, separating students into these blocks allowed us to understand how students made such transitions throughout the course (i.e., from the preclinical to clinical stages and from the clinical to clerkship stages).
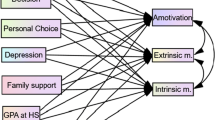
The different motivational dimensions were compared—using the AMS at baseline (2016) and after the 30-month follow-up—through pre–post two-tailed paired t-tests. Stepwise linear regression models (0.05 for entry and 0.15 for removal) were then developed with the baseline variables as independent variables (i.e., age, sex, family income, medical training stage, whether one has previously been enrolled in another undergraduate program, Biggs’ surface approach, Biggs’ deep approach, hours per week dedicated to studies (outside classroom activities), studying the material just before examinations, sleep quality, and stress factors associated with medical students, such as “Learning environment and academic performance,” “Relationship,” “Health,” “Lack of time,” and “Learning issues”); the motivation scale and subscale scores after the 30-month follow-up were the dependent variables. All assumptions for conducting linear regression were satisfied.
A p-value of ≤ 0.05 was considered statistically significant, and all statistical analyses were performed using SPSS version 20.
Results
Of the 523 eligible students, 303 (57.9%) completed both questionnaires at baseline and the 30-month follow-up and were subsequently included in the study. The sample comprised 167 (55.1%) women, 202 (66.7%) White participants, 191 (63.2%) participants with a family income ≤ 10 Brazilian minimum wage, and 58 (19.1%) participants who had attended other undergraduate programs prior to studying medicine. Regarding the medical training stage, 194 (64.0%) students were in the first or second years and 109 (36.0%) in the third or fourth years. The mean age of the sample was 20.58 (SD: 2.48) years.
Mean baseline scores on the R-SPQ-2F scale were 29.71 (SD: 6.33) for the “Deep Approach” and 22.14 (SD: 6.26) for the “Surface Approach.” Scores on the Medical Students Stress Factor (MSSF) scale were 5.22 (SD: 1.20) for the dimension “Learning Environment and Academic Performance,” 2.81 (SD: 1.18) for the dimension “Relationship,” 4.22 (SD: 1.45) for the dimension “Health,” 5.23 (SD: 1.30) for the dimension “Lack of Time,” and 4.33 (SD: 1.30) for the dimension “Learning issues.” A total of 203 students (67.0%) dedicated > 6 h per week of home study (outside classroom activities), and 114 (37.6%) reported always or often studying just before the exam.
The different components of motivation measured at baseline and after the 30-month follow-up are given in Table 1. For the total sample, the results show an increase in amotivation (p < 0.001) and extrinsic motivation through external regulation (p < 0.001) and a decrease in intrinsic motivation (p < 0.001) and extrinsic motivation through integrated regulation (p = 0.001). Stratifying by the medical training stage, greater changes in motivation are evident among first- and second-year students than among third- and fourth-year students.
Factors at baseline associated with the subdimensions of motivation after the 30-month follow-up are given in Table 2. The factors are associated as follows: (a) amotivation: greater level of the surface approach; (b) intrinsic motivation: greater level of the deep approach; (c) extrinsic motivation through social regulations: lower level of the deep approach and greater stress associated with the relationship dimension; (d) extrinsic motivation through identified regulation: male sex; (e) extrinsic motivation through integrated regulation: lower level of the surface approach, greater stress associated with health, and greater level of the deep approach; (f) extrinsic motivation through introjected regulation: greater stress associated with the learning environment and relationship dimension; and (g) extrinsic motivation through external regulation: greater level of the surface approach and higher age.
Table 3 shows the factors at baseline associated with the motivation subdimensions after the 30-month follow-up according to the medical training stage. The following associations were identified among first- and second-year students (Table 3): (a) amotivation: fewer studying hours and worse sleep quality; (b) intrinsic motivation: greater level of the deep approach; (c) extrinsic motivation through social regulations: lower level of the deep approach; (d) extrinsic motivation through identified regulation: male sex; (e) extrinsic motivation through integrated regulation: lower stress associated with Learning issues and greater level of the deep approach; (f) extrinsic motivation through introjected regulation: greater stress associated with the learning environment; and (g) extrinsic motivation through external regulation: greater level of the surface approach and higher age.
The associations for third- and fourth-year students (Table 3) were as follows: (a) amotivation: greater stress associated with the learning environment and greater level of the surface approach; (b) intrinsic motivation: greater level of the deep approach and less study just before examinations; (c) extrinsic motivation through social regulations: greater stress associated with the relationship dimension, fewer studying hours, and lower income; (d) extrinsic motivation through identified regulation: male sex; (e) extrinsic motivation through integrated regulation: lower level of the surface approach, lower stress associated with Learning issues, lower stress associated with the relationship dimension, and greater stress associated with the learning environment; (f) extrinsic motivation through introjected regulation: greater stress associated with the learning environment; and (g) extrinsic motivation through external regulation: greater level of the surface approach and lower income.
Discussion
This study revealed an increase in medical students’ amotivation (9.44 to 11.02, p < 0.001) and extrinsic motivation through external regulation (e.g., “I come to school to earn a degree”; 16.50 to 19.47, p < 0.001) and a decrease in their intrinsic motivation (12.45 to 11.38, p < 0.001) and extrinsic motivation through integrated regulation (e.g., “because studying broadens our horizons”; 21.62 to 20.47, p = 0.001) during a 30-month follow-up in the course of their medical degree. Students in earlier stages of medical training showed a greater increase in amotivation. Factors such as the learning approach, hours spent studying, sex, stressors, studying just before examinations, and sleep problems were predictors of the different dimensions of motivation after the 30-month follow-up.
These results are similar to the findings of a previous longitudinal study by Del-Ben et al. [23] that showed a reduction in intrinsic motivation among a medical school’s first-year medical students who were followed up with for 1 year [23]. Another study by the same authors comparing students’ motivation for two different curricula found that students exposed to a reformed curriculum (i.e., content reduction, fostering of interdisciplinary integration, and early contact with clinical activities) exhibited no loss of motivation in the sixth year relative to the first year of medical training. By contrast, students who followed the traditional curriculum showed a significant decrease in motivation [24].
Although these longitudinal studies reported valuable results, they included a relatively low number of students (fewer than 100 participants) and failed to assess the potential predictors of amotivation.
Our findings seem to be supported, at least partially, by the SDT, which holds that motivation depends on the innate psychological needs for three factors: competence, autonomy, and relatedness. Based on this, individual factors or those connected with the socioeducational context facilitate motivations that are less driven by secondary gains [1].
Medical school curriculum workload is a major factor contributing to students’ perceived difficulties, particularly among freshmen, for whom the educational transition from secondary school to medical school is challenging [21]. The traditional, discipline-based curriculum adopted in the medical school in this study with few active learning methods—that is, not student-centric—may contribute to an educational setting that promotes amotivation as the course progresses.
The analysis of the two groups by training stage showed that the first- and second-year students had worse outcomes after 30 months compared to the third- and fourth-year students, exhibiting increased amotivation (“I don’t see why I should come to school”) and extrinsic motivation through external regulation (“I come to school to not get marked absent”), in addition to decreased intrinsic motivation (“because coming to the university is a pleasure for me”) and extrinsic motivation through integrated regulation (“because studying broadens our horizons”). This finding is attributable to the fact that first- and second-year students are more exposed to new interactions and must manage larger academic workloads and high-stress academic situations with greater exposure to assessments, competition for grades, and first direct contact with patients [29].
Conversely, students in the third and fourth years at baseline exhibited only increased extrinsic motivation through external regulation (e.g., “I come to school to earn a degree”) after the 30-month follow-up. This may be because this group of mature students had had more time to adapt to the group and new stimuli, promoting the maintenance of these forms of internalization and leading to less change in motivation [1]. In addition, after the 30-month follow-up, these students had achieved clerkship, which was accompanied by a strong desire to complete their medical training, possibly explaining the higher scores for extrinsic motivation through external regulation.
In addition to the changes in motivation investigated by the present study, the potential predictors of motivation over time were assessed. Of the factors associated with motivation, the main predictors were learning approaches. The surface approach was more associated with amotivation (Std. beta = 0.242, p < 0.001), whereas the deep approach proved to be more associated with intrinsic motivation (Std. beta = 0.258, p < 0.001). These findings were expected because previous studies have shown that upon experiencing curriculum overload, students tend to develop surface approaches to learning [30]. Having failed to develop more self-regulated learning, these students experience less adaptation and lower motivation [31,32,33].
With regard to stressors, the learning environment was associated with greater extrinsic motivation through introjected regulation (“I come because it is what’s expected of me”) for the total sample (Std. beta = 0.279, p < 0.001) and for both first- and second-year students (Std. beta = 0.353, p < 0.001) and third- and fourth-year students (Std. beta = 0.280, p = 0.004). Owing to some degree of internalization of the reasons for learning in introjected regulation (“to show myself that I am an intelligent person”) coupled with a strong component of obligation or pressure [34], this finding is expected, as grades and assessments are still important motivating factors [7].
Learning issues stressors (e.g., the inability to answer patients’ questions and difficulties in understanding the entire content) were associated with lower integrated regulation (e.g., “because studying broadens our horizons”) for both first- and second-year students (Std. beta = − 0.198, p = 0.011) and third- and fourth-year students (Std. beta = − 0.233, p = 0.031). This finding is particularly meaningful, highlighting that teachers should be alert to negative educational experiences involving patients and difficulties faced by students regarding content [35].
In terms of the stressors associated with the relationship dimension, third- and fourth-year students were the most affected by these factors, resulting in amotivation (Std. beta = 0.379, p < 0.001), extrinsic motivation through social regulation (“to see my friends is the main reason I come to the university”; Std. beta = 0.309, p = 0.001), and extrinsic motivation through integrated regulation (“because studying broadens our horizons”; Std. beta = − 0.196, p = 0.040). This may be related to the fact that, upon embarking on clerkship, these students have greater responsibilities, a workload involving greater practice in clinical settings, and relationships with students assisting in medical shifts, clinical routines, and visiting rounds [21].
Other issues commonly affecting students, such as the hours spent studying [36] and sleep quality [37], also influenced motivational levels. Fewer studying hours were associated with greater extrinsic motivation through social regulation (e.g., “to see my friends is the main reason I come to the university”; Std. beta = − 0.227, p = 0.003), possibly explained by the fact that these students did not prioritize studying when attending medical school. Accordingly, spending fewer hours studying in the run-up to the examinations was associated with greater intrinsic motivation (Std. beta = − 0.239, p = 0.020), corroborating the findings of another study [38].
Worse sleep quality was also a factor associated with greater demotivation in the group of first- and second-year students (Std. beta = − 0.184, p = 0.015). Although low sleep quality and greater sleepiness have been associated with mental health problems among medical students [39], few studies explore the role of these factors in motivation. Previous studies involving other populations have shown that changes in sleep are associated with lower motivation [40, 41].
Among sociodemographic factors, the male sex was associated with lower extrinsic motivation through identified regulation (e.g., “I come because attending classes is necessary for learning”) across all analyses (Std. beta = − 0.180, p = 0.021 for the total sample). This study’s results are similar to those of another study showing that men have a greater surface approach and self-perception of competence, whereas women exhibit better competencies and are more influenced by external pressures [42]. Hence, women tend to believe that attending classes is more important for their learning.
This study has some limitations that should be considered. We note the loss of respondents in the second wave and that data were collected at one point in time and may thus reflect recent events rather than longer periods of time. However, students with lower levels of motivation likely responded less, further increasing the relevance of changes in the subdimensions of motivation. A second issue pertains to the study setting of a traditional curriculum with the introduction of active strategies, raising a question as to whether the results would differ for more student-centered curricula. Finally, we separated students according to their stages of medical training (preclinical and clinical). This approach may have included students at different moments of formation (i.e., first- and second-year students in the same group). However, as the curriculum was fragmented, preclinical students had similar educational strategies and learning environments, which made this block uniform. Therefore, investigating this transition was possible in our sample. Another option would be to separate students into four cohorts according to their year of medical school. This option was not exercised because the sample size would have been limited, resulting in an increase in type 2 errors. Despite these limitations, the present study’s strengths include the 30-month follow-up spanning all stages of medical training and the in-depth analysis of factors associated with changes in the subdimensions of motivation. The results provide a basis for the further analysis of the reasons underlying shortcomings and the factors contributing to success to help devise mechanisms that can guide and effectively influence learning–teaching processes. Future qualitative studies (i.e., using open ended questions) can provide insights to enhance comprehension of these findings.
Conclusion
The findings of this study have clinical and educational implications that warrant further discussion. The SDT is currently one of the main theories explaining motivational processes; it seeks to aid understanding on whether student motivation is more autonomous or controlled and helps predict implications for the educational setting [43, 44]. This study found different changes in the subdimensions of motivation of the SDT for different stages of medical training and predictive factors.
Knowledge of the different types of motivational states displayed by students can help educators and managers adapt their curricula accordingly. This includes the adoption of strategies promoting greater levels of motivation and extrinsic motivation through integrated regulation (e.g., “because studying broadens our horizons”). This can be achieved through educational initiatives focused on challenging, appropriate, and student-centered tasks that introduce progressive responsibility, while providing vertical integration and greater contact with patients throughout students’ medical training [44]. Our results highlight that traditional curricula should be rethought in the present medical school and other schools worldwide, motivating their students through interactive theoretical activities and early exposure to simulated and real patients.
At an individual level, strategies should help students find ways of monitoring their academic progress through feedback, coping with the high medical training workload [45], and managing their time [46]. Moreover, initiatives should identify and address the sources of students’ stress to promote more autonomous motivations, influence students’ choices while encouraging them to take responsibility for them, and instill greater reflection. Previous studies have found mindfulness/meditation, curriculum-level changes, and stress management [47, 48] to be promising interventions to mitigate students’ mental health problems in medical schools, and these should be considered by educators.
In conclusion, the study showed that medical students’ motivation changed significantly throughout the stages of medical training. Several factors predicted student motivation, which should be considered by educators and medical schools when redesigning curricula and implementing strategies for reducing amotivation and boosting students’ intrinsic motivation.
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BAMS:
-
Brazilian version of the Academic Motivation Scale-BAMS
- MSSF:
-
Medical Student Stress Factor scale
- R-SPQ-2F scale:
-
Revised Two-factor Study Process Questionnaire
- SDT:
-
Self-Determination Theory
- UFJF:
-
Federal University of Juiz de Fora, Brazil
References
Deci EL, Ryan RM. The what and why of goal pursuits: human needs and the self-determination of behavior. Psychol Inq. 2000;11(4):227–68.
Kusurkar RA, Ten Cate TJ, Van Asperen M, Croiset G. Motivation as an independent and a dependent variable in medical education: a review of the literature. Med Teach. 2011;33(5):e242–62.
Reeve J, Deci EL, Ryan RM. Self-determination theory: a dialectical framework for understanding socio-cultural influences on student motivation. Big theories revisited. 2004;4:31–60.
Reeve J. A self-determination theory perspective on student engagement. Handbook of research on student engagement. Springer 2012. p. 149–72.
Silva R, Rodrigues R, Leal C. Academic Motivation Scale: development, application and validation for Portuguese accounting and marketing undergraduate students. Int J Bus Manag. 2018;13(11):1–16.
Vallerand RJ, Pelletier LG, Blais MR, Briere NM, Senecal C, Vallieres EF. The academic motivation scale: a measure of intrinsic, extrinsic, and amotivation in education. Educ Psychol Measur. 1992;52(4):1003–17.
Sawalha K, Al Ali M, Sawalha A, Ko H, Abdelli I, El Shawish S, et al. Factors influencing academic motivation among UOS medical students. J Health Sci. 2017;5:177–80.
Ahmad Z, Anantharaman RN, Ismail H. Students’ motivation, perceived environment and professional commitment: an application of Astin’s college impact model. Acc Educ. 2012;21(2):187–208.
Islam M, Chakrabarty S. A study of the relationship between familial factors and academic motivation and achievement in high school students. Psychol Stud. 2020;65(1):87–96.
Lyndon MP, Masters T, Yu T-C, Shao R, Alyami H, Henning M, et al. Medical student motivation and well-being: a systematic review. Educ Med J. 2016;8(3):11–20.
Vallerand RJ, Blssonnette R. Intrinsic, extrinsic, and amotivational styles as predictors of behavior: a prospective study. J Pers. 1992;60(3):599–620.
Biggs J, Kember D, Leung DY. The revised two-factor Study Process Questionnaire: R-SPQ-2F. Br J Educ Psychol. 2001;71(1):133–49.
Dart BC, Clarke JA. Helping students become better learners: a case study in teacher education. High Educ. 1991;22(3):317–35.
Groves M. Problem-based learning and learning approach: is there a relationship? Adv Health Sci Educ. 2005;10(4):315.
Moutinho ILD, Lucchetti ALG, da Silva EO, Lucchetti G. Mental health and quality of life of Brazilian medical students: incidence, prevalence, and associated factors within two years of follow-up. Psychiatry Res. 2019;274:306–12.
Damiano RF, Cruz AOd, Oliveira JGd, DiLalla LF, Tackett S, Ezequiel OdS et al. Mapping scientific research on the negative aspects of the medical school learning environment. Revista da Associação Médica Brasileira. 2019;65(2):232–9.
Shim E-J, Jeon HJ, Kim H, Lee K-M, Jung D, Noh H-L, et al. Measuring stress in medical education: validation of the Korean version of the higher education stress inventory with medical students. BMC Med Educ. 2016;16(1):302.
Chang E, Eddins-Folensbee F, Coverdale J. Survey of the prevalence of burnout, stress, depression, and the use of supports by medical students at one school. Acad Psychiatry. 2012;36(3):177–82.
Hill MR, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Med Educ Online. 2018;23(1):1530558.
Brewer EW, Burgess DN. Professor’s role in motivating students to attend class. J STEM Teacher Educ. 2005;42(3):3.
Barbosa J, Silva Á, Ferreira MA, Severo M. Do reciprocal relationships between academic workload and self-regulated learning predict medical freshmen’s achievement? A longitudinal study on the educational transition from secondary school to medical school. Adv Health Sci Educ. 2018;23(4):733–48.
Shrestha L, Pant SN. Motivational profiles of medical students of Nepalese Army Institute of health sciences. J Nepal Health Res Counc. 2017;15(3):252–7.
Del-Ben CM, Machado VF, Madisson MM, Resende TL, Valério FP, Troncon LEDA. Relationship between academic performance and affective changes during the first year at medical school. Med Teach. 2013;35(5):404–10.
Del-Ben CM, Shuhama R, Costa MJ, Troncon LEdA. Effect of changes to the formal curriculum on medical students’ motivation towards learning: a prospective cohort study. Sao Paulo Med J. 2019;137(2):112–8.
Guimarães S, Bzuneck JA. Propriedades psicométricas de uma medida de avaliação da motivação intrínseca e extrínseca: um estudo exploratório. Psico-USF. 2002;7(1):1–8.
Sobral DT. Learner’s motivation in medical studies: use of the academic motivation scale. Psicologia: Teoria e Pesquisa. 2003;19(1):25–31.
Guimarães SÉR. Propriedades psicométricas de um instrumento para avaliação da motivação de universitários. Ciências & Cognição. 2008;13(1):101–13.
Damiano RF, de Oliveira IN, Ezequiel ODS, Lucchetti AL, Lucchetti G. The root of the problem: identifying major sources of stress in Brazilian medical students and developing the Medical Student Stress Factor Scale. Braz J Psychiatry. 2020;43(1):35–42.
Gomathi KG, Ahmed S, Sreedharan J. Psychological health of first-year health professional students in a medical university in the United Arab Emirates. Sultan Qaboos Univ Med J. 2012;12(2):206.
Devlin M, Gray K. In their own words: a qualitative study of the reasons Australian university students plagiarize. High Educ Res Dev. 2007;26(2):181–98.
Artino AR Jr, Dong T, DeZee KJ, Gilliland WR, Waechter DM, Cruess D, et al. Achievement goal structures and self-regulated learning: relationships and changes in medical school. Acad Med. 2012;87(10):1375–81.
Krause KL, Coates H. Students’ engagement in first-year university. Assess Eval High Educ. 2008;33(5):493–505.
Kassab SE, Al-Shafei AI, Salem AH, Otoom S. Relationships between the quality of blended learning experience, self-regulated learning, and academic achievement of medical students: a path analysis. Adv Med Educ Pract. 2015;6:27.
Deci EL, Koestner R, Ryan RM. Extrinsic rewards and intrinsic motivation in education: reconsidered once again. Rev Educ Res. 2001;71(1):1–27.
Ryan RM, Deci EL. Intrinsic and extrinsic motivations: classic definitions and new directions. Contemp Educ Psychol. 2000;25(1):54–67.
Idris A, Al Saadi T, Edris B, Sawaf B, Zakaria MI, Alkhatib M, et al. Self-reported study habits for enhancing medical students’ performance in the National Medical Unified Examination. Avicenna J Medicine. 2016;6(2):39.
Loayza HMP, Ponte TS, Carvalho CG, Pedrotti MR, Nunes PV, Souza CM, et al. Association between mental health screening by self-report questionnaire and insomnia in medical students. Arq Neuropsiquiatr. 2001;59(2A):180–5.
Bickerdike A, O’Deasmhunaigh C, O’Flynn S, O’Tuathaigh C. Learning strategies, study habits and social networking activity of undergraduate medical students. Int J Med Educ. 2016;7:230.
Pacheco JP, Giacomin HT, Tam WW, Ribeiro TB, Arab C, Bezerra IM, et al. Mental health problems among medical students in Brazil: a systematic review and meta-analysis. Brazilian Journal of Psychiatry. 2017;39(4):369–78.
Ritland BM, Simonelli G, Gentili RJ, Smith JC, He X, Oh H, et al. Sleep health and its association with performance and motivation in tactical athletes enrolled in the reserve Officers’ training corps. Sleep Health. 2019;5(3):309–14.
Poon CYS, Hui VKY, Yuen GWC, Kwong VWY, Chan CS. A well-slept teacher is a better teacher: A multi-respondent experience-sampling study on sleep, stress, and emotional transmission in the classroom. Psych J. 2019;8(3):280–292
Kusurkar R, Croiset G, ten Cate O. Implications of gender differences in motivation among medical students. Med Teach. 2013;35(2):173–4.
Vansteenkiste M, Lens W, Deci EL. Intrinsic versus extrinsic goal contents in self-determination theory: another look at the quality of academic motivation. Educational Psychologist. 2006;41(1):19–31.
ten Cate OTJ, Kusurkar RA, Williams GC. How self-determination theory can assist our understanding of the teaching and learning processes in medical education. AMEE guide No. 59. Medical Teacher. 2011;33(12):961–73.
Kember* D. Interpreting student workload and the factors which shape students’ perceptions of their workload. Stud high Educ. 2004;29(2):165–84.
Van der Meer J, Jansen E, Torenbeek M. ‘It’s almost a mindset that teachers need to change’: first-year students’ need to be inducted into time management. Stud High Educ. 2010;35(7):777–91.
Witt K, Boland A, Lamblin M, McGorry PD, Veness B, Cipriani A. Effectiveness of universal programmes for the prevention of suicidal ideation, behaviour and mental ill health in medical students: a systematic review and meta-analysis. 2019;22(2):84–90. https://doi.org/10.1136/ebmental-2019-300082.
Yusoff MSB. Interventions on medical students’ psychological health: a meta-analysis. J Taibah Univ Medical Sci. 2014;9(1):1–13.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception, design, and material preparation. Data collection was performed by Pedro Freitas Melo, Marcela Gonik Dias, Daniel Ferreira Lana e Silva, Thaís Laranjeira Lameira, Giulia Machado Caldeira Ardisson, and Bruna Teixeira de Almeida; the analyses were performed by Giancarlo Lucchetti and Alessandra Lamas Granero Lucchetti. The first draft of the manuscript was written by Oscarina da Silva Ezequiel and Giancarlo Lucchetti, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The project was approved by the University Teaching Hospital/UFJF’s Research Ethics Committee under Permit No. 2.742.787, and all study participants signed a consent form.
Consent for Publication
Not applicable
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
da Silva Ezequiel, O., Lucchetti, A.L.G., Melo, P.F. et al. Factors Associated with Motivation in Medical Students: A 30-Month Longitudinal Study. Med.Sci.Educ. 32, 1375–1385 (2022). https://doi.org/10.1007/s40670-022-01651-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-022-01651-5