Abstract
Purpose
The objective of this study is to assess the effectiveness of integrating research-based biomedical sciences into a clinical medicine program. This reform aims to enable medical students to conduct both clinical and independent research work at an early stage and to consider human disease through a mechanistic and evidence-based perspective.
Method
We designed this innovative medical program using modules that are different from those used in traditional medical programs in both China and Western countries. Thus, in this new program, we incorporated biomedical sciences components including essential theoretical and practical elements, active learning, and research skills training in the first 3 years of a 5-year program. We also offered students opportunities for oral presentation, teamwork, and leadership training.
Results
We find that students are actively engaged in this program and are enthusiastic about medical research, academically competent, and confident at expression and presentation of their data. They demonstrate leadership and teamwork skills that are essential for contemporary medical practice and prepare them by developing these skills at this early stage as they embark on their medical career. We show that students who train through this reformed program perform well at various nationwide and province-wide academic contests and show increased competitiveness in applications onto post-graduate programs.
Conclusion
Overall, we provide evidence that this new program is proving to be successful and is a worthwhile reform establishing a new paradigm for Chinese medical education. Furthermore, we suggest it is a reform that would be of interest to other countries whose medical education is not delivering the desired output of research- and evidence-based–driven doctors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
It has been 100 years since the Flexner report attempted to standardize medical education in the USA [1]. While American medical education has arguably developed the most advanced medical education model, it is undeniable that pedagogical reform needs to continue not only to reflect the changing nature of medicine in the twenty-first century, but also to improve the learning process and develop better competency in graduates.
The Global Minimum Essential Requirements (GMER), defined by the Institute for International Medical Education (IIME), proposes a number of essential competencies that a medical graduate should possess [2]. The GMER proposes seven different educational domains, of which three underpin all the others: communication skills, management of information, and critical thinking and research. Graduates therefore need to be able to analyze biomedical information through searching diverse sources, and be able to collect, organize, and interpret such information [2]. In this study, we looked to introduce reforms that are pertinent not only to improve medical education in China, but also to make it more relevant for rapidly developing healthcare advances in new disciplines.
The curriculum for Chinese medical students includes the essential disciplines of preclinical medicine consisting of core scientific subjects and clinical medicine. There has been intensive interest in medical education reform concerning ways to integrate these two parts [3,4,5,6,7]. Thus, many Chinese medical schools apply one or more of the following methods in their educational programs: problem-based learning (PBL) [8, 9], organ/system-based learning [10], case-based learning (CBL) [11], computer-assisted learning [12], and medical simulation learning [13]. The emphasis behind such reforms has been to enhance students’ motivation and ability for self-study and clinical hands-on exposure.
There are a number of significant differences between traditional Chinese medical education and contemporary Western medical education. In many medical schools in Western countries, the coalescence of preclinical core sciences with clinical medicine occurs within the first 2 years, and courses are delivered mostly through integrated organ/system-based teaching, problem-based learning, and case-based learning. The next 2 (USA) or 3 (UK) years consists of clinical clerkship and post-clerkship periods during which almost no lectures are given. Instead, students take clinical rotations during their clerkship where students undertake self-directed learning alongside bedside clinical training under the supervision of clinical staff for different clinical disciplines. After that, students come back to spend time in disciplines of their interest either in clinical or research rotations for additional post-clerkship training [14]. In most medical schools in China, medical education is dominated by individual discipline-based learning, where students sit in the classroom being exposed to didactic teaching methods for most of the timetabled curriculum [5]. Clinical medicine is taught separately in lectures in the fourth year and is combined with observation rotations in the clinical setting. Internship (clerkship) with hands-on clinical rotation is undertaken in the fifth year. The final mark of the medical course examination is the major way to evaluate the pedagogical effect, which mainly assesses the rote learning of students. However, medical education reforms embracing some of the current methods of Western medical schools are being conducted in the top Chinese medical schools, as well as in many medical schools implementing a segregated “talented class” (of selected academically excellent students) [4, 5].
According to statistical data from the China State Council in 2018, there are more than 3.6 million physicians in China (http://www.china.org.cn/china/2019-04/22/content_74707219.htm). Many Chinese physicians have extensive experience in clinical work and are capable of solving problems by using reference books, but are relatively weak at implementing evidence-based medicine and also in taking the clinical cases they encounter forward in a research perspective. Relatively few Chinese-trained physicians working in China have been internationally recognized as pioneers and leaders in medical research in either basic medical science or clinical science disciplines, while the number of physicians capable of and actively conducting research is huge in Western countries. Probably, this is the reason why a majority of medical technologies, techniques, and novel treatments are invented/developed by physicians trained in the USA, Europe, and Japan, compared with relatively few in China. Therefore, we argue that the incorporation of research-based biomedical sciences into clinical medicine programs in Chinese medical education is crucial for training a new generation of Chinese physicians equipped to catch up with the pace of medical development and innovation of the West.
Nanchang University (NCU) and Queen Mary University of London (QMUL) have launched a joint program of clinical medicine and biomedical sciences that offers a novel curriculum leading to the award of two degrees: a bachelor of sciences degree in biomedical sciences and a bachelor of medicine degree in clinical medicine (with which the graduates are eligible to take the medical license exams and thereafter practice medicine). It has been approved by the Chinese Ministry of Education and started recruiting students back in 2013. QMUL is a research-intensive institution and member of the prestigious Russell Group of leading UK universities, and NCU has a long history of clinical education and training of physicians. Together, the two universities devised a curriculum that aims to integrate basic science elements (theoretical and practical) with clinical practice, stresses the importance of evidence-based medicine, and looks to foster the independent and critical thinking ability of students and their research skills. The hope is to train future physicians who will be able to consider diseases they encounter through a research perspective with underlying mechanistic insight and curiosity.
Methods
Study Subjects and Related Ethics
Effectiveness of education is compared between NCU-QMUL joint program students with those studying on the traditional medical programs of NCU from 2013 to 2019. No discrete ethical permission is required for the project because only aggregated student scores and outcomes of education are collected and analyzed (as agreed by the ethics committee of Nanchang University Medical College). No human materials and individual personal information were required for the study and the survey was carried out anonymously.
Program Course Design
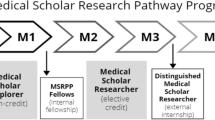
This study considered all joint program students as a whole to assess the effect of the medical pedagogy reform. Because of the dual requirements of the two degrees, course design is different from that of traditional Chinese medical programs. The characteristic teaching mode of the joint program is to transform traditional passive rote learning to active self-learning student processes (Fig. 1). Students studying on the joint program have to complete a 5-year study period encompassing three phases of medical education: preclinical medicine, clinical medicine, and clerkship. During the first 3 years, students take courses in biomedical sciences that have resonance with preclinical courses and also have incorporated advanced knowledge of biomedical research, such as genetics, cell biology, human anatomy, biochemistry, microbiology, immunology, developmental biology, pharmacology, and neurobiology. Preclinical medicine courses such as histology, physiology, pathology, cancer biology, and pathophysiology are included in the joint program curriculum. Clinical medicine courses are didactically delivered in the fourth year of the program and clerkship takes place in hospitals in the fifth year. In the first degree, standard class sizes consist of ~ 40 students, but teaching events take place in class sizes of 120 students, 40 students, 20 students, or fewer depending on the nature of the delivery and the degree of interaction needed for the teaching activity to achieve its aims.
Program course design to rebalance student learning. The joint program courses include two parts: passive learning that requires memorization of necessary elements, and active learning consisting of evidence-based study, original work that is born out of theory, group study, and problem-based learning (PBL) associated with individual modules. Efforts are made to transform passive learning processes of students to active learning
Incorporation of Research Components in the Curriculum
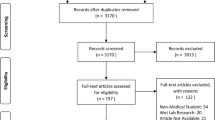
Several changes were made to the curriculum to specifically strengthen the concept of research and training of research skills in medicine: (1) practical courses associated with individual modules designed to help students learn how theory is built on research-based evidence; (2) the module Techniques in Biomedical Sciences teaches the principles of essential contemporary biotechniques and familiarity of choosing the appropriate technology for the investigation; (3) independent research project or investigative research skills are compulsory modules of the program that require students to write a thesis or report and undertake an oral defense of their individual research findings. In addition, the program also helps students look for research labs to conduct extracurricular research on specific projects (Fig. 2) and places students who are particularly interested in research to short internships in laboratories at Tsinghua University and Peking University.
Leadership and Teamwork
To develop leadership skills, the joint program initiates various group activities inside and outside class, including assessments on lecture-taught and self-learned knowledge. These activities cultivate students’ comprehensive ability and help students develop and understand their personal strengths in communication, expression, and artistic ability that together ensure students to become all-round talents rather than pedants (Fig. 3). For teamwork training, students are divided into groups of 4–6 individuals with a specific study topic. They organize meetings by themselves, upload notes, and share ideas. Everyone in the group is assigned roles; either leader or team player, with these roles changing from time to time depending on the developing nature of the topic through the groups’ work and the individual expertise each of the students could bring to bear on the topic.
Survey on Satisfaction of the Joint Program Education
The survey was conducted anonymously among joint program students to inquire about their satisfaction as students on the program. We sent the questionnaire to all cohorts from the second to fifth years. As freshman students do not yet have significant experience of the teaching approach on the joint program and therefore are less informed to make a clear judgement call on the survey, these year 1 students were excluded from this survey. The questionnaire was distributed online and voluntarily filled without collecting information on name, gender, and age to retain anonymity. The questionnaire was designed by asking four questions. For each question, there are five levels of response: strongly disagree, disagree, neither agree nor disagree, agree, and strongly agree. Using a 5-point Likert scale, strongly disagree is recorded as 1 and 5 is strongly agree. Answers which were not completely filled or did not follow the 5-point Likert scale rules were discarded. Then the mean score for each evaluation question was with a 95% confidence interval (CI).
Statistical Analysis
Statistical significance between paired groups is analyzed using the Chi-square test. Probability of P < 0.05 is of significance.
Results
The purpose of reforming the joint program curriculum was to foster the broad medico-scientific interest of students as well as training in a comprehensive ability for independent study and work. The research-integrated medical education of the joint program resulted in highly motivated students who sought out labs for extracurricular research and were able to write research papers in English. According to our statistical analysis in 2019 where academic achievements were analyzed among 2014 cohort students, the number of scientific articles published in English in peer-reviewed journals by the joint program students was significantly higher than that by traditional medical program students in the same cohort in Jiangxi Medical College (Table 1; P < 0.0001). In addition, joint program students were enthusiastic about participation in various extracurricular contests at national and provincial levels and have made magnificent achievements. The percentage of awardees in contests coming from the joint program was also significantly greater than that from the traditional medical programs in 2019 (Table 1; P < 0.01). Interestingly, NCU held an oral English contest in 2017, and joint program students took almost 50% of the awards despite being in a minority, contrasting to the majority of competing students from all other majors, even from an English major (data not shown).
By summer 2019, two cohorts had graduated from the joint program. In light of the physician to population ratio in China, there is still a shortage of physicians especially in rural areas, community hospitals, and private practitioner groups. Therefore, if graduates wish to take up such jobs, it is relatively easy after the 5 years of study. However, if students want to pursue a career in major urban hospitals, for example, the first tiered national or provincial hospitals, this is far more competitive and students need to have post-graduate qualifications, from Master to Doctoral levels. More than half of the joint program graduates have been successfully recruited onto post-graduate programs for post-graduate education. From the first (2013 entry) cohort, 97 students graduated and ~ 70% of students went on to a post-graduate program following two rounds of application. For the 2014 cohort, 50% students were admitted to a post-graduate program on their first attempt, which was not evidently different from the traditional medical program graduates (P > 0.5, Table 2). Of note, in terms of rote-learning–based national exams for post-graduate entrance, there was no significant difference in examination scores achieved by students from these two programs. In addition, we also have received unsolicited feedback from universities where our graduates applied for post-graduate study. In the interview process for post-graduate admission which tests comprehensive knowledge, responsiveness to questions, and presentation skills, the joint program students showed their strength compared with the students from the traditional medical programs. In Table 2, we further compared the post-graduate admissions between the two student groups. Rather than just considering the generic parameter of post-graduate acceptance across all universities, we drilled down in the data to identify the acceptance rate to the top five medical schools in China and top 200 world-ranked universities. These top universities put more weight on interview performance of students rather than entrance exam scores alone once an academic threshold is reached. They are highly competitive for admittance. Among students entering post-graduate programs, ~ 41% of the joint program students were admitted to this highly competitive category of universities, while only 18% of the students from the traditional medical programs were accepted (P < 0.0001) revealing a statistically significant difference in level of achievement. Given this program has been established for only 7 years, while the traditional medical program has a long history, these initial achievements of student outcomes on the joint program are satisfying and inspiring for teachers.
Finally, we performed an extensive survey on the satisfaction of the joint program education. Students actively participated in the survey (average rate is 87%). As illustrated in Table 3, the majority of students “agree” or strongly agree” that the joint program cultivates essential knowledge of clinical medicine and research skills (86.8%, 4.21 ± 1); integrates clinical medicine and biomedical sciences (85.44%, 4.14 ± 0.75); develops critical thinking and independent working ability (86.5%, 4.16 ± 0.64); and helps to apply biomedical theory to clinical issues (79.9%, 4.04 ± 0.9).
We should point out that this survey on the same content could not be performed among the traditional program students because the objective of training and course settings are very different and the same questionnaire to different programs will definitely produce biased results. The purpose of the joint program aims to cultivate the ability of students for both clinical practice and research, while the traditional program focuses on the former and student responses on each program to the same survey would not be comparable given students’ different experiences.
In the Chinese education system, parents are far more heavily involved in the education of their kids, and regular face-to-face meetings and phone enquiries are made by parents to Chinese faculty on the program. We have received extensive feedback from parents during the study period and after graduation of satisfaction with the experience and the outcomes of the program on their children. Furthermore, hospital faculty have also provided feedback when we have enquired about our students, and have commented that our students are qualitatively different from the traditional medical students and are confident to ask questions. Such non-systematic anecdotal evidence is not meant to be comparative nor statistically significant, but is encouraging that both parents, and hospital and research faculty, either from their interaction with students in independent research projects or internships, are very positive about the joint program to date. However to properly analyze the effects of the program, we will need to wait to evaluate the long-term graduate destination and achievements of our students in a comparative fashion with the traditional medical program using medical practice, basic/medical research, and both metrics combined!
Discussion
Active Learning
Chinese medical students have traditionally relied almost wholly on passive rote learning. Lecturers cram huge amounts of knowledge in lectures that are didactically delivered in limited time in classes so that students have no chance to express themselves or interact with lecturers or the knowledge presented. They then spend the majority of time outside class to review lectures and memorize what has been taught. There is thus no time to challenge knowledge nor understand the basis of knowledge creation. In contrast, as summarized in Fig. 1, the biomedical sciences program advocates active self-learning and critical thinking, which teaches students what knowledge is, how it is discovered, and importantly how understanding can be extended through research, a critical skill if medical science is to move forward. In addition to providing reference to key textbooks in the early stages of the curriculum, lecturers also provide links to original research articles regarding specific biomedical findings and even discuss original data in class to make sure the students understand how to critically analyze data and research findings and learn the process of knowledge acquisition. Students are continually challenged to extend their knowledge in a critical manner ensuring this is evidence-based. Students are expected to collect and make use of information from the published literature and the Internet, and thus lecturers also train them how to utilize and judge the quality and source of available data. For example, when studying cancer genetics, there are many types of cancer and each is due to different gene mutations and genetic combinations. The lecturers do not obligate students to memorize every molecular change of those cancers, but rather teach students to utilize public databases in an informed manner. This is more fitting with the clear ongoing evolution of medicine where physicians and patients alike will have a wealth of information at their fingertips; the expertise of the physician will be in interpretation and judgement of the quality of that information and effectively use such information for design of the best treatment for optimizing patient outcomes. In workshops that run alongside the advanced biomedical courses, lecturers first guide students how to search for useful papers and database information in the public domain step by step. Subsequently, students are given assignments on specific topics where students use these new skills within a limited timeframe.
The transition from rote learning that students employ during high school to the active learning style discussed above on the joint program requires support and guidance, and this is as true for Western as well as Chinese students. To support joint program students in this transition, the Personal Development Program (PDP) module is a prominent feature of the joint program during years 1–3. For example, PDP provides students with many opportunities to develop and practice presentations in small groups. Students learn professional presentation skills such as preparation of clear and eye-catching PowerPoint presentations, coaching in personal conduct when delivering the presentation, and receiving tailored guidance for individual development of their own oral presentation styles. For every theme addressed by PDP, students are engaged in active learning and complete assignments ranging from short essays to presentations.
Research Skills
Despite significant investment in medical research in China, the internationally recognized research advances that might be expected from Chinese physicians have yet to match this investment. We suggest that exposure to research throughout early medical training will prepare Chinese physicians and medical researchers to be far more competitive on the international stage. Hence, the joint program puts significant emphasis on training laboratory and research skills in the first 3 years during the biomedical science degree (Fig. 2) including lab practicals associated with all modules and a specific research skills module. However, especially important in their development, in year 3, students are introduced into independent research through undertaking either the Research Project or Investigative Skills modules as a significant part of the biomedical sciences degree. In these modules, students learn to formulate research questions under the direction of supervisors, read and identify the appropriate evidence-based literature on specific biomedical topics, write proposals for experimental design to address their research questions, and then carry out the short research projects. On completion of their projects, students write thesis reports in an identical format for normal scientific publishing and present and defend their research findings in examination. The top research projects are selected for an annual oral presentation contest and they answer questions from members of a judging panel consisting of invited national and international professors. This process is central in changing the mindset of medical students to become future research leaders by training students how to carry out research, interpret, present, and defend research data and this inspires their biomedical research interest as well.
The curriculum in the first 3 years thereby confers students with advanced essential knowledge in biomedical sciences and exposes them progressively to research, by routinely presenting the research base of fundamental knowledge. These learning experiences improve students’ ability to comment, criticize others’ work, and interact with peers as well.
Interestingly, a related study also identified that the medical curriculum could be improved by introducing foundational science electives during the clinical clerkship period [14]. In this study analyzing a single cohort of students, the science electives proved highly popular among the student cohort tested, who further commented their belief that this intervention would positively impact their clinical training and practice (14). In our study, we introduce mandatory fundamental evidenced-based science from the start of the curriculum, at a time where we believe may have yet greater impact on their development as future research active and innovative clinicians. Joint program students also positively responded to the innovations we introduced, but we also present evidence of increasing competitiveness of joint program students at post-graduate entrance as well as other graduate attributes.
Leadership and Teamwork Skills
In current medical practice, leadership and teamwork are especially important requirements for qualified doctors. As we enter an era of big data, systems biology, and networks in medicine, it has become clear that these large datasets and information systems cannot be effectively used by isolated individuals but, instead, rely on teamwork and effective collaboration. Likewise, leadership styles have been shown to correlate with medical outcomes for individual patients [15]. Therefore, modern medical education should educate students to be adapted for both leadership and teamwork roles (Fig. 3). As the joint program emphasizes training in these graduate attributes, students pay significant attention to assigned group tasks and actively take part in group activities, where they give feedback on each other’s work. These activities help students develop critical thinking and improve interpersonal skills, teamwork ability, and leadership as they not only receive but also give feedback. All these approaches convert passive didactic learning into active self-learning, leading to marked increases in students’ interest in study. They also help develop their underlying self-confidence and ability to deal with unknown problems encountered in their future careers.
To become a leader, students have to be confident and adept in communication. They have many chances to be called upon to express themselves in the joint program, such that their personal courage and confidence are nurtured and developed. In the interview part of post-graduate application, many joint program students feedback to us that they can answer interviewers’ questions fluently. Besides showing their deep understanding of research, they tend to express themselves well and not be afraid of communicating in English. Being trained with various presentation skills, they achieve excellent results with a high ranking and are hugely competitive compared with traditional medical students (Table 2). Therefore, we can see the joint program students are good at communicating in English and are capable of giving presentations confidently, clearly, and convincingly.
In summary, students studying on the joint program progressively learn how to obtain evidence throughout the foundation biomedical science modules and learn how to discover and evaluate mechanisms behind the phenomena. When it comes to clinical practice, the joint program students can not only symptomatically treat patients, but also have learned skills to find evidence to support their diagnosis. By being able to evaluate the current knowledge of the mechanisms behind the diseases they encounter, they are well placed to be in a position to also become research leaders in the field of their chosen specializations as their medical careers mature. In terms of patient outcomes, we hope this translates into an ability where they can treat patients precisely with clear targets and be well positioned to develop improvements in treatment.
Conclusions
Our joint venture between NCU and QMUL reforms medical education through the integration of biomedicine with clinical medicine by including research center stage in both fundamental and medical sciences to ultimately find resonance in the clinic. Thus, throughout the program, students are encouraged to challenge current theory and learn that not everything published or taught is necessarily correct, and all these can be tested by experimental research. In this study, we present evidence that this novel approach has thus far proven to be successful.
In the West, medical advancement has progressed at pace where clinical practice and scientific research go hand in hand. This infrastructure has also been recognized to be essential to advance medicine in China, and we believe that our educational reforms will equip graduates to particularly thrive under the shifting sands of clinical practice and research and their interplay.
Data Availability
Available upon request.
Abbreviations
- PBL:
-
problem-based learning
- CBL:
-
case-based learning
- NCU:
-
Nanchang University
- QMUL:
-
Queen Mary University of London
- BSc:
-
Bachelor of Sciences
- PDP:
-
Personal Development Program
- GMER:
-
Global Minimum Essential Requirements
- IIME:
-
Institute for International Medical Education
References
Flexner A. Medical education in the United States and Canada. From the Carnegie Foundation for the Advancement of Teaching, Bulletin Number Four, 1910. Bull World Health Organ. 2002;80(7):594–602.
Core Committee IfIME. Global minimum essential requirements in medical education. Med Teach. 2002;24(2):130–5.
Field M, Geffen L, Walters T. Current perspectives on medical education in China. Med Educ. 2006;40(10):938–9.
Huang L, Cai Q, Cheng L, Kosik R, Mandell G, Wang SJ, et al. Analysis of curricular reform practices at Chinese medical schools. Teach Learn Med. 2014;26(4):412–9.
Huang L, Cheng L, Cai Q, Kosik RO, Huang Y, Zhao X, et al. Curriculum reform at Chinese medical schools: what have we learned? Med Teach. 2014;36(12):1043–50.
Lam TP, Wan XH, Ip MS. Current perspectives on medical education in China. Med Educ. 2006;40(10):940–9.
Xu D, Sun B, Wan X, Ke Y. Reformation of medical education in China. Lancet. 2010;375(9725):1502–4.
Davis MH. AMEE Medical Education Guide No. 15: Problem-based learning: a practical guide. Med Teach. 1999;21(2):130–40.
Dahle LO, Brynhildsen J, Behrbohm Fallsberg M, Rundquist I, Hammar M. Pros and cons of vertical integration between clinical medicine and basic science within a problem-based undergraduate medical curriculum: examples and experiences from Linkoping, Sweden. Med Teach. 2002;24(3):280–5.
Brooks WS, Woodley KT, Jackson JR, Hoesley CJ. Integration of gross anatomy in an organ system-based medical curriculum: strategies and challenges. Anat Sci Educ. 2015;8(3):266–74.
Samuelson DB, Divaris K, De Kok IJ. Benefits of case-based versus traditional lecture-based instruction in a preclinical removable prosthodontics course. J Dent Educ. 2017;81(4):387–94.
Murray TS, Cupples RW, Barber JH, Hannay DR, Scott DB. Computer-assisted learning in undergraduate medical teaching. Lancet. 1976;1(7957):474–6.
Piette A, Muchirahondo F, Mangezi W, Iversen A, Cowan F, Dube M, et al. Simulation-based learning in psychiatry for undergraduates at the University of Zimbabwe medical school. BMC Med Educ. 2015;15:23.
Dahlman KB, Weinger MB, Lomis KD, Nanney L, Osheroff N, Moore DE Jr, et al. Integrating foundational sciences in a clinical context in the post-clerkship curriculum. Med Sci Educ. 2018;28(1):145–54.
Shubeck SP, Kanters AE, Dimick JB. Surgeon leadership style and risk-adjusted patient outcomes. Surg Endosc. 2019;33(2):471–4.
Acknowledgments
We thank Mr. Huaan Xiao, and Ms. Ping Liu and Jiahe Yu for assistance in collecting aggregated data.
Funding
This work was supported by the Jiangxi Province Education Reform Grant (JXJG-15-1-7). This grant aimed to support studies on education reform including curricular design, innovation of teaching and learning methods, and improvement of students’ learning experiences.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to this work including formulation of the concept, design of the structure, and writing of the manuscript. ZTL and YH wrote most of manuscript. MM, ZJL, and YY were responsible for the design of the joint program courses. ZJL supervised ZTL to draft the manuscript and make corrections. MM provided critical ideas and inputs on the writing of manuscript and helped with English editing.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval and Consent to Participate
The protocol was submitted to the ethics committee of Nanchang University Jiangxi Medical College before the study was conducted. Since the study did not involve human materials and personal information, but rather analyzed aggregated data, approving process by the Institutional Review Boards was exempted.
Consent for Publication
Not applicable. The usage of data was approved by the NCU Department of Teaching Affairs and the Deans’ office of Nanchang University Queen Mary School.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, Z., He, Y., Yang, Y. et al. A Medical Pedagogy Reform by Integration of Biomedical Research into the Clinical Medicine Program. Med.Sci.Educ. 30, 1569–1576 (2020). https://doi.org/10.1007/s40670-020-01105-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-020-01105-w