Abstract
Purpose
Empathy tends to decline during medical education, typically beginning in the third year of medical school and often continuing throughout residency and the physician’s medical career. The purpose of this study was to determine if first year medical student empathy is affected by small group interactions with patients with neurological disorders, and to investigate if changes in empathy persisted over time.
Materials and Methods
Eighty first year medical students participating in a Neuroscience Module interacted with a variety of neurological patients in a small group informational session. Prior to the experience, participants completed the Jefferson Scale of Physician Empathy–Student (JSPE-S) version. After the experience, students completed a post-test JSPE-S questionnaire, and a final post-post-test JSPE-S questionnaire was completed 5 weeks later. Empathy scores were compared with a repeated measures MANOVA. The relationship between gender and empathy, and the effect of the age of the neurological patients on empathy scores were also examined.
Results
Empathy scores for seventy-one students who completed the JSPE-S questionnaires were analyzed. Students had significantly higher empathy immediately after the patient interaction experience, and the change in empathy was sustained over the course of 5 weeks (p = 0.015). The age of the neurological patients had a significant effect on empathy scores. There was no significant difference between empathy scores and gender.
Conclusions
This study supports the incorporation of a group patient interaction experience into the medical school curriculum as an inexpensive and practical method of enhancing medical student empathy in a non-clinical setting.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There are several different ways to define empathy—a concept that is frequently described in the literature as ambiguous and elusive. Some researchers have portrayed empathy as an affective attribute, primarily involving feeling the concerns of an individual [1, 2], while others have described empathy as a cognitive attribute, primarily involving understanding the concerns of another [3, 4]. Empathy can also be viewed as a multi-factorial concept, containing both affective and cognitive components [5]. Yet in the clinical context of health professional education and patient care, empathy is most often defined as a predominately cognitive characteristic [6]. This definition emphasizes understanding, as opposed to feeling, a patient’s experiences and perspectives—combined with a capacity to communicate this understanding in order to create an intention to help [7, 8]. A focus on this cognitive conceptualization has provided a framework for the development of a content-specific instrument for measuring empathy in the context of medical education and patient care [8], the Jefferson Scale of Physician Empathy–Student (JSPE-S) version. Since its development in 2001, the JSPE-S has been used for different health professional students and practitioners in more than 70 countries [9]. Three different versions of the JSPE are available for medical students, physicians/other health professionals, and students in any health profession fields other than medicine. Evidence in support of the JSPE’s construct validity [7], criterion-related validity [10], predictive validity [11], internal consistency reliability [10], and test-retest reliability [7] has been reported.
Clinical empathy plays an important role in the physician-patient relationship by allowing physicians to better understand the experiences and perspectives of their patients [12]. Higher physician empathy is linked to better glycemic control [13], greater patient satisfaction and empowerment [14], and increased treatment compliance [14]. In regard to clinicians, increased physician empathy results in higher supervisor ratings of clinical competence, decreased malpractice litigation, and increased job satisfaction [12]. The Association of American Medical Colleges (AAMC) recognizes the importance of empathy and includes enrichment of interpersonal skills and empathy among the educational objectives of undergraduate medical education [15]. Empathy has been shown to be relevant to medical student clinical performance, as demonstrated by a study that found a positive association between empathy scores and ratings of clinical competence in core clinical clerkships [16]. Significant inverse associations between empathy and burnout have also been observed among medical students [17,18,19].
Evidence supporting the positive effects of empathy in the clinical environment is abundant, yet despite these known benefits, it has been reported that as many as 75% of medical students become more cynical about academic life and the medical profession as they progress through medical school [20]. Longitudinal studies have observed a significant decline in empathy between the beginning and the end of the third medical school year [8, 20]. Research also indicates that empathy continues to decline during residency training [21]. The loss of empathy beginning in medical school can be attributed to several factors, including lack of role models, a high volume of educational material, time pressure, and patient and environmental factors [8]. It has also been reported that the emphasis of modern medical education (with an overreliance on computer-based diagnostic and therapeutic technology) promotes emotional detachment, affective distance, and clinical neutrality [22,23,24]. Individual medical students may also have an inherent difference in their level of empathy, as evidenced by a number of studies suggesting that females tend to have greater empathic responses than males, particularly in regard to the affective component of empathy [15]. In terms of age, there is a lack of significant associations in the literature between age and empathy, although higher JSPE empathy scores have been observed among older individuals [15].
Not all studies examining medical student empathy have found similar patterns of decline, causing researchers to question a lack of consistency regarding the definition of empathy, study design and instrumentation, and an over-reliance on cognition and self-report [16]. In addition, most of the work reporting a decline in empathy has originated from medical schools in the USA, whereas reports originating in the UK appear to demonstrate no change or even increases in empathy scores across medical training [25, 26]. A study done in Ethiopia showed an increase in cognitive empathy between the first and final year of training, but showed no change in emotional empathy [27], while a study conducted in Iran showed no difference throughout medical training [28]. These findings likely highlight the importance of cultural differences on clinical training, practice, and environments.
Although the AAMC recognizes the importance of empathy in undergraduate medical education [15], there is a varying amount of emphasis among medical schools that is placed on the development and enhancement of student empathy skills. A lack of curriculum hours focusing on the teaching and discussion of the psychosocial aspects of patient care, along with infrequent formal testing, may be a contributing factor to the observed decline in empathy during medical school [29]. These findings suggest that formative efforts should be implemented to improve empathy skills. A systematic review by Kelm et al. (2014) supports the notion that empathy can be enhanced by teaching [30]. Various approaches have been implemented to increase and sustain medical student empathy, including perspective taking, interpersonal skills training, exposure to role models, role playing, studying humanities, and reviewing recordings of simulated patient encounters [31,32,33]. Yet other interventions have yielded differing results, such as a study by Lim et al. (2016) demonstrating that the introduction of an empathy teaching innovation increased medical students’ portrayal of clinical empathy as perceived by simulated patients, but did not significantly increase student self-reported empathy [29]. The variation in the literature among self-reported empathy suggests that individual perceptions of empathy may not always be accurate. Research has shown that learning appropriate body language and phrases to use during standardized patient encounters may not necessarily lead to “genuine” empathy, since students are often looking inward during these situations rather than adopting the outward perspective integral to empathy [12].
During the first year of medical school at the University of South Carolina School of Medicine Greenville (USCSOMG), students are given immediate exposure to patient care and community engagement by becoming certified Emergency Medical Technicians. Additional patient interactions are incorporated into the first 2 years of medical school in the form of patient panels and a unique small group session involving neurological patients, the Meet the Patients experience. While the goal of implementing these distinctive experiences is to increase patient exposure, the students may also be receiving the benefit of increased awareness and understanding of how to deliver compassionate, patient-centered care. The purpose of this study was to determine if first year medical student empathy is affected by small group interactions with patients with neurological disorders, and to investigate if changes in empathy persisted over time.
Materials and Methods
Our study included 80 first year medical students (54 females and 26 males) who participated in the Meet the Patients experience at the University of South Carolina School of Medicine Greenville (USCSOMG). The study was approved by the Institutional Review Board of the University of South Carolina, and all students consented to participate.
The Meet the Patients Experience and Group Debriefing
The Meet the Patients (MTP) experience at the USCSOMG is conducted during the Neuroscience Module in the first year of medical school. Through this experience, students are given the opportunity to interact with patients who have been diagnosed with a variety of different neurological disorders. The purpose of the MTP experience is to help the students learn about the disorders as they relate to the patients themselves, rather than focusing on the pathophysiology alone. Ten different patients with neurological disorders volunteer to come to the medical school campus to discuss their diagnosis, their activities of daily living, their prognosis, and how the disorder affects their families. The neurological disorders typically represented in the MTP experience are demonstrated in Table 1.
Students in the Neuroscience Module are divided into groups of 10, and each group spends 30 min with one of the patients. After meeting with the first patient, the students meet with another of the 10 patients for an additional 30 min. Each student meets with two different patients, but not all students meet with the same patients. Students are given the opportunity to ask questions pertinent to the patient’s disorder. Patients’ family members are also available to answer students’ questions regarding the patients’ conditions, as well as their own challenges in working with the patients at home. Immediately following the small group interactions with the patients, all students gather together for a discussion of the experience.
The group debriefing, during which students share their observations with one another, takes approximately 2 h. Biomedical sciences faculty and clinicians (such as neurologists, neurosurgeons, and neuroradiologists) also take part in the discussion and expand upon pertinent clinical and neuroscience-related concepts to further contribute to the overall experience. The patients are not present during the debriefing session. Student groups are given the opportunity to choose 2–3 members to present each patient to the class. The group representatives state the patient’s condition and general demographic information, and then reflect on their discussion with the patient by sharing what they learned from the interaction, how they were impacted emotionally, and how the experience enhanced their understanding of neuroscience-related concepts introduced in the module.
Jefferson Scale of Physician Empathy–Student Version
Medical student empathy was assessed using the Jefferson Scale of Physician Empathy–Student (JSPE-S) version. This task is the most widely used measure of cognitive empathy in the context of patient care, and numerous studies support the construct [7], criterion-related [10], and predictive validity [11], as well as the internal consistency [10] and test-retest reliability [7]. Two questions addressing demographic information were additionally included in the participant questionnaire. Students provided answers to the JSPE-S questions using a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The following statements are examples of phrases that were used to assess empathy in the JSPE-S: “Physicians’ understanding of their patients’ feelings and the feelings of their patients’ families does not influence treatment outcomes”; “Patients feel better when their physicians understand their feelings”; “It is difficult for a physician to view things from patients’ perspectives.”
Data Collection and Analysis
Immediately prior to the MTP experience, the participating medical students were given the JSPE-S (referred to as the pre-test version), including the demographic questions, to complete online. Following completion of the questionnaire, the participants were divided into small groups and began the MTP experience. After the completion of the MTP experience and group debriefing, participants were given the same version of the JSPE-S (referred to as the post-test version) to once again complete electronically. Five weeks after the MTP experience, participants were given the same version of the JSPE-S (referred to as the post-post-test version) to complete online. A timeline of the study procedure is demonstrated in Table 2. A within-subjects design was used to compare participant data.
Mean empathy scores were initially analyzed using a repeated measures MANOVA to determine if the Meet the Patients experience affected medical student empathy, and if the effect lasted over time. A between-subjects MANOVA was used to compare mean empathy scores by gender. A Pearson correlation was used to examine the relationship between medical student empathy scores and the age of the neurological patients. The 10 neurological patients taking part in the Meet the Patients experience were divided into two groups, below the age of 20 (teenage) and above the age of 20 (adult). There were four teenage patients and six adult patients.
Results
Of the 80 total participating medical students, data for 9 participants was excluded due to the completion of only one of the three JSPE-S surveys. The 71 analyzed participants completed at least two of the three JSPE-S surveys (the pre-test questionnaire and either the post-test or post-post-test questionnaire). The response rate for the JSPE-S surveys for the analyzed participants is as follows: 71 students (100%) completed the pre-test questionnaire, 69 students (86.25%) completed the post-test questionnaire, and 37 students (48.75%) completed the post-post-test questionnaire. Of the 71 analyzed participants, 49 (69%) were female and 22 (31%) were male. Participating medical students ranged between the ages of 20 and 36 (mean age 22, SD 2.4 years).
The Meet the Patients Experience and Empathy
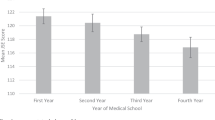
We calculated the mean medical student empathy scores for the pre-test (112.07, SD 8.96), post-test (114.1, SD 8.96), and post-post-test (113.44, SD 10.50) JSPE-S surveys. We performed a repeated measures MANOVA to compare the mean empathy scores and found that the Meet the Patients experience significantly increased medical student empathy (Fig. 1). A Tukey’s LSD post hoc analysis revealed a significant difference between the pre-test and post-test empathy scores, F(2,32) = 4.766, p = 0.015. There was also a significant difference between the medical student pre-test and post-post-test mean empathy scores (p < 0.05), reflecting that the increase in medical student empathy was sustained over the course of 5 weeks. There was no significant difference between the mean empathy scores for the post-test and the post-post-test JSPE-S survey.
Mean medical student JSPE-S empathy scores for the pre-test, post-test, and post-post-test questionnaires. There was an increase in mean empathy scores immediately after the MTP experience, and a significant difference was found between the pre-test and post-test empathy scores, F(2,32) = 4.766, p = 0.015. There was also a significant difference between the pre-test and post-post-test mean empathy scores (p < 0.05), reflecting that the increase in medical student empathy was sustained over the course of 5 weeks. There was no significant difference between the mean empathy scores for the post-test and the post-post-test JSPE-S survey
Gender and Empathy
We calculated the mean empathy scores for males and females for the JSPE-S pre-test (males = 111.86, SD 9.66; females = 109.13, SD 6.87), post-test (males = 114.94, SD 9.73; females = 112.91, SD 7.56), and post-post-test (males = 115.36, SD 10.07; females = 112.66, SD 10.81) survey. A between-subjects MANOVA was used to compare the mean empathy scores by gender, and no significant difference was found. Although it was not significant, the mean empathy scores for males were higher than those of the female participants for each of the three time periods.
Age of Neurological Patients and Empathy
There was no significant relationship between patient age and medical student post-test mean empathy scores. However, a significant inverse relationship was present between patient age and medical student post-post-test mean empathy scores (Fig. 2). The teenage neurological patients elicited a higher medical student empathic response after the course of 5 weeks compared with that of the adult neurological patients, r(38) = − 0.383, p < 0.05. Medical students who met at least one teenage patient had a mean post-post-test empathy score of 119.70 (SD 4.90), while medical students who met only adult patients had a mean post-post-test empathy score of 111.02 (SD 9.10).
Discussion
It has been suggested that a lack of curriculum hours focusing on the teaching and discussion of the psychosocial aspects of patient care may be a contributing factor to the observed decline in empathy during medical school [29]. The purpose of our study was to determine if the implementation of an experience involving small group interactions with patients with neurological disorders would result in changes in first year medical student empathy. Our analysis of the JSPE-S surveys showed a significant increase in mean empathy scores immediately after the Meet the Patients experience, and this increase was sustained over the course of 5 weeks. The measurement of long-term assessment for durability of effect distinguishes this study from several other reports of educational interventions to promote medical student empathy. Many studies reporting increases in empathy as a result of implementing an educational intervention do not examine the durability of the change. In the future, we plan to conduct a similar study assessing the effects of the Meet the Patients Experience on empathy over a longer time period, potentially throughout the students’ next 2 years of medical school. Given that the decline in medical student empathy often begins during the third year, focusing on first year students allows educators to capture these individuals when they are potentially at the height of their empathic nature. The results of our study show that the Meet the Patients experience is an effective curricular tool that can increase empathy in the earliest phase of a future physician’s career. We hope to implement similar patient interaction experiences in the second and third years of medical school in order to further investigate if similar patterns can be replicated as students progress throughout their undergraduate medical education.
Our results support the idea that various interdisciplinary approaches and curricular interventions, such as reflective writing [34] and activities focusing on perspective taking and exposure to role models [31,32,33], do have the ability to both enhance and sustain medical student empathy. The Meet the Patients experience specifically allows medical students attending the USC School of Medicine Greenville to expand their knowledge of a neurological disorder by learning more about the medical care of that disorder through an individual patient’s perspective. This emphasis on communicating an understanding of a patient’s experiences and perspectives reflects the cognitive conceptualization of empathy, which provided the framework for the development of the JSPE-S. Therefore, our use of the validated JSPE-S focusing on empathy as a cognitive attribute further strengthens our results. Another study utilizing the experience of neurological patients showed a similar increase in medical student empathy [35]. Students participated in a simulated experience as either a stroke patient or a caregiver, and the experiential learning role play resulted in a statistically significant increase in mean JSPE-S scores from baseline to post-participation [35].
In regard to the age of the neurological patients, the results of our study showed that medical students who met at least one teenage patient, as opposed to students who met only adult neurological patients, experienced a significantly higher increase in mean empathy scores at the end of the 5-week study period. There is little evidence in the literature to support whether patient age has a significant effect on medical student or physician empathy, and no studies have been conducted that directly compare provider empathy levels towards adult and teenage or pediatric populations. One potential explanation may relate to the assumption that younger people are not expected to be affected by illness as frequently as adults, and/or that many diseases are normally associated with older individuals. It is possible that the medical students empathized more with younger patients due to being closer in age to those patients. However, we did not find any relationship in our study between the age of the participant and the age of the patient, and the age of the participant was not related to empathy scores (either pre, post, or post-post) (p > .05). The results of our study do not support that students were able to empathize more with individuals closer to their own age, but further research is needed to determine whether the age of a patient influences medical student or physician empathy in the clinical context.
Upon examining gender, and in contrast to previous findings, our results showed no significant difference between gender and mean empathy scores of participating medical students. Our study included 80 first year medical students (54 females and 26 males). The roughly 2:1 ratio of female to male participants does not reflect the class demographic (which is ~ 57% female and ~ 43% male), but is rather representative of the fact that more women volunteered to be a part of the study. There is a large body of evidence suggesting that females tend to have greater empathic responses than males, particularly in regard to the affective component of empathy [15]. Although the difference was not significant, the mean empathy scores for males in our study were higher than those of the female participants for each of the three time periods. The mechanisms underlying these results require further exploration.
While the gender differences we observed in our study were not significant, it is important to consider, as evidenced by previous research, that some students may be more vulnerable to losing their sense of empathy [8]. One study demonstrated that students with lower empathy scores at the beginning of medical school lost more empathy over time than those with relatively higher scores at baseline [8]. This factor may play a role in differing individual responses to curricular interventions designed to maintain or enhance empathy. Shapiro et al. (2019) demonstrated that the development and implementation of a mandatory human kindness curriculum given during the initial 2 years of medical school was associated with significant positive changes in self-reported empathy, particularly among students entering with low scores [36]. This multi-specialty and interdisciplinary approach also showed that empathy levels were maintained among students with initially high scores [36]. The positive implications associated with physician empathy, in addition to the established relationship between empathy and clinical competence [37], has led some researchers to recommend that the capacity for empathy and relevant personal qualities be included in the selection criteria for admission to medical school [38].
Limitations
The limitations of our study include the absence of a control group in the survey design, attrition bias among participants, and individual patient variation within the Meet the Patients experience. We ideally would have included a control group in our study, but all first year medical students at the USC School of Medicine Greenville are required to participate in the Meet the Patients experience as part of the Neuroscience Module. The use of a within-subjects design to analyze the JSPE-S scores was chosen to reflect our single study population. We also were not able to control the outside experiences of our student participants between the post- and post-post-test questionnaires. Students may have had additional patient encounters through EMT shifts or large group patient panels in their Integrated Practice of Medicine course between completing these surveys, but these experiences are consistent with what medical students in Greenville are exposed to throughout the entire school year. A control group consisting of students who do not participate in the Meet the Patients experience could be achieved with the recruitment of first year medical students from a different medical school that does not have a similar patient interaction activity within the same 5-week time period. This expanded study population will be considered for future studies.
The neurological patients who volunteer to participate in the Meet the Patients experience represent individuals with a variety of disorders and differing levels of severity. Because the first year medical students are split into multiple small groups during the Meet the Patients experience, with each group spending 30 min with two different patients, all students are not able to meet the same patients. Although the students were not asked to rate the severity of the patients’ disorders, conditions that likely would be rated as more severe had significantly higher post and post-post empathy scores than disorders that likely would be considered less severe, F(10,55) = 2.63, p = .016. For example, a Tukey’s post hoc analysis showed that students who saw patients with myasthenia gravis and Tourette’s syndrome elicited significantly lower empathy scores (both post- and post-post-test) in comparison to students who saw patients with cerebral palsy and amyotrophic lateral sclerosis. However, the effect size was relatively small (휂2 = 0.4). In order to further explore whether certain neurological disorders have different effects on empathy, we plan to repeat our study in the future and incorporate participant ratings of disorder severity. This addition will allow for a stronger analysis of empathy scores based on which neurological patients were seen by the participating students. Patient age, in addition to disorder severity, will also be taken into account when designing the next annual Meet the Patients experience.
Conclusions
While there are many factors that may contribute to a decline in medical student empathy, this study showed that small group interactions with patients with neurological disorders enhanced first year medical student empathy, both immediately and over the course of 5 weeks. As a result, we believe that the Meet the Patients experience serves as a valuable part of the curriculum at the University of South Carolina School of Medicine Greenville. Exposure to patient interaction outside of the clinical environment can be an inexpensive and powerful tool to further a student’s understanding of how patients personally experience a particular disorder, which may influence the way in which the medical student will one day empathize with future patients. Increasing medical student empathy will ultimately benefit both physicians and patients, leading to better health outcomes and increased physician job satisfaction. Future studies examining longitudinal changes in medical student empathy over longer time periods are needed to further examine the lasting effects of similar curricular interventions, and continuing to explore individual patient characteristics (such as age and disorder severity) would provide useful information regarding additional factors that may affect medical student and physician empathy.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on request.
References
Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159(9):1563–9.
Neumann M, Bensing J, Mercer S, Ernstmann N, Ommen O, Pfaff H. Analyzing the “nature” and “specific effectiveness” of clinical empathy: a theoretical overview and contribution towards a theory-based research agenda. Patient Educ Couns. 2009;74(3):339–46.
Kohut H. The psychoanalytic treatment of narcissistic personality disorders: outline of a systematic approach. The psychoanalytic Study of the Child. 1968;23(1):86–113.
Basch MF. Empathic understanding: a review of the concept and some theoretical considerations. J Am Psychoanal Assoc. 1983;31(1):101–26.
Youssef FF, Nunes P, Sa B, Williams S. An exploration of changes in cognitive and emotional empathy among medical students in the Caribbean. Int J Med Educ. 2014;5:185–92.
Hojat M, Mangione S, Gonnella JS, Nasca T, Veloski JJ, Kane G. Empathy in medical education and patient care. Acad Med. 2001;76(7):669.
Hojat M. Empathy in patient care: antecedents, development, measurement, and outcomes. N Engl J Med. 2007;356(17):1792.
Hojat M, Vergare MJ, Maxwell K, Brainard G, Herrine SK, Isenberg GA, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182–91.
Hojat M, Gonnella JS. Eleven years of data on the Jefferson scale of empathy-medical student version (JSE-S): proxy norm data and tentative cutoff scores. Med Princ Pract. 2015;24(4):344–50.
Hojat M, Mangione S, Nasca TJ, Cohen MJM, Gonnella JS, Erdmann JB, et al. The Jefferson Scale of Physician Empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001;61(2):349–65.
Hojat M, Mangione S, Nasca TJ, Gonnella JS, Magee M. Empathy scores in medical school and ratings of empathic behavior in residency training 3 years later. J Soc Psychol. 2005;145(6):663–72.
Fowler LA, Ellis S. The effect of 12 hour shifts, time of day, and sleepiness on emotional empathy and burnout in medical students. Clocks Sleep. 2019;1(4):501–9.
Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359–64.
Hojat M, Louis DZ, Maxwell K, Markham F, Wender R, Gonnella JS. Patient perceptions of physician empathy, satisfaction with physician, interpersonal trust, and compliance. Int J Med Educ. 2010;1:83.
Sulzer SH, Feinstein NW, Wendland CL. Assessing empathy development in medical education: a systematic review. Med Educ. 2016;50(3):300–10.
Hojat M, Gonnella JS, Mangione S, Nasca TJ, Veloski JJ, Erdmann JB, et al. Empathy in medical students as related to academic performance, clinical competence and gender. Med Educ. 2002;36(6):522–7.
Shanafelt TD, West C, Zhao X, Novotny P, Kolars J, Habermann T, et al. Relationship between increased personal well-being and enhanced empathy among. J Gen Intern Med. 2005;20(7):559–64.
Thomas MR, Dyrbye LN, Huntington JL, Lawson KL, Novotny PJ, Sloan JA, et al. How do distress and well-being relate to medical student empathy? A multicenter study. J Gen Intern Med. 2007;22(2):177–83.
Brazeau CM, Schroeder R, Rovi S, Boyd L. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. 2010;85(10):S33–6.
Hojat M, Mangione S, Nasca TJ, Rattner S, Erdmann JB, Gonnella JS, et al. An empirical study of decline in empathy in medical school. Med Ed. 2004;38(9):934–42.
Bellini LM, Shea JA. Mood change and empathy decline persist during three years of internal medicine training. Acad Med. 2005;80(2):164–7.
Halpern J. From detached concern to empathy: humanizing medical practice. Oxford University Press; 2001. Am J Psychiatry 160:11
Farber NJ, Novack DH, O’brien MK. Love, boundaries, and the patient-physician relationship. Arch Intern Med. 1997;157(20):2291–4.
Coulehan J, Williams PC. Vanquishing virtue: the impact of medical education. Acad Med. 2001;76(6):598–605.
Quince TA, Parker RA, Wood DF, Benson JA. Stability of empathy among undergraduate medical students: a longitudinal study at one UK medical school. BMC Med Educ. 2011;11(1):90.
Tavakol S, Dennick R, Tavakol M. Empathy in UK medical students: differences by gender, medical year and specialty interest. Educ Prim Care. 2011;22(5):297–303.
Dehning S, Girma E, Gasperi S, Meyer S, Tesfaye M, Siebeck M. Comparative cross-sectional study of empathy among first year and final year medical students in Jimma University, Ethiopia: steady state of the heart and opening of the eyes. BMC Med Educ. 2012;12(1):34.
Rahimi-Madiseh M, Tavakol M, Dennick R, Nasiri J. Empathy in Iranian medical students: a preliminary psychometric analysis and differences by gender and year of medical school. Med Teach. 2010;32(11):e471–8.
Lim BT, Moriarty H, Huthwaite M, Gallagher P, Perera R. Teaching empathy to undergraduate medical students: translation to practice. FoHPE. 2016;17(1):59–70.
Kelm Z, Womer J, Walter JK, Feudtner C. Interventions to cultivate physician empathy: a systematic review. BMC Med Educ. 2014;14(1):219.
Batt-Rawden SA, Chisolm MS, Anton B, Flickinger TE. Teaching empathy to medical students: an updated, systematic review. Acad Med. 2013;88(8):1171–7.
Hojat M, Axelrod D, Spandorfer J, Mangione S. Enhancing and sustaining empathy in medical students. Med Teach. 2013;35(12):996–1001.
Stepien KA, Baernstein A. Educating for empathy. J Gen Intern Med. 2006;21(5):524–30.
Chen I, Forbes C. Reflective writing and its impact on empathy in medical education: systematic review. J Educ Eval Health Prof. 2014;11.
Koblar S, Cranwell M, Koblar S, Carnell B, Galletly C. Developing empathy: does experience through simulation improve medical-student empathy? Med Sci Educ. 2018;28(1):31–6.
Shapiro J, Youm J, Kheriaty A, Pham T, Chen Y, Clayma R. The human kindness curriculum: an innovative preclinical initiative to highlight kindness and empathy in medicine. Educ Health. 2019;32(2):53.
Streit-Forest U. Differences in empathy: a preliminary analysis. Acad Med. 1982;57(1):65–7.
Kupfer DJ, Drew FL, Curtis EK, Rubinstein DN. Personality style and empathy in medical students. J Med Educ. 1978;53(6):507–9.
Acknowledgments
The authors wish to thank Dr. Karen Lichty, Dr. Michael Lynn, the University of South Carolina School of Medicine Greenville, the participating members of the class of 2022, and the Meet the Patients participants and their accompanying family members and caregivers.
Funding
This study was funded by the University of South Carolina School of Medicine Greenville.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Dr. Lauren A. Fowler and Catherine Eve Tisdale. The first draft of the manuscript was written by Catherine Eve Tisdale. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
Ethical approval was granted for this study by the Institutional Review Board of the University of South Carolina in February of 2019 (PRO 00086527).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent to Publish
The authors affirm that human research participants provided informed consent regarding submission of the research report to the journal.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tisdale, C.E., Black, A.C., Jain, S. et al. The Impact of Meeting Patients with Neurological Disorders on Medical Student Empathy. Med.Sci.Educ. 30, 1561–1568 (2020). https://doi.org/10.1007/s40670-020-01102-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-020-01102-z