Abstract
Objective
Determine and describe the impact of student/student mentoring (SSM) on the senior medical student mentor involved in a formal SSM program.
Method
An anonymous online survey was administered to fourth-year medical students at the University of North Carolina with questions regarding participation in SSM programs (formal and informal) as well as the impact of these experiences. Responses from fourth-year mentors were compared to non-mentors’ answers. Data was analyzed to assess the value of, understand motivations for not participating in, and to describe perceptions regarding SSM.
Results
One hundred seven of 178 students in the fourth-year class completed the survey, a 60% response rate. Forty-two students participated in the formal SSM program, 48 did not have mentors (non-mentors), and 17 were excluded as they participated in informal mentoring programs. There were no differences in gender, age, or matched specialty between mentors and non-mentors. Ninety-five percent of all students agreed that SSM was valuable in a way that was different from student/resident or student/faculty mentoring. Mentors were nearly twice as non-mentors likely to believe that being the mentee in an SSM relationship would be beneficial. In addition, mentors were 4 times more likely to believe that being a mentor in an SSM program was valuable and 83% stated they would mentor again. Lastly, nearly three quarters of mentors felt that this was a worthwhile experience.
Conclusions
Students who served as mentors as part of an SSM program had positive experiences and found it a valuable addition to traditional faculty/student mentoring.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The concept of mentorship is not a recent phenomenon and may even be traceable back to Greek Mythology where the word “mentor” came into existence with the story of Odysseus and his entrusted friend, Mentor, who helped him prepare for the Trojan War [1]. Thus, Webster’s dictionary defines a mentor as a trusted counselor or guide [2]. Similar to Mentor for Odysseus, the value and benefits of mentoring, to both mentor and mentee, have long been accepted [3]. Undergraduate academic mentoring has been shown to help the mentee focus on individual growth and accomplishment, noted to encompass broad forms of support including career development, role modeling, and psychological support, and has been found to be beneficial for both the mentee and the mentor [4]. Furthermore, mentoring is effective at promoting job satisfaction, increasing the rate of promotion in the work setting, and increasing the number of academic publications [5,6,7]. Mentoring also helps to promote leadership development and overall encourages academic success particularly in cases where students are at a risk for failure or dropping out [5,6,7].
Since the 1990s, various medical professions began introducing formal mentoring programs between students and faculty and later between students and their peers [8]. A study looking at the correlation between peer mentorship programs and the retention of nursing students found that mentoring yielded benefits not only for the student receiving help, but also for the student who provided help, i.e., the mentor [9]. The University of North Carolina School of Medicine (UNC SOM) established its first formal student/student mentoring program, The Cicerone Mentor Program (CMP) in the summer of 2015. Two goals were identified at the onset of the program: (1) provide students in the preclinical years with peer mentorship from upper-level medical students and (2) strengthen the sense of unity between classes and in the school as a whole. Other students/student mentoring opportunities are also available at UNC School of Medicine such as interest groups and specialty-specific pairs. However, CMP is UNC SOM’s only mentoring opportunity in which the mentors are formally paired with their mentees. Formal mentoring pairings are defined as programs that formally and thoughtfully assign the mentor to the mentee, in lieu of a mentee picking a mentor of his/her free choice or vice versa. However, despite data in the nursing field, very little data exist in the field of medicine in regard to how medical students actually perceive student to student mentoring and if they find it beneficial, whether as a mentee or a mentor. The objective of this study was to describe the impact of student/student mentoring on the mentor, the senior medical student.
Methods
After obtaining an exemption from the Institutional Review Board, subject matter experts (SOM professors with additional degrees in education, SOM student advisors, and medical students with experience as CMP mentors) developed an anonymous online survey using Qualtrics (Qualtrics, Provo, UT). The survey was reviewed for clarity by CMP leadership. Next, the survey was piloted with a small group of students; their feedback was incorporated. Questions included topics regarding participation in informal student/student mentoring groups/programs and CMP, as well as the impact of these groups and demographic data. The survey was emailed out to the graduating fourth-year medical students in June of 2016. Two reminder emails were sent at 24 h and 1 week.
Respondents were sorted based on involvement in mentoring. Respondents who participated in the CMP were specifically compared to those who did not participate in any form of student/student mentoring (SSM). A second purely descriptive analysis was performed; this one only including those students who did not participate in any mentoring. The goal of this analysis was to better understand motivations for not participating in a formal SSM program. Then, a final analysis was performed including only Cicerone students to assess perceptions those students had regarding the experience of SSM. In each of these analyses, the relationship of age, gender, and medical vs surgical specialty were assessed. In the “Results” section and the table, the term “Agree” includes all students answering affirmatively to the prompt, specifically those who selected agree and those who selected strongly agree. Surgical specialties were defined as General Surgery, Obstetrics and Gynecology (OB/GYN), Emergency Medicine (EM), Orthopedics, Urology, and Anesthesia. Medical specialties were defined as Internal Medicine, Pediatrics, Radiology, Neurology, Pathology, Psychiatry, Family Medicine, Medicine-Pediatrics, and Radiology Oncology. Older age was defined as age greater than 27 years old, and this was the 75% for the respondent population.
Simple statistics were used to analyze the data, Fishers exact and chi-squares for categorical variables, and t tests and Kruskal-Wallis for continuous variables. In cases where comparisons were not performed, means with standard deviations and medians with interquartile ranges were calculated. The analysis was performed using Stata software (version 13; Stata Corporation, College Station, TX, USA). A p value of less than 0.05 was considered significant. Free-text responses were also obtained. Given the low number of free-text responses, formal qualitative analysis was not performed. Alternatively, demonstrative examples of student comments were cited in the text directly.
Results
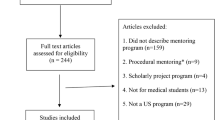
The response rate for the survey was 60% (107/178). There were 42 students participated in the Cicerone program; 48 were non-mentors (Fig. 1). Of note, the Cicerone program had 77 participating fourth-year students; thus, 55% of Cicerone participants completed the survey. No differences in gender, age, or matched specialty between mentors and non-mentors were found (Table 1).
Regarding non-mentor rationale, students cited not knowing about the program as the most common reason for not participating (69%) and the most important reason (71%). However, “not having time” (26%) and “not believing it was useful” (23%) were also common responses. There were no differences in the rationale for not participating by age or by specialty. However, men were more likely than women to cite non-participation due to “not knowing about the program” as well as because they “did not believe it would be useful” (p = 0.03 and p = 0.02, respectively, Table 2).
When asked hypothetically, if they would join was a mentee, 83% CMP students but only 24% of non-CMP students said yes. Similarly, when asked hypothetically if they would join again as a mentor, CMP students were twice as likely to say yes (88% vs 47%)(Table 3). These trends were more pronounced among male students (79% vs 14%, p < 0.01 and 87% vs 41%, p < 0.01 rejoining as a mentee and mentor, respectively). These differences were not seen among women. Although more than 90% of all students agreed that SSM is different from student/resident or student/faculty mentoring, CMP mentors were significantly more likely to strongly agree with these statements (Table 3). Cicerone mentors were almost twice as likely to believe that being the mentee in an SSM relationship was beneficial in medical school and 4.5 times as likely to strongly believe this (Table 3).
Nearly 75% of CMP mentors felt that this was a worthwhile experience. Among participants in CMP, older students less likely to find it useful than younger students (50% vs 84%, p = 0.03). There were no differences in perceived utility by gender or specialty. Career choice was discussed by 33 (79%) pairs, and 17 (42%) mentors felt more positively about their career choice as a result of SSM. Many fourth-year CMP mentors strongly valued the program’s goals and thoroughly enjoyed being a part of the program. One mentor stated, “I discovered that I liked being a mentor more than anticipated and I want to continue to do this in residency and beyond.” Almost 80% of CMP mentors talked about career choice and medical specialties with their mentees, despite many of their mentees being undecided on their own career choice. For example, in the free response section, one mentor commented, “I think [discussing it] made me more excited about the choice that I made and reaffirmed why I chose that path.” CMP was even talked about during residency interviews with one mentor stating, “[CMP] further strengthened by the desire to work [with] students in the future.” Finally, one student wrote, “[I] discovered that I liked being a mentor more than anticipated, want to continue to do this in residency and beyond.”
Discussion
In this study, we found that fourth-year students who served as mentors to other students were impacted in a positive way by this experience. This group believed much more so than non-mentors that SSM was important for medical students. Participants also described a unique value to this relationship that was different from the value gained in having a faculty mentor or a resident mentor. Not only was this group more likely to mentor again compared to non-mentors, they also recognized the importance of the mentoring relationship with the mentee. They also described a stronger desire to be a mentee if they had the opportunity earlier in their medical school career.
The literature has shown that mentoring relationships are reciprocal and beneficial, not only to the mentee, but also to the mentor [4]. From a faculty perspective, the benefits of being a mentor include increasing his/her professional recognition and accelerated productivity [10, 11]. In the opinions of resident mentors, many find mentoring rewarding and it helps their skills as resident teachers [12]. Our study brings light to that serving as a student mentor in a student/student mentorship program is similarly valuable and may be helpful in shaping a student’s medical school career. Though the numbers are small, there is a suggestion from our data that serving as a student mentor may inspire individuals who would not have otherwise mentored to participate in mentoring at higher levels as they progress in their careers.
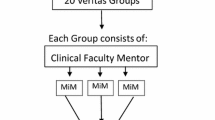
The Cicerone Mentor Program is a unique way to implement formal student/student mentoring into a medical institution. Many medical schools have informal student/student mentoring. In this style of mentoring, friends often discuss components of education and share tips for success. Informal mentoring, though important, may not link students by career goal, life plan, or common interests. However, intentional and thoughtful formal pairing connects students who may not have otherwise have known each other in a valuable and meaningful way. By pairing students based on shared interests and goals, the CMP created a safe space for students to ask difficult career or personal questions they may not have felt comfortable asking residents or faculty members. Another unique aspect of CMP is that fourth-year students are paired with second-year students and third-year students are paired with first-year students. This helped to bridge the gap between clinical and preclinical students. The feedback from participants illustrated the fact that students typically know other students from the class below and above them, but not those 2 years above or 2 years below. This program helped bridge that unfamiliarity and built relationships that may not have had the opportunity to form otherwise.
This study has some unique aspects. There is a lot of literature on mentoring in general as well as some data on student/student mental health counseling [13]. However, the data regarding the value of student/student mentoring is sparse. Thus, specifically looking at the impact on the mentor is somewhat novel. By using an anonymous and electronic application to disperse our survey, we hoped to minimize bias and ensure that students felt comfortable answering honestly. Qualtrics also has a very easy smartphone view, making quick survey completion easier for respondents as well. We also deployed our survey after fourth-year students had career plans set, again to attempt to optimize student response and minimize bias. However, our study is not without limitations. Because we deployed the survey late in the students’ fourth year, we did have a low response rate and were at risk for recall bias. Additionally, we did not survey the mentees, although the objective in this study was to focus on the mentor experience. Our survey also did not ask specifics as to why peer to peer mentoring was different from other kinds of mentoring. This sort of qualitative data would be helpful in future studies to better understand the reason for the positive impact on peer to peer mentoring. Because CMP is a newer program, this class of mentors was not mentees first. It is hard to assess the impact this had on their skill, experience, and opinions regarding being a mentor. Another weakness of this study was the lack of a validated survey instrument. Though, the survey was reviewed, piloted, and edited for clarity prior to deployment in an attempt to mitigate the risk for bias as much as possible. As this is a relatively new program, the number of participants was also lower in this class than in upcoming classes, which could increase the chance of type 2 error.
The graduating fourth-year students had a positive experience with their peer mentorship and, when compared to non-mentors, found a unique value in student/student mentoring over traditional faculty or attending/student mentoring and resident/student mentoring. Many stated that this experience increased their likelihood to mentor in the future. Future studies are needed to better quantify the value of this relationship and to better understand the impact from the mentee perspective. Because the fourth-year students who participated as a mentor in student/student mentoring programs had an overwhelmingly positive experience, they may be more likely to mentor again as their careers in medicine progress.
References
Crisp GCI. Mentoring college students: a critical review of the literature between 1990 and 2007. Res High Educ. 2009;50(6):525–45. https://doi.org/10.1007/s11162-009-9130-2.
Merriam-Webster Inc. Merriam-Webster’s dictionary of law. Springfield. Massachusetts: Merriam-Webster, Incorporated; 2016.
Cohen NH. Development and validation of the principles of adult mentoring for faculty mentors in higher education [dissertation]. Philadelphia: Temple University; 1993.
Jacobi M. Mentoring and undergraduate academic success: a literature review. Rev Educ Res. 1991;61(4):505–32.
Allard WG, Dodd JM, Peralez E. Keeping LD students in college. Acad Ther. 1987;22(4):359–65.
Fagenson EA. The mentor advantage: perceived career/job experiences of Protégés Versus Non-protégés. J Organ Behav. 1989;10(4):309–20.
Evans NJ, Bourassa DM, Woolbright C. Working with young undergraduate women. New Dir Stud Serv. 1985;1985(29):45–9.
Frei E, Stamm M, Buddeberg-Fischer B. Mentoring programs for medical students--a review of the PubMed literature 2000–2008. BMC Med Educ. 2010;10:32. https://doi.org/10.1186/1472-6920-10-32.
Jacobs S, Atack L, Ng S, Haghiri-Vijeh R, Dell’Elce C. A peer mentorship program boosts student retention. Nursing. 2015;45(9):19–22. https://doi.org/10.1097/01.NURSE.0000470424.40180.a0.
Garmel GM. Mentoring medical students in academic emergency medicine. Acad Emerg Med. 2004;11(12):1351–7. https://doi.org/10.1197/j.aem.2004.06.013.
Keyser DJ, Lakoski JM, Lara-Cinisomo S, Schultz DJ, Williams VL, Zellers DF, et al. Advancing institutional efforts to support research mentorship: a conceptual framework and self-assessment tool. Acad Med. 2008;83(3):217–25. https://doi.org/10.1097/ACM.0b13e318163700a.
Isenberg-Grzeda E, Weiss A, Blackmore MA, Shen MJ, Abrams MS, Woesner ME. A survey of American and Canadian psychiatry residents on their training, teaching practices, and attitudes toward teaching. Acad Psychiatry. 2016;40(5):812–5. https://doi.org/10.1007/s40596-016-0491-5.
Lau KS, Siong KH, Tang HY, Cheng PW, Cheung KS, Chan SW, et al. An innovative web-based peer support system for medical students in Hong Kong. Med Teach. 2007;29(9):984–6. https://doi.org/10.1080/01421590701551748.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by the University of North Carolina IRB committee.
Informed Consent
A statement of informed consent was sent with the survey link, and consent was implied by completion of the survey. The survey was anonymous.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous Presentations
Breakout Presentation at the 2017 CREOG & APGO Annual Meeting in Orlando, Florida.
Electronic Supplementary Material
ESM 1
(XLSX 28 kb)
Rights and permissions
About this article
Cite this article
Fleischman, A., Plattner, A., Lee, J. et al. Insights into the Value of Student/Student Mentoring from the Mentor’s Perspective. Med.Sci.Educ. 29, 691–696 (2019). https://doi.org/10.1007/s40670-019-00739-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-019-00739-9