Abstract
We designed a curriculum to help sustain pre-clinical knowledge for MD/PhD trainees in their graduate training phase while securing regular providers for our student-run free clinic. MD/PhD involvement increased from 1.91 to 2.45 students-per-clinic-day following implementation, and participants affirmed increased preparedness and comfort entering medical school clinical clerkships.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Following two years of pre-clinical curriculum, MD/PhD dual-degree trainees experience limited structured clinical exposure during graduate training (~ 3–5 years) prior to resuming the final two years of clinical training. This inherently disjointed curriculum contributes to poor self-perceptions of clinical capabilities relative to medical school colleagues [1, 2].
Student-run free clinics offer interactive platforms for students to hone clinical skills [3]. The East Harlem Health Outreach Partnership (EHHOP) is a medical student-run, attending-supervised, free clinic at the Icahn School of Medicine at Mount Sinai. The clinic’s mission is to provide health care to uninsured East Harlem residents and enhance knowledge, skills, and behaviors of trainee providers. EHHOP operates weekly and relies on continued recruitment of students to serve as primary care providers. As most qualifying students (those who have completed their second year of medical school) are often occupied with clinical clerkship obligations, MD/PhD trainees in the graduate school phase offer an invaluable pool of reliable providers with more accommodating schedules.
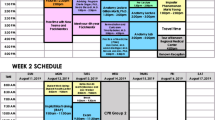
The EHHOP Physician-Scientist Track was established in 2014 to capitalize on this opportunity to augment clinic volunteer participation while increasing MD/PhD students’ comfort and preparedness for medical school clinical clerkships through hands-on exposure in a clinic setting. The curriculum is adapted annually based on the expressed needs of current students and is spearheaded by a senior MD/PhD student. Students must volunteer ≥ 4 times annually and attend monthly student-led didactic sessions facilitated by faculty or residents. These didactics review physiology, pathophysiology, history-taking, and physical exam skills learned in the first two years of medical school, and incorporate discussion of high-yield medical management through multiple choice examination questions in preparation for third-year shelf exams—a known area of difficulty for MD/PhD students [3].
Nineteen (out of 63 eligible students) who participated in the course for ≥ 1 year between 2014 and 2017 answered a survey to gauge program effectiveness (25 students participated since 2014, but 6 have since graduated). Each student participated for 1.92 ± 0.68 (mean ± SD) years; 12–14 were enrolled annually. Since the program began, 28.6% of participating students in clinic were MD/PhDs (~ 2.16/7.56 clinicians per clinic day). Students volunteered for an average 3.16 clinic days per year (range 1–8; ≥ 2 patients seen per day). Participants (7/19) also served in other EHHOP teaching, research, and leadership roles in the future. A summary of survey responses is presented in Table 1.
To our knowledge, this is the only MD/PhD-specific clinical program conducted in the context of a student-run clinic. This spaced, longitudinal volunteering, combined with didactic sessions, sufficiently helped students feel more prepared and comfortable entering their clinical years without being cumbersome alongside their research responsibilities. Notably, MD/PhD participation spiked on weekends coincident with clerkship shelf exams preoccupying their medical school colleagues, showcasing the implications of this recruitment strategy for sustainable clinic function. Finally, the resulting increase in MD/PhD interest and participation in additional clinic roles provided important institutional memory for an endeavor where a majority of student volunteers turnover annually. In conclusion, our curriculum affords mutual long-term benefits for both MD/PhD trainees and the student-run free clinic.
References
Goldberg C, Insel PA. Preparing MD-PhD students for clinical rotations: navigating the interface between PhD and MD training. Acad Med. 2013;88:745–7.
Raat ANJ, Kuks JBM, van Hell EA, Cohen-Schotanus J. Peer influence on students’ estimates of performance: social comparison in clinical rotations. Med Educ. 2013;47:190–7.
Swartz TH, Lin JJ. A clinical refresher course for medical scientist trainees. Med Teacher. 2014;36:475–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval/Informed Consent
This study was determined to be exempt by the IRB at the Mount Sinai Hospital in New York, NY, as it was an assessment of an ongoing educational curriculum.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Laitman, B.M., Chandrasekaran, S., Rifkin, R. et al. Benefits of a Physician-Scientist-Tailored Curriculum at a Medical Student-Run Free Clinic. Med.Sci.Educ. 29, 9–10 (2019). https://doi.org/10.1007/s40670-018-00668-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-018-00668-z