Abstract
Case-based tutorials (CBTs), in medical education, promote an in-depth understanding of knowledge acquired through lectures, in an inquiry-based manner to correlate basic science with clinical problems. Due to the intensive demands of resources in problem-based learning (PBL), there is a growing interest in reviving CBT as an alternative pedagogical approach of active learning. Case-based tutorials are less prone to group dysfunction and are easier to implement than PBL and team-based learning. Despite these advantages, there are some challenges faced in CBTs. However, few studies have described strategies that could be used by tutors to overcome those challenges. The strategies provided in this article and a working example of a specific patient case scenario should help tutors make CBTs productive learning events. This article may be useful for faculty development, especially for teaching assistants, and inexperienced faculty to create similar CBTs, linking basic science concepts to clinical problems and practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There are several formats of teaching and learning in medical education including didactic lecture, case-method teaching (CMT), case-based tutorial (CBT), problem-based learning (PBL), and team-based learning (TBL) [1]. Among these formats, case-based teaching is the oldest form of interactive teaching in medical education, which was first demonstrated to have distinct advantages over the traditional didactic lecture in the 1800s [2], well before the Flexner report [3]. Both CMT and CBT involve a teaching method of shared guidance between the teacher and students, which promote active learning, problem-solving skills, and professional competencies [4,5,6]. In medical education, CMT and CBT use inquiry-based learning for students to apply basic science concepts to solve clinical problems. However, whereas CMT can accommodate large participant group sizes, with longer class sections, CBT usually allows for a smaller group of participants [7,8,9,10].
Although case-based studies were introduced in the 1800s [2], PBL has been the most popular pedagogical approach in curricula renewal [11, 12]. This popularity is driven by the move toward active and lifelong learning, and professional competencies [13,14,15,16]. However, the resource-intensive demands posed by PBL on curriculum development are a matter of concern [7, 17,18,19]. Moreover, several studies have found no significant difference between PBL and traditional learning in terms of students’ acquisition of knowledge and performance [20]. These shortcomings of PBL have led to medical educators adopting alternative student-centered pedagogical approaches such as CBL and TBL [21,22,23], which require less institutional resources [4,5,6]. Nevertheless, there are some common challenges to overcome by tutors to successfully facilitate CBTs, such as writing multiple cases and passive student participation [7, 24]. Although there is enough information on strategies for successful delivery of PBL [19, 25] and TBL [26, 27], very little is known about practical strategies for successful delivery of CBTs. Here, we describe practical strategies, which are based on sound educational theories and research, and the authors’ teaching experiences, to address these challenges. These strategies may be useful for faculty development, especially for inexperienced faculty and graduate teaching assistants. Several teaching tasks are important components for successful CBTs:
Task 1: Pre-session Planning
Generally, there are challenges and anxiety for both students and tutors during tutorials. This is especially true for new faculty facilitating tutorials as their first teaching experience, and also for first year students. These challenges are, in part, due to uncertainty about tutors’ role and performance [19, 25], whereas students are unsure about their expectations, performance, and behavior [28, 29]. There are several steps in the pre-planning stage.
Step 1: Scheduling
Sequencing of tutorials and recruitment of tutors are among the most important activities to consider when setting up the timetable for CBTs. Since CBTs foster a deeper understanding of the basic science concepts, it is important for them to follow the lectures. This sequential arrangement minimizes the chances of turning tutorials into mini-lectures. When recruiting tutors, it is important to realize that effective CBTs depend on subject-matter expertise and facilitation skills. If possible, efforts should be made not to recruit tutors for a tutorial session only. This use of “drop-in tutors” makes it difficult for relationship to flourish between students and tutors. A positive relationship between tutor and students is best served by assigning a tutor to the same tutorial group [19, 30].
Step 2: Orientation
Students will have positive learning experiences if they are familiar with the purpose and guidelines of the tutorials, and what is expected of their behavior and attitude for a successful tutorial. It is also important for faculty, especially new and inexperienced faculty, to know their role as tutors [7, 9, 19, 29]. Orientation gives both faculty and students the opportunity to share their concerns and opinions on the, purpose, ground rules, regulations, and their expectation, of the tutorials:
Purpose
The purpose of a CBT in medical education is to give students the chance to gain an in-depth understanding of the clinical relevance of biomedical knowledge, and to acquire professional skills. They achieve these goals by:
-
Applying concepts and theories
-
Synthesizing ideas
-
Engaging in critical thinking
-
Gaining effective communication skills
-
Cooperating with other students
-
Self-regulated learning
-
Gaining skills in team work
Ground Rules
They are rules that students should abide by for effective group participation. However, students and tutors might add their own rules upon prior agreement. Some of the rules are:
-
Students must come prepared for the tutorials
-
Students should actively participate
-
Attendance is compulsory and will be rewarded
-
Distracting behavior is unacceptable
-
Students must respect other students
-
Tutorials are examinable
Step 3: Students’ Expectation and Tutor’s Role
Students’ Expectation
Students are expected to contribute to the success of the tutorials by actively engaging in the discussion, where they learn problem-solving skills. They should remember that the success of the tutorial depends on them and the group effort. They can achieve these goals by:
Preparing for the Tutorial
-
Students should prepare well in advance
-
Students should attempt all the questions
-
The group should appoint a timekeeper and a scribe. The scribe should record the answers and other important information for the class.
Participating in the Tutorials
-
Explaining their ideas through examples
-
Making positive comments
-
Debating constructively
-
Asking questions when in doubt
-
Learning from other students
-
Valuing everyone’s opinion
Tutor’s Role
In contrast to PBL, the tutor in CBTs is expected to be a subject-matter expert [7]. The tutor can effectively facilitate the tutorial discussion by:
-
Motivating the students
-
Activating students’ prior knowledge
-
Skillful questioning
-
Providing feedback
-
Creating a positive learning environment
-
Identifying and correcting gaps, and misconceptions in students’ knowledge
-
Accepting that the tutor and student can have different perspectives
Task 2: Lesson Planning
Effective design of a lesson plan for a CBT is influenced by several factors including the learning objectives, quality of the case narrative, and the tension between time and coverage of content [31,32,33]. Therefore, it is important to devote considerable effort to carefully design the lesson plan.
Step 1: Learning Objectives
The lesson plan begins with the learning objectives that determine what the students should know, and defines the content. In order to alleviate the pressure to cover the content on time, it is imperative to limit the content to a few concepts. The authors find that three main concepts can just be covered in a typical 50-min session.
The Learning Objectives should Help Pre-clerkship Students to:
-
Have a deep understanding of the basic concepts
-
Have an appreciation of an authentic clinical problem
-
Understand the relevance of basic science knowledge in understanding disease mechanisms
-
Extend their basic science knowledge to analyze patients’ data
-
Develop the ability to critically appraise biomedical literature
The Learning Objectives Should Help Clerkship Students to:
-
Apply their pre-clerkship knowledge to identify the interrelationships between the primary and secondary causes of diseases
-
Have a deep understanding of the link between the primary and secondary causes of diseases
-
Make a differential diagnosis
-
Make a prognosis and treatment or management plan
-
Develop the ability to critically appraise the literature on clinical problems and management
Step 2: Constructing Cases
The effectiveness of a CBT is dependent, to a large extent, on the quality of the case narrative [31, 32]. A good quality narrative should stimulate interest in the case, and covers the learning objectives. The case narratives in pre-clerkship should involve clinical problems, although students are unfamiliar with patients. In clerkship, designing a clinical case is much easier, because students are familiar with patients’ clinical records. In contrast to pre-clerkship, the cases can be complex and open-ended. There are general principles that can be applied to design effective cases including activation of prior knowledge, promotion of professionalism, and integration of knowledge [33].
Framework of How to Construct a Case Scenario
When developing a CBT, it is best to use a curricular framework that reflects the scientific process. One such framework is the backward design model [34]. The backward design involves these steps:
-
1.
Identify the basic science and clinical themes
-
2.
Determine the learning objectives and assessment format
-
3.
Select a real-life medical situation
-
4.
Plan the learning activities
-
5.
Get feedback and revise accordingly
Working Example of How to Construct a Specific Patient Case Scenario
As an essential first step, tutors need to identify the basic science theme, concepts and clinical problem they want their students to know, and work back from there to create a realistic patient scenario. For this working example, the themes are “Disorders of Hydrogen ion Homeostasis” and “Aortic Aneurysm.” These themes are covered under the popular topics of “Acid-base Imbalance and Control” and the pathophysiology of “Diseases of the Aorta.” Once the themes have been selected, the title, aim, learning objectives and activities, and assessment can be determined:
Title: “Acid-base Imbalance and Control.”
Aim
The purpose of this tutorial is for the students to apply the concepts of the homeostatic mechanisms of acidosis and alkalosis to clinical problems and practice.
Learning Objectives
-
1.
Describe the causes of metabolic acid-base disorders
-
2.
Identify the underlying mechanisms of metabolic acid-base disorders
-
3.
Explain the compensatory mechanisms to metabolic acid-base disorders
-
4.
Describe how clinical problems are associated with metabolic acid-base disorders
-
5.
Compare and contrast the clinical consequences of metabolic acid-base disorders
Now that the learning objectives have been identified, they will guide the design of the case scenario and the determination of the type of clinical and laboratory test data:
Specific Patient Case Scenario
A 67-year-old lawyer (height 169 cm; weight 73 kg) was admitted to the hospital with back pain, severe abdominal pain, and lower limb weakness. He had no history of gastrointestinal referral, chest pain, or hemoptysis, and the abdominal pain had begun 3 h earlier. He was in shock and had a large, stiff abdomen; his femoral pulses were hardly felt. CT scan confirmed a ruptured, 14-cm diameter abdominal aortic aneurysm. Analysis of arterial blood showed:
pH | 6.95 |
|---|---|
pCO2 | 3.8 kPa |
pO2 | 11.90 kPa |
\( \left[{\mathrm{HCO}}_3^{-}\right] \) | 7.48 mmol/L |
Anion gap | 23 mmol/L |
This case is designed for a 50-min session, which can be offered to first year students during an integrated “Foundation of Medicine” course at a medical school with a hybrid curriculum. Experienced tutors can facilitate the case. Each tutorial group could comprise of 10–12 students. This CBT shows that basic science concepts can be linked to a complex and real-life medical emergency. Students are given specific instructions for the preparatory work. They should receive the complete case with questions, and accompanying notes with references:
Questions
Careful consideration should be given to the selection of questions. Questions will help tutors to identify gaps in learning, guide the level of difficulty of the application of concepts, and integration of knowledge:
-
1.
What is the most likely acid-base disturbance in this case?
-
2.
What is the probable primary cause of this acid-base disturbance?
-
3.
What is the significance of the bicarbonate ion concentration?
-
4.
Why is it that an even lower partial pressure of carbon dioxide might have been expected, although this is not the case?
-
5.
What could be the effect of the ruptured abdominal aneurysm on the kidneys?
-
6.
What could be the effect of the ruptured abdominal aneurysm on the liver?
-
7.
What could be the effect of the ruptured abdominal aneurysm on the heart muscles?
The accompanying class notes and reference readings should cover the following topics:
-
Henderson Hasselbach equation
-
Bicarbonate, phosphate, and protein buffer systems
-
Metabolic acid-base disorders and their clinical effects
-
Anion gap
-
Respiratory acid-base disorders and their clinical effects
-
Role of the lungs, kidneys, and respiratory failure in acid-base disorders
-
Pulse oximetry
-
Pathobiology of aortic diseases
A sample of the recommended reading materials and references, and preparatory work for the specific patient case scenario are described below:
Required Readings
-
1.
Medical Sciences, Jeannette Naish and Court (2nd edition). “Chapter 1; Acid-Base Balance: homeostatic control of hydrogen ions”; pages 10–14
-
2.
Goldman’s Cecil Medicine (24th edition). “Chapter 78; Diseases of the Aorta”; pages 482–485
Preparatory Activities
The tutorial groups should be encouraged prior to the session to discuss the case and draw a concept map of how disorders in hydrogen ion homeostasis are linked to aortic aneurysm. This group discussion will help the students to answer the tutorial questions and to reduce their anxiety of participating in the tutorials. The tutors should discuss the case during a pre-tutorial meeting in anticipation of students’ responses. This meeting is also important for the tutors to decide to adopt similar strategies in guiding the discussion, and reaching consensus on the solutions to the tutorial questions. Such meetings can serve as a mentoring platform for tutors that are unfamiliar with the case, and to help reduce their level of anxiety in anticipation of the session.
Step 3: Reading and Supplemental Materials
The challenge of alleviating the tension between content coverage and time has been made more difficult in medical education by the reduction in basic science teaching in favor of professionalism. Nevertheless, this tension can be partly alleviated by providing supplemental materials to complement the tutorial notes. We find that for a 50-min session, five pages of notes, two required reference materials is not overbearing for the students. The reference material can also be a review article. Assigned reading materials such as referral to web pages, learning and teaching portals that have been proven effective [35] could be useful for CBTs.
Task 3: Preparing for Facilitation
Case-based tutorials require tutors with subject-matter expertise, as well as facilitation skills. This is in contrast to PBL where group facilitation skills are more important than subject-matter expertise [36,37,38]. Nevertheless, one of the main tasks for tutors is to effectively facilitate group discussions [7, 9]. Facilitation involves:
-
Step 1:
Organization of Learners
-
Become familiar with your tutorial group
-
Encourage your group to brainstorm
-
Encourage your group to share reference materials
-
Step 2:
Communication
-
Give students the option of submitting their answers well in advance of the sessions, giving you the opportunity to catch as many misconceptions and gaps in knowledge as possible.
-
Decide ahead of time (with students’ input) how the group is going to approach the case.
-
Give students the opportunity to submit questions, in context of the case, that they would like addressed.
-
Step 3:
Revision of notes and handouts
-
Make sure your audiovisual aids are legible.
-
Revise your handouts to make last minute corrections or changes, and repost.
-
Prepare practice questions.
Task 4: Facilitation Skills
The tutors have to lead the discussions by encouraging the students to participate, to share their perspectives, and to reach a common consensus. The tutors, who are familiar with the students’ prior knowledge and learning, are in a better position to guide the discussions and to enhance deep learning. They should allow the students to elaborate on their knowledge, synthesize new knowledge, and critically appraise the sources of information. Numerous skills are involved in making small group learning a positive experience for students [39, 40]. The important skills are:
-
Starting the session by creating a non-threatening atmosphere
-
Motivating students
-
Creating a positive and safe learning environment
-
Practicing effective communication
-
Maximizing the breadth and depth of learning
-
Encouraging deep learning
Working Example of How to Facilitate the Specific Patient Case Study
To demonstrate how the “Acid-base Imbalance and Control” tutorial is discussed, a working example is described:
Preamble
The tutorial is about a patient diagnosed with a ruptured abdominal aortic aneurysm and metabolic acidosis. The discussion is guided to emphasize the underlying mechanisms of acid-base disorders associated with this rupture, and the clinical consequences due to the loss of blood from the aneurysm. These consequences include impaired tissue perfusion, inadequate oxygenation (despite the normal partial pressure of oxygen), increased anaerobic metabolism of glucose to lactic acid, and possible compromise in renal, liver, and muscle functions. The case presented an opportunity to examine other causes of lactic acidosis, to review the Cori cycle and diagnostic imaging. The cognitive domain of learning model [41] can be applied to guide the discussion of this tutorial. This model (Fig. 1) has several levels of learning, progressing from surface learning to deep learning, which can guide the case discussion through skillful questioning by using the tutorial questions to identify the clinical problems and their underlying mechanisms, and to eventually determine diagnostic, treatment, and prognostic options.
Flow chart of case discussions, from surface to higher-level learning: adapted from reference [41]
Knowledge and comprehension: gathering information about the relevant clinical issues and test data; and understanding of the broad context of the case.
The session starts with a student reading the case aloud, giving time for the students to settle in. The tutor engages the students to ascertain that they understand the terminology in the context of the case, such as the definition of hemoptysis, aneurysm, and palpable pulse. It is difficult to see how the students can begin to analyze the case without outlining the specific facts of the case including the clinical problems. Thus, at these levels of learning, the students should summarize the relevant information of the patient’s history, physical examination, clinical problems, and laboratory test data. They should analyze the test results to identify normal and abnormal values. So far, the discussion has addressed the general knowledge of the students of the case and their ability to understand the meaning of the data. A representative summary of the patient’s information can be divided into clinical and laboratory test data (Tables 1, 2).
Application and analysis: connecting the patient’s history, physical examination, clinical consequences to the primary diagnosis; connecting the laboratory test results to the underlying primary mechanisms of the acid-base disorders.
After identifying the clinical problems and abnormal test results, the discussion focuses on establishing interrelationships between the clinical problem and its consequences (Fig. 2a), and applying the concepts of hydrogen ion homeostasis to the primary mechanisms underlying the acid-base disorders (Fig. 2b). At this stage, students are also encouraged to hypothesize so that different perspectives on the case can flourish toward preliminary decisions. The tutors guide the discussion through skillful questioning using trigger and probing questions, and providing “prompts.”
Trigger questions are used to stimulate discussion of a broad knowledge of concepts and topics, without focusing on in-depth knowledge, which are suggestive of relationships, or underlying mechanisms. For example, the following tutorial questions were used as trigger questions:
-
What is the most likely acid-base disturbance in this case?
-
What is the probable primary cause of this acid-base disturbance?
-
What is the significance of the bicarbonate ion concentration?
Probing questions, which are questions that follow trigger questions, focus on specific details. For example, after identifying that the most likely acid-base disturbance is metabolic acidosis (Fig. 2b), the following probing questions can be used:
-
What are the other causes of metabolic acidosis?
-
Why is the acid-base disorder non-respiratory in origin?
-
What triggers the compensatory response to the metabolic acidosis?
Prompts are comments that can act as clues to questions. They can be useful to guide students to extend their knowledge of concepts, or to elaborate on their answers. For example, here are prompts to one of the tutorial questions:
(Question #2): What is the probable primary cause of this acid-base disturbance?
Prompts
-
Inadequate oxygen to the tissues
-
Increased anaerobic metabolism of glucose
-
The Cori cycle
As the discussion progresses, interrelationships between the clinical data are easier to identify because the diagnosis (ruptured abdominal aortic aneurysm) is provided. So, the successive discussions are mainly to integrate the clinical problems with the test results and the underlying primary mechanisms. This case scenario is in contrast to a case where basic science concepts are applied to make diagnostic decisions. Establishing interrelationships between the laboratory test data separately from the interrelationships between the clinical data is appropriate at this stage of the curriculum for first year students. This is particularly important since the students are unfamiliar with CBTs, and they have yet to cover enough pathology. This format allows the tutor to assess the students’ level of understanding of the basic science concepts and underlying mechanisms of the clinical problems. It also allows the tutors to make necessary adjustments to the discussions that follow.
Synthesis and evaluation: interrelationships between the clinical problems and the underlying mechanisms of the acid-base disorders; interrelationships between the primary and secondary mechanisms underlying the acid-base disorders and their effects and interactions across the various organs, diagnosis, treatment, and prognosis.
So far, the discussion has yet to link the relevance of the basic sciences (i.e., concepts of acid-base disorders) directly to the clinical problem (ruptured aortic aneurysm and its consequences). Specifically, to demonstrate this relevance, the acid-base disorders and their underlying primary and secondary mechanisms are to be integrated with the consequences of the clinical problem (Fig. 3). For example, the metabolic acidosis and the possible impairment of kidney and liver functions are directly linked to the aortic aneurysm, through reduced tissue perfusion. Further, the underlying primary mechanisms (e.g., acidosis) could lead to secondary effects (e.g., hyperkalemia and neuromuscular irritability), which could lead to impairment of the functions of the various organs (e.g., cardiac arrest) (Fig. 3). These effects on the various organs are indirect consequences of the clinical problems.
The discussion to link the basic sciences to the clinical problems requires an approach to critical thinking, where the students should be guided to enhance their ability to make predictions and extrapolate data based on evidence, to generate new ideas, to criticize, and judge the value of the decisions and data. This approach to higher-level or deep learning is required to establish a differential diagnosis, albeit the diagnosis is confirmed as a ruptured aortic aneurysm. Critical thinking is also needed to devise treatment plans and make prognostic judgments. Tutors foster critical thinking by skillful questioning using higher-level questions that go beyond recollection of factual information. In this tutorial, the following specific questions were used to stimulate critical thinking and problem-solving skills:
-
Why is it that an even lower partial pressure of carbon dioxide might have been expected, although this is not the case?
-
What could be the effect of the ruptured abdominal aneurysm on the kidneys?
-
What could be the effect of the ruptured abdominal aneurysm on the liver?
-
What could be the effect of the ruptured abdominal aneurysm on the heart muscles?
These questions explore the effects of anaerobic metabolism of glucose (production of lactic acid) on abdominal muscles, kidneys, lungs, and liver. More in-depth consideration of specific details to link lactic acid production to cardiac failure are guided by probing questions such as:
-
What is the relationship between acidosis and potassium?
-
What is the effect of potassium on cardiac muscles?
-
What is the relationship between acidosis and neuromuscular activity?
Here are useful questions and their corresponding prompts:
Question: What is the relationship between acidosis and potassium?
Prompt: Hydrogen ion exchange between the ECF and ICF and potassium disorders (hypokalemia and hyperkalemia).
Question: What is the effect of potassium on cardiac muscles?
Prompt: Potassium and resting membrane potential of cells, relationship between resting membrane potential and muscle strength and weakness, typical ECG changes associated with hyperkalemia and hypokalemia.
Question: What is the relationship between acidosis and neuromuscular activity?
Prompt: Effects of acidosis on nerves and muscles.
The above-mentioned model for facilitating this session, which was based on the different levels of the cognitive learning domain, could be a strategy for the students to use as they subsequently engage in solving medical problems. The complete flow of the discussions of this tutorial (Fig. 4) illustrates the interrelationships between the ruptured aortic aneurysm, its consequences and the basic science concepts, underlying mechanisms of acid-base disorders, and their interaction across, and impact on, the liver, kidneys, heart, and brain.
Curricular Issues
The success of teaching CBTs also depends on where and when in the curriculum it is adopted. This adoption is even made more challenging when CBTs are used to integrate the basic sciences with longitudinal courses, such as evidence-based medicine, social and community sciences [42]. Thus, the issues of how many CBTs are offered and when, timelines for facilitating, and the length of, CBTs should be addressed.
Frequency and the Types of Tutorials
In a pre-clerkship, foundational curriculum with system-based blocks teaching that extends over 4 weeks, CBTs could be offered on a weekly basis. Due to the limitations of writing multiple cases, recruiting tutors, and curricular time, it is hard to visualize how CBTs can be offered on a daily basis. However, multiple case vignettes can be used as quizzes on a daily basis during lecture slots beyond the CBT sessions of the week. In addition, CBTs can be offered monthly to integrate the basic sciences with longitudinal courses including doctoring and health policies. In clinical curriculum, CBTs are being used to further integrate basic science knowledge into clinical teaching [43], where they can be offered as electives at the end of a clinical rotation, or weekly and monthly as seminars. Senior medical students present these seminars. In other formats, CBTs can be offered annually as “Bench to Bedside” teaching series to demonstrate how basic science research is translated into clinical practice.
Timelines for Facilitation
The steps taken in facilitating a CBT can be divided into the information gathering (Level I), hypothesizing and application of concepts (Level II), problem-solving and critical thinking (Level III) phases (Fig. 1). The duration of each level depends mainly on the learning objectives and how the case unfolds. From the authors’ experience, for a 50-min session during the first year of the pre-clerkship curriculum, 30 min is devoted to level II, and 10 min each to levels 1 and III. In the second year of the pre-clerkship curriculum, and for clerkship, 30 min could be devoted to level III, since at this stage students have had enough training in gathering information, hypothesizing and applying biomedical knowledge to clinical medicine. So, for them, making differential diagnosis, treatment and management decisions are important priorities.
Session Timelines
After adopting a CBT as a teaching format, the question invariably arises as to how long the sessions will last. The duration of a session for any CBT depends on several factors including the topics, learning objectives, and how the case is processed. Case-based tutorials can be processed in many different ways. The process defines the type of case scenario, which in turn, determines the duration of the session. Paper-based cases usually last for 50–60 min, if students are expected to review the case and complete the tutorial assignments in advance of the session [8]. However, other formats of CBTs that are paperless can last for more than 60 min depending on the learning activity. These types of CBTs usually link basic science concepts to clinical practice during the session. For example, a CBT that incorporates peer-to-peer interaction lasted 2 h [44]. These tutorials incorporate clinical skills including hands-on experience where the students take history and do a physical examination, and analyzed test data. These activities occur in real time, thus, students need enough time to carry out the tasks. Similarly, web-based tutorials with multiple case vignettes can last for more than 2 h [45].
Task 5: Assessment and Feedback
Learning involves not only cognition but also students sharing their experiences and socializing in a way that is productive [46, 47]. Therefore to assess students, we have to take into account all aspects of learning. Although examinations are important, we also have to value the efforts made by students in preparing for the tutorials, socializing in group studies, and participating and contributing to discussions by sharing and learning from their experiences. There are numerous small group assessment practices that could be useful for CBTs, such as tutors’, peers’, and self-assessments [48, 49].
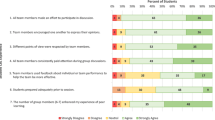
Feedback evaluations of the tutorials are important for tutors’ reflection on them, in order to improve the quality of the cases and their facilitation skills, which contribute to the positive learning experiences of students. The students should receive and provide feedback including feedback from their peers. There are several feedback methods that are appropriate for CBTs [50, 51] including:
-
1.
Curriculum evaluation seminar, where students’ representatives meet with the tutorial coordinator to discuss their concerns.
-
2.
Survey questionnaires for tutor’s subject-matter expertise and facilitation skills.
-
3.
Focus group interviews for the students to elaborate on the weaknesses and strengths of the tutorials.
-
4.
Direct observation of tutorial sessions by education specialists.
-
5.
Post-tutorial debriefing sessions for tutors, which are necessary to discuss their experience in the sessions, and to revise the case accordingly.
In Conclusion
Case-based tutorials promote active learning, deep learning [52], and engage students in acquiring professional skills. We have described practical strategies for tutors to effectively deliver CBTs. It is critical for them to follow the five essential tasks to guarantee the success of a session. However, there will always be challenges facing tutors, especially new and inexperienced faculty. Some of the challenges are the difficulty in writing multiple cases with good quality narratives that covers the learning objectives and professional competencies, and faculty development of tutors to improve their facilitation skills. Multidisciplinary and collaborative approaches among new and seasoned tutors could effectively address the difficulties encountered in constructing and renewing multiple cases. In addition, there is also a challenge to recruit tutors with the relevant subject-matter expertise and facilitation skills. Results from few studies that have examined how medical students evaluate basic science (PhD) and clinical faculty (MD) teaching PBL, showed that co-tutoring by basic science and clinical faculty improves students’ problem-solving skills [53]; basic science faculty felt more uncomfortable when the cases became more clinical [54]; and first and second year students rated basic science and clinical faculty equally, while second year students rated clinicians more highly overall [55]. Taken together, these studies open the possibility of enhancing CBTs by pairing basic scientists and clinicians, especially during clerkship where the cases are more clinically oriented.
The need for tutors to attain facilitation skills can be addressed in several ways including mentoring of junior faculty by senior tutors, effective faculty development workshops that take into consideration tutors’ needs, teaching context [56, 57], and feedback from peers and students [50, 51]. These strategies and others [29, 58, 59] are most likely to be effective in enhancing tutors’ attitude, skills, and performance, if they are followed by tutorial practice. Although, as mentioned above, CBTs and other forms of active learning are increasingly being adopted as alternative pedagogical approaches to PBL because of their distinct advantages, it may also be that their effectiveness are influenced by the learning objectives, curricular integration, and the teaching environment. Nevertheless, having CBT as an alternative approach to small group learning adds to the repertoire of teaching methods that are effective in the appropriate context. Thus, medical educators could use the strategies presented herein to improve small group teaching and learning.
References
Mourad A, Jurjus A, Hussein HI. The what or the how: a review of teaching tools and methods in medical education. Med Sci Educ. 2016;26(4):723–8.
Cannon WB. The case method of teaching systematic medicine. Boston Med Surg J. 1900;42(2):31–6.
Flexner A. Medical education in the United States and Canada: a report to the Carnegie Foundation for the Advancement of Teaching: Carnegie Foundation. 1910 (Bulletin No. 4).
Patil M, Karadesai S. Effectiveness of case-based tutorials as compared to traditional tutorials in microbiology. Natl J Integr Res Med. 2016;7(2):5–8.
Garvin DA. Making the case, professional education for the world of practice. Harv Mag. 2003;106(1):56–66.
Stjernquist M, Crang SE. Applying the case method for teaching within the health professions—teaching the students. Educ Health. 2007;20(1):15. Available from: http://www.educationforhealth.net
Tärnvik A. Revival of the case method: a way to retain student-centered learning in a post-PBL era. Med Teach. 2007;29(1):e32–6.
Dupuis RE, Persky AM. Use of case-based learning in a clinical pharmacokinetics course. Am J Pharm Educ. 2008;72(2):29.
Bowe CM, Voss J, Thomas AH. Case method teaching: an effective approach to integrate the basic and clinical sciences in the preclinical medical curriculum. Med Teach. 2009;31(9):834–41.
Thistlethwaite JE, et al. The effectiveness of case-based learning in health professions education. A BEME systematic review: BEME guide no. 23. Med Teach. 2012;34(6):e421–44.
Neufeld VR, Barrows HS. ‘The McMaster philosophy’: an approach to medical education. J Med Educ. 1974;49(11):1040–50.
Neville AJ. Problem-based learning and medical education forty years on. Med Princ Pract. 2009;18(1):1–9.
Steitz JA. Commentary: Bio2010—new challenges for biology educators. Cell Biol Educ. 2003;2(2):87–91.
Pratt DD, Arseneau R, Collins JB. Reconsidering ‘good teaching’ across the continuum of medical education. J Contin Educ Heal Prof. 2001;21(2):70–80.
Committee on the Engineer of 2020, Phase II. Educating the engineer of 2020: adapting engineering education to the new century. Washington DC: National Press Academy; 2005.
Koh GC. Revisiting the ‘essentials of problem-based learning’. Med Educ. 2016;50(6):596–9.
Taylor D, Miflin B. Problem-based learning: where are we now? Med Teach. 2008;30(8):743–8.
Dolmans D, et al. Should we choose between problem-based learning and team-based learning? No, combine the best of both worlds! Med Teach. 2015;37(4):354–9.
Azer SM. Challenges facing PBL tutors: 12 tips for successful group facilitation. Med Teach. 2005;27(8):676–81.
Colliver JA. Effectiveness of problem-based learning curricula: research and theory. Acad Med. 2000;75(3):259–66.
Ahmad KA, Malik FY, Hulbert JR. Student preference for case studies: enhanced learning in a human physiology course. Med Sci Educ. 2012;22(3):117–20.
Koles PG, et al. The impact of team-based learning on medical students’ academic performance. Acad Med. 2010;85(11):1739–45.
Thompson BM, et al. Team-based learning at ten medical schools: two years later. Med Educ. 2007;41(3):250–7.
Barrington D, Wing L, Latimer K, Alpers J, Prideaux D. Evaluation of a change from traditional case studies to patient-based, problem-based learning: a case study. Med Teach. 1997;19(2):104–7.
Lee G-H, Lin C-S, Lin Y-H. How experienced tutors facilitate tutorial dynamics in PBL groups. Med Teach. 2013;35(2):e935–42.
Hrynchak P, Batty H. The educational theory basis of team-based learning. Med Teach. 2012;34(10):796–801.
Kamei RK, Cook S, Puthucheary J, Starmer CK. 21st century learning in medicine: traditional teaching versus team-based learning. Med Sci Educ. 2012;22(2):57–64.
Steinert Y. Student perceptions of effective small group teaching. Med Educ. 2004;38(3):286–93.
Edmunds S, Brown G. Effective small group learning; AMEE guide no. 48. Med Teach. 2010;32(9):715–20.
Harden RM, Crosby J. AMEE guide no 20: the good teacher is more than a lecturer—the twelve roles of the teacher. Med Teach. 2000;22(4):334–7.
Herreid CF. What makes a good case? Some basic rules of good storytelling help teachers generate students’ excitement in the classroom. J Coll Sci Teach. 1997;27(1):163–5.
Jonassen DH, Hernandez-Serrano J. Case-based reasoning and instructional design: using stories to support problem solving. Educ Technol Res Dev. 2002;50(2):65–77.
Kim S, et al. A conceptual framework for developing teaching cases: a review and synthesis of the literature across disciplines. Med Educ. 2006;40(9):867–76.
Wiggins G, McTighe J. Understanding by design. 1st ed. Alexandria: Association for Supervision and Curriculum Development; 1998.
Mclean M. Web pages an effective method of providing CAI resource material in histology. Med Teach. 2001;23(3):263–9.
Hitchcock MA, Mylona ZE. Teaching faculty to conduct problem-based learning. Teach Learn Med. 2000;12(1):52–7.
Dalrymple KR, et al. PBL core skills faculty development workshop 1: an experiential exercise with PBL process. J Dent Educ. 2007;71(2):249–59.
Wuenschell CW, Dalrymple KR, Shuler CF. PBL core skills faculty development workshop 2: training faculty in group learning facilitation skills through role-modeling and role play activities. J Dent Educ. 2007;71(5):606–18.
Khalil MK, Elkhider AR, Ingiaimo M, Johnson TE. Utilization of team process framework to improve small-group learning in medical education. Med Sci Educ. 2017;27(1):123–34.
Jaques D. Teaching small groups. BMJ. 2003;326(7387):492–4.
Bloom BS, Krathwohl DR. Taxonomy of educational objectives: the classification of educational goals, by a committee of college and university examiners in handbook 1: cognitive domain. New York: Longmans; 1956.
Dolan BM, Goel MS, Jean-Jacques M, Persell SD. Development of a case-based learning curriculum to engage preclerkship students in principles of health equity, quality, safety, teamwork, and economics. Med Sci Educ. 2015;25(4):493–6.
Spencer AL, Brosenitsch T, Levine AS, Kanter SL. Back to the basic sciences: an innovative approach to teaching senior medical students how best to integrate basic science and clinical medicine. Acad Med. 2008;83(7):662–9.
Hudson JN, Buckley P, McMillen IC. Linking cardiovascular theory to practice in an undergraduate medical curriculum. Adv Physiol Educ. 2001;25(4):193–201.
Buzzell PR, Chamberlain VM, Pintauro SJ. The effectiveness of web-based, multimedia tutorials for teaching methods of human body composition analysis. Adv Physiol Educ. 2002;26(1):21–9.
Dennick R. Twelve tips for incorporating educational theory into teaching practices. Med Teach. 2012;34(8):618–24.
Yardley S, Teunissen PW, Dornan T. Experiential learning: AMEE guide no.63. Med Teach. 2012;34(2):e102–15.
Reiter HI, Eva KW, Hatala RM, Norman GR. Self and peer assessment in tutorials. Application of relative-ranking model. Acad Med. 2002;77(11):1134–9.
Papinczak T, Young L, Groves M, Haynes M. An analysis of peer, self, and tutor assessment in problem-based learning tutorials. Med Teach. 2007;29(5):e122–32.
Dolmans DHJM, Ginns P. A short questionnaire to evaluate the effective of tutors in PBL: validity and reliability. Med Teach. 2007;27(6):534–8.
Sargeant J, et al. Exploring a model (emotion, content, outcomes) for facilitating multisource feedback. Med Teach. 2011;33(9):744–9.
Kulak V, Genevieve N. A guide to using case-based learning in biochemistry education. Biochem Mol Biol Educ. 2014;42(6):457–73.
Henderson JE, Conochie LB, Steinert Y. Co-tutors in the basis of medicine. Clin Invest Med. 2000;23(1):86–9.
Maudsley G. The limits of tutors’ comfort zones with four integrated knowledge themes in a problem-based undergraduate medical curriculum (interview study). Med Educ. 2003;37(5):417–23.
Stevenson FT, Bowe CM, Gandour-Edward R, Kumari GV. Paired basic science and clinical problem-based learning faculty teaching side by side: do students evaluate them differently? Med Educ. 2005;39(2):194–201.
Baroffio A, et al. Effect of teaching context and tutor workshop on tutorial skills. Med Teach. 2006;28(4):e112–9.
Shields HM, et al. Faculty development program to train tutors to be discussion leaders rather than facilitators. Acad Med. 2007;82(5):486–92.
Jacques D. Teaching small group. BMJ. 2003;326(7387):429–94.
Al-Modhefer A-K, Roe SM. Tutorials for large classes of common foundation program biomedical science students: successes and challenges. Nurse Educ Today. 2010;30(4):365–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Amara, F., Ghia, JE. Practical Strategies for Using Case-based Tutorials in Small Group Learning: Challenges and Solutions. Med.Sci.Educ. 27, 767–778 (2017). https://doi.org/10.1007/s40670-017-0463-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-017-0463-8