Abstract
Purpose
Patient hand-over is a critical skill to develop in the era of reduced duty hours. There is insufficient data in the literature that medical students, especially in the third year, are being instructed to participate in a patient hand-over. Early introduction into the curriculum should provide earlier competency which has the potential to decrease the number of medical errors related to communication.
Methods
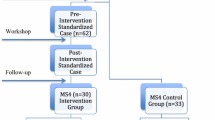
All students were expected to use our institution’s hand-over mnemonic SAFETIPS when signing out on inpatient wards. Students were randomly assigned to a curriculum or control group and completed patient hand-over student confidence pre-surveys. The curriculum group participated in a faculty-led workshop at the beginning of the clerkship teaching hand-overs. Faculty members assessed student hand-overs at the end of clerkship, followed by a student post-survey.
Results
The statistically significant difference (P = .001) in median inventory scores (alpha = .70) for students in the curriculum (13.0(±2.0)) vs. control (12.0(±5.0)) is coupled to an effect size (Cliff’s d = 0.34). Five SAFETIPS items reported significant increases (p ≤ .050) for students in the curriculum vs. control. Significant increases in pre-/post-survey (alpha = .84/.87) scores are reported for students in the curriculum (pre/post difference = 9.0, P = .001) and in the control group (difference = 7.3, P = .001) for the survey. The largest individual item increases for both groups were “using SAFETIPS to give/listen to hand-over of patients” (difference = 2.0, P = .001).
Conclusions
Third-year medical student skill and confidence level giving patient hand-over using SAFETIPS is improved with the use of a formal curriculum.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In June 2002, the Accreditation Council for Graduate Medical Education (ACGME) approved a reduction in the number of hours that medical residents are allowed to work due to concern for an increase in errors in patient care caused by resident fatigue [1–4]. As a result of this reform, the medical training of physicians has undergone significant changes since 2003 [5]. In particular, the number of patient hand-overs has necessarily increased due to the reduction in resident work hours [6–9]. A patient hand-over is a communication process whereby information and responsibility are transferred from one medical professional to another. Studies have shown that communication during hand-overs is prone to omissions and inaccuracies and has led to an increase in preventable medical errors that are occurring predominantly in the hands of the cross-covering team [6, 8, 10, 11]. In response, accrediting bodies now require that patient hand-overs be standardized and practiced in the face of mounting medical errors related to these gaps in communication [12, 13].
While formal training curriculums are emerging in residency programs across the country, there is insufficient data in the literature that medical students, especially in the third year, are being instructed and assessed on how to participate in a patient hand-over [14–16]. A large review of clerkship directors reported that only a very small percentage of medical students were taught patient hand-over in a formal curriculum; most medical students are learning this task by observing their interns [17]. The small number of studies cited in the literature that had reported formal curriculums in their medical schools were during the fourth year [18, 19].
There are several studies that support early introduction of patient hand-over training in the medical school curriculum. One group of educators responded to student anxiety about feeling unprepared to participate in a patient hand-over and developed a 1-hour educational session for them to attend [20]. Students self-reported that their knowledge on hand-over of care had improved and rated the session favorably. Another study looked at the process by which patient hand-over can decrease redundancies in work, saving both time and money, but requires competency in the ACGME domains of communication and professionalism [21]. Because the skill set required for patient hand-over hinges on these core competencies, it should be introduced as early as possible into the medical school curriculum, especially as medical schools transition to a more integrated approach and students are increasingly seeing patients in the first year of medical school [16, 22, 23]. Patient hand-over literature within the framework of the psychology of communication has reported that interns have overestimated the efficacy of their sign out, even when they left out key information [24]. This underscores that the patient hand-over is a complex interaction that is affected by competencies other than medical knowledge and should be taught as early as possible. It is important to note that junior medical students have demonstrated a readiness to successfully participate in patient hand-over and support the idea of formal hand-over training prior to working with patients [25].
There are many curriculum factors that make the third year of medical school ideal for introducing patient hand-over training. The third year of medical school is the year that students have the most abundant clinical experiences and are exposed to the highest volume of patients. Additionally, students on clerkships often have protected time to attend clerkship lectures and participate in research, requiring them to sign out the patients they are following to other members of the healthcare team. Lastly, without early hand-over training, interns are expected to sign out patients on their first day of work despite evidence that they feel underprepared to do so [25].
We developed a curriculum using a previously described patient hand-over mnemonic SAFETIPS for third-year medical students (M3) during their pediatric clerkship to measure objective and subjective acquisition of skill in this area [26, 27]. We hypothesized that this faculty-led training and feedback would improve their skill and confidence level with this specialized form of communication.
Methods
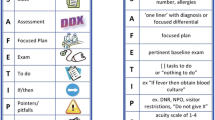
This study was approved by the institutional review board of the Medical College of Wisconsin and Froedtert Hospital. During the 2013–2014 academic year, all N = 185 M3 students were randomly assigned to a curriculum (N = 94) or control group (N = 91) prior to starting the pediatric clerkship. The clerkship is 8 weeks with 4 weeks spent on inpatient service at a busy academic hospital. While on inpatient, the student schedule mirrors the schedule of a pediatric intern including a week of night float. At orientation on the first day of the clerkship, the students received the SAFETIPS patient hand-over card our pediatric residents use. SAFETIPS is a standardized patient hand-over tool that was developed using criteria set forth by the Joint Commission [26, 28]. In this study, medical student hand-overs were analyzed with the SAFETIPS instrument which includes an eight-point checklist where S = stats (patient name, age, sex, room number, allergies), A = assessment (“one liner” with diagnosis or focused differential), F = focused plan, E = pertinent baseline exam, T = tasks to do or “nothing to do,” I = if/then (anticipatory guidance), P = pitfalls (such as patient is do not resuscitate (DNR), nothing by mouth (NPO)), S = sick-o-meter (acuity scale of 1–4 with 1 being stable to 4 being very sick). Both groups participated in the pediatric clerkship to the same degree. On the first day of the clerkship, all students completed patient hand-over confidence pre-surveys. The curriculum group participated in a faculty-led session providing formal instruction on patient hand-over. The faculty member explained that the goal of the session was to help students learn how to perform a safe patient hand-over so they could practice this skill more effectively prior to starting an intern year. The session was a 60-minute interactive presentation detailing the adverse consequences of poor patient hand-over and showed video-taped examples of patient hand-over scenarios. The students were asked to identify and improve errors in the flawed scenarios and comment on the strengths of the excellent ones.
At the end of each clerkship, all students participated in a patient hand-over simulation with two dedicated and trained faculty members who were blinded to the group each student was in. The students were given the same written patient encounter (mock history and physical examination of a patient with meningitis that was created by the faculty) which included history, physical examination, and laboratory results and then asked to sign out to the faculty. The students were allowed to use their SAFETIPS card during the hand-over scenario as the goal of a successful patient hand-over is not memorizing the mnemonic but transferring critical information to a colleague in an organized fashion. This exchange was assessed by the faculty using a hand-over checklist containing the SAFETIPS components on a three-point Likert scale where a score of 2 was given if the student did well (supplied the necessary amount of information), 1 if it was an area for improvement (supplied too much or too little information), or 0 if they missed the item completely (Table 1). In addition, a single item for assessing the organization of student presentation labeled “item format” was added to the SAFETIPS instrument, which assessed the overall organization of the hand-over. At the end of the encounter, the faculty provided feedback to the student and marked whether the student was in the curriculum or control group. All students then completed a patient hand-over confidence post-survey with the results compared to the pre-survey (Tables 2 and 3). The pre- and post-survey had seven identical five-point Likert scale items (1 = extremely uncomfortable, 3 = neutral, 5 = extremely comfortable). Pre-/post-survey data was anonymously reported and not paired.
Results
The descriptive and inferential statistics for the SAFETIPS patient hand-over structured clinical observation inventory are reported in Table 1. Medians and inter-quartile ranges (IR) were used for descriptive statistics, and Mann-Whitney U tests were used to determine statistically significant differences in the median scores for curriculum vs. no curriculum. All eight individual items were summed and a Shapiro-Wilk test was used to assess normality for the sum but was statistically significant indicating non-normality. Kendall’s tau-b (τ B ) correlations were used to establish relational strength of inventory items with themselves and with the item labeled as “format correct” which measured the student’s organization of the eight SAFETIPS items while adjusting for ties shown in Table 2.
The descriptive and inferential statistics for the pre/post SAFETIPS student survey for students in the curriculum are reported in Table 3, while students in the control group are reported in Table 4. Anonymously reported pre/post data was not paired, and therefore, an independent group Mann-Whitney U test was used to determine statistically significant differences in median scores for the individual survey items. The seven survey items were summed and a Shapiro-Wilk test was used to assess normality for the sum of the items which was not statistically significant indicating normality. A two-way univariate analysis of variance (ANOVA) was used to determine the effects of (a) curriculum/control and (b) pre/post on the sum of the survey items. Kendall’s tau-b correlations were used to establish relational strength of survey items. The inter-item reliability for the survey and inventory data was reported as Cronbach alpha. All statistical analyses were generated with IBM® SPSS® 21.0.
Inventory
The statistically significant difference (P = .001) in median inventory scores for students in the curriculum (13.0(±2.0)) vs. control (12.0(±5.0)) is coupled to an effect size (Cliff’s d = 0.34). Five of eight individual SAFETIPS items reported significant increases (P ≤ .050) for students in the curriculum vs. control as reported in Table 1, which included items measuring student assessment, focused and relevant plan, baseline exam, “to do” tasks assigned, and an “if/then” included.
The inter-item reliabilities of the inventory items for the curriculum group were alpha = 0.54 and the control group were alpha = 0.72. The inter-item Kendall’s tau-b correlation matrix for the eight inventory items consisted of 28 correlations. The three strongest, statistically significant correlations for the curriculum (all τ B > 0.40) and control (all τ B > 0.40) groups involved the pairing of the assessment item with these three items: focused and relevant plan (τ B = .447, P = .001), baseline exam (τ B = .482, P = .001), and “to do” tasks (τ B = .422, P = .001).
The strongest three statistically significant correlations of SAFETIPS items with the “format correct” item in decreasing order of correlation strength for both the curriculum and control groups as reported in Table 2 are (1) assessment, (2) focused plan, and (3) baseline exam. Note for Table 2, NA = not available due to one variable having identical scores for all participants (i.e., constant).
Survey
The Shapiro-Wilk test for normality of the sums of all seven survey items was not statistically significant for the curriculum (P = .065) or control groups (P = .052), and data for each group was determined to fit a normal distribution. The two-way ANOVA yielded statistically significant main effects for both (a) curriculum/control (P = .001) and (b) pre/post (P = .001) as predictors of the outcome variable of sum of the seven survey items, but there was no statistically significant (P = .057) interaction effect (curriculum/control x pre/post). Statistically significant pre/post increases in survey median scores for all seven individual items are reported for curriculum and control groups in Tables 3 and 4, respectively. The statistically significant mean difference in the sum of all seven survey item scores for students in the curriculum (pre/post difference = 9.0, P = .001) is larger than the difference for the control group (difference = 7.3, P = .001). For the individual survey item “asking the recipient to discuss problems or questions,” a larger pre/post median increase was also reported for the curriculum group (difference = 2.0, P = .001) than the control group (difference = 1.0, P = .001). The largest increases for both the curriculum and control groups was “using SAFETIPS to give/listen to hand-over of patients” (difference = 2.0, P = .001).
The inter-item reliabilities of the curriculum group were alpha = 0.84 (pre) and alpha = 0.87 (post) and the control group were alpha = 0.84 (pre) and alpha = 0.89 (post).
Discussion
The assessment of our implemented SAFETIPS curriculum suggests a significant improvement in M3 patient hand-over. This was encouraging given the clerkship is only 8 weeks, the low number of faculty needed to implement the curriculum, and students reported they had not received hand-over training prior to our clerkship. Generally, we found the hand-over components of presenting an assessment, focused and relevant plan, baseline exam, “to do” tasks assigned, and anticipatory guidance were the most difficult for M3 students to master. Using our curriculum, we were able to report that there was significant improvement in student performance in these five areas. The curriculum group not only demonstrated improvements in most aspects of the SAFETIPS hand-over but also in the overall organization of the hand-over. This suggests that the control group may have struggled with hand-overs by presenting unnecessary and/or unrelated details which could lead to the recipient tuning out critical details [29, 30]. The improvement in these areas is encouraging given other studies have reported that interns often struggle with similar items in their own sign out [8].
The assessment SAFETIPS item was determined to be the best indicator of the organization of the student presentation. It was also well associated with focused and relevant plan, baseline exam, and “to do” tasks suggesting that this single item gives a reasonable preliminary indication of overall performance before other items are measured. Students with weaker diagnostic skills could be informed that improving this particular skill is necessary to complete an acceptable hand-over.
The survey results reported statistically significant pre/post increases for both groups; however, the curriculum group reported a larger increase than the control group. The literature has indicated that interns had positive subjective experiences with a similar curriculum, but our study also demonstrates an objective increase in skill [31]. While student confidence is important, reaction data is still an indirect measure of actual learning outcomes according to Kirkpatrick’s hierarchy [23].
One limitation of our study is that the pre/post surveys were not linked to the inventory for each student to preserve their anonymity. Without this information, it is impossible to conclude that a student’s perceived increase in skill was related to an objective increase. The finding that both groups felt more confident with patient hand-over at the end of the clerkship may be due to the fact that each group had the opportunity to sign out to faculty and get immediate feedback irrespective of being in the curriculum group which was perceived as a valuable learning experience by the students. This study used SAFETIPS for patient hand-over so we cannot generalize our findings to other published methods for patient hand-over. Lastly, because our study was conducted on a pediatric clerkship, it may not be generalizable to other specialties.
The literature is replete with strategies to implement hand-over teaching to medical professionals, but there is a paucity of data that demonstrates formal instruction translates into improved patient outcomes, and our study is consistent with other studies [23, 32]. The number of published studies examining hand-over curriculums would suggest that leaders in education believe it will make a positive impact, so it is encouraging to see that there is emerging literature reporting that implementation of a hand-over program with residents is translating into decreased medical errors and preventable adverse events [33]. Our study is unique in that it took advantage of the third year of medical school as a place to introduce the concept of a patient hand-over and reported a significant positive impact on medical student skill and confidence level. As medical education becomes increasingly seamless and students are seeing patients throughout their 4 years of medical school, hand-over curriculums are relevant at this stage of training. Students have indicated wanting to learn this skill before intern year, interns have reported feeling underprepared to participate in a patient hand-over, and accrediting bodies mandate hand-over training for all healthcare providers. The idea that hand-over training should be withheld until intern year is challenged by data that suggests a hand-over is a compilation of several distinct skills that are built upon and enhanced over time throughout training [16, 23]. It has been the experience of clerkship directors at our institution that a hand-over curriculum is feasible to add to a third-year pediatric clerkship, and there are several concepts from this pilot that would be generalizable to other clerkships irrespective of the hand-over tool used. Further areas of study to support the addition of hand-over curriculum in the third year of medical school could examine whether the increase in skill and confidence level that our study demonstrated is retained intern year.
References
Accreditation Council for Graduate Medical Education. Report of the work group on resident duty hours. http://www.ttuhsc.edu/sop/residencies/documents/ACGME_work_hour_policy.pdf. Accessed December 10, 2014.
Steinbrook R. The debate over residents’ work hours. N Engl J Med. 2002;347:1296–302.
Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–48.
Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, Rothschild JM, Katz JT, Lilly CM, Stone PH, Aeschbach D, Czeisler CA. Effect of reducing interns’ weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351:1829–37.
Philibert I, Friedmann P, Williams WT. New requirements for resident duty hours. JAMA. 2002;288:1112–4.
Horwitz LI, Krumholz HM, Green ML, Huot SJ. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med. 2006;166:1173–7.
Vidyarthi AR, Arora V, Schnipper JL, Wall SD, Wachter RM. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1:257–66.
Horwitz LI, Moin T, Krumholz HM, Wang L, Bradley EH. What are covering doctors told about their patients? Analysis of sign-out among internal medicine house staff. Qual Saf Health Care. 2009;18:248–55.
Van Eaton EG, Tarpley JL, Solorzano CC, Cho CS, Weber SM, Termuhlen PM. Resident education in 2011: three key challenges on the road ahead. Surgery. 2011;149:465–73.
Petersen LA, Brennan TA, O’Neil AC, Cook EF, Lee TH. Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med. 1994;121:866–72.
Mukherjee S. A precarious exchange. N Engl J Med. 2004;351:1822–4.
Agency for Healthcare Research and Quality. Patient safety primers: handoffs and signouts. http://www.psnet.ahrq.gov/primer.aspx?primerID=9. Accessed February 10, 2015.
Accreditation Council for Graduate Medical Education. Common program requirements. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/CPRs2013.pdf. Accessed December 10, 2014.
Gakhar B, Spencer AL. Using direct observation, formal evaluation, and an interactive curriculum to improve the sign-out practices of internal medicine interns. Acad Med. 2010;85:1182–8.
DeRienzo CM, Frush K, Barfield ME, Gopwani PR, Griffith BC, Jiang X, et al. Handoffs in the era of duty hours reform: a focused review and strategy to address changes in the accreditation council for graduate medical education common program requirements. Acad Med. 2012;87:403–10.
Gordon M. Training on handover of patient care within UK medical schools. Med educ online. 2013;18:1–5.
Solet DJ, Norvell JM, Rutan GH, Frankel RM. Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med. 2005;80:1094–9.
Farnan JM, Paro JA, Rodriguez RM, Reddy ST, Horwitz LI, Johnson JK, et al. Hand-off education and evaluation: piloting the observed simulated hand-off experience (OSHE). J Gen Intern Med. 2010;25:129–34.
Chu ES, Reid M, Burden M, Mancini D, Schulz T, Keniston A, et al. Effectiveness of a course designed to teach handoffs to medical students. J Hosp Med. 2010;5:344–8.
Darbyshire D, Gordon M, Baker P. Teaching handover of care to medical students. Clin Teach. 2013;10:32–7.
Arora VM, Johnson JK, Meltzer DO, Humphrey HJ. A theoretical framework and competency-based approach to improving handoffs. Qual Saf Health Care. 2008;17(1):11–4.
Humphris GM, Kaney S. Assessing the development of communication skills in undergraduate medical students. Med Educ. 2001;35:225–31.
Gordon M, Findley R. Educational interventions to improve handover in health care: a systematic review. Med Educ. 2011;45:1081–9.
Chang VY, Arora VM, Lev-Ari S, D’Arcy M, Keysar B. Interns overestimate the effectiveness of their hand-off communication. Pediatrics. 2010;125:491–6.
Cleland JA, Ross S, Miller SC, Patey R. “There is a chain of chinese whispers…”: empirical data support the call to formally teach handover to prequalification doctors. Qual Saf Health Care. 2009;18:267–71.
Shaughnessy EE. Pediatric resident sign-out education. https://www.mededportal.org/publication/8321. Accessed March, 2013.
Shaughnessy EE, Ginsbach K, Groeschl N, Bragg D, Weisgerber M. Brief educational intervention improves content of intern handovers. J Grad Med Educ. 2013;5:150–3.
Arora V, Johnson J. A model for building a standardized hand-off protocol. Jt Comm J Qual Patient Saf. 2006;32:646–55.
Arora V, Johnson J, Lovinger D, Humphrey HJ, Meltzer DO. Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005;14:401–7.
WHO Collaborating Center for Patient Safety Solutions. Communication during patient hand-overs. http://www.who.int/patientsafety/solutions/patientsafety/PS-Solution3.pdf. Accessed December 20, 2014.
Chu ES, Reid M, Schulz T, Burden M, Mancini D, Ambardekar AV, et al. A structured handoff program for interns. Acad Med. 2009;84:347–52.
Riesenberg LA, Leitzsch J, Massucci JL, Jaeger J, Rosenfeld JC, Patow C, et al. Residents’ and attending physicians’ handoffs: a systematic review of the literature. Acad Med. 2009;84:1775–87.
Starmer AJ, Spector ND, Srivastava R, West DC, Rosenbluth G, Allen AD, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371:1803–12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding/Support
This study was funded in part by a Medical College of Wisconsin Learning Resource Fund grant PRO00019619.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by the institutional review board of the Medical College of Wisconsin/Froedtert Hospital.
Rights and permissions
About this article
Cite this article
Saudek, K., Treat, R. Does Medical Student Hand-Over Training on a Third-Year Pediatric Clerkship Improves Skill and Confidence Level?. Med.Sci.Educ. 26, 649–655 (2016). https://doi.org/10.1007/s40670-016-0327-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-016-0327-7