Abstract
Introduction
Hyperkalemia, one of the most important electrolyte abnormalities of chronic kidney disease (CKD), often limits the use of renin–angiotensin–aldosterone system inhibitors and can increase in the postprandial period. In this study we report a real-world experience with the new non-adsorbed potassium binder patiromer in stage 3b-4 CKD patients. Moreover, we performed a cross-sectional analysis to evaluate, for the first time, the efficacy of patiromer in the control of postprandial potassium concentrations.
Methods
We retrospectively collected data of 40 patients at the time of patiromer initiation (T0), and after 2 (T2), 6 (T6) and 12 (T12) months of treatment. For cross sectional analysis, a blood sample was collected 2 h after the main meal for the evaluation of postprandial potassium concentrations.
Results
Eighty-two point five percent of patients (33/40) reached normal potassium concentrations at T2. Serum potassium significantly decreased at T2 compared to T0 (5.13 ± 0.48 vs 5.77 ± 0.41 mmol/L, respectively; p < 0.001) and the reduction remained significant during the follow-up (5.06 ± 0.36 at T6 and 5.77 ± 0.41 at T12; p < 0.001 vs T0). Renin–angiotensin–aldosterone system inhibitors were continued by 93% of patients (27/29). Adverse events were reported in 27.5% of patients and were all mild-to-moderate. Postprandial potassium concentrations did not significantly change compared to fasting state potassium measured at T12 (4.53 ± 0.33 vs 5.06 ± 0.36 mmol/L; p = 0.15).
Conclusions
In a real-world setting of advanced CKD patients, patiromer is a useful treatment for hyperkalemia, since it significantly reduces serum potassium levels over the long term and is able to maintain potassium concentrations in the normal range even in the post-prandial period.
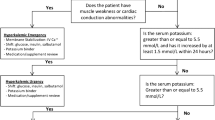
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperkalemia represents one of the most important electrolyte abnormalities observed in chronic kidney disease (CKD), due to its potential to cause life-threatening cardiac arrhythmias [1].
Usually defined as potassium concentrations ≥ 5 mmol/L, hyperkalemia is the result of impaired urinary potassium metabolism, extracellular shift of K + due to CKD-associated metabolic acidosis, and/or drugs interfering with renal potassium excretion, in particular renin–angiotensin–aldosterone system inhibitors (RAASi) [2, 3].
Strategies aimed at reducing potassium concentrations typically include low-potassium dietary intake, addition of a loop or thiazide diuretic, correction of acidosis with sodium bicarbonate, potassium binders, and reduction or discontinuation of RAASi [4].
Renin–angiotensin–aldosterone system inhibitors are known to provide long-term reno- and cardio-protection [5, 6], and evidence-based treatment guidelines recommend their use for patients with CKD [7,8,9,10], while there is increasing evidence that their discontinuation leads to worse outcomes [11, 12]. However, RAASi use can be hindered by hyperkalemia [11, 13, 14], that represents the main cause of the large gap reported between guideline recommendations and real-world practice in chronic kidney disease.
Therefore, efforts to maintain normokalemia and allow continuation of RAASi is a goal for optimal CKD management [15].
In the past, the availability of only a few effective agents limited treatment of hyperkalemia [15]. The potassium binder sodium polystyrene sulfonate was the only oral hyperkalemia therapy for many years; however, the shortage of data supporting its efficacy and the frequently reported gastrointestinal side effects strongly limited its use [16, 17].
The more recent oral potassium-binding agents patiromer and sodium zirconium cyclosilicate have been reported to be safe and effective in the treatment of hyperkalemia in patients with normal or reduced glomerular filtration rate (GFR) [18, 19]. Patiromer is a sodium-free, non-absorbed polymer that exchanges potassium with calcium, predominantly in the distal colon, thus increasing fecal potassium excretion and lowering serum potassium levels [18].
Of note, hyperkalemia can worsen in the postprandial period. In particular, postprandial hyperkalemia risk increases as GFR declines below 45 mL/min/1.73 m2; accordingly, CKD patients have been reported to have impaired dietary potassium tolerance, resulting in an increased postprandial serum potassium level with potassium peaks observed 2 h after the meal [20, 21]. However, since plasma potassium levels are usually measured in the fasting state, the acute effects of dietary potassium intake on plasma concentrations in a real-world setting have never been detected.
Few published real-world studies evaluated potassium management in non-dialysis CKD patients receiving potassium-binding agents and, in particular, no data are available on the control of postprandial hyperkalemia in patients with impaired renal function.
The present study aimed to retrospectively report the use of patiromer in non-dialysis CKD patients in a real-world clinical setting [22, 23]; in addition, we performed a cross-sectional analysis to evaluate, for the first time, the use of patiromer in the control of postprandial potassium peaks.
Methods
This is a single center retrospective longitudinal cohort study with a cross-sectional phase.
Retrospective study
For the retrospective cohort analysis, we used healthcare data from the medical records of patients with stage 3b-4 CKD referred to the Department of Nephrology of the University “Federico II” of Naples from March 2022 to April 2023.
Inclusion criteria were the following: adult patients (≥ 18 years of age); diagnosis of hyperkalemia, defined as serum potassium levels between 5.5 and 6.5 mmol/L at two follow-up visits before starting patiromer; patients treated for at least 1 year with a stable regular dose of patiromer; estimated GFR (eGFR) between 45 and 15 mL/min/1.73 m2; ≥ 90% completeness of the mandatory data (see below); and informed consent for participation in the study. For patients treated with antihypertensive drugs and diuretics, doses had to be stable for 28 days before patiromer initiation.
We excluded patients on Renal Replacement Therapy (RRT) requiring dialysis or kidney transplant in the study period; potassium-related electrocardiographic changes; uncontrolled or unstable arrhythmias or clinically significant ventricular arrhythmias, acute coronary syndrome, transient ischemic attack or stroke within the previous 2 months; severe gastrointestinal disorders; type 1 diabetes and uncontrolled type 2 diabetes.
Patients treated with patiromer received a dose of 8.4 g once daily, taken with food at least 3 h before or 3 h after other medications. Moreover, we scheduled a first follow-up visit 4 weeks after therapy initiation for all treated patients.
In patients who fulfilled the inclusion criteria, data of interest were retrospectively collected at baseline (time of start of patiromer treatment, T0), and after 2, 6 and 12 months of therapy with patiromer (T2, T6 and T12, respectively).
Age, sex, underlying cause of CKD and comorbid conditions were recorded for all patients at the baseline visit. Complete clinical assessment was performed at each visit, according to the clinical practice currently in use in our center. Baseline and follow-up visit recordings included blood and urine sample tests (including serum creatinine, potassium and magnesium levels), eGFR evaluation, clinical examination and vital sign measurements. All laboratory values were measured by the standardized methods used in our hospital. Glomerular filtration rate was estimated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [24]. Medication and medication changes with prescription details were recorded at each visit, such as date of prescription, medication type, dose, and quantity.
The endpoints were: the proportion of patients that achieved the target serum potassium levels (between 3.8 and 5.2 mmol/L) at T2; the change in serum potassium levels from baseline to T2, T6 and T12; the percentage of patients continuing RAASi therapy in the follow-up.
Cross-sectional analysis
In addition to the retrospective study, we performed a cross-sectional analysis aimed at evaluating the effects of patiromer on postprandial potassium concentrations.
For this analysis, we selected patients from the retrospective study who achieved the target potassium levels in the follow-up period and were still on therapy with a stable dose of patiromer for at least one month after T12. Within the first month after T12, the enrolled patients underwent a single blood withdrawal performed 2 h after the main meal to evaluate their postprandial potassium concentration. Finally, the postprandial potassium values were compared to the serum potassium levels measured in the fasting state at T12.
The study was conducted in accordance with the principles outlined in the Declaration of Helsinki and was approved by the local ethics committee. Written informed consent was obtained from all participants.
Statistical analysis
Data were tested for normal distribution using the Shapiro–Wilk test. Normally distributed data were reported as mean and standard deviation, while non-normally distributed data as median and interquartile range.
Comparisons were performed with analysis of variance for parametric data and the Friedman test for non-parametric data. Post hoc analysis was performed using the Tukey test for parametric data and Nemenyi test for non-parametric data. Differences were considered significant if p < 0.05.
All statistical analyses were performed using the software R Core Team (2019). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL hhtps://www.R-project.org/.
Results
Retrospective study
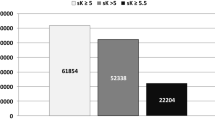
We identified 303 adult patients with stage 3b-4 CKD and serum potassium levels between 5.5 and 6.5 mmol/L, referring to our Chronic Renal Failure Outpatient Clinic between March 2022 and April 2023. Of these, 61 received a prescription for patiromer in the study period and met the inclusion criteria for enrollment in the retrospective study, and 40 finally resulted eligible for the study cohort (Fig. 1).
The main baseline characteristics of the retrospective study cohort are reported in Table 1. In summary, 70% of patients were male, with a mean age of 60.2 ± 13.0 years; eGFR was 22.7 ± 10.4 ml/min/1.73 m2 and serum K + levels were 5.77 ± 0.3 mmol/L. A total of 85% of patients had hypertension, 52.5% had type 2 diabetes and 30% heart failure. Of note, 20% of patiromer initiators had a history of sodium polystyrene sulfonate administration prior to the baseline period (data not shown).
Of the 40 patients treated with patiromer, 33 (82.5%) reached potassium serum levels in the target range 2 months after treatment initiation (T2). Serum potassium levels significantly decreased from T0 to T2 (5.77 ± 0.3 vs 5.13 ± 0.48 mmol/L, respectively; p < 0.001). The reduction remained statistically significant vs baseline at T6 and T12 (5.16 ± 0.45 and 5.06 ± 0.36 mmol/L, respectively; p < 0.001) (Fig. 2A, B).
Of the 40 patients included in the study, 29 (72.5%) were treated with at least one renin–angiotensin–aldosterone system inhibitor. Among these patients, 6 (20.7%) changed RAASi treatment prescription—2 (6.9%) discontinued RAASi treatment, 1 patient (3.4%) had a dose reduction, and 1 (3.4%) had a reduction in the number of RAASi drugs, changing from a combination of an angiotensin converting enzyme inhibitor and an angiotensin II receptor blocker to monotherapy; an increased dose of these agents was prescribed to 2 patients (6.9%).
Patiromer was prescribed at the standard dose of 8.4 g once daily, and no patient required a dose adjustment during the whole treatment period.
Eleven patients (27.5%) reported at least one adverse event during follow-up. The most common adverse events are shown in Table 2; no serious adverse events occurred, and mild-to-moderate constipation was the most common adverse event (reported in 10% of patients). A slight, not significant decrease in magnesium levels was observed after initiation of patiromer, though not requiring magnesium-replacement therapy; however, mean serum magnesium levels remained within the normal range throughout the whole treatment period (data not shown).
Cross-sectional analysis
Twelve of the 40 patients in the retrospective study achieved the target potassium levels in the follow-up period, were still on therapy with a stable dose of patiromer for at least one month after T12, and provided consent to participate in the cross-sectional analysis.
The mean postprandial potassium levels measured 2 h after the main meal were 4.53 ± 0.33 mmol/L. Of note, postprandial potassium concentrations remained within the normal range (between 3.8 and 5.2 mmol/L) in all patients. Finally, when compared to the serum potassium levels measured in the same patients in fasting state at T12, postprandial potassium concentrations resulted slightly, albeit not significantly reduced (5.06 ± 0.36 vs 4.53 ± 0.33 mmol/L; p = 0.15) (Fig. 3).
Discussion
Our study confirmed the safety and effectiveness of patiromer in non-dialysis hyperkalemic CKD patients in a real-world clinical setting, and reported for the first time the effectiveness of a stable dose of this new potassium-binder in the control of postprandial hyperkalemia.
To date, several studies have reported that patiromer is safe and effective in the treatment of hyperkalemia in CKD patients [18, 19]. In particular, two prospective, randomized clinical trials, the AMETHYST-DN [25] and OPAL-HK [26] trials established the efficacy of patiromer for hyperkalemia treatment in patients with stage 3–4 CKD, diabetes, hypertension, and/or heart failure, receiving RAASi therapy. Results of the AMETHYST-DN trial showed that patiromer significantly reduced potassium serum levels after 4 weeks, and the reduction was maintained for 52 weeks in patients with mild (5.0 to < 5.5) or moderate (> 5.5 to < 6.0) hyperkalemia [25]. The OPAL-HK trial showed that the majority (76%) of patients with mild (5.1 to < 5.5 mmol/L) and moderate hyperkalemia (5.5 to < 6.5 mmol/L), respectively receiving patiromer at the dose of 8.4 g and 16.8 g per day, achieved normokalemia (potassium concentration ranging from 3.8 to 5.1 mmol/L) after 4 weeks [26].
Moreover, although limited, real-world data seem to confirm these results [22, 23].
The main finding of our study is that in a real-world setting, therapy with patiromer is associated with a significant reduction in serum potassium levels, which was already observed after 2 months of therapy; this reduction was maintained in the follow-up and was similar to the reduction reported in randomized controlled trials [25,26,27,28,29] and real-world studies [22, 23]. Of note, the proportion of patients who achieved serum potassium levels within the target range (3.8 to < 5.2 mmol/L) during the 1-year follow-up was greater than 80%.
Another important result of our study was that RAASi were continued throughout the entire follow-up period by 93% of patients on patiromer (27/29), an even higher proportion than what was observed in the two previous real-world experiences with advanced CKD patients [22, 23]. Furthermore, of these 27 patients continuing RAASi, only 2 were prescribed a reduced dose or number of drugs, while the remaining 86% of patients continued at the same or increased doses.
Our study demonstrated that only 20% of patiromer initiators had a history of sodium polystyrene sulfonate administration before the baseline period. This result confirmed data of previous studies reporting a relatively low implementation of hyperkalemia treatments despite its high prevalence in advanced CKD populations [23, 30, 31].
In addition to its effectiveness in achieving and maintaining normokalemia, our data confirmed that patiromer was safe and well tolerated throughout the whole study period [26], with only 27.5% of patients reporting at least one adverse event. Moreover, mild-to-moderate constipation was the most common adverse event (reported in 10% of patients); all adverse reactions were only mild-to-moderate in nature and no serious adverse events occurred. Since we enrolled only patients receiving at least 1 year of stable therapy with the regular dose of Patiromer, no data about adverse events leading to discontinuation are available.
For the first time, our data demonstrate the ability of chronic treatment with patiromer to control serum potassium levels in the postprandial period. It is well known that prandial potassium load may worsen hyperkalemia, since this electrolyte is absorbed by passive diffusion from the bowel and the peak of plasma potassium concentration is usually observed 0.5–2 h after the meal [21]. Evidence from kinetic studies using potassium salts showed that CKD patients may be more susceptible to transient diet-related increases in postprandial plasma potassium concentrations [32]. The ability of the kidney to increase kaliuresis in response to dietary potassium intake declines proportionally in CKD, disappearing for values of eGFR lower than 15 mL/min/1.73 m2 [20]. Moreover, although the intestinal secretion of potassium increases in CKD to maintain external potassium balance, it does not appear sufficient to prevent an acute increase in plasma potassium levels following a potassium load [20]. However, little is known about the management of postprandial hyperkalemia, especially among CKD patients. In fact, observational studies exploring the association of potassium intake with hyperkalemia in CKD patients usually measure plasma potassium concentrations in the fasting state, and therefore are not able to detect the acute effects of dietary potassium on plasma concentrations [33]. By contrast, in our cross-sectional analysis we measured serum potassium levels 2 h after the main meal in order to evaluate the effects of patiromer on postprandial potassium peaks. Interestingly, our results showed that postprandial serum potassium levels were maintained within the normal range in all the evaluated patients, confirming the effectiveness of patiromer on acute potassium peaks. Moreover, when compared to the serum potassium levels of the same 12 patients measured in the fasting state after 12 months of treatment, postprandial potassium values were slightly, though not significantly, lower.
The main limitations of our study are mostly due to its retrospective observational design: in particular, the lack of comparison with a control group could limit the strength of the conclusions. Another limitation is the low number of enrolled patients and the impossibility to exclude the role of concomitant hyperkalemia management therapies.
In conclusion, our study demonstrated that in a real-world setting of patients with advanced CKD, patiromer is a useful treatment for hyperkalemia, since its chronic use is associated with a significant reduction in serum potassium levels over the long term.
Moreover, therapy with patiromer was able to maintain normal concentrations even in the post-prandial period, ensuring the safety of continuing the RAASi treatment without the aid of other potassium binders or other additional measures of potassium control.
Data availability
All data are available upon reasonable request.
References
Einhorn LM, Zhan M, Hsu VD et al (2009) The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med 169:1156–1162
Sarnowski A, Gama RM, Dawson A et al (2022) Hyperkalemia in chronic kidney disease: links, risks and management. Int J Nephrol Renovasc Dis 15:215–228
Clase CM, CarreroJJ EDH et al (2020) Potassium homeostasis and management of dyskalemia in kidney diseases: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) controversies conference. Kid Kidney Int 97:42–61
Larivée NL, Michaud JB, More KM et al (2023) Hyperkalemia: prevalence. Predict Emerg Treat Cardiol Ther 12(1):35–63
Maschio G, Alberti D, Janin G et al (1996) The Angiotensin converting-enzyme inhibition in progressive renal insufficiency study group. Effect of the angiotensin-converting-enzyme inhibitor benazepril on the progression of chronic renal insufficiency. N Eng J Med 334:939–945
The GISEN Group (Gruppo Italiano di Studi Epidemiologici In Nefrologia) (1997) Randomised placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy. Lancet 349:1857–1863
Cheung AK, Chang TI, Cushman WC et al (2019) Blood pressure in chronic kidney disease: conclusions from a kidney disease: improving global outcomes (KDIGO) controversies conference. Kidney Int 95:1027–1036
Kidney Disease Improving Global Outcome (KDIGO) Working Group (2012) KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int 2:337–414
Taler SJ, Agarwal R, Bakris GL et al (2013) KDOQI US commentary on the 2012 KDIGO clinical practice guideline for management of blood pressure in CKD. Am J Kidney Dis 62:201–213
Capuano I, Buonanno P, Riccio E et al (2022) Randomized controlled trials on renin angiotensin aldosterone system inhibitors in chronic kidney disease stages 3–5: are they robust? a fragility index analysis. J Clin Med 11(20):6184
Epstein M, Reaven NL, Funk SE et al (2015) Evaluation of the treatment gap between clinical guidelines and the utilization of renin-angiotensin-aldosterone system inhibitors. Am J Manag Care 21:S212-220
Yildirim T, Arici M, Piskinpasa S et al (2012) Major barriers against renin–angiotensin–aldosterone system blocker use in chronic kidney disease stages 3–5 in clinical practice: a safety concern? Ren Fail 34:1095–1099
McCullogh PA, Rangaswami J (2018) Real or perceived: hyperkalemia is a major deterrent for renin-angiotensin aldosterone system inhibition in heart failure. Nephron 138:173–175
Riccio E, Capuano I, Buonanno P et al (2022) RAAS inhibitor prescription and hyperkalemia event in patients with chronic kidney disease: a single-center retrospective study. Front Cardiovasc Med 9:824095
Palmer BF (2004) Managing hyperkalemia caused by inhibitors of the renin–angiotensin–aldosterone system. N Engl J Med 351:585–592
Sterns RH, Rojas M, Bernstein P, Chennupati S (2010) Ion-exchange resins for the treatment of hyperkalemia: are they safe and effective? J Am Soc Nephrol 21:733–735
Harel Z, Harel S, Shah PS et al (2013) Gastrointestinal adverse events with sodium polystyrene sulfonate (Kayexalate) use: a systematic review. Am J Med 126(3):264.e9-264.e24
Buysse JM, Huang IZ, Pitt B (2012) PEARL HF: prevention of hyperkalemia in patients with heart failure using a novel polymeric potassium binder, RLY5016. Futur Cardiol 8:17–28
Agarwal R, Rossignol P, Romero A (2019) Patiromer versus placebo to enable spironolactone use in patients with resistant hypertension and chronic kidney disease (AMBER): a phase 2, randomised, double-blind, placebo-controlled trial. Lancet 394(10208):1540–1550
St-Jules DE, Fouque D (2022) Etiology-based dietary approach for managing hyperkalemia in people with chronic kidney disease. Nutr Rev 80(11):2198–2205
Hinderling PH (2016) The pharmacokinetics of potassium in humans is unusual. J Clin Pharmacol 56(10):1212–1220
Kovesdy CP, Gosmanova EO, Woods SD et al (2020) Real-world management of hyperkalemia with patiromer among United States Veterans. Postgrad Med 132(2):176–183
Pecoits-Filho R, McCullough K, Muenz D et al (2022) Patiromer utilization in patients with advanced chronic kidney disease under nephrology care in Germany. Clin Kidney J 16(1):176–183
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Bakris GL, Pitt B, Weir MR et al (2015) Effect of patiromer on serum potassium level in patients with hyperkalemia and diabetic kidney disease: the AMETHYST-DN randomized clinical trial AMETHYST-DN. Invest JAMA 314(2):151–161
Weir MR, Bakris GL, Bushinsky DA, OPAL-HK Investigators et al (2015) Investigators patiromer in patients with kidney disease and hyperkalemia receiving RAAS inhibitors. N Engl J Med 372(3):211–221
Pitt B, Bakris GL, Bushinsky DA et al (2015) Effect of patiromer on reducing serum potassium and preventing recurrent hyperkalaemia in patients with heart failure and chronic kidney disease on RAAS inhibitors. Eur J Heart Fail 17:1057–1065
Pitt B, Bakris GL, Weir MR et al (2018) Long-term effects of patiromer for hyperkalaemia treatment in patients with mild heart failure and diabetic nephropathy on angiotensin-converting enzymes/angiotensin receptor blockers: results from AMETHYST-DN. ESC Heart Fail 5:592
Drieling RL, LaCroix AZ, Beresford SA et al (2016) Validity of self-reported medication use compared with pharmacy records in a cohort of older women: findings from the women’s health initiative. Am J Epidemiol 184:233–238
Pecoits-Filho R, Fliser D, Tu C et al (2019) Prescription of renin-angiotensin-aldosterone system inhibitors (RAASi) and its determinants in patients with advanced CKD under nephrologist care. J Clin Hypertens (Greenwich) 21:991–1001
Sabbatini M, Garofalo G, Borrelli S et al (2014) Efficacy of a reduced pill burden on therapeutic adherence to calcineurin inhibitors in renal transplant recipients: an observational study. Patient Prefer Adherence 8:73–81
te Dorsthorst RPM, Hendrikse J, Vervoorn MT et al (2019) Review of case reports on hyperkalemia induced by dietary intake: not restricted to chronic kidney disease patients. Eur J Clin Nutr 73(1):38–45
Ramos CI, González-Ortiz A, Espinosa-Cuevas A et al (2021) Does dietary potassium intake associate with hyperkalemia in patients with chronic kidney disease? Nephrol Dial Transplant 36(11):2049–2057
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
AP had the original idea; AP, ADE, AS, ODM, IC, MA, MR followed the patients; PB performed the statistical analysis; ER wrote the paper; all authors revised the paper and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that no conflict of interest exists.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institute and regional research committee and with the 1964 Helsinki declaration and its later amendments of comparable ethical standards.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
All participants signed written informed consent for participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Riccio, E., D’Ercole, A., Sannino, A. et al. Real-world management of chronic and postprandial hyperkalemia in CKD patients treated with patiromer: a single-center retrospective study. J Nephrol 37, 1077–1084 (2024). https://doi.org/10.1007/s40620-024-01897-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-024-01897-9