Abstract
Background
Estimation of muscle mass is a pivotal component in the diagnosis of protein-energy wasting and sarcopenia. While bioimpedance spectroscopy is a widely accepted technique for the assessment of lean tissue related to the diagnosis of sarcopenia, to date skeletal muscle ultrasound (US) has not gained full acceptance for this purpose. The aim of this study was to assess the predictive value for mortality of the indexed thickness of the quadriceps vastus intermedius, as measured by US, compared to lean tissue index as estimated by bioimpedance spectroscopy, both combined with handgrip strength in a group of patients with end-stage kidney disease (ESKD) on maintenance hemodialysis (HD).
Methods
The cut-off values for low handgrip strength were < 27 kg for males and < 16 kg for females. The cut-off value for low lean tissue index was obtained from an age-matched healthy control group, with low lean tissue index being defined as values below the 10th percentile of the distribution of healthy subjects. The cut-off values for low quadriceps vastus intermedius thickness index were < 3.44 mm/m2 for males and < 3.52 mm/m2 for females.
Results
Ultrasound and bioimpedance spectroscopy were performed in 99 patients, and handgrip strength was assessed in 64 patients, all on maintenance HD. After a median follow-up of 28 months (interquartile range 19–41 months) 38 patients died. Lean tissue index was not associated with mortality, while low quadriceps vastus intermedius thickness index and low handgrip strength were associated with an increased hazard of death. In the fully adjusted model, only the combination of low handgrip strength and low quadriceps vastus intermedius thickness index was significantly associated with higher mortality.
Conclusion
When combined with low handgrip strength, low quadriceps muscle US outperformed low lean tissue index as assessed by bioimpedance spectroscopy in predicting mortality in a cohort of patients on maintenance HD. Ultrasound may be a useful and convenient technique for the assessment of sarcopenia and protein-energy wasting in this patient population.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Protein-energy wasting is common in patients with end-stage kidney disease (ESKD) [1]. As to the diagnosis of protein-energy wasting, one of the criteria is low muscle mass [2]. Moreover, to establish a diagnosis of sarcopenia, which represents a prevalent and relevant nutritional disorder in ESKD patients [3], both low muscle mass and low muscle strength must be present [4]. Both protein-energy wasting and sarcopenia are related to frailty, reduced health-related quality of life and an increased risk of death in patients with ESKD [3, 5,6,7].
Several methods are available for the estimation of muscle status. Computed tomography and magnetic resonance imaging, which are considered “gold standard” methods for accurately assessing muscle mass, have several drawbacks that limit their use to the research setting [8]. Surrogate methods assessing lean body mass, such as dual energy X-ray absorptiometry and bioimpedance analysis are more readily available in clinical practice [8]. Because of their high portability and relatively low cost, bioimpedance analysis and bioimpedance spectroscopy, have been routinely used in clinical practice to evaluate lean body mass in patients with ESKD. While bioimpedance analysis is based on a 2-compartment model that is theoretically able to discriminate between fat mass and free fat mass, it is in fact susceptible to inaccurate measurements in the presence of fluid overload [9]. On the other hand, bioimpedance spectroscopy is based on a 3-compartment model, and can thus theoretically discriminate fluid overload from lean body mass [10]. More recently, ultrasound (US) has been proposed as an alternative to computed tomography and magnetic resonance imaging to evaluate skeletal muscle mass. Advantages of US include its high portability, feasibility of measurements at bedside or in outpatients, relatively low cost, and no radiation exposure [8, 11]. While total body skeletal muscle cannot be derived by US, this technique can be used to perform a segmental assessment in different muscle groups. Low muscle mass as assessed by US evaluation of the quadriceps muscles and other major muscle groups of the lower limbs has shown a strong association with the development of frailty and disability [12, 13]; indeed, these muscle groups seem to be primarily affected when physical activity levels are decreased [13]. Moreover, US evaluation of the quadriceps muscles is not affected by fluid overload [14], and measurements of muscle thickness by US showed a good correlation with the same measurements performed by computed tomography [15, 16]. Furthermore, as US allows direct measurement of muscle thickness, the use of predictive equations is unnecessary.
On these grounds, the aim of the present study was threefold. Firstly, we compared quadriceps muscle thickness as measured by US with lean tissue index as assessed by bioimpedance spectroscopy for the prediction of mortality in ESKD patients on HD. Secondly, we evaluated if and to what extent sarcopenia, as diagnosed by the combination of low muscle mass assessed by either US or bioimpedance spectroscopy and low hand-grip strength, is related to mortality. Lastly, we analyzed the correlation between quadriceps muscle thickness as assessed by US and lean tissue index as evaluated by bioimpedance spectroscopy.
Patients and methods
Study design and patients
This is a secondary analysis involving 99 patients on maintenance HD from 3 dialysis centers in northern and central Italy (1 in Reggio Emilia and 2 in Livorno), out of a larger cohort of 181 HD patients from 6 Italian dialysis centers (3 in Parma, 1 in Reggio Emilia and 2 in Livorno) who were enrolled in an observational, longitudinal and prospective study and who had undergone bioimpedance spectroscopy at the time of the US assessment [17, 18]. The study was approved by the local Institutional Review Board (AVEN, ref. n° 45,737, December 12th, 2015). The procedures were performed in agreement with the Declaration of Helsinki, and written informed consent was obtained from all participants. Patients were evaluated between January 1st, 2016 and March 31st, 2018, and followed for mortality until May 31st, 2020. The main objective of the general study project was to assess the correlation between muscle mass, as assessed by US, and other nutritional parameters [17]. Only adult patients (≥ 18 years of age) who had been on HD for at least 6 months were enrolled. Exclusion criteria were the presence of malignancy or conditions with mandatory immobilization, including major amputation of the lower limbs. Due to the study protocol involving bioimpedance spectroscopy evaluation, patients with amputation of one or both upper limbs were also excluded.
Data collection
Demographic, clinical, and anthropometric data (height, body weight, body mass index (BMI)) were collected at baseline from medical records. Demographic data included age, sex, and dialysis vintage. Clinical data included chronic comorbidities, age-corrected Charlson comorbidity index, and dialysis modality. Blood samples were collected pre-dialysis as per institutional routine, preferably on a mid-week dialysis day, for the measurement of serum creatinine, blood urea nitrogen, albumin, and C-reactive protein.
Ultrasound technique
Quadriceps vastus intermedius thickness was measured by three experienced assessors (1 for both centers of Parma and Reggio Emilia, 1 for each of the 2 centers of Livorno) using a B-mode ultrasonography, wall tracking ultrasound system (Philips hd7xe, Logiq and General Electric) and 7.5 MHz linear array transducers. The technique has been described in detail elsewhere [14, 17]. Briefly, measurements were performed in both lower limbs during the HD session, with the patient lying in a supine position with both knees extended but relaxed and toes pointing upwards. Quadriceps vastus intermedius thickness was measured at a point located between the lower third and upper two-thirds of a line joining the anterior superior iliac spine with the upper pole of the patella [14, 19]. The transducer was placed perpendicular to the long axis of the thigh with a large amount of gel and without applying pressure to avoid compression of the muscle. The vertical diameter of the muscle was measured at the widest point, on the inner edge of the muscle fascia. Measurements were performed directly while obtaining the images using electronic calipers. The average of measurements taken at both limbs was used for the analysis. For further analyses, measurements were normalized by height squared and expressed in mm/m2 (quadriceps vastus intermedius thickness index). Based on data obtained from analyses performed in the whole cohort of the 181 patients originally enrolled, low muscle mass by US was defined by quadriceps vastus intermedius thickness index < 3.52 mm/m2 for females and < 3.44 mm/m2 for males, as these cut-off values (which correspond to the 50th percentile of the group) were associated with the highest accuracy in predicting mortality [18].
Bioimpedance spectroscopy
Body composition was assessed using the Body Composition Monitor (BCM, Fresenius Medical Care). Due to logistical reasons, all patients were evaluated immediately before the mid-week dialysis session. The electrodes were placed on the hand of the arm without the arteriovenous fistula and on the ipsilateral foot, and whole body bioimpedance spectroscopy was performed across 50 different frequencies between 5 kHz and 1 MHz after the patient had rested in the supine position for at least 5 min. Using equations based on a three-compartment model, the body composition monitor estimates the amount of excess fluid mass (overhydration, free fluid), normally hydrated adipose tissue mass, and normally hydrated lean tissue mass. Lean tissue index is defined as lean tissue mass normalized by height squared, and expressed as kg/m2. The lean tissue index was used as a proxy of total body muscle mass, and lean tissue index values were normalized by age and gender and expressed in percentiles of normal values. Patients with lean tissue index lower than the 10th percentile of the values obtained in healthy subjects were considered to have low muscle mass, and patients with a lean tissue index equal to or greater than the 10th percentile of normal values were considered to have normal muscle mass [20,21,22].
Muscle strength
Muscle strength was assessed by handgrip strength with a portable digital dynamometer (KERN & SOHN GmbH, Ballingen, Germany). After a lag period to let participants accommodate the instrument comfortably in their hand, they were requested to squeeze the instrument handle with maximum strength and minimal wrist extension (30 degrees or less). Two measurements were performed on the contralateral arm to the arteriovenous fistula before the HD session, with a resting period of 15 s between tests, and the highest value was recorded. The cut-off values used were 27 kg for men and 16 kg for women [4]. Handgrip strength measurements were available for 64 patients.
Sarcopenia diagnosis
Patients were diagnosed with sarcopenia when both muscle mass, as assessed by either quadriceps muscle thickness index or lean tissue index, and muscle strength, as assessed by handgrip strength were below the reference values [4].
Statistical analysis
Results were expressed as mean and standard deviation (SD) for continuous variables, or median and range for non-normally distributed data, and as frequencies for categorical variables. Normality was assessed by the Kolmogorov–Smirnov test. The correlation between quadriceps vastus intermedius thickness and quadriceps vastus intermedius thickness index with other nutritional variables (namely, BMI, lean tissue index and handgrip strength) was investigated using Pearson or Spearman correlation coefficient depending on variable distributions. Correlation values between 0.1 and 0.3 were considered weak correlations, > 0.3–0.5 were regarded as moderate correlation and > 0.5 were considered strong correlations according to Cohen [23]. The agreement between bioimpedance spectroscopy and US in the identification of low muscle mass was calculated by Kappa statistics. Differences in variables between surviving and deceased patients were analyzed using Student’s t test and the Mann–Whitney U test for normally distributed and non-normally distributed data, respectively. Kaplan–Meier survival curves were fitted to estimate the cumulative incidence of mortality in patients stratified by the presence of low handgrip strength, low quadriceps vastus intermedius thickness index, low lean tissue index, and sarcopenia diagnosed using either low lean tissue index or low quadriceps vastus intermedius thickness index in combination with low handgrip strength. Cox proportional hazards regression analysis was performed to analyze the independent risk of death associated with low handgrip strength, low quadriceps vastus intermedius thickness index, low lean tissue index, and sarcopenia diagnosed using either low lean tissue index or low quadriceps vastus intermedius thickness index in combination with low handgrip strength. We tested different multivariable Cox regression models by adjusting for potential confounders identified by univariate analysis (albuminemia and age-corrected Charlson comorbidity index). All analyses were performed using IBM Statistical Package for Social Sciences version 27.0 (IBM SPSS Statistics Inc. Chicago IL. USA). Statistical significance was set at P < 0.05 for all tested parameters.
Results
Clinical, demographic and nutritional characteristics of enrolled patients
In this secondary analysis, we studied 99 patients that had undergone bioimpedance spectroscopy evaluation at the time of US, of whom 64 also had information available regarding handgrip strength (Table 1). Most patients were male, and the mean (SD) age was 66 (17) years. In general, patients were highly comorbid, with only 6 (6%) having no comorbidities and 19 (19%) patients having only one comorbidity. Nutritional characteristics of the cohort, as a whole and partitioned by sex, are reported in Table 2. Thirteen patients were obese with BMI ≥ 30 kg/m2 and 2 patients were malnourished with BMI < 18.5 kg/m2. Of note, the mean value of handgrip strength in male patients was below the sex-specific cut-off value for the diagnosis of sarcopenia [4].
Correlation between quadriceps muscle thickness and nutritional variables
Table 3 reports the results of the correlation analysis between lean tissue index, quadriceps vastus intermedius thickness and quadriceps vastus intermedius thickness index, BMI, and handgrip strength. In particular, handgrip strength correlated strongly with quadriceps vastus intermedius thickness, and less strongly with quadriceps vastus intermedius thickness index. Lean tissue index showed a moderate correlation with handgrip strength and both quadriceps vastus intermedius thickness and quadriceps vastus intermedius thickness index. Body mass index was also correlated with both parameters of muscle mass. On the other hand, there was no agreement between lean tissue index and quadriceps vastus intermedius thickness index in establishing low muscle mass (Kappa 0.160 [standard error 0.096], P = 0.102).
Comparison between surviving and deceased patients
During follow-up (median 28 [IQR 19–36] months), the mortality rate was 38.4% (38/99). Eighty-four percent of the deceased patients were male. When compared to survivors, deceased patients were significantly older, had lower handgrip strength and lower quadriceps vastus intermedius thickness index (Supplementary Table 1). Lean tissue index, which is a proxy of total body muscle mass, did not differ between groups. Among the deceased patients, the prevalence of sarcopenia based on low lean tissue index was lower than that based on low quadriceps vastus intermedius thickness index, but this difference did not reach statistical significance (30% vs. 52%, P = 0.09). In addition, when using muscle US to identify sarcopenic patients, the prevalence of sarcopenia among deceased patients was higher compared to that in survivors (52% vs. 18%, P = 0.002), while no difference was observed when using lean tissue index.
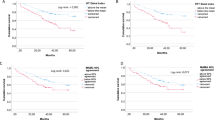
In order to assess survival in the presence of low muscle mass and low muscle strength, we fitted Kaplan–Meier survival curves by analyzing the parameters of sarcopenia either individually (Fig. 1A–C) or combined (Fig. 2A, B). When these parameters were analyzed individually, only low quadriceps vastus intermedius thickness index and low handgrip strength were associated with lower survival (Fig. 1A–C). When combined parameters of sarcopenia were analyzed, only the combination of quadriceps vastus intermedius thickness index and handgrip strength was associated with lower survival (Fig. 2A, B). At Cox regression analysis (Table 4), when handgrip strength and parameters of muscle mass were evaluated individually at univariate analysis, only low quadriceps vastus intermedius thickness index and low handgrip strength were associated with an increased hazard of death. However, this association lost significance in the adjusted model. On the other hand, when the diagnosis of sarcopenia was based on the combination of low quadriceps vastus intermedius thickness index and low handgrip strength, a greater hazard of death remained significant also in the adjusted analysis.
A–C Kaplan–Meier survival curves of patients with end-stage kidney disease on hemodialysis stratified by individual sarcopenia parameters: muscle strength assessed by handgrip (A), muscle mass assessed by quadriceps vastus intermedius thickness index (B) and lean tissue index (C). A Handgrip strength was assessed in 64 patients; B quadriceps vastus intermedius thickness index was assessed in 99 patients; C lean tissue index was assessed in 99 patients
A, B Kaplan–Meier survival curves of patients with end-stage kidney disease on hemodialysis stratified by sarcopenic status using low quadriceps vastus intermedius thickness index (A) and low lean tissue index (B) to assess low muscle mass. For both A and B, sarcopenia was diagnosed when muscle mass and muscle strength were below reference values. Because handgrip strength was available for 64 patients, in the first figure A 78 patients were included, while 21 patients were excluded because they presented low muscle mass by US, but no information regarding muscle strength. In the second figure B, 93 patients were included and 7 patients were excluded because they presented low muscle mass by lean tissue index, but no information regarding muscle strength
Discussion
The main result of this study is that the combination of low quadriceps vastus intermedius thickness index and low handgrip strength, but not the combination of low lean tissue index and handgrip strength, was associated with mortality after adjusting for relevant confounders. Importantly, neither a low quadriceps vastus intermedius thickness index as measured by US nor a low lean tissue index as measured by bioimpedance spectroscopy were independently associated with the risk of death when analyzed individually.
These findings are at variance with those of other investigators, who found that a low lean tissue index was a predictor of adverse outcomes [10, 24,25,26]. However, in another study, low lean tissue index was not significantly associated with mortality when analyzed as a single risk factor, but enhanced the risk of adverse outcomes in combination with other predictors such as inflammation or fluid overload [27].
Of note, there is a conceptual difference between US, which actually measures muscle size at a regional level, and bioimpedance spectroscopy, which estimates total body lean tissue index based on various theoretical assumptions and uses prediction equations not always validated in dialyzed patients. In fact, we found only a moderate, though significant correlation between lean tissue index and quadriceps vastus intermedius thickness index.
The reasons why we failed to detect a significant independent association between lean tissue index and mortality, in contrast to most, but not all [27], previous investigations are unclear. Because previous studies showed that low lean tissue index was especially related to increased mortality in combination with other risk factors, such as inflammation, fluid overload, or a reduced fat mass [25, 27], the lack of significance of the association between the combination of low lean tissue index and handgrip strength with mortality in our cohort was unexpected. However, since bioimpedance spectroscopy measurements were performed before the dialysis session, we cannot exclude any influence that fluid overload might have had on lean tissue index measurements. We reasoned that the difference in the prevalence of low lean tissue index between males and females found in our study (Table 1) might also be due to the relatively small sample size. In fact, another paper with a relatively small sample size found an imbalance in the prevalence of low lean tissue index between sexes [28]. Although our study cannot rule out a potential association of low lean tissue index with outcomes, especially with respect to the combination of low lean tissue index and low handgrip strength, the predictive value of the combination of low quadriceps vastus intermedius thickness index and low handgrip strength was instead robust. This suggests that combining US of the quadriceps muscle with the measurement of handgrip strength might be a powerful tool to predict outcomes in the dialysis population.
The US technique for muscle measurement has a rapid learning curve, is not time-consuming, and can also be applied at bedside or in outpatients with a portable device. In this regard, its intra-operator and inter-operator reliability and its validity against computed tomography have been reported in critically ill patients with acute kidney injury [14, 15]. In addition, previous studies showed that, as opposed to bioimpedance analysis/bioimpedance spectroscopy models [29, 30], muscle US was not influenced by the hydration status when measurements were performed before and after the dialysis session [14, 17]. While a recent study showed that US of the quadriceps muscle had greater accuracy in predicting protein-energy wasting in patients on HD compared to bioimpedance spectroscopy [11], these two techniques have not been directly compared with respect to their predictive value towards mortality in this population. Presently, an important drawback of the US muscle measurement is the absence of cut-off values. However, in a recent study, we used the median value of the distribution of quadriceps vastus intermedius thickness index stratified by sex to identify patients with low muscle mass [18]. In that study, distal quadriceps vastus intermedius thickness index below the 50th percentile was associated with the highest mortality risk in a fully adjusted model (HR 2.16, 1.27–3.69, P = 0.005) in comparison to anthropometry and other US parameters [18].
Evaluation of muscle strength is also crucial for the diagnosis of sarcopenia [4]. The screening of patients for low muscle strength has an important advantage in comparison to evaluating muscle mass, since it can be easily assessed in hospitals, outpatient settings, and community centers, by using a portable handheld dynamometer to measure grip strength. In addition, studies in elderly patients have shown that low muscle strength has a greater predictive performance towards adverse outcomes compared with low muscle mass [31]. Moreover, the rate of decrease in muscle strength is faster than the rate of muscle loss, and both are independent of the loss or gain of body weight [32]. It has been suggested that chronic kidney disease patients manifest a phenotype of accelerated aging [33], which could be magnified in patients with ESKD on HD. In the present study, handgrip strength had a positive correlation with quadriceps vastus intermedius thickness and lean tissue index, which is in agreement with earlier studies investigating the correlation between body composition and measures of physical function in HD patients [34, 35]. A positive correlation between muscle strength and muscle mass was expected because the former is partly dependent on lean tissue mass [29]. While we found that handgrip strength was a stronger predictor of mortality than muscle mass as assessed both by bioimpedance spectroscopy and US at univariate analysis, only the combination of handgrip strength with low muscle mass as assessed by US remained significantly associated with outcomes after adjusting for relevant confounders. These observations suggest that both assessments complement each other and are necessary for individualized nutritional and physical interventions.
Our study has limitations. Firstly, it is a secondary analysis of a larger study, and the smaller sample size may have diminished the power to detect an independent association of either low lean tissue index by bioimpedance spectroscopy or low muscle mass by US with mortality when these parameters were analyzed individually. Moreover, due to logistical reasons, bioimpedance spectroscopy was performed before the HD session, which might have affected lean tissue index values related to overhydration. In addition, we found an independent association with mortality of the combination of low muscle mass as assessed by US, but not by bioimpedance spectroscopy, with low muscle strength. This suggests that, combined with the measurement of handgrip strength, US may be a more sensitive tool compared to bioimpedance spectroscopy in predicting outcomes in dialysis patients. Secondly, handgrip strength data were available for only two thirds of the patients. This forced us to remove the patients with reduced muscle mass but unavailable muscle strength data from the analyses, as we could not establish the presence or absence of sarcopenia in these patients. However, notwithstanding a decrease in power, the combination of low quadriceps vastus intermedius thickness index with low handgrip strength was independently and significantly associated with adverse outcomes. Thirdly, we did not have data on subjective global assessment and malnutrition inflammation score for most patients. Pre-albumin values were also unavailable because prealbumin was not part of the routine laboratory panel of tests at the participating dialysis clinics. Thus, we could not adjust our analyses for indexes of malnutrition. However, based on BMI, albumin and C-reactive protein values, the patients enrolled in this study appeared to be in good general conditions and nutritional status, which suggests that this was a relatively selected population. Lastly, because our data were obtained in a specific group of patients with ESKD on HD, their generalization to other patient populations cannot be inferred, and a validation of the reference values applied for muscle US should be performed in patients with different diseases. Despite these limitations, to our knowledge this is the first study comparing muscle US and bioimpedance spectroscopy, combined with handgrip strength assessment, with respect to their predictive performance towards mortality in patients with ESKD on HD. In addition, our study has important potential implications for the diagnosis of sarcopenia in clinical practice.
In conclusion, in the present study the combination of low quadriceps vastus intermedius thickness index and low handgrip strength was an independent predictor of mortality in dialysis patients. In combination with handgrip strength, quadriceps muscle US outperformed bioimpedance spectroscopy in predicting mortality in this cohort. Quadriceps muscle US may be a useful technique in the assessment of sarcopenia and protein-energy wasting in patients on HD.
References
Kovesdy CP, Kopple JD, Kalantar-Zadeh K (2013) Management of protein-energy wasting in non-dialysis-dependent chronic kidney disease: reconciling low protein intake with nutritional therapy. Am J Clin Nutr 97(6):1163–1177. https://doi.org/10.3945/ajcn.112.036418
Fouque D, Kalantar-Zadeh K, Kopple J, Cano N, Chauveau P, Cuppari L et al (2008) A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int 73(4):391–398. https://doi.org/10.1038/sj.ki.5002585
Sabatino A, Cuppari L, Stenvinkel P, Lindholm B, Avesani C (2020) Sarcopenia in chronic kidney disease: what have we learned so far? J Nephrol. https://doi.org/10.1007/s40620-020-00840-y
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48(1):16–31. https://doi.org/10.1093/ageing/afy169
Giglio J, Kamimura M, Lamarca F, Rodrigues J, Santin F, Avesani C (2018) Association of sarcopenia with nutritional parameters, quality of life, hospitalization, and mortality rates of elderly patients on hemodialysis. J Ren Nutr 28(3):197–207. https://doi.org/10.1053/j.jrn.2017.12.003
Pereira R, Cordeiro A, Avesani C, Carrero J, Lindholm B, Amparo F et al (2015) Sarcopenia in chronic kidney disease on conservative therapy: prevalence and association with mortality. Nephrol Dial Transpl. https://doi.org/10.1093/ndt/gfv133
Kovesdy CP, Kalantar-Zadeh K (2009) Why is protein-energy wasting associated with mortality in chronic kidney disease? Semin Nephrol 29(1):3–14. https://doi.org/10.1016/j.semnephrol.2008.10.002
Sabatino A, D’Alessandro C, Regolisti G, di Mario F, Guglielmi G, Bazzocchi A et al (2020) Muscle mass assessment in renal disease: the role of imaging techniques. Quant Imaging Med Surg 10(8):1672–1686. https://doi.org/10.21037/qims.2020.03.05
Beaudart C, Bruyère O, Geerinck A, Hajaoui M, Scafoglieri A, Perkisas S et al (2020) Equation models developed with bioelectric impedance analysis tools to assess muscle mass: a systematic review. Clin Nutr ESPEN 35:47–62. https://doi.org/10.1016/j.clnesp.2019.09.012
Broers N, Canaud B, Dekker M, van der Sande F, Stuard S, Wabel P et al (2020) Three compartment bioimpedance spectroscopy in the nutritional assessment and the outcome of patients with advanced or end stage kidney disease: What have we learned so far? Hemodial Int 24(2):148–161. https://doi.org/10.1111/hdi.12812
Sahathevan S, Khor B, Singh B, Sabatino A, Fiaccadori E, Daud Z et al (2020) Association of ultrasound-derived metrics of the quadriceps muscle with protein energy wasting in hemodialysis patients: a multicenter cross-sectional study. Nutrients 12(11):3597. https://doi.org/10.3390/nu12113597
Fried LP, Hadley EC, Walston JD, Newman AB, Guralnik JM, Studenski S et al (2005) From bedside to bench: research agenda for frailty. Sci Aging Knowl Environ 2005(31):pe24. https://doi.org/10.1126/sageke.2005.31.pe24
Cesari M, Leeuwenburgh C, Lauretani F, Onder G, Bandinelli S, Maraldi C et al (2006) Frailty syndrome and skeletal muscle: results from the Invecchiare in Chianti study. Am J Clin Nutr 83(5):1142–1148. https://doi.org/10.1093/ajcn/83.5.1142
Sabatino A, Regolisti G, Bozzoli L, Fani F, Antoniotti R, Maggiore U et al (2017) Reliability of bedside ultrasound for measurement of quadriceps muscle thickness in critically ill patients with acute kidney injury. Clin Nutr 36(6):1710–1715. https://doi.org/10.1016/j.clnu.2016.09.029
Sabatino A, Regolisti G, di Mario F, Ciuni A, Palumbo A, Peyronel F et al (2020) Validation by CT scan of quadriceps muscle thickness measurement by ultrasound in acute kidney injury. J Nephrol 33(1):109–117. https://doi.org/10.1007/s40620-019-00659-2
Nijholt W, Scafoglieri A, Jager-Wittenaar H, Hobbelen J, van der Schans C (2017) The reliability and validity of ultrasound to quantify muscles in older adults: a systematic review. J Cachexia Sarcopenia Muscle 8(5):702–712. https://doi.org/10.1002/jcsm.12210
Sabatino A, Regolisti G, Delsante M, Di Motta T, Cantarelli C, Pioli S et al (2019) Noninvasive evaluation of muscle mass by ultrasonography of quadriceps femoris muscle in end-stage renal disease patients on hemodialysis. Clin Nutr 38(3):1232–1239. https://doi.org/10.1016/j.clnu.2018.05.004
Sabatino A, Kooman J, Di Motta T, Cantarelli C, Gregorini M, Bianchi S et al (2022) Quadriceps muscle thickness assessed by ultrasound is independently associated with mortality in hemodialysis patients. Eur J Clin Nutr 76(12):1719–1726. https://doi.org/10.1038/s41430-022-01166-7
Tillquist M, Kutsogiannis DJ, Wischmeyer PE, Kummerlen C, Leung R, Stollery D et al (2014) Bedside ultrasound is a practical and reliable measurement tool for assessing quadriceps muscle layer thickness. JPEN J Parenter Enteral Nutr 38(7):886–890. https://doi.org/10.1177/0148607113501327
Wieskotten S, Heinke S, Wabel P, Moissl U, Becker J, Pirlich M et al (2008) Bioimpedance-based identification of malnutrition using fuzzy logic. Physiol Meas 29(5):639–654. https://doi.org/10.1088/0967-3334/29/5/009
Chamney P, Wabel P, Moissl U, Müller M, Bosy-Westphal A, Korth O et al (2007) A whole-body model to distinguish excess fluid from the hydration of major body tissues. Am J Clin Nutr 85(1):80–89. https://doi.org/10.1093/ajcn/85.1.80
van Biesen W, Claes K, Covic A, Fan S, Lichodziejewska-Niemierko M, Schoder V et al (2013) A multicentric, international matched pair analysis of body composition in peritoneal dialysis versus haemodialysis patients. Nephrol Dial Transplant 28(10):2620–2628. https://doi.org/10.1093/ndt/gft296
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Psychology Press, New York
Rosenberger J, Kissova V, Majernikova M, Straussova Z, Boldizsar J (2014) Body composition monitor assessing malnutrition in the hemodialysis population independently predicts mortality. J Ren Nutr 24(3):172–176. https://doi.org/10.1053/j.jrn.2014.01.002
Marcelli D, Usvyat L, Kotanko P, Bayh I, Canaud B, Etter M et al (2015) Body composition and survival in dialysis patients: results from an international cohort study. Clin J Am Soc Nephrol 10(7):1192–1200. https://doi.org/10.2215/CJN.08550814
Hwang S, Lee J, Lee S, Kim J, Kim M, Song J (2018) Risk of overhydration and low lean tissue index as measured using a body composition monitor in patients on hemodialysis: a systemic review and meta-analysis. Ren Fail 40(1):51–59. https://doi.org/10.1080/0886022X.2017.1419963
Dekker M, Konings C, Canaud B, van der Sande F, Stuard S, Raimann J et al (2018) Interactions between malnutrition, inflammation, and fluid overload and their associations with survival in prevalent hemodialysis patients. J Ren Nutr 28(6):435–444. https://doi.org/10.1053/j.jrn.2018.06.005
Broers N, Martens R, Cornelis T, Diederen N, Wabel P, van der Sande F et al (2015) Body composition in dialysis patients: a functional assessment of bioimpedance using different prediction models. J Ren Nutr 25(2):121–128. https://doi.org/10.1053/j.jrn.2014.08.007
Konings C, Kooman J, Schonck M, van Kreel B, Heidendal G, Cheriex E et al (2003) Influence of fluid status on techniques used to assess body composition in peritoneal dialysis patients. Perit Dial Int 23(2):184–190
Lukaski H (2013) Evolution of bioimpedance: a circuitous journey from estimation of physiological function to assessment of body composition and a return to clinical research. Eur J Clin Nutr 67(Suppl 1):S2–S9. https://doi.org/10.1038/ejcn.2012.149
Leong D, Teo K, Rangarajan S, Lopez-Jaramillo P, Avezum A, Orlandini A et al (2015) Prognostic value of grip strength: findings from the prospective urban rural epidemiology (PURE) study. Lancet 386(9990):266–273. https://doi.org/10.1016/S0140-6736(14)62000-6
Delmonico M, Harris T, Visser M, Park S, Conroy M, Velasquez-Mieyer P et al (2009) Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr. https://doi.org/10.3945/ajcn.2009.28047
Kooman J, Kotanko P, Schols A, Shiels P, Stenvinkel P (2014) Chronic kidney disease and premature ageing. Nat Rev Nephrol 10(12):732–742. https://doi.org/10.1038/nrneph.2014.185
Gadaen R, Kooman J, Cornelis T, van der Sande F, Winkens B, Broers N (2021) The effects of chronic dialysis on physical status, quality of life, and arterial stiffness: a longitudinal study in prevalent dialysis patients. Nephron 145(1):44–54. https://doi.org/10.1159/000510624
Martinson M, Ikizler TA, Morrell G, Wei G, Almeida N, Marcus RL et al (2014) Associations of body size and body composition with functional ability and quality of life in hemodialysis patients. Clin J Am Soc Nephrol 9(6):1082–1090. https://doi.org/10.2215/cjn.09200913
Acknowledgements
This is a secondary analysis of a larger observational, longitudinal and prospective study for which Alice Sabatino was the recipient of a young investigator research fellowship by the Italian Society of Parenteral and Enteral Nutrition (SINPE, Società Italiana di Nutrizione Parenterale ed Enterale) for the project: “Valutazione nutrizionale nell'insufficienza renale mediante ecografia del muscolo quadricipite femorale” (“Nutritional assessment of patients with chronic kidney disease and acute kidney injury through ultrasound of the quadriceps femoris muscle”).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
The study was approved by the local Institutional Review Board (AVEN, ref. n° 45737, December 12th, 2015). The procedures were performed in agreement with the Declaration of Helsinki, and written informed consent was obtained from all participants.
Human and animal rights
The study was approved by the institutional ethics committee. This article does not contain any studies performed with animals by any of the authors.
Informed consent
Informed consent was obtained from all the patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sabatino, A., Kooman, J., Avesani, C.M. et al. Sarcopenia diagnosed by ultrasound-assessed quadriceps muscle thickness and handgrip strength predicts mortality in patients on hemodialysis. J Nephrol 37, 993–1003 (2024). https://doi.org/10.1007/s40620-023-01867-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-023-01867-7