Abstract
Background
Intradialytic hypotension (IDH) has a dramatic impact on the main outcomes of dialysis patients. Early warning of hemodynamic worsening during dialysis would enable preventive measures to be taken. Blood oxygen saturation (SO2) is used for hemodynamic monitoring in the critical care setting and may provide useful information about IDH onset.
Aim
To evaluate whether short- and medium-term variations in the SO2 signal (ST-SO2var, MT-SO2var,) during dialysis are a predictor of IDH.
Methods
In this 3-month observational cohort study, 51 hypotension-prone chronic hemodialysis (HD) patients, with vascular access by arteriovenous fistula (AVF) or central venous catheter (CVC), were enrolled. Continuous non-invasive blood SO2 was monitored (fc = 0.2 Hz) by an optical sensor on the arterial line of the extracorporeal circulation; blood pressure (every 30 min), symptoms and their time of appearance were noted. Predictive power of IDH was expressed by the area under curve (AUC) sensitivity and specificity based on intradialytic variations in SO2.
Results
A total of 1290 HD sessions were analyzed. Overall, off-line ST-SO2var analysis proved able to correctly predict IDH in 67 % of the sessions where IDH occurred. The best predictive performance was found in the presence of highly arterialized AVF (SO2 > 95 %) (75 % sensitivity; AUC 0.825; p < 0.05). On the contrary, in sessions with CVC, IDH prediction proved more efficient by MT-SO2var (AUC 0.575; p = 0.01).
Conclusions
Intradialytic SO2 variability could be a valid parameter to detect in advance the hemodynamic worsening that precedes IDH. Appropriate timely intervention could help prevent IDH onset.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preventing intradialytic hypotension (IDH) remains one of the most pressing clinical targets for the fragile uremic population [1–3]. Death risk for hypotension-prone patients is higher than for the hypotension-resistant [4, 5]. The complexity of the pathophysiologic mechanisms involved in the cardiocirculatory, hormonal and neurologic response to hemodialysis (HD) [6–8] is the main reason why valid preventative measures cannot be implemented during each session.
During the last 20 years many innovative devices able to assess, more or less continuously, some of the factors involved in the IHD genesis, such as blood volume changes [9, 10], ultrafiltration and sodium profiles [11, 12], and thermal balance [8, 13], have been proposed as a means to mitigate the incidence of IDH. However, the availability of devices providing a true IDH prediction, i.e. early identification of precise forewarning signs of IDH, is still a long way off. Since IDH is a hemodynamic phenomenon, the only way is to look for a physiological parameter in some way related to the cardiocirculatory changes occurring during the dialysis session. Moreover, given that most chronic HD patients are outpatients, non-invasive measurement is mandatory, and the cost must not weigh too heavily on the dialysis treatment overall cost [14].
Oxygen saturation (SO2) is one of the most important hemodynamic parameters measured in critically ill patients in intensive care units [15–18]. It is affected by cardiac output, hemoglobin concentration, blood oxygenation and oxygen delivery to tissues. Thus, it can be taken as a surrogate marker of the hemodynamic stability. However, apart from some isolated papers [19], there is no large study demonstrating the validity of measuring this parameter during the HD session. We previously conducted a pilot study [20] that suggested the specific value of continuously monitoring this parameter. Given the possible warning role of SO2 changes in IDH onset, a rigorously conducted larger study was needed in order to decide whether measurement of SO2 is worthwhile or not.
The aim of the present study was to evaluate the changing pattern of SO2 during HD in a large number of chronic hypotension-prone dialysis patients, thus verifying the SO2 predictive power with regard to IDH episodes.
Materials and methods
Study design
This multicenter trial (ClinicalTrials.gov Identifier: NCT01759641) was conducted according to an observational, prospective, open-label design in 18 public dialysis centers in Italy. The study lasted 3 months for each patient, and no changes in the usual dialysis prescription were introduced.
Patients
Hypotension-prone chronic HD patients (IDH events in at least 20 % of the sessions in the month before the study started) were considered eligible if they had been on a thrice-weekly standard bicarbonate dialysis for at least 6 months, and were aged between 18 and 85 years. Patients with both well-functioning arteriovenous fistula (AVF) and central venous catheter (CVC) were included.
IDH was defined, as previously reported [21], as one of the following three situations: (1) for patients starting the dialysis session with systolic arterial pressure (SAP) ≥100 mm Hg, a SAP value ≤90 mm Hg, even in the absence of any typical low blood pressure symptom; (2) in the case of patients with pre-dialysis SAP <100 mm Hg, a SAP reduction of at least 10 % % of the pre-dialysis value, accompanied by characteristic symptoms (nausea, vomiting, sweating, dizziness, yawning); (3) any SAP reduction ≥25 mm Hg compared to the pre-dialysis value, in the presence of the typical symptoms accompanying hypotension, requiring an immediate therapeutic maneuver (Trendelenburg position, saline infusion, etc.).
Exclusion criteria were: chronic obstructive pulmonary disease with documented functional respiratory deficit or needing oxygen supplementation during dialysis; hemoglobin levels lower than 10 gr/dl; poor vascular access requiring single-needle HD; routine use of any profiling and/or biofeedback system aimed to influence cardiovascular stability.
The authors acted as the treating physicians for the participants of the study. Patients did not undergo any change in their treatment. The study was illustrated to the patients by the treating physician involved in the study in each Dialysis Centre. Data were collected prospectively and were collected specifically for this study. Data treated by the persons in charge of the statistical analysis were rigorously anonymous.
Hemodialysis equipment and prescription
A Formula Therapy dialysis monitor (Bellco srl, Mirandola, MO, Italy), equipped with an optical sensor for oxygen saturation, was used in all patients. The Hemox sensor (Datamed srl, Milan, Italy) is placed just below the arterial drip chamber and before the dialyzer inlet. It measures hematocrit, oxygen saturation, and relative changes in blood volume. Its functioning has been described elsewhere [20].
Bicarbonate-buffered HD was administered to all patients. Low-flux PES membrane dialyzers, 1.7–2.2 m2, were used. Blood flow (QB) was set as usual for each patient; dialysate flow (QD) was set to 500 ml/min and the prescribed dialysis length was 240 min. Total ultrafiltration volume was set according to individual requirements. Dialysate sodium, bicarbonate, potassium, calcium, magnesium, chloride glucose and acetate concentrations, as well as the dialysate temperature, were kept as in the usual dialysis prescription. Any relevant intervention during the treatment was recorded.
Measurements and data collection
SO2 and hematocrit signals were acquired during the treatment with a frequency of 1 sample per 5 s (12 samples per minute) by means of the Hemox sensor. An example of the different behavior of SO2 during sessions is reported in Fig. 1.
Examples of the SO2 signal trend recorded during 3 different dialysis sessions involving patients with AVF (a, b) and CVC (c). In the 3 examples the SO2 signal shows different values (around 90 % in a, between 90 and 100 % in b, and lower, 50−40 % in c) and different trends: stable in a, with more or less frequent fluctuations in b and c. SO 2 blood oxygen saturation, AVF arteriovenous fistula, CVC central venous catheter
Systolic and diastolic arterial pressures (SAP, DAP) were measured before dialysis and every 30 min during treatment (automatic oscillometric sphygmomanometer). Moreover, blood pressure was measured also at any moment the patient felt unwell, or whenever there was a decreasing blood pressure trend according to the standard clinical practice. Occurrence of typical low pressure symptoms (muscular cramps, headache, dizziness, vomiting, nausea, sweating), their time of appearance, as well as any fluid infusion (saline, plasma expanders, sodium), was recorded on a case report form. Data downloaded by the dialysis monitors were stored and analyzed in a PC equipped with Matlab 7.8 and NCSS.
Data analysis
Arterial pressure and symptoms were analyzed off-line in order to correctly define acute hypotension episodes. Sessions with at least one hypotensive episode were classified as “positive”, while dialysis sessions with no IDH episodes were classified as “negative”. Two methods were developed to extract information from the SO2 signal: the first evaluates the short-term variability of SO2 (ST-SO2var), while the second one is based on SO2 variations in the medium term (MT-SO2var). ST-SO2var was quantified by computing every minute the SO2 standard deviation (SO2SD) over a 5-min- long window. MT-SO2var was quantified every minute as the difference (∆SO2) between the current mean SO2 (computed over a 30-min long window, according to Cordtz et al. [19]) and the initial mean SO2 [22].
In the ST-SO2var analysis, the first 10 min of each session were discarded, as generally done in studies concerning hemodynamics during hemodialysis in order to avoid artifactual oscillations related to connecting the patient to the extracorporeal circuit or initial instabilities (see, for example, artifactual very low SO2 starting values in Fig. 1, panels a and b). To define the SO2 short-term variability the standard deviation (SD) was computed. During the course of the session, SD was calculated over short time series composed of 60 SO2 values (5 min). Each time series was extracted from the overall signal by means of a shifting window producing epochs overlapping by 80 % (1 min time-shift). As a result, an SD value is computed every minute based on the 5-min interval ending in that minute. In each epoch, the outliers were identified and discarded according to the “box and whisker” scheme [23].
In the MT-SO2var method, after discarding the first 10 min, epochs 30-min in length (1 min time-shift) were selected. The mean value in the first epoch was assumed as the reference value (initial SO2). In each epoch, the mean value of SO2 was computed and a difference (∆SO2) between that value and the initial SO2 was calculated.
For both methods a binary classifier was then elaborated, assuming SO2SD or ∆SO2 as the test variable and comparing it with a threshold value throughout each session.
In “positive” sessions, the analysis was truncated when a hypotension episode occurred; if more than one episode occurred in one session the analysis was truncated at the first of such episodes. All the 12 SO2 measurements in the minute corresponding to a hypotension episode were discarded. In “negative” sessions, the last 30 min were discarded because the indexes could predict a possible instability that does not occur simply because the session ends leading to an overestimation of false negative sessions. In each session complicated by hypotension, the alarm time (AT) was defined as the time from the first threshold crossing (SO2_first) to the actual time of hypotension occurrence (IDH_onset).
Finally, in order to examine the impact of the different vascular accesses on the predictive power of the SO2 temporal variations, we stratified sessions on the basis of the patients’ vascular access, i.e. AVF or CVC.
Statistical analysis
Receiver operating characteristic (ROC) curve analysis was run to define the predictive power of the SO2 temporal variations and to identify a threshold leading to a good compromise between sensitivity and specificity in the IDH prediction. To evaluate SO2SD and ∆SO2 specificity and sensitivity, it was necessary to assess the number of correct and incorrect classifications by comparing the test results with the off-line classification. Contingency tables and confidence intervals were calculated for any discrete threshold value obtained from the ROC curves, and the z test was used to compare two areas under the curve (AUCs) [24].
Results
Fifty-one out of 90 screened patients from 18 dialysis units were admitted to the study according to the inclusion and exclusion criteria (Table 1). Out of 1580 dialysis sessions recorded, 290 (18 %) were discarded due to incomplete data collection, resulting in a total number of 1290 sessions analyzed.
Blood flow (QB) was 292 ± 16 ml/min, dialysate flow (QD) 500 ml/min, dialysate temperature 36.5 ± 0.4 °C; dialysis session length was 230 ± 10 min. The total ultrafiltration volume proved to be 3.0 ± 0.8 l per session, corresponding to an ultrafiltration rate of 751 ± 202 ml/h. The average dialysate total conductivity was 14.1 ± 0.3 mS/cm, bicarbonate conductivity 3.0 ± 0.1 mS/cm, K+ 2.9 ± 0.2 mmol/l, Ca++ 1.45 ± 0.15 mmol/l, Mg++ 0.6 ± 0.1 mmol/l, Cl− 109 + 0.1 mmol/l, Na+ 139.9 ± 0.9 mmol/l, CH3COO− 3 mmol/l, glucose 1 g/l.
On the basis of off-line analysis of the arterial blood pressure, 273 (21 %) sessions were classified as positive (i.e. complicated by hypotension) and 1017 (79 %) as negative (no hypotension). The SO2 signal time course was found to be affected by the patients’ hemodynamic behavior. During sessions with hypotension two different patterns were observed (Fig. 2): either an increase in the SO2 SD or a slow decrease in the ∆SO2. In sessions without hypotension, instead, the SO2 signal was found to be substantially stationary (Fig. 2).
Exemplifying cases of dialysis sessions complicated by intradialytic acute hypotension (panels a and b) and an example of a session with stable blood pressure (panel c). Each column depicts systolic and diastolic blood pressure (BP), SO2 signal, SO2 SD and ∆SO2, as indexes of short-term variability and medium-term variations. An arrow and a diamond marker are placed at the point of hypotension onset. In a and b, hypotension is preceded, respectively, by a marked increase in SO2 SD and a slow decrease in ∆SO2. On the contrary, in the session without hypotension (panel c) the SO2 signal remains stationary, with a minimal short-term variability (SO2 SD around zero) and restrained medium-term variations (∆SO2)
To evaluate the predictive potential in terms of sensitivity and specificity of SO2 changes, ROC curves were used. The efficacy in correctly predicting hypotension events based on ST-SO2var as well as on MT-SO2var is reported in Fig. 3 (panels a and b, respectively). In panel a, the total area under the curve (AUC) was 0.652 [95 % confidence interval (CI95 %) 0.615–0.687], indicating a significant prediction power of ST-SO2var. The binary test based on a threshold equal to 1.95 % (circle in Fig. 3, panel a) correctly recognized 182/273 sessions with hypotension (sensitivity 67 %, CI95 % 61–73) and 618/1017 hypotension-free sessions (specificity 61 %, CI95 % 58–64). The hypotension onset time was 130 ± 46 min and the alarm time (AT), calculated by ST-SO2var, was 89 ± 51 min. The MT-SO2var predictive power was also significant, as shown by the ROC curve in Fig. 3, panel b, with AUC equal to 0.625 (CI95 % 0.587–0.663). Upon choosing a threshold for MT-SO2var variations equal to −1.14 %, 155/273 sessions with hypotension (sensitivity 57 %, CI95 % 51–63), and 627/1017 stable sessions (specificity 62 %, CI95 % 59–65) were correctly predicted. AT was shorter than that previously obtained by ST-SO2var and equal to 66 ± 43 min.
ROC curves for hypotension detection based on short- (panel a) and medium-term (panel b) SO2 variability. In the short-term variability analysis, the area under the curve (AUC) was 0.652 (CI 95 % 0.615–0.687). To obtain a good compromise between sensitivity (S) and specificity (Sp), the threshold value was chosen equal to 1.95 %. In the medium-term variation analysis, the AUC was 0.625 (CI 95 %, 0.587–0.663) and the threshold chosen as a good compromise between sensitivity and specificity was −1.14 %. Sensitivity (S) and specificity (Sp) are shown for SO2 SD (expression of short-term variability) and ∆SO2 (expression of medium-term variations) threshold values equal to 1.95 and −1.14 %, respectively (grey circles). ROC receiver operating characteristic, AUC area under the curve. For other abbreviations, see previous figures
In order to assess if the choice of excluding from the analysis the last 30 min of data in the sessions without hypotension significantly affected the results, we repeated the analysis including the last 30 min of data. The results did not change significantly; the AUC for ST-SO2var and MT-SO2var were, respectively, AUC = 0.65 (CI95 % 0.613–0.685) and AUC = 0.622 (CI95 % 0.58–0.66). Moreover, in order to exclude that different fistula blood flow rates could influence the values of the SO2-derived parameters (SO2 SD and ∆SO2), we analyzed a subset of dialysis sessions in which the blood flow rate was changed during the session (range 150–400 ml/min) and we did not find any correlation (p > 0.05, R2 < 0.2).
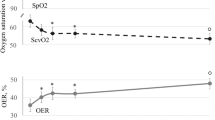
Concerning the predictive performance of SO2 according to vascular access (AVF or CVC), ST-SO2var analysis (Fig. 4a) slightly increased the AUC value when applied to the AVF group vis-à-vis all patients, though without reaching significance (AUCAVF = 0.664, NS). On the contrary, predictive power was reduced in the CVC group (AUCCVC = 0.575, p = 0.01). Moreover, in patients with AVF and a high percentage of arterial blood, witnessed by initial values of SO2 ≥95 %, the improvement was significant in comparison to the whole data set (AUC≥ 95 = 0.739, p = 0.03, Table 2). In this case, the best compromise between sensitivity and specificity resulted in a SO2SD threshold equal to 1.67 % (SS = 71 % CI95 % 59–83, Sp = 67 % CI95 % 61–73). The resulting AT was 102 ± 53 min. In sessions with the highest SO2 initial values (≥97 %), the ST-SO2var predictive power further increased (Table 2; Fig. 4a): at an SO2SD cut-off value of 1.68 % both sensitivity and specificity reached 75 % (CI95 % 58–92 and 68–82, respectively). In this case, the AT decreased to 93 ± 55 min.
ROC curves for hypotension prediction based on SO2 short- (a) and medium-term (b) variations, depending on the vascular access. AVF arteriovenous fistula, CVC central venous catheter, SO 2_I , initial SO2. See Table 2 for AUC values
On applying MT-SO2var analysis to the AVF and CVC subgroups, hypotension prediction proved better in the CVC than in the AVF group (Fig. 4b). In the CVC group, setting a threshold equal to −2.78 %, sensitivity was 62 % (CI95 % 54–70) while specificity was 62 % (CI95 % 57–67), AT further reduced to 58 ± 40 min.
Discussion
This study shows that the variations in the SO2 signal measured on the extracorporeal blood during HD are associated with IDH and could have predictive value for its onset, especially in patients with a highly arterialized fistula (SO2 > 95 %). Intradialytic acute hypotension events are often sudden and unpredictable, although in clinical practice skilled nurses may sometimes predict IDH on the basis of slight clinical changes (paleness, drowsiness, yawning). However, elderly and comorbid patients, with blunted cardiovascular and neurohormonal reflexes, may present sudden hypotension without any warning signal, even at a modest ultrafiltration volume [25]. Very early information about worsening in the cardiocirculatory response to dialysis would be of great value, making it possible to carry out preventive measures. Even continuous intra-dialytic blood volume (BV) monitoring, initially proposed as a useful variable for predicting blood pressure (BP) instability [9, 10], may provide contradictory information, because of its not univocal behavior [26, 27].
In this cultural wasteland surrounding IDH prevention, by way of looking for a meaningful “new” hemodynamic parameter, we decided to study and continuously measure SO2, partly because of the availability of a dedicated sensor measuring O2 saturation directly in the blood [20]. Cardiovascular instability and decreasing BP may negatively affect both macro- and micro-circulation [28] and consequently the gas exchanges at a tissue level, thus resulting in a variation in SO2. In the critical care setting, the so-called “mixed venous oxygen saturation” (SvO2), is a crucial parameter for hemodynamic monitoring [15–18]. However, its use is limited because of the need for a pulmonary artery catheter. A good correlation has been demonstrated between SvO2 and SO2 measured in blood from a central vein [29]. Thus, SO2 measured on central venous blood sampling may represent a surrogate marker of cardiac output [18]. Moving to the specific context of dialysis, continuous non-invasive monitoring of SO2 in hypotension-prone patients with a CVC might be a convenient and simple way to evaluate the cardiac output dynamics in response to dialysis. By contrast, SO2 measured in blood from an AVF is mainly affected by the mixing of arterial and venous blood which determines the final saturation. Arterialization implies that SO2 in an AVF is highly affected by the respiratory function. In a dynamic situation like the HD session, where biochemical as well as hemodynamic and respiratory phenomena are continuously changing, the instant value of SO2 is likewise expected to change frequently in the short term.
In effect, in our study the association with IDH was stronger for SO2 short-term variability in sessions with an AVF, and for SO2 medium-term variations in sessions with a CVC. About this discrepancy, we can only conjecture, bearing in mind the different implications of SO2 measured in the arteriovenous blood of an AVF or in blood drawn from the right atrium with a CVC. In highly arterialized AVFs, the presence of a high percentage of arterial blood may cause a rapid change in SO2 when hypovolemia appears. In this situation, an analysis like SO2 short-term variability is probably the kind that may best capture the rapid hemodynamic phenomena. Thus, the sensitivity of ST-SO2var improves with the O2 concentration increase, an expression of the degree of arterialization.
Instead, in pure venous blood from a CVC, SO2 changes are slower and belated, probably because central SO2 suffers the consequences of peripheral O2 extraction. The slow reduction in SO2 might reflect a progressive intradialytic decrease in cardiac output, leading to acute hypotension and tissue hypoperfusion, with consequent high O2 extraction by the tissues and a decrease in central SO2.
Hence, when considering blood from a CVC, the SO2 variations may be captured best with an analysis working on the slow variation, in agreement with observations by Cordtz et al. [19], but with a different mathematical analysis based on the vascular access. Likewise, Solem et al. [30], predicted the importance of measuring oxygen saturation in HD. However, this study, carried out on few sessions and patients, is based on a pulse oximetry device, a tool which, though non-invasive, is not well tolerated by patients because it has to be clipped onto the fingers of the hand contralateral to the vascular access, thus impeding movements. Moreover, a pulse-oximeter placed on a fingertip is highly affected by vascular stiffness, and can thus provide unreliable measurements. By contrast, our data were obtained by a completely non-invasive optical sensor placed on blood lines, not irritating to the patient and not affected by signal distortion due to the pathology of the peripheral vascular tree. In our analysis we did not find any patient-specific factor related to failed measurements by the SO2 sensor. They were only related to some offset affecting the sensor/measurement system, which caused “saturation” of the signal to a constant, artifactual, 100 % value.
Another strength of our study is the large number of hypotension-prone patients involved and the high number of dialysis sessions studied (nearly 1300). It is well known that even hypotension-prone patients do not present IDH in all their dialysis sessions. Having studied both “positive” and “negative” HD sessions (with or without IDH) enabled us to verify the merits as well as shortcomings of SO2 and its association with IDH onset. Our method proved able to provide information as to the hypotension risk associated with each individual session of a given patient. This is a more clinically relevant target than simple recognition of hypotension-prone and hypotension-resistant patients, as already achieved in previous studies [19].
Although the estimated global predictive performances are promising, there is room for improvement. The first problem to face is striking the most appropriate compromise between sensitivity and specificity. In clinical practice this means the possibility to tune the acceptable rate of any false alarms. Obviously, by increasing the alarm threshold it would be possible to decrease the total number of unnecessary interventions at the cost of reducing the percentage of correct predictions.
Inevitably, due to the multifactorial nature of IDH, a single parameter could never have absolute predictive capacity and an AUC >0.8 is generally required for clinical relevance. For this reason, SO2 variability analysis could be integrated into a multiparameter control system, managing other variables as well, such as heart rate or BV changes, with a view to overall hemodynamic monitoring.
The main limitation of our study is that some important measurements like cardiac output and peripheral vascular resistance could not be measured.
In conclusion, SO2 variability would seem to stand confirmed as a parameter associated with hypotension events during HD, albeit with specific differences based on the vascular access type (AVF or CVC). Larger studies are warranted to confirm these results and investigate the predictive power of SO2 behavior on hypotension onset, reduction of which could positively impact on morbidity and mortality.
References
Mancini E, Mambelli E, Irpinia M, Gabrielli D, Cascone C et al (2007) Prevention of dialysis hypotension episodes using fuzzy logic control system. Nephrol Dial Transplant 22:1420–1427
Palmer BF, Henrich WL (2008) Recent advances in the prevention and management of intradialytic hypotension. J Am Soc Nephrol 19:8–11
Agarwal R (2012) How can we prevent intradialytic hypotension? Curr Opin Nephrol Hypertens 21:593–599
Shoji T, Tsubakihara Y, Fujii M, Imai E (2004) Hemodialysis-associated hypotension as an independent risk factor for 2-year mortality in hemodialysis patients. Kidney Int 66:1212–1220
Tisler A, Akocsi K, Borbas B, Fazakas L, Ferenczi S et al (2003) The effect of frequent or occasional dialysis-associated hypotension on survival of patients on maintenance haemodialysis. Nephrol Dial Transplant 18:2601–2605
Daugirdas JT (2001) Pathophysiology of dialysis hypotension: an update. Am J Kidney Dis 38:S11–S17
Cavalcanti S, Ciandrini A, Severi S, Badiali F, Bini S et al (2004) Model-based study of the effects of the hemodialysis technique on the compensatory response to hypovolemia. Kidney Int 65:1499–1510
Selby NM, McIntyre CW (2006) A systematic review of the clinical effects of reducing dialysate fluid temperature. Nephrol Dial Transplant 21:1883–1898
Paolini F, Mancini E, Bosetto A, Santoro A (1995) Hemoscan: a dialysis machine-integrated blood volume monitor. Int J Artif Organs 18:487–494
Steuer RR, Leypoldt JK, Cheung AK, Senekjian HO, Conis JM (1996) Reducing symptoms during hemodialysis by continuously monitoring the hematocrit. Am J Kidney Dis 27:525–532
Donauer J, Kolblin D, Bek M, Krause A, Bohler J (2000) Ultrafiltration profiling and measurement of relative blood volume as strategies to reduce hemodialysis-related side effects. Am J Kidney Dis 36:115–123
Moret K, Aalten J, van den Wall BW, Gerlag P, Beerenhout C et al (2006) The effect of sodium profiling and feedback technologies on plasma conductivity and ionic mass balance: a study in hypotension-prone dialysis patients. Nephrol Dial Transplant 21:138–144
Maggiore Q, Pizzarelli F, Santoro A, Panzetta G, Bonforte G et al (2002) The effects of control of thermal balance on vascular stability in hemodialysis patients: results of the European randomized clinical trial. Am J Kidney Dis 40:280–290
Locatelli F, Buoncristiani U, Canaud B, Kohler H, Petitclerc T et al (2005) Haemodialysis with on-line monitoring equipment: tools or toys? Nephrol Dial Transplant 20:22–33
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A et al (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
Secher NH, Van Lieshout JJ (2005) Normovolaemia defined by central blood volume and venous oxygen saturation. Clin Exp Pharmacol Physiol 32:901–910
Bauer P, Reinhart KBM (2008) Significance of venous oximetry in the critically ill. Med Intensiva 32(33):134–142
Perner A, Haase N, Wiis J, White JO, Delaney A (2010) Central venous oxygen saturation for the diagnosis of low cardiac output in septic shock patients. Acta Anaesthesiol Scand 54:98–102
Cordtz J, Olde B, Solem K, Ladefoged SD (2008) Central venous oxygen saturation and thoracic admittance during dialysis: new approaches to hemodynamic monitoring. Hemodial Int 12:369–377
Mancini E, Corazza L, Soverini ML, Cannarile DC, Cavalcanti S et al (2008) Short-term variability of oxygen saturation during hemodialysis is a warning parameter for hypotension appearance. Comput Cardiol 35:881–883.
Santoro A, Mancini E, Basile C, Amoroso L, Di Giulio S et al (2002) Blood volume controlled hemodialysis in hypotension-prone patients: a randomized, multicenter controlled trial. Kidney Int 62:1034–1045
Perazzini C, Bolasco P, Corazza L, Tramonti M, Mancini E et al (2013) Prediction of intradialytic hypotension based on oxygen saturation variations. Comput Cardiol 40:1223–1226.
McGill R, Tukey JW, Larsen WA (1978) Variations of boxplots. Am Stat 32:12–16
Zhou X, Obuchowski N, McClish D (2002) Statistical methods in diagnostic medicine. Wiley, New York, p 185
Santoro A, Mancini E (2010) Hemodialysis and the elderly patient: complications and concerns. J Nephrol 23(Suppl 15):S80–S89
Santoro A, Mancini E (1997) Clinical significance of intradialytic blood volume monitoring. Int J Artif Organs 20:1–6
Dasselaar JJ, Huisman RM, de Jong PE, Franssen CF (2005) Measurement of relative blood volume changes during haemodialysis: merits and limitations. Nephrol Dial Transplant 20:2043–2049
Santesson P, Danielsson A, Iseda I, Adamson U, Lins PE et al (2010) Impaired peripheral micro- and macrocirculation during hemodialysis in uremic patients. Int Angiol 29:362–370
Berridge JC (1992) Influence of cardiac output on the correlation between mixed venous and central venous oxygen saturation. Br J Anaesth 69:409–410
Solem K, Olde B, Sornmo L (2010) Prediction of intradialytic hypotension using photoplethysmography. IEEE Trans Biomed Eng 57:1611–1619
Acknowledgments
The authors would like to thank Fabio Grandi, Maria Luigia Colucci and Nicoletta Pergoloni for their help. This work was partially supported by the grants of the project Optimization of Dialysis with Artificial Kidney (POR-FESR - Regione Emilia Romagna).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
LC and MA are employes of the Company producing the dialysis machine used in the study. They only had a role of technical support in the use of the sensor and the machine. The other authors have declared that no competing interests exist.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
All the patients gave their informed consent before entering the study.
Additional information
E. Mancini and C. Perazzini contributed equally to this work.
Rights and permissions
About this article
Cite this article
Mancini, E., Perazzini, C., Gesualdo, L. et al. Intra-dialytic blood oxygen saturation (SO2): association with dialysis hypotension (the SOGLIA Study). J Nephrol 30, 811–819 (2017). https://doi.org/10.1007/s40620-016-0346-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-016-0346-x