Abstract
Purpose
Craniopharyngiomas (CPGs) are aggressive brain tumors responsible of severe morbidity in children. The best treatment strategies are under debate. Our study evaluates surgical, pituitary, and hypothalamic outcomes of a tailored staged-surgical approach compared to a single-stage radical approach in children with CPGs.
Methods
Multicenter retrospective study enrolling 96 children treated for CPGs in the period 2010–2022. The surgical management was selected after a multidisciplinary evaluation. Primary endpoint includes the inter-group comparison of preservation/improvement of hypothalamic–pituitary function, the extent of resection, and progression-free survival (PFS). Secondary endpoints include overall survival (OS), morbidity, and quality of life (QoL).
Results
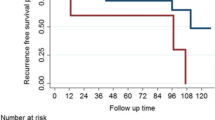
Gross Total Resection (GTR) was reached in 46.1% of cases in the single-stage surgery group (82 patients, age at surgery 9 ± 4.7 years) and 33.3% after the last operation in the staged surgery group (14 patients age 7.64 ± 4.57 years at first surgery and 9.36 ± 4.7 years at the last surgery). The PFS was significantly higher in patients addressed to staged- compared to single-stage surgery (93.75% vs 70.7% at 5 years, respectively, p = 0.03). The recurrence rate was slightly higher in the single-stage surgery group. No significant differences emerged in the endocrinological, visual, hypothalamic outcome, OS, and QoL comparing the two groups.
Conclusions
In pediatric CPGs’ surgical radicality and timing of intervention should be tailored considering both anatomical extension and hypothalamic–pituitary function. In selected patients, a staged approach offers a safer and more effective disease control, preserving psychophysical development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Craniopharyngioma (CPG) is a benign, slow-growing tumor of the suprasellar region (WHO grade I neoplasm), which accounts for about 4–10% of primary intracranial neoplasm [1, 2], being the most frequent non-neuroepithelial pediatric brain tumor. While the papillary form is more common in adults, the adamantinomatous histological variant shows a twin peak in its age distribution (5–15 years and 45–60 years) [3]. The reported 5-year overall survival ranges between 55% and 85% [4]. Adamantinomatous CPG has high rates of morbidity and mortality due to its aggressive behavior toward important surrounding neurovascular structures and its propensity to recur after surgery [5]. Current treatment strategies are still debated, including both gross total resection (GTR) in patients with favorable tumor localization as well as subtotal resection (STR) to preserve hypothalamic and visual functions. Recently, the adjuvant radiotherapy (RT) technique following STR resection has been proposed, with the aim of improving disease control [6,7,8,9,10]; however, its potential consequences on hypothalamic function, neurological and psychological development, and the risk of radiating-induced neoplasms should be considered [11, 12].
We conducted an international multicenter study aiming to analyze the implications of single-stage versus staged surgery on endocrinological and visual outcomes, overall survival (OS), progression-free survival (PFS), and quality of life (QoL) in children affected by CPG.
Materials and methods
Study design and cohort of study
This is a multicentric, retrospective, cohort study. Consecutive pediatric patients (≤ 18 years old at the time of surgery) with a histopathological diagnosis of CPG, treated by means of endoscopic endonasal transsphenoidal surgery (EETS) and microsurgical transcranial approach (MTA) from 2000 to 2021, in four European referral tertiary Centers (University of Insubria-ASST Sette Laghi, Varese; Institute of Neurosurgery-Catholic University Medical School, Rome; IRCCS Istituto Giannina Gaslini, Genoa; and Saarland University Homburg), were screened for enrollment. Clinical and radiological data were retrieved from the local institutional databases, medical records, outpatients’ evaluations, and questionnaires administered to the patients during the follow-up (Supplementary material). Major criteria of exclusion were patient > 19 years old, unavailability of a complete clinical and surgical data, and follow-up at last treatment < 6 months. When available, a revision of the surgical videos was conducted. Demographic features (age at surgery, sex), radiological features, endocrinological and neurological status, previous treatments, type of surgical approach, histopathology, and long-term complications are summarized in Table 1.
Endocrinological, visual, and functional assessment
Patients underwent an extensive endocrinological assessment to evaluate the pre-and post-operative hypothalamic–pituitary axis (HPA). Baseline pituitary function was assessed at diagnosis, at 3 and 6 months after surgery and then every 12 months; and included blood tests to investigate the somatotropic axis [somatomedin (IGF-1) and growth hormone (GH)], gonadial axis [follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol for girls and testosterone for boys, in several cases anti-Mullerian hormone or inibinB], prolactin (PRL), thyroid function [thyroid stimulating hormone (TSH), free thyroxine (FT4), free triiodothyronine (FT3)], adrenal axis [cortisol, adrenocorticotropin hormone (ACTH)], and the indirect evaluation of desmopressin secretion (plasmatic and urinary osmolarity, urinary specific gravity, and plasmatic electrolytes) [13,14,15,16,17]. In selected cases, the insulin tolerance provocative test (ITT) was performed for GH and ACTH axis assessment [18, 19]. Despite patient’s enrollment required a quite long period during which applied laboratory techniques evolved, however, tests had high sensibility. The endocrinological investigation used in the evaluation of the hypothalamic–pituitary–adrenal axis is highlighted in Supplementary Table.
Anthropometric data [weight (kg), eight (centimeters), height velocity and growth curves, genetic target (based on the calculation of the mid parental height), arm span, waist circumference (centimeters), body mass index (weight/height2)], pubertal stages (Tanner stages), and bone age (applying the Greulich and Pyle atlas) were collected in most of the patients at diagnosis and during follow-up at scheduled outpatient evaluation [20, 21]. Hypothalamic dysfunction (HD) included eating disorders, sleep disturbance, temperature dysregulation, and/or behavior change. A complete ophthalmological analysis, with both visual acuity and visual field examinations, was performed by skinned ophthalmologists.
Radiological evaluation
Radiological assessment included multiplanar computed tomography angiography (CTA) scan, contrast-enhanced magnetic resonance images (MRI), and magnetic resonance angiography (MRA). Digital Imaging and Communications in Medicine (DICOM) files were uploaded on a dedicated software (Osirix; Pixmeo SARL©, Bernex, Switzerland). The following tumoral features were collected: size, consistency (solid, cystic, mixed), location according to diaphragm sellae position (infra-diaphragmatic or supradiaphragmatic), ventricular invasion, parasellar extension, optic apparatus, and vascular encasement. Tumoral volumetric measures were quantified based on preoperative isotropic T1 + images at MRI scan, using the software mentioned above (Osirix; Pixmeo SARL©, Bernex, Switzerland).
Surgical management
The surgical strategy (including timing and type of surgical intervention) was planned in each center by a dedicated multidisciplinary board leaded by experienced pediatric endocrinologists, pediatric neurosurgeons, and neuropsychologists. Other specialists involved in the decision-making process were neuroradiologists, ophthalmologists, and otorhinolaryngologists. A multidisciplinary board made decisions on surgical scheduling based on pre-operative hypothalamic–pituitary state and radiological characteristics in accordance with a standard procedure across the involved Centers (Fig. 1). Indications for surgery included hydrocephalus, acute or progressing visual disturbances, hormonal deficiency, mass effect, and worsening neurological symptoms. The choice of the surgical approach and the access route (endoscopic endonasal or microsurgical) depended on the intrinsic features of the tumor (location, size, consistency, extension, neurovascular encasement), the surgeon’s preferences (according to personal experience, safeness, comfort on the performing the procedure), and hypothalamic–pituitary axis preservation.
Flowchart summarizing the risk-based treatment algorithm for pediatric craniopharyngiomas. CPG Craniopharyngioma; CT computed tomography; MRI magnetic resonance image; EVD external ventricular drainage; VAD ventricular access device; GH growth hormone; LH luteinizing hormone; FSH follicle-stimulating hormone; GTR gross total resection; STR subtotal resection; IFN interferon; RT radiotherapy
Patients with a normal preoperative pituitary function, taking account of the above-mentioned intrinsic characteristics of the lesion, underwent a staged approach (S group) with the aim of preserving the normal hormonal status, the regular child psychophysical and physical growth, before scheduling a more radical resection (Fig. 2). All the other patients were selected for a single-stage surgical treatment (SS group) (Fig. 3).
A case treated according to the principles of the “Staged surgery”. A 9-year-old boy affected by a cystic suprasellar CFG extended into the third ventricle (A, B). Considering the normal function of his hypothalamic–hypophyseal axis, he was addressed to a staged surgery with intentional endoscopic transcranial STR and Ommaya catheter insertion. He was kept under clinical radiological observation. Postoperatively, he was functionally independent and hormonal axis was normal. Three years later, for the progressive growth of the tumor (C, D), he underwent a reoperation with EETA and GTR. A 6-month MRI showed a persistence of a suprasellar cystic lesion (E, F) and gamma knife RT was administered. During the 3 years later, a progressive shrinkage of the lesion was observed and there was no presence of the tumor or further disease progression at last follow-up (G, H). He is currently on replacement therapy for diabetes insipidus and growth hormone deficiency, but he is attending school with excellent results
A case treated according to the principles of “single-stage” surgical treatment. A 13-year-old boy with panhypopituitarism due to a suprasellar craniopharyngiomas extended into the third ventricle and involving the pituitary stalk (A, B) underwent an extended endoscopic endonasal approach with gross total resection and resection of pituitary stalk (C, D) as confirmed on the 3-month post-operative MRI
The staged surgery group (S) was named S_1 (at the first operation) and S_F (at the last operation). Regarding the tumor extension, Yasargil classification system [22] was used in every case to aid surgical planning, while Kassam classification was employed only for tumors treated via endoscopic endonasal transsphenoidal approach [23]. GTR was defined as the absence of any residual mass, subtotal (STR), and partial resection (PR) corresponded, respectively, to the 51–90% and 10–50% of tumor removal.
Follow-up
Brain MRI with Gadolinium was planned 3 months after surgery and then every 1 or 2 years. All subjects underwent periodical clinical and biochemical assessment by a dedicated team of endocrinologists (as previously described) and ophthalmological examinations. In all the centers, quality of life was assessed on the basis of the Karnofsky Performance Status scores. In one center, specific questionnaires were used to assess five age-related domains: physical function, emotional well-being, cognitive function, and behavior (including eating behavior and sleep–wake rhythm). The Child Behavior Checklist (CBCL) was used to detect behavioral and emotional impairment, social relations, and school and total competence. The “Identification of problematic eating behaviors” scale was used to assess eating disorders, while the sleep–wake diary was used to evaluate sleep–wake rhythm. The specific questionnaires were fulfilled by patients with family support. Time to recurrence (TTR) was defined as the time from the curative surgery (respectively, the only operation in the single-stage surgery group and the last operation in case of staged surgery) to recurrence.
Statistical analysis
Continuous variables were described as mean values ± Standard deviation (SD). Differences between groups were measured by Student’s t test for continuous variables and by the Chi-square test for categorical variables. P value was set at 0.05 for a significant difference. Survival analysis was achieved using Kaplan–Meier survival plots and log-rank analysis. Cox regression multivariate analysis included sex, pre- and post-operative hypothalamic dysfunction (HD), pre- and post-operative diabetes insipidus, and extent of resection (EOR). Statistical analyses were performed using the statistical program SPSS version 27 (IBM, Armonk, NY, USA).
Results
Pre-operative evaluation
Our cohort consisted of 96 patients (54 male and 42 female), divided into two groups: single-stage surgery (n = 82, mean age 9 ± 4.47 SD) and staged surgery (n = 14, mean age 7.64 ± 4.57 SD at the first operation). Sex distribution and mean age at surgery were not statistically different comparing the two cohorts (respectively, SS vs S_1 p = 0.29 and SS vs S_F p = 0.78) (Table 1). All the CPGs in our cohort had an adamantinomatous histotype. Mean hospitalization duration was 17 ± 34 days (range 7–37).
The percentage of patients suffering from hydrocephalus (SS vs S_1, p = 0.38), neurological symptoms (SS vs S_1, p = 0.18), visual field defects (p = 0.83), and hypothalamic dysfunction (p = 0.53) was not statistically different comparing single-stage group with staged surgery group before the first surgery. Similar results emerged comparing SS group with staged surgery group before the last planned surgery.
No significant differences emerged in the presence of diabetes insipidus (DI), which was diagnosed, respectively, in 13 (15.9%) and 2 (14.3%) patients in groups SS and S_1 and 3 (21.4%) cases in group S_F (inter-group comparison p = 0.85). Hormonal serum tests in the single-stage group revealed a condition of multiple pituitary hormone deficiencies (MPHD) in 36 (43.9%) patients, panhypopituitarism in 9 (11%), and normal pituitary function in the remaining. In the S_1 group, nine patients were eupituitaric and five were diagnosed with MPHD, and no patients presented with panhypopituitarism. In the group S_F, 6 (42.9%) patients had MPHD and 2 (14.3%) had panhypopituitarism preoperatively. The incidence of pituitary deficiency, including GH deficit, was not significantly different among the three groups (p = 0.54). Mean tumor volume was not different comparing single-stage group (21.71 ± 22.94 cm3) with the stage surgery group before the first surgery (23.82 ± 22.27 cm3, p = 0.75), neither before the last surgery (19.76 ± 20.88 cm3, p = 0.78). No differences in histological subtypes’ frequency or in the presence of calcifications were detected (Table 1).
Post-operative results
Pituitary function
In the single-stage group, DI resolved in 23% of cases and appeared de novo in 40 patients (58% of the 69 cases without pre-operative DI), without a significant variation comparing pre- vs post-surgical incidence (p = 0.19). In the staged surgery group, two patients had pre-operative DI, which resolved in one, while two patients developed DI after the first surgery. One of the three patients affected by DI after the first surgery recovered after the second surgery, but two additional patients developed DI (DI incidence pre- vs post-surgery p = 0.17). With the limitation of the small sample size, in the inter-group comparison (SS vs S), the rate of new-onset post-operative DI was slightly higher after the single operation in the single-stage group compared to the outcome of the multiple-stage surgery group (p = 0.06) (Table 2).
In the SS group, after surgery 31 patients (37.8%) had panhypopituitarism, 38 patients (46.3%) had MPHD, and the remaining had a normal pituitary function (Table 2). Among the 37 children who preoperatively had normal pituitary function, 28 developed a pituitary hormone deficiency (16 MPHD and 12 panhypopituitarism) (Fig. 4A). Pituitary dysfunction resolved in 4 patients with MPHD (4/36, 11.1%) and improved in 9 patients with panhypopituitarism (13/36, 33.3%) (Fig. 4B). The hormone deficiency in MPHD worsened in 13 patients (13/36, 36.1%). In summary, in this group, 41 (50%) patients faced post-operative worsening of pituitary function (pre- vs post-surgical prevalence of hypopituitarism p = 0.034) (Fig. 4C).
Endocrinological results. Hormonal status before and after single-stage surgery (SS) (Panel A) and the variation of the hormone status in the post-operative period is reported (Panel B); furthermore, the deficit of each hormonal axis after surgery is specified and related to the relative pre-operative hormonal status (Panel C); hormonal status before and after staged surgery (S). Post-operative results are highlighted after the first and the radical operation (S_1 and S_F) (Panel D); CAI central adrenal insufficiency; GHD growth hormone deficiency; MPHD multiple pituitary hormone deficiency
After the first operation in the S group, 6 (42.9%) patients had normal pituitary function, 7 (50%) had MPHD, and 1 (7.1%) had panhypopituitarism (pre- vs post-surgical prevalence of hypopituitarism p = 0.234). MPHD developed de novo in nine patients and recovered in one patient.
After the last surgery, the prevalence of post-operative complete hypopituitarism was significantly higher compared to the pre-surgical period (p = 0.01), with 28.6% of the group experiencing worsening pituitary function and no patient seeing improvement (Fig. 4D).
Thirty-seven (35.1%) of the 37 GH-deficient patients recovered following surgery, but 18 (40%) of the 40 unaffected patients experienced a new-onset deficiency (odds ratio 2.769, 95% interval confidence 1.125–6.816). The prevalence of post-operative GH deficiency was significantly higher in the multiple-stage surgery group after their first operation compared to baseline (p = 0.002). No significant variation emerged after the last surgery. The difference in the prevalence of new-onset post-operative GH deficiency was not different comparing the three groups (p = 0.09) (Table 2). In the inter-group analysis, the rate of post-operative panhypopituitarism in group SS exceeded the expected frequency (p = 0.05). Puberty induction for hypogonadotropic hypogonadism was necessary in 10 (12.2%) cases in the single-stage group and in 1 (7.1%) case in the staged group.
Functional and visual outcome
HD improved postoperatively in 17 out of 22 patients (77.3%) in the single-staged group and in five patients in the multiple-stage surgery group (both after the first and the last surgery). Four patients in SS group (4.9%) and one patient (7.1%) in the S group (4.9%) had a new-onset HD dysfunction, consisting of eating disorders, sleep cycles’ disturbances in all the cases and in temperature dysregulation in one case of the first group.
No significant differences were observed in the frequency of post-operative neurological recovery and visual defects improvements or worsening among the three groups (respectively, p = 0.6, and p = 0.09).
Complications
Post-operative general medical complications were reported in 18 (21.9%), 2 (14.2%), and 7 (50%) of cases, respectively, in the single-stage group and after the first and the last operation in the multiple-stage group (inter-group comparison p = 0.05). The most frequently reported post-surgical medical issue was the syndrome of inappropriate antidiuretic hormone secretion (SIADH), followed by cerebrospinal fluid leakage, without differences due to the surgical strategy (p = 0.332 and p = 0.51). Three (3.1%) cases of post-operative hemorrhages were reported in the entire cohort: two in single-stage group and one in the staged surgery group. Post-operative hydrocephalus was diagnosed in 4 (4.9%) cases after the single surgery, whereas no similar cases were reported in the staged procedure. Early surgical mortality occurred in two patients.
Recurrence
Twenty-nine patients in the whole cohort (29.6%) faced tumor progression at neuroradiological follow-up; of these, 10 (10.2%) were lost at follow-up after recurrence diagnosis, and 19 (19.4%) patients underwent reoperation. Tumor resection rate in patients with recurrence did not differ significantly comparing single-stage with staged surgery groups (GTR p = 0.836, STR p = 0.887). No differences emerged in the percentage among the patients treated with adjuvant RT comparing the two groups (p = 0.310).
Follow-up and survival analysis
The mean follow-up was 81.2 ± 53.1 months for SS group, 55.6 ± 43.8 months for S_F group, and 102.4 ± 44 months for recurrent CPGs (Table 3). A total of 28/78 (35.9%), 3/16 (15.8%), and 1/13 (7.7%) patients showed tumor progression, respectively, in the single-stage group, staged-surgical group after the last operation (S_F) and in the recurrent groups. The difference in the progression ratio was statistically significant comparing the single-stage group with multiple-stage group (p = 0.04, two-way chi-squared test), but not with the recurrence group (p = 0.07), neither comparing multiple-stage group with recurrences (p = 0.45). In the inter-group comparison, log-rank analysis of Kaplan–Meier survival and hazard plots confirmed that the rate of progression-free patients was significantly lower when undergoing one-stage resection rather than staged resection and or in recurrent surgery (p = 0.03) (Fig. 5).
Considering the QoL, 72 patients (75%) attended school regularly, without major social limitation, regardless of the timing of the treatment. Nearly 24 (25%) however, needed some form of assistance in their daily activities (mostly for visual impairment, attention disorders, and sleep-rhythm disturbances).
This finding was mainly observed in patients undergoing one-step surgery with GTR especially in case of retrochiasmatic tumor location and hypothalamic involvement.
Discussion
Craniopharyngioma is a benign tumor with propensity to recur and high late morbidity due to brain injury. Despite the continuous advances in surgical techniques, the management of CPGs remains controversial, particularly in pediatric age. It is beyond the scope of this study to describe the advantages of one surgical technique over the other, as described elsewhere [24, 25]. Herein, we performed a retrospective analysis of data gathered by four European Referral Centers to evaluate the long-term outcomes of a surgical tailored approach.
Several authors suggested delaying the definitive treatment (radical surgery/RT or both) as long as possible in accordance with the patient's age [26, 27], while others support a more aggressive treatment to lower the risk of subsequent recurrences despite potential higher complications. Data regarding predictors of recurrence and survival are inconsistent due to multiple variables involved, including histological features. Due to the greater prevalence of the adamantinomatous variant, the recurrence rate is higher in children than in adults, and some authors embraced the thesis that radical surgery in children could not completely eradicate the risk of recurrence, which is around 36% after GTR [1, 27, 28]. Furthermore, few data are available about the natural history of untreated CPG, even if some contributions stated that untreated lesions carried a threatening growth potential [29]. The goal of reducing the risk of relapse should be balanced with the importance of preserving hypothalamic/pituitary function [30, 31], focusing on the patient’s long-term QoL.
Multiple variables steps should be considered to guide the extent of resection, surgical approach and route, and the timing of surgery in pediatric patients, including the patient’s age, visual and neurological statuses, hypothalamic involvement, pituitary residual function and the psychophysical growth, previous surgical and/or radiotherapy treatments (Fig. 1).
In our study protocol, patients were addressed to radical one-stage surgery or to multiple-stage surgery according to their pre-operative hormonal status and age at surgery. Patients with hormonal deficiencies were considered eligible for a radical intervention, while patients with a normal hypothalamic–pituitary–adrenal axis were treated preferentially with staged operations’ approach aimed to limit tumor growth, sparing neuro-cognitive and pituitary functions.
In our cohort, GTR was obtained in 44% of patients. This only partially agrees with previous findings reporting a higher frequency of complete resection (49–84% of the cases) [29]. This gap could be explained by the application of an individualized risk-based approach. The presence of crucial structures, and the impossibility of predicting tumor adhesion with neurovascular structures, increases the risk of damage independently of the extent of the resection [29]. No difference emerged in post-operative complications between the groups, confirming that complications depend much more on the unpredictability of the individual lesion and the manipulation of neurovascular structures rather than the EOR.
During follow-up, the resolution of pre-operative DI was observed in 23% phenomenon had been reported rarely in the literature [32, 33]. Otherwise, the onset of new post-operative DI appeared higher (58%) in patient treated with a single-stage surgical treatment (group SS) as consequence of a more aggressive manipulation of the pituitary stalk. Considering other endocrine sequelae, the reversal of a pre-existing pituitary hormonal deficiency after any surgical intervention is quite rare [34]; however, some authors reported cases of partial recovery of the pituitary function after craniopharyngioma removal even after pituitary stalk section [35, 36]. We interestingly found a partial restoration of the pituitary function in 15% of cases. Within the deep analysis, the rate of post-operative pituitary function worsening was higher in patients in group SS and complete hypopituitarism exceeded expected frequency.
An important concern is whether GH hormone replacement therapy contributes to tumor recurrence. A meta-analysis has recently demonstrated that GH replacement is not associated with the recurrence of craniopharyngioma [37]; however, especially in case of residual tumor after a partial resection, the introduction of GH replacement treatment should be evaluated case by case. In each group considered, a significant post-operative GH deficiency was observed, despite the surgical strategy. Considering the extent of resection, it was preferred to start the GHRT after a single-staged surgery (SS) and to postpone it after the complete resection (S_F) in the staged surgery.
Considering puberal induction for hypogonadotropic hypogonadism, it was required in both groups (12.2% vs 7.1%).
Regarding neurological and visual post-operative outcome, the rate of neurological recovery improved significantly after surgery and did not differ across the groups, while there was no difference in visual outcome was observed. Visual symptoms at presentation seems to be associated with a significant poorer visual outcome [38, 39]; however, in our cohort, only 13% of patients who presented preoperatively a visual defect worsened after surgery.
Considering the post-operative HD, the “hypothalamus sparing” surgery has been shown to decrease the occurrence of severe obesity without increasing the local recurrence rate [27, 30, 40]. Furthermore, other authors recently reported interesting results particularly in post-operative improvement in body temperature and outcome of the sleep–wake cycle and body temperature using the EETS [41]. In the present cohort, pre- and post-operative HD rate within groups is comparable with the relevant literature. A total of 5% of obesity, food intake, and sleep cycle disorders were observed among patients treated in group SS and only one case of obesity and sleep disorders, respectively, in group S_1 (7.1%) and S_F (6.3%). Remarkably, we found a complete resolution of HD symptoms in 100% of patients treated with staged surgery and in 77% after a primary surgery. This discrepancy is unusually considering the risk of tumor remnant growth and the relative cumulative risk of hypothalamic involvement over time. It could be explained, however, considering the possibility, granted by a staged surgery, to approach the tumor from different naïve routes (i.e., TCA during the first approach followed by EETS when nasal sinus is developed and pneumatized) allowing a decompression of the suprasellar tumor and hypothalamus and removing in a second time the residual tumor avoiding scars of the previous surgical route.
CPGs are associated with decreased survival, and several authors have reported an overall mortality rate five times higher to the general population [42]. In the earlier studies, mostly about mixed or adult population the survival rates were as low as 67–69% at 5 years and 43% at 10 years. In recent years, with the evolution of the surgical treatment and new approaches to this tumor, an improvement has been demonstrated, reaching 80–94% of survivors at 5-year follow-up [31, 43]. At 10-year follow-up rates differs according to treatment, being 60–100% the survival after GTR, 25–60% after STR/PR, and 77–100% after STR + RT [29]. In our cohort, the cumulative survival rate in the entire group of patients was 98% at 5 years and 95.9% at 10 years, which agrees with the relevant literature. Further analysis showed no difference in 5- and 10-year survival probability among treatment groups (P, S_F, and R), while the progression-free survival and recurrence rate were significantly lower among patients undergoing a primary resection (P). This finding may be because a more radical removal is possible by means of staged surgery, allowing the use of different surgical routes. In relapses, the progression-free survival is certainly related to radiotherapy which in this subgroup of patients is a valid option and can reduce the rate of disease progression after tumor removal.
Considering functional outcome, hypothalamic damage plays a central role in the development of post-operative functional impairment in terms of obesity and awake-sleep, body temperature disorders, emotions, and mood disorders. Despite some factors have been defined as predictor of post-operative HD (tumor size greater than 3.5 cm, hydrocephalus, and preoperative increase of BMI greater than 2 DS), the role of preoperative neurobehavioral disturbances has not been evaluated yet. Despite radical surgery seems associated with a less-favorable outcome [44] and hypothalamus sparing treatment is recommended [45], however, the morbidity scores are not different between children who received RT after STR and those who had GTR [46]. In this scenario, proton beam therapy or radiosurgery with Gamma Knife or Cyber knife should be evaluated during a long follow-up to assess their long-term efficacy and toxicity, particularly in terms of potential reduction in treatment-related hypothalamic damage and neurobehavioral deficits [47].
We also evaluated the QoL not only considering post-operative visual deficits or obesity, but also the eventual decline of cognitive functions resulting after the surgical treatments (one-stage vs staged surgery) or RT, using questionnaires that were submitted to patients and parents to quantify the social reintegration of children and cognitive abilities.
Indeed, considering the current literature, data on neurobehavioral outcome are inconsistent or contradictory, and they are commonly based on the surgeon’s subjective judgment and no disease-specific measures for health-related quality of life (HRQOL), eating behaviors, and sleep–wake rhythm have been validated for craniopharyngiomas and hypothalamic damage. We only considered the QoL after a single approach and we did not consider QoL according to the number of operations and recurrences, which remain the factors that most affect quality of life along with the hypothalamic involvement of the tumor. In the present cohort, three-quarters of patients attended school regularly, without major social limitation, regardless of the timing of the treatment after a single stage or a staged surgery. Nearly one quarter, however, needed some form of assistance in their daily activities, especially after the single-stage surgical treatment when a GTR was attempted and a hypothalamic involvement was preoperatively suspected.
The effects of preoperative hypothalamic involvement and operative/post-operative hypothalamic damage on patients’ QoL cannot be assessed independently, because these two entities are strongly correlated.
For this reason, a greater effort should be given on preoperative evaluation of each subclinical hypothalamic involvement even before surgery.
Strengths and limitations of this study
This manuscript provides an accurate description of both epidemiology and outcomes in a contemporary cohort of consecutive patients that were treated in different centers by different surgeons. In all the different institutions, the treatments have been tailored to the individual patient according to age, anatomy, and clinical–endocrinological status. The number of collected patients is significantly higher than a standard pediatric series.
The results of this study are limited by their retrospective nature, the lower rate of patients treated with staged surgery and by heterogeneity of QoL’s data. Moreover, considering the small number of patients that underwent RT, it was out of our purpose to compare long-term results between GTR and STR + RT. A further limitation could be given by the heterogeneity in the cut-off used for the definition of the various pituitary defects over the years and between the different laboratories of the involved centers. It must also be recognized that an increasingly important role in terms of tumor behavior and recurrence risk could be played by the tumor microenvironment.
Conclusions
Currently, the first objective in the management of CPGs is the preservation of a good QoL with protection of neurobehavioral, cognitive, and hypothalamic functions. However, despite all the advancement, the optimal treatment in pediatric patients is not established and patient management remains debated. To our knowledge, this is the first report describing results of a staged surgery in pediatric patients. The role of a “staged therapy”, in selected patients, has shown to be safe and effective, allowing a physiological growth of the child with an initial normality in their hypothalamic–pituitary axis before a more radical operation.
References
Sarkar S, Chacko SR, Korula S et al (2021) Long-term outcomes following maximal safe resection in a contemporary series of childhood craniopharyngiomas. Acta Neurochir 163:499–509. https://doi.org/10.1007/s00701-020-04591-4
Visser J, Hukin J, Sargent M et al (2010) Late mortality in pediatric patients with craniopharyngioma. J Neurooncol 100:105–111. https://doi.org/10.1007/s11060-010-0145-5
Ostrom QT, Gittleman H, Liao P et al (2017) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2010–2014. Neuro Oncol 19:v1–v88. https://doi.org/10.1093/neuonc/nox158
Louis DN, Perry A, Reifenberger G et al (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Muller HL, Merchant TE, Warmuth-Metz M et al (2019) Craniopharyngioma. Nat Rev Dis Primers 5:75. https://doi.org/10.1038/s41572-019-0125-9
Yang I, Sughrue ME, Rutkowski MJ et al (2010) Craniopharyngioma: a comparison of tumor control with various treatment strategies. Neurosurg Focus 28:E5. https://doi.org/10.3171/2010.1.FOCUS09307
Asha MJ, Oswari S, Takami H et al (2020) Craniopharyngiomas: challenges and controversies. World Neurosurg 142:593–600. https://doi.org/10.1016/j.wneu.2020.05.172
Ali ZS, Bailey RL, Daniels LB et al (2014) Comparative effectiveness of treatment options for pediatric craniopharyngiomas. J Neurosurg Pediatr 13:178–188. https://doi.org/10.3171/2013.11.PEDS1320
Drapeau A, Walz PC, Eide JG et al (2019) Pediatric craniopharyngioma. Child’s Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 35:2133–2145. https://doi.org/10.1007/s00381-019-04300-2
Beltrand J, Brauner R, Pinto G et al (2013) Childhood craniopharyngioma: hypothalamus-sparing surgery decreases the risk of obesity. J Clin Endocrinol Metab 98:2376–2382. https://doi.org/10.1210/jc.2012-3928
Hill TK, Baine MJ, Verma V et al (2019) Patterns of care in pediatric craniopharyngioma: outcomes following definitive radiotherapy. Anticancer Res 39:803–807. https://doi.org/10.21873/anticanres.13178
Clark AJ, Cage TA, Aranda D et al (2013) A systematic review of the results of surgery and radiotherapy on tumor control for pediatric craniopharyngioma. Child’s Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 29:231–238. https://doi.org/10.1007/s00381-012-1926-2
Maghnie M, Uga E, Temporini F et al (2005) Evaluation of adrenal function in patients with growth hormone deficiency and hypothalamic–pituitary disorders: comparison between insulin-induced hypoglycemia, low-dose ACTH, standard ACTH and CRH stimulation tests. Eur J Endocrinol 152:735–741. https://doi.org/10.1530/eje.1.01911
Yeliosof O, Gangat M (2019) Diagnosis and management of hypopituitarism. Curr Opin Pediatr 31:531–536. https://doi.org/10.1097/MOP.0000000000000779
Lamberts SW, de Herder WW, van der Lely AJ (1998) Pituitary insufficiency. Lancet (Lond, Engl) 352:127–134. https://doi.org/10.1016/s0140-6736(98)85043-5
Fenske W, Allolio B (2012) Clinical review: current state and future perspectives in the diagnosis of diabetes insipidus: a clinical review. J Clin Endocrinol Metab 97:3426–3437. https://doi.org/10.1210/jc.2012-1981
Dickstein G (2003) The assessment of the hypothalamo-pituitary-adrenal axis in pituitary disease: are there short cuts? J Endocrinol Invest 26:25–30
Ghigo E, Bellone J, Aimaretti G et al (1996) Reliability of provocative tests to assess growth hormone secretory status. Study in 472 normally growing children. J Clin Endocrinol Metab 81:3323–3327. https://doi.org/10.1210/jcem.81.9.8784091
Petersenn S, Quabbe H-J, Schöfl C et al (2010) The rational use of pituitary stimulation tests. Deutsch Arzteblatt Int 107:437–443. https://doi.org/10.3238/arztebl.2010.0437
Bayley N, Pinneu SR (1952) Tables for predicting adult height from skeletal age: revised for use with the Greulich-Pyle hand standards. J Pediatr 40:423–441. https://doi.org/10.1016/s0022-3476(52)80205-7
Tanner JM, Whitehouse RH (1976) Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child 51:170–179. https://doi.org/10.1136/adc.51.3.170
Yasargil MG, Curcic M, Kis M et al (1990) Total removal of craniopharyngiomas. Approaches and long-term results in 144 patients. J Neurosurg 73:3–11. https://doi.org/10.3171/jns.1990.73.1.0003
Kassam AB, Gardner PA, Snyderman CH et al (2008) Expanded endonasal approach, a fully endoscopic transnasal approach for the resection of midline suprasellar craniopharyngiomas: a new classification based on the infundibulum. J Neurosurg 108:715–728. https://doi.org/10.3171/JNS/2008/108/4/0715
Locatelli D, Veiceschi P, Castelnuovo P et al (2019) Transsphenoidal surgery for pituitary adenomas in pediatric patients: a multicentric retrospective study. Child’s Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 35:2119–2126. https://doi.org/10.1007/s00381-019-04179-z
Locatelli D, Massimi L, Rigante M et al (2010) Endoscopic endonasal transsphenoidal surgery for sellar tumors in children. Int J Pediatr Otorhinolaryngol 74:1298–1302. https://doi.org/10.1016/j.ijporl.2010.08.009
Steňo J, Bízik I, Steňo A, Matejčík V (2013) Craniopharyngiomas and the hypothalamus. J Neurosurg 119:1646–1650
Puget S, Garnett M, Wray A et al (2007) Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. J Neurosurg 106:3–12. https://doi.org/10.3171/ped.2007.106.1.3
Caldarelli M, Massimi L, Tamburrini G et al (2005) Long-term results of the surgical treatment of craniopharyngioma: the experience at the Policlinico Gemelli, Catholic University, Rome. Child’s Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 21:747–757. https://doi.org/10.1007/s00381-005-1186-5
Karavitaki N, Brufani C, Warner JT et al (2005) Craniopharyngiomas in children and adults: systematic analysis of 121 cases with long-term follow-up. Clin Endocrinol 62:397–409. https://doi.org/10.1111/j.1365-2265.2005.02231.x
Elowe-Gruau E, Beltrand J, Brauner R et al (2013) Childhood craniopharyngioma: hypothalamus-sparing surgery decreases the risk of obesity. J Clin Endocrinol Metab 98:2376–2382. https://doi.org/10.1210/jc.2012-3928
Daubenbuchel AMM, Muller HL (2015) Neuroendocrine disorders in pediatric craniopharyngioma patients. J Clin Med 4:389–413. https://doi.org/10.3390/jcm4030389
Honegger J, Buchfelder M, Fahlbusch R (1999) Surgical treatment of craniopharyngiomas: endocrinological results. J Neurosurg 90:251–257. https://doi.org/10.3171/jns.1999.90.2.0251
Ogawa Y, Niizuma K, Tominaga T (2017) Recovery from diabetes insipidus and preservation of thyroid function after craniopharyngioma removal and pituitary stalk sectioning. Clin Neurol Neurosurg 162:36–40. https://doi.org/10.1016/j.clineuro.2017.09.005
Bereket A (2020) Postoperative and long-term endocrinologic complications of craniopharyngioma. Hormone Res Paediatr 93:497–509. https://doi.org/10.1159/000515347
Ogawa Y, Tominaga T (2019) Partial reconstitution of the hypothalamo-pituitary axes after pituitary stalk sectioning and specific magnetic resonance imaging findings. World Neurosurg 131:e81–e87. https://doi.org/10.1016/j.wneu.2019.07.057
Berg C, Meinel T, Lahner H et al (2010) Recovery of pituitary function in the late-post-operative phase after pituitary surgery: results of dynamic testing in patients with pituitary disease by insulin tolerance test 3 and 12 months after surgery. Eur J Endocrinol 162:853–859. https://doi.org/10.1530/EJE-09-0997
Alotaibi NM, Noormohamed N, Cote DJ et al (2018) Physiologic growth hormone-replacement therapy and craniopharyngioma recurrence in pediatric patients: a meta-analysis. World Neurosurg 109:487-496.e1. https://doi.org/10.1016/j.wneu.2017.09.164
Duff J, Meyer FB, Ilstrup DM et al (2000) Long-term outcomes for surgically resected craniopharyngiomas. Neurosurgery 46:291–295. https://doi.org/10.1097/00006123-200002000-00007
Abrams LS, Repka MX (1997) Visual outcome of craniopharyngioma in children. J Pediatr Ophthalmol Strabismus 34:223–228
Mazzatenta D, Zoli M, Guaraldi F et al (2020) Outcome of endoscopic endonasal surgery in pediatric craniopharyngiomas. World Neurosurg 134:e277–e288. https://doi.org/10.1016/j.wneu.2019.10.039
Zoli M, Sambati L, Milanese L et al (2016) Postoperative outcome of body core temperature rhythm and sleep–wake cycle in third ventricle craniopharyngiomas. Neurosurg Focus 41:1–9. https://doi.org/10.3171/2016.9.FOCUS16317
Bulow B, Attewell R, Hagmar L et al (1998) Postoperative prognosis in craniopharyngioma with respect to cardiovascular mortality, survival, and tumor recurrence. J Clin Endocrinol Metab 83:3897–3904. https://doi.org/10.1210/jcem.83.11.5240
Karavitaki N (2014) Management of craniopharyngiomas. J Endocrinol Invest 37:219–228. https://doi.org/10.1007/s40618-013-0050-9
Zada G, Kintz N, Pulido M, Amezcua L (2013) Prevalence of neurobehavioral, social, and emotional dysfunction in patients treated for childhood craniopharyngioma: a systematic literature review. PLoS ONE 8:e76562. https://doi.org/10.1371/journal.pone.0076562
Bogusz A, Müller HL (2018) Childhood-onset craniopharyngioma: latest insights into pathology, diagnostics, treatment, and follow-up. Expert Rev Neurother 18:793–806. https://doi.org/10.1080/14737175.2018.1528874
De Vile CJ, Grant DB, Kendall BE et al (1996) Management of childhood craniopharyngioma: can the morbidity of radical surgery be predicted? J Neurosurg 85:73–81. https://doi.org/10.3171/jns.1996.85.1.0073
Elson A, Bovi J, Kaur K et al (2014) Effect of treatment modality on the hypothalamic–pituitary function of patients treated with radiation therapy for pituitary adenomas: hypothalamic dose and endocrine outcomes. Front Oncol 4:73. https://doi.org/10.3389/fonc.2014.00073
Funding
This research did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. MLT and DG are members of the Editorial Board of the Journal of Endocrinological Investigation.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (name of institute/committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
All patients involved in this study signed a consent form to publish their data or clinical images whenever useful.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
40618_2022_1993_MOESM2_ESM.docx
Supplementary Table: Diagnostic criteria for pituitary disfunction. The normal values of the single hormone, the method used to dose them are documented along with the inter-intraassay variability. Lowercase letters (a, b,c) refers to individual centers. ECLIA: electro-chemiluminescence immunoassay; ChLIA: chemiluminescence immunoassay; CMIA: chemiluminescent microparticle immunoassay; IRMA: Immunoradiometric assay; RIA: Radioimmunoassay. Supplementary file2 (DOCX 26 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Agresta, G., Campione, A., Veiceschi, P. et al. Clinical and oncological outcomes in single-stage versus staged surgery for pediatric craniopharyngiomas: a multicenter retrospective study. J Endocrinol Invest 46, 1219–1232 (2023). https://doi.org/10.1007/s40618-022-01993-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01993-2