Abstract
Background
While low testosterone (T) was described as a predictor of unfavorable coronavirus-disease 19 (COVID-19) outcome in men, data concerning the role of T in women with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection are scant and limited to small cohorts. This study investigated the relationship between serum T values and outcomes of COVID-19 in a large female hospitalized cohort.
Methods
One-hundred-sixty-eight adult women (median age 77, range 18–100 years; 154 in post-menopause) hospitalized for COVID-19 were assessed for PaO2/Fio2 ratio, serum T and inflammatory parameters.
Results
Median duration for hospital stay was 14.2 days (range 1–115) with overall mortality of 26% (n = 44). Subjects who died were significantly older (p < 0.001), had significantly more comorbidities (p = 0.015) and higher serum T (p = 0.040), white blood cells (p = 0.007), c-reactive protein (CRP; p < 0.001), interleukin-6 (IL-6; p < 0.001), procalcitonin (PCT; p < 0.001), lactate dehydrogenase (LDH; p = 0.001), D-dimer (p = 0.035), fibrinogen (p = 0.038) and lower serum free-triiodothyronine (FT3; p < 0.001) and luteinizing hormone (LH; p = 0.024) values. In post-menopausal women, significant associations were observed between T levels and serum CRP (rho: 0.23; p = 0.002), IL-6 (rho: 0.41; p < 0.001), LDH (rho: 0.34; p < 0.001), D-Dimer (rho: 0.21; p = 0.008), PCT (rho: 0.26; p = 0.001) and HDL cholesterol (rho: – 0,22, p = 0.008). In multivariate regression analyses, serum T maintained the significant association with mortality after correction for age, coexistent comorbidities and serum LH and FT3, whereas it was lost after correction for inflammatory parameters.
Conclusion
In females, high serum T levels might be a mirror of inflammatory phenotype and worse COVID-19 course.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection has caused a devastating pandemic with more than 6 million deaths worldwide (https://covid19.who.int). The rapid emergence of SARS-Cov-2 variants has raised concerns because of their higher transmissibility and their possible escape from vaccines and natural immunity resulting in new waves and growing reinfections [1]. Thus, the control of SARS-Cov-2 progression and death is still a major challenge.
The clinical heterogeneity of coronavirus-disease 19 (COVID-19) infection, ranging from entirely asymptomatic infection to the acute respiratory insufficiency (ARI) and death, is widely demonstrated [2, 3]. However, with the advent of vaccines and new variants, symptoms and clinical course of SARS-Cov-2 infection also become changeable with an even more variability in clinical manifestation [4]. Since new infection waves are highly expected, the identification of pathogenic mechanisms underlying the clinical heterogeneity is crucial to allow a better risk stratification. Several studies have revealed age, gender and pre-existing comorbidities, mainly chronic metabolic disease (diabetes, obesity, hypertension, cardiovascular, cerebrovascular and kidney disease), as major risk factors for the occurrence of acute respiratory distress syndrome (ARDS) and fatal outcome [5]. Epidemiological data on hospitalized COVID-19 patients highlighted a gender disparity with higher incidence, severity and mortality rate in males than in females [6]. However, the possible determinants of the gender issue of the COVID-19 pandemic are still argue of intense scientific debate. Previous data published by our group and other authors demonstrated the role of low circulating T levels as a marker of higher risk of severe outcomes among COVID-19 male patients [7,8,9], corroborating in SARS-Cov-2 infection the modulatory action of testosterone.
Conversely, data on the possible role of T in women with SARS-Cov-2 infection are scant and limited to small cohorts [10]. In this study, we aimed at evaluating the association between serum T values and inflammation markers in a large cohort of COVID-19 female subjects.
Methods
This is a monocentric study of 168 consecutive female patients hospitalized for COVID-19 at the IRCCS Humanitas Research Hospital, Rozzano-Milan, Italy between November 1, 2020 and March 31, 2021. The inclusion criteria were: (1) laboratory pharyngeal-nose swab positivity of SARS-Cov-2 assessed by real-time reverse-transcriptase–polymerase-chain-reaction; (2) female sex; (3) older than 18 years; (4) completed hospital course at study end (discharged or dead). The first endpoint of the study was the association between serum T levels and inflammatory parameters at study entry. Secondary endpoint was to explore the associations between serum T levels and in-hospital mortality.
At study entry, before starting any treatment for COVID-19, enrolled patients were evaluated for arterial partial pressure oxygen (PaO2)/fraction of inspired oxygen (FiO2) ratio, measured by arterial blood gas analysis. ARI was defined as PaO2/FiO2 ratio < 300 mmHg on oxygen [11].
In 146 patients was also assessed the Body mass index (BMI), defined by the individual’s weight in kilograms divided by the square of their height in meters. On the first morning after the admission blood samples were drawn for the determination of serum T (nmol/L), luteinizing hormone (LH, U/L), total white blood cells (WBC, n*103/ml), interleukin-6 (IL-6, pg/mL), C-reactive protein (CRP, mg/dL), procalcitonin (PCT, mg/dL), D-Dimer (ng/mL), fibrinogen (mg/dL), glycemia (mg/dL), 25-hydroxyvitamin vitamin D (25OHD, ng/mL), thyroid-stimulating hormone (TSH, μUI/mL), free-triiodothyronine (fT3, pmol/L), free-thyroxine (fT4, pmol/L), total cholesterol (TC, mg/dL), HDL cholesterol (HDL, mg/dL) and triglycerides (TG, mg/dL). Calculated low-density lipoprotein (cLDL, mg/dL) was obtained using TC, TG and HDL according with Friedewald’s formula [12]. Testosterone was measured using Access Testosterone assay (Beckman Coulter Inc, Fullerton, CA), a competitive immunoassay method that has analytical and clinical acceptable correlation with mass-spectrometry method [13]. Other parameters were measured using standardized methods routinely used for hospital clinical practice.
From the medical records we have also collected data about the following clinical conditions: hypertension, coronary artery diseases (CAD), past or active cancer, chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD) associated with stages 3–5 renal insufficiency as defined by estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73m2 (calculated by CKD-EPI).
The study was approved by the Ethics Committee of IRCCS Humanitas Research Hospital and the patients gave their consent to use the clinical and biochemical data for research purposes.
Statistical analysis
Data were presented as median and absolute range, unless otherwise stated. Since most of variables were non-normally distributed as assessed by Kolmogorov–Smirnov test, non-parametric tests were used. The comparisons were performed by Mann–Whitney test. Spearman’s correlation coefficient (ρ) was calculated to determine association between continuous variables. Strength of r correlation was defined according to Evan’s classification [14]. Multivariate logistic regression model was performed and the odds ratio (OR) with 95% confidence interval (95% C.I.) were calculated to evaluate determinants of mortality. All risk factors with a p value under 0.10 in univariate analyses were submitted to multivariable logistic regression analyses taking into account the minimal guidance criterion of ten events per variable [15]. P value < 0.05 was considered as significant. Statistical analysis was performed using SPSS version 25.0.
Results
The study included 168 unselected adult women (median age 77; range 18–100 years; median BMI 26.3; range 15.6–48.6; 154 in post-menopause). Median duration for hospital stay was 14.2 days (range 1–115). Baseline characteristics of study population are summarized in Table 1. At time of hospitalization, ARI was diagnosed in 102 subjects (60%). During hospital stay, 44 subjects (26.0%) died. Subjects who died were significantly older (p < 0.001) and had significantly more comorbidities (p = 0.015) and higher serum T levels (p = 0.040), WBC (p = 0.007), CRP (p < 0.001), IL-6 (p < 0.001), PCT (p < 0.001), LDH (p = 0.001), D-dimer (p = 0.035), fibrinogen (p = 0.038) and lower serum FT3 (p < 0.001) and LH (p = 0.024) as compared to subjects who did not die, without significant differences in BMI, menopause status, serum TSH, fT4, 25(OH)D, ferritin, FBG, TC, HDL, Tg and cLDL values (Table 1).
In post-menopausal women (154 cases), serum T was significantly correlated with serum CRP (rho: 0.23; p = 0.002), IL-6 (rho: 0.41; p < 0.001), LDH (rho: 0.34; p < 0.001), D-Dimer (rho: 0.21; p = 0.008), PCT (rho: 0.26; p = 0.001) and HDL (rho: – 0.22; p = 0.008). After exclusion of outliers, the associations between T and IL-6, D-Dimer and PCT were maintained (Fig. 1a–c). No outliers of CRP, LDH and HDL were detected. In pre-menopausal women (14 cases), serum T did not result to be significantly correlated with any biochemical parameter (data not shown).
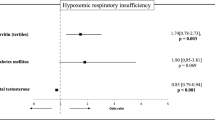
In multivariate regression analyses including all covariates significantly associated with mortality in univariate analysis (Table 1), serum T maintained the significant association with mortality after correction for age, coexistent comorbidities and serum LH and FT3, whereas it was lost after correction for inflammatory parameters and use of anti-inflammatory drugs (Table 2).
Discussion
This study reports an association between serum T levels and inflammatory parameters in COVID-19 female patients and, for the first time, the evidence of higher serum T levels in females deceased for SARS-Cov-2 infection, suggesting a possible predictive role of T on clinical outcome.
These results confirm in a large cohort what previously reported by a study performed in a smaller sample by Di Stasi et al. [10], who found in a cohort of 17 female patients with SARS-Cov-2 pneumonia a significant and positive association between T levels and inflammatory markers, including PCT, CRP and fibrinogen as well as higher T levels as predictor of a worse hospital course in terms of hospitalization length. The authors hypothesized that the high T level found in COVID-19 female patients was mostly produced by the adrenal gland because of an adrenal cortex hyperactivity in response to the stressful condition induced by SARS-Cov-2 infection, arguing that T was a mirror, rather than a pathogenetic factor, of the inflammatory status reported in these patients. The adrenal origin of T was supported by the strong association with cortisol level and by the surprising evidence of relative low LH level for the menopausal patients’ cohort. The authors suggested an inhibitory effect of high T levels of adrenal source on the physiological post-menopausal LH increase [10]. Interestingly in this concern, our results are consistent with the data from Di Stasi et al. [10], since a positive correlation was observed between serum T levels and main inflammatory parameters. Moreover, in our cohort of postmenopausal women, low LH level were found, endorsing the hypothesis of the negative feedback exerted by high T levels on pituitary. The evidence of lower LH levels in postmenopausal women with an unfavorable outcome confirms in these patients a greater inflammatory status of adrenal origin and consistent greater negative feedback. Conversely, we found no correlation between serum T levels and hospital in stay duration. Significantly higher serum T levels were found in women who died as compared to survivors even after correction for age, comorbidities and serum LH and fT3 values. However, such an association was lost after correction for inflammatory parameters and use of anti-inflammatory drugs, suggesting that increase of testosterone values does not represent an independent predictor of clinical outcome of SARS-CoV-2 infection in women, but it is likely to reflect a functional dysregulation linked to disrupted inflammation mechanisms. Noteworthy, high T levels have been investigated as one of the factors responsible for the higher risk of COVID-19 infection in women with PCOS [16,17,18]. Androgen excess is a crucial feature of PCOS and women with PCOS and hyperandrogenism have a worse metabolic profile than women with PCOS and normal androgen level [19, 20]. Moreover, hyperandrogenism is a primary driver of increased risk of diabetes and fatty liver disease in PCOS women [21, 22]. In addition to the higher susceptibility to SARS-Cov-2 infection, PCOS women with hyperandrogenic phenotype are more likely to develop clinical symptoms of COVID-19 compared to their non-hyperandrogenic counterparts [23]. Although potential mechanisms underpinning these observations are not fully understood, high T levels in this clinical setting could reflect the result of a chronic metabolic dysfunction, which ultimately influences outcome in SARS-Cov-2 infection. Several studies stated that T controls the expression of transmembrane serine protease 2 (TMPRSS2) involved in the proteolytic processing of the SARS-Cov-2 spike protein [24, 25]. Thus, high T levels in female patients could influence COVID-19 severity both directly, facilitating viral penetration into cells of various tissues, and indirectly, promoting the inflammatory status.
Overall, the clinical scenario depicted in women is remarkably different from the one occurring in men. Mortality from COVID-19 is higher in men with lower testosterone levels, worse metabolic control, and presence of relevant comorbidities [26]. Testosterone has a dimorphic role in inflammation [27], reducing the inflammatory response in men [28] and promoting the inflammatory status in women [18]: however, in men low testosterone is also associated with worse metabolic control [29], therefore providing further reasons for increased disease severity.
Finally, our results confirm the contribution to mortality from dysregulation of thyroid function during acute COVID-19 illness, consistent with what previously described [30, 31].
This study has some limitations. Due to the lack of a control group, we cannot confirm the causative relationship of T as a determinant of increased mortality in the study cohort. Serum T was measured in a single blood sample at admission not allowing to estimate the duration of exposure to high T values during hospital stay. Moreover, lack of serum sex-hormone binding globulin (SHBG) assay, we did not provide information on the true peripheral T status in the enrolled women. Furthermore, the lack of information on adrenal function did not allow to draw conclusion on the origin of serum T levels.
Notwithstanding these limitations, our study points out an opposite role of T in female patients with COVID-19 infection than one observed in males suggesting a different action of this hormone in inflammation response depending on gender.
Conclusion
This study cohort adds consistent evidence to previous reports about the role of T as a mirror of higher inflammatory phenotype in female with SARS-Cov-2 infection and provides first evidence on possible predictive role of T on COVID-19 clinical outcome. Further studies are needed to clarify the pathophysiology of the gender differences observed and to establish the clinical relevance of high T levels in COVID-19 female patients.
Data availability statement
The data used for this manuscript will be made available upon reasonable request to the corresponding author.
References
Malik JA, Ahmed S, Mir A, Shinde M, Bender O, Alshammari F et al (2022) The SARS-CoV-2 mutations versus vaccine effectiveness: new opportunities to new challenges. J Infect Public Health 15(2):228–240
D’Arena G, Penna A, Crocamo A, Sguazzo F, Viceconti R, Barlotti V et al (2021) Heterogeneity of clinical and radiological findings of COVID-19. Postgrad Med J 97(1146):268–269
Al Maqbali M, Al Badi K, Al Sinani M, Madkhali N, Dickens GL (2022) Clinical Features of COVID-19 patients in the first year of pandemic: a systematic review and meta-analysis. Biol Res Nurs 24(2):172–185
El-Shabasy RM, Nayel MA, Taher MM, Abdelmonem R, Shoueir KR, Kenawy ER (2022) Three waves changes, new variant strains, and vaccination effect against COVID-19 pandemic. Int J Biol Macromol 204:161–168
Geng J, Yu X, Bao H, Feng Z, Yuan X, Zhang J et al (2021) Chronic diseases as a predictor for severity and mortality of COVID-19: a systematic review with cumulative meta-analysis. Front Med (Lausanne) 8:588013
Galbadage T, Peterson BM, Awada J, Buck AS, Ramirez DA, Wilson J et al (2020) Systematic review and meta-analysis of sex-specific COVID-19 clinical outcomes. Front Med (Lausanne) 7:348
Rastrelli G, Di Stasi V, Inglese F, Beccaria M, Garuti M, Di Costanzo D et al (2021) Low testosterone levels predict clinical adverse outcomes in SARS-CoV-2 pneumonia patients. Andrology 9(1):88–98
Vena W, Pizzocaro A, Maida G, Amer M, Voza A, Di Pasquale A et al (2022) Low testosterone predicts hypoxemic respiratory insufficiency and mortality in patients with COVID-19 disease: another piece in the COVID puzzle. J Endocrinol Invest 45(4):753–762
Corona G, Vena W, Pizzocaro A, Pallotti F, Paoli D, Rastrelli G, et al (2022) Andrological effects of SARS-Cov-2 infection: a systematic review and meta-analysis. J Endocrinol Invest. https://doi.org/10.1007/s40618-022-01801-x
Di Stasi V, Rastrelli G, Inglese F, Beccaria M, Garuti M, Di Costanzo D et al (2022) Higher testosterone is associated with increased inflammatory markers in women with SARS-CoV-2 pneumonia: preliminary results from an observational study. J Endocrinol Invest 45(3):639–648
Ware LB, Matthay MA (2000) The acute respiratory distress syndrome. N Engl J Med 342(18):1334–1349
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18(6):499–502
Dittadi R, Matteucci M, Meneghetti E, Ndreu R (2018) Reassessment of the Access Testosterone chemiluminescence assay and comparison with LC-MS method. J Clin Lab Anal. 32(3)
Evans JD (1996) Straightforward Statistics for the Behavioral Sciences: Brooks/Cole Publishing Company
Pavlou M, Ambler G, Seaman SR, Guttmann O, Elliott P, King M et al (2015) How to develop a more accurate risk prediction model when there are few events. BMJ British Med J 351:h3868
Subramanian A, Anand A, Adderley NJ, Okoth K, Toulis KA, Gokhale K et al (2021) Increased COVID-19 infections in women with polycystic ovary syndrome: a population-based study. Eur J Endocrinol 184(5):637–645
de Medeiros SF, Yamamoto MMW, de Medeiros MAS, Yamamoto A, Barbosa BB (2022) Polycystic ovary syndrome and risks for COVID-19 infection: a comprehensive review: PCOS and COVID-19 relationship. Rev Endocr Metab Disord 23(2):251–264
González F (2012) Inflammation in Polycystic Ovary Syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids 77(4):300–305
Glintborg D, Rubin KH, Nybo M, Abrahamsen B, Andersen M (2018) Cardiovascular disease in a nationwide population of Danish women with polycystic ovary syndrome. Cardiovasc Diabetol 17(1):37
Glueck CJ, Goldenberg N (2019) Characteristics of obesity in polycystic ovary syndrome: Etiology, treatment, and genetics. Metabolism 92:108–120
O’Reilly MW, Glisic M, Kumarendran B, Subramanian A, Manolopoulos KN, Tahrani AA et al (2019) Serum testosterone, sex hormone-binding globulin and sex-specific risk of incident type 2 diabetes in a retrospective primary care cohort. Clin Endocrinol (Oxf) 90(1):145–154
Kumarendran B, O’Reilly MW, Manolopoulos KN, Toulis KA, Gokhale KM, Sitch AJ et al (2018) Polycystic ovary syndrome, androgen excess, and the risk of nonalcoholic fatty liver disease in women: a longitudinal study based on a United Kingdom primary care database. PLoS Med 15(3):e1002542
Cadegiani FA, Lim RK, Goren A, McCoy J, Situm M, Kovacevic M et al (2021) Clinical symptoms of hyperandrogenic women diagnosed with COVID-19. J Eur Acad Dermatol Venereol 35(2):e101–e104
Baratchian M, McManus JM, Berk MP, Nakamura F, Mukhopadhyay S, Xu W et al (2021) Androgen regulation of pulmonary AR, TMPRSS2 and ACE2 with implications for sex-discordant COVID-19 outcomes. Sci Rep 11(1):11130
Mohamed MS, Moulin TC, Schiöth HB (2021) Sex differences in COVID-19: the role of androgens in disease severity and progression. Endocrine 71(1):3–8
Sansone A, Mollaioli D, Ciocca G, Limoncin E, Colonnello E, Vena W et al (2021) Addressing male sexual and reproductive health in the wake of COVID-19 outbreak. J Endocrinol Invest 44(2):223–231
Sex TV, Response HDI (2018) Front Immunol 9:1931
Kalinchenko SY, Tishova YA, Mskhalaya GJ, Gooren LJ, Giltay EJ, Saad F (2010) Effects of testosterone supplementation on markers of the metabolic syndrome and inflammation in hypogonadal men with the metabolic syndrome: the double-blinded placebo-controlled Moscow study. Clin Endocrinol (Oxf) 73(5):602–612
Corona G, Rastrelli G, Vignozzi L, Mannucci E, Maggi M (2011) Testosterone, cardiovascular disease and the metabolic syndrome. Best Pract Res Clin Endocrinol Metab 25(2):337–353
Lania A, Sandri MT, Cellini M, Mirani M, Lavezzi E, Mazziotti G (2020) Thyrotoxicosis in patients with COVID-19: the THYRCOV study. Eur J Endocrinol 183(4):381–387
Pizzocaro A, Colombo P, Vena W, Ariano S, Magnoni P, Reggiani F et al (2021) Outcome of Sars-COV-2-related thyrotoxicosis in survivors of Covid-19: a prospective study. Endocrine 73(2):255–260
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: AGL, GM. Data curation: MFB, SJ. Data analysis: WV, GM. Funding acquisition: not applicable. Supervision: AGL, GM. Original draft writing: MFB, WV. Review and editing: AP, EL, AB, NB, ACB, GM, AGL. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Walter Vena received a project grant from IBSA. All other authors declare they do not have any conflict of interest that is relevant to the subject matter or materials included in this work.
Ethical approval
All the procedures performed in the study were in accordance with the ethical standards of the Ethics Committee of IRCCS Humanitas Research Hospital, Rozzano-Milan, Italy, and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all the individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Birtolo, M.F., Vena, W., Pizzocaro, A. et al. Serum testosterone mirrors inflammation parameters in females hospitalized with COVID-19. J Endocrinol Invest 46, 939–945 (2023). https://doi.org/10.1007/s40618-022-01957-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01957-6