Abstract
Purpose
Autoimmune thyroid diseases (AITDs) are chronic organ-specific autoimmune disorders, predominantly including Graves’ disease (GD), and Hashimoto’s thyroiditis (HT). This study aimed to investigate whether single-nucleotide polymorphisms (SNPs) in MAGI2 and MAGI3 gene contributed to the etiology of AITDs.
Methods
We conducted a case–control study including 1001 patients with AITDs (625 GD, 376 HT) and 846 healthy controls. Subgroup analyses in GD and HT were also performed.
Results
The genotypes of rs2160322 in MAGI2 showed a borderline association with AITDs (P = 0.048), and they had a strong correlation with GD (P = 0.012). The frequency of the minor allele G of rs2160322 was significantly higher in the GD patients than in the controls (P = 0.027; OR 1.91; 95% CI 1.020–1.391), especially for GD females (P = 0.008; OR 1.304; 95% CI 1.072–1.587), and those who had positive family history (P = 0.011; OR 1.412; 95% CI 1.083–1.843). For genetic model analysis, the recessive model and homozygous model of rs2160322 showed significant associations with AITDs (P = 0.009; P = 0.019) and GD (P = 0.004; P = 0.005). Nevertheless, our study could not identify any relationship between these SNPs and HT. Due to the low mutation rate of rs1343126 in MAGI3, we were unable to obtain a credible conclusion on its association with AITDs.
Conclusions
Our study identified that MAGI2 rs2160322 was strongly associated with GD susceptibility. The potential dysfunction of tight junction proteins and aberrant epithelial barrier caused by abnormal MAGI2 expression may be a novel mechanism of GD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autoimmune thyroid diseases (AITDs) are a class of chronic organ-specific autoimmune diseases, predominantly including Graves’ disease (GD) and Hashimoto’s thyroiditis (HT) [1, 2]. The incidence of AITDs in the overall population is 2–5%, of which women have an absolute preponderance, with the ratio of female to male ranges from 5:1 to 10:1 [3,4,5]. The exact etiology of AITDs has not yet fully elucidated, and it is usually thought to be multifactorial, involving genetic susceptibility, impaired immune system homeostasis, and environmental factors [6,7,8].
Membrane-associated guanylate kinase inverted (MAGI)2 and MAGI3 are the main members of the tight junction (TJ) family and are closely related in function. TJ proteins, encoded by TJ gene families (F11R, MAGI1, MAGI2, MAGI3, PARD3, PTEN, and TJP1) [9], have been demonstrated to exert a vital role in maintaining the appropriate intercellular space [10]. TJ proteins between thyroid epithelial cells can make belt-like structures jointing the luminal pole and limit the paracellular permeability [11]. In physiological situations, tight epithelial lining of thyroid gland as a paracellular barrier is crucial to euthyroidism. In contrast, under the pathological conditions, the dysfunction of TJ proteins leads to abnormal cell interval, which promotes the infiltration of T lymphocytes and might facilitate the exposure of normal secluded body antigens to immune system [11]. The above processes offer the possibility of TJ proteins dysfunction-induced chronic autoimmune inflammatory reactions and spur the occurrence of autoimmune diseases.
In recent years, numerous in vivo studies have observed the involvement of TJ molecules in autoimmune diseases, such as rheumatoid arthritis [12], systemic lupus erythematosus [13], and inflammatory bowel disease (IBD) [14,15,16]. In TJ gene families, MAGI2 and MAGI3, two closely linked genes mediated by phosphatase and tensin homologue (PTEN), have been identified as candidate susceptibility genes of IBD [14,15,16]. MAGI2 is reported to be significantly associated with Crohn’s disease (CD) and ulcerative colitis (UC) [16], while MAGI3 is also proved to have close associations with CD and UC [15]. Given the fact that AITDs share many genetic variations with other autoimmune diseases, we aimed to extend the observations about MAGI2 and MAGI3 to encompass AITDs. In this study, one SNP in MAGI2 gene (rs2160322) and one in MAGI3 (rs1343126) were detected in a set of 1001 patients with AITDs and 846 healthy controls in Chinese Han population.
Materials and methods
Informed consent and approval
The experiment was approved by the ethics committee of Jinshan Hospital of Fudan University. Informed consent was signed in both the patient group and the control group. All subjects in this experiment were voluntary and did not receive any financial compensation.
Study design, setting, and size
A case–control study was conducted to explore the relationship between MAGI2, MAGI3, and AITDs. This study included 1052 Chinese Han patients with an established diagnosis of AITDs and 874 healthy Chinese Han controls at Jinshan Hospital between the years of 2016 and 2017. Among them, 51 AITDs patients and 28 normal controls (NC) were excluded, because the DNA extraction concentration was too low (< 100 μg/ml) or the unqualified DNA purity (A260/280 was not between 1.8 and 2.0). The valid data ultimately included in this study came form 1001 AITD patients and 846 healthy controls.
Participants, diagnosis criteria, and subgroup
The AITDs’ group included a random sample of 625 GD patients (186 males and 439 females) and 376 HT patients (54 males and 322 females), with no subjective selectivity. All patients and normal controls came from Jinshan Hospital. Patients were arbitrarily recruited from Endocrinology Clinics, while healthy controls were consecutively enrolled from the Healthy Check-Up Center with ethnically and geographically matching.
The diagnosis criteria for GD used in this study met international requirements [7], including clinical manifestations of thyrotoxicosis, biochemical markers of hyperthyroidism, positive circulating thyroid-stimulating hormone receptor antibody (TRAb) and diffuse goiter of the thyroid gland observed by ultrasonography or palpation. The definition of HT cases was based on thyroid enlargement and high levels of autoantibodies [thyroid peroxidase antibody (TPOAb) or thyroglobulin antibody (TgAb)].
To more accurately investigate the relationship between SNPs and different clinical phenotypes of AITDs, we set clinical classifications of GD and HT in the current study, including: (1) the onset age of GD or HT (≤ 18 years or ≥ 19 years); (2) presence or absence thyrotoxic exophthalmos in GD group; (3) goiter or normal volume of thyroid gland; (4) euthyroidism or hypothyroidism in HT group; and (5) presence or absence of AITDs family history (disease in immediate relatives within three generations).
Graves’ ophthalmopathy (GO), also called thyroid-associated ophthalmopathy, is characterized by inflammation and fibrosis of the extra ocular muscles, chemosis, proptosis, excess tearing, and episcleral vascular injection [7]. The thyroid goiter was determined by palpation and was clinically divided into three degrees clinically. The definition of I degree is that the goiter cannot be seen, but it can be palpated. Degree II is defined as the visible and palpable goiter, but is still confined to the sternocleidomastoid region. The degree III is characterized by enlarged thyroid tissue beyond the sternocleidomastoid muscle [7]. Demographic statistics and clinical phenotypes of subjects in patient groups are shown in Table 1.
Potential bias
To rule out potential genetic background interference, we ensured that each patient was independent and had no genetic relationship. To minimize interference from environmental factors, all subjects included in this study lived in the same area (Shanghai, China). In addition, all members did not have any other immune disease, inflammatory infection, and chronic disease to eliminate interference from other diseases.
Sources of data and measurements
DNA sample collection and extraction
Genomic DNA was isolated by The Relax Gene Blood DNA System (Tiangen Biotech Co., Ltd., Beijing, China), from 1 ml peripheral venous blood of each subjects. To ensure that the extracted DNA had high quality, we used Nano Drop 2000 Spectro-photometer (Thermo Scientific Company, Waltham, MA, USA) to determine the concentration and purity of the extracted DNA. A DNA sample that satisfies both conditions of a concentration ≥ 100 ug/ml and A260/280 between 1.8 and 2.0 was considered a qualified sample. Unqualified DNA samples were discarded.
SNP selection and genotyping
Two TJ-related genes and two SNPs were investigated in the present study, MAGI2 (rs2160322) and MAGI3 (rs1343126). The products of these two genes interact with each other and belonged to the TJ protein network [9]. The multiplex polymerase chain reaction (PCR) method was used to amplify the target DNA sequence. Specific primer sequences were designed as follows: MAGI2 (rs2160322) upper primer—CTAAAGAAGGTGCCTCTGATTTCACTGG; lower primer—CTAGGAAGCTTTTGATTCTGCCTATTTGGG; MAGI3 (rs1343126) upper primer—GCAGAACACATTTCCTTATCATTTTCCC; lower primer—CATTGGGGTAATCCATTTAACATTAAACG.
Statistical analysis
Statistical methods, quantitative variables, and missing data
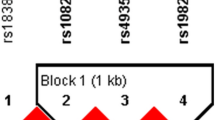
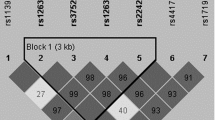
This study used SPSS statistical version 23 (IBM, Chicago, IL, USA) to calculate all odds ratios (OR), 95% confidence intervals (95% CI), and P values, based on the two-tailed Pearson Chi-square test (χ2 test) for genotype/allele frequency of each SNP. The P value < 0.05 was considered to be statistically significant. For each SNP, deviation from Hardy–Weinberg equilibrium (HWE) was estimated using the HWE program (http://ihg.gsf.de/cgi-bin/hw/hwa1.pl), and the P value (HWpval) of the two tag SNPs meets the criteria of HWpval > 0.05. Linkage analysis and haplotype analysis were also performed in this study. A linkage disequilibrium (LD) test was conducted using Haploview Software [version 4.2 (Broad Institute, Cambridge, MA, USA)]. In addition, because the mutation rate of polymorphism rs1343126 in MAGI3 (susceptible allele T) in our DNA samples was too low (< 5%), it was not enough to obtain reliable statistical results, so we have discarded this part of data. The data results associated with rs1343126 in MAGI3 would not appear in the next results section.
Adjustment and genotyping–clinical phenotype analysis
To consolidate the evidence, we performed an adjustment analysis and gave the P value before and after adjustment. Specifically, significant findings were further examined by multiple logistic regression, adjusting for potential interfering factors (gender and age) simultaneously. To obtain more detailed conclusions, we also performed an χ2 test analysis between each clinical subgroup.
Outcomes
The main outcome of this study was to confirm whether SNPs in MAGI2 and MAGI3 gene contributed to the etiology of AITDs. In addition, we further derived the relationship between different AITDs subtypes and MAGI2 gene (rs2160322).
Results
In the current study, we examined the frequency distribution for each allele and analyzed the association for each SNP in a case–control manner. Associations of rs2160322 in MAGI2 gene with AITDs, GD, and HT are shown in Table 2. In the genotype analysis, the SNP marker in MAGI2 (rs2160322) was weakly related to AITDs (P = 0.048) in the subjects, but was strongly correlated with GD (P = 0.012). The susceptibility allele G also showed a strong relationship with GD (P = 0.027; OR 1.91; 95% CI 1.020 and 1.391), and the trend was more significantly in females (P = 0.008; OR 1.304; 95% CI 1.072–1.587). In males, the genotype distribution displayed positive relationship (P = 0.036), while the allele distribution did not show any difference between patient group and normal controls. We further analyzed the genotype and allele frequencies of rs2160322 in MAGI2 in different GD clinical phenotypes, as shown in Table 3. We found that in the respect of family history, rs2160322 in MAGI2 was strongly correlated with those who had a positive family history (Pgenotype = 0.012; Pallele = 0.011, OR 1.412, 95% CI 1.083–1.843). However, there was neither correlation between GO and rs2160322 in MAGI2, nor correlation between early onset of disease and this gene locus. This suggests that female patients and those with family history are more closely related to rs2160322 compared to the whole patients group.
To analyze the relationship between rs2160322 and AITDs in more depth, we conducted genetical model analysis, which can be seen in Tables 4 and 5. From Table 4, we can acquire the information that for the total AITDs patients, both the recessive model and homozygous model embodied a strong correlation with AITDs (P = 0.016; P = 0.031, respectively), especially after the adjusting of the possible cofounders (age and gender) (P = 0.009; P = 0.019, respectively). As shown in Table 5, the GD group displayed significant association with either allele model, recessive model, or homozygous model of rs2160322 (P = 0.011, P = 0.003, and P = 0.003, respectively), despite after sex and age adjustment (P = 0.010, P = 0.004 and P = 0.005). It should be noted that although there was no obvious difference between the general GD populations and healthy controls in dominant model (P = 0.061), a statistically significant P value was observed between females’ GD patients and normal controls after adjusting for age (P = 0.008). In patients with positive GD family history, the allele model, dominant model, recessive model and homozygous model all displayed a strong positive P value after adjustment (P = 0.004, P = 0.039, P = 0.002, and P = 0.002, respectively). The results of this study suggested that there was a significant gender difference in the relationship between rs2160322 and AITDs, and their relationship was more pronounced in patients with a family history. No correlation between rs2160322 in MAGI2 and the HT group was observed in our experiment.
Discussion
In the present study, we found a strong correlation between the genotypes of rs2160322 in MAGI2 and individual’s susceptibility to GD. The frequency of the minor allele G was significantly higher in the GD patients than in the healthy controls, especially for GD females and those with family history.
GD, as an autoimmune disease, has a complex genetic background [7]. Our research team has previously found that GD is associated with SNPs of various immune genes, including CD40, CTLA4, STAT4, IL37, and so on [17,18,19]. Because autoimmune diseases have a degree of similarity in immune imbalance and genetic background, it is often found that certain genes are associated with multiple autoimmune diseases. The previous studies have found that MAGI2 and MAGI3 are associated with IBD [15, 16]. In this study, we, for the first time, found that MAGI2 rs2160322 was significantly related to GD. Our results suggest that the role of rs2160322 in promoting GD is more pronounced in female patients, which is consistent with the prevalence of gender differences in the incidence of GD. The dominant mechanism of women in GD has not been fully understood, and may be related to genetic differences, sex hormones, and psychological factors [20, 21].
Although GD is not a hereditary disease in the traditional sense, it has a certain degree of family aggregation and genetic susceptibility [22]. The probability of hyperthyroidism occurring in identical twins is as high as 30–60%, while fraternal twins are only 3–9% [1]. Furthermore, GD has the most obvious genetic predisposition in all the types of hyperthyroidism, while other types of hyperthyroidism appear to be not directly related to heredity [1]. Our study found that the relationship between rs2160322 and GD was pronounced in patients with family history in the subgroup analysis. Thus, mutations in the rs2160322 loci of MAGI2 gene may play a greater role in GD patients with family history.
MAGI2, located on chromosome 7, is a gene that contains roughly 1.4 megabases with 21 exons [16]. It encodes a scaffolding TJ protein of 2410 amino acids, which maintains the architecture of cell junctions and regulates the cell spacing [23]. MAGI2 protein includes six PDZ domains, two WW domains, and a guanylate kinase (GK) domain [24, 25]. The function of the above domains is quite sophisticated that endows MAGI2 with the capacity to interact with many extracellular compartments (cell adhesion molecules, receptors, and lumens) and intracellular signaling structures [26].
TJ is a complex of several integral membrane-spanning components, partly including claudin, zonula occludens (ZO), occludin, and junctional adhesion molecule (JAM) [10]. MAGI2 is associated with epithelial tight proteins assembly and appropriate localization [25,26,27]. Accordingly, it is plausible to consider that defects in MAGI2 expression or function may participate in the pathogenesis of AITDs by disassembly of TJ protein networks. In a previous study, high expression of three connexins was detected in GD, namely, ZO-1, JAM-A, and claudin [11]. However, HT displays a significant difference in TJ protein expression with GD. In HT, a high claudin level was demonstrated, while the expression of JAM-A and ZO-1 was lower than that of GD [11]. This discrepancy may partly explain why the SNP rs2160322 in MAGI2 does not play a great role in HT like in GD, as our result shows.
Lymphocyte transmigration has been demonstrated in the thyroid tissues of AITDs’ patient and is deemed to be a pathological feature of AITDs [3, 4], while MAGI2 has been proved to inhibit cell migration and proliferation [28]. Infiltrating T-helper 1 (Th1) cells have been found to impair the epithelial barrier seriously, through releasing IFN-γ, a cytokine that can downregulate a junction protein (claudin-1) in cultured thyroid tissue of GD patients in vitro [29, 30]. Nilsson et al. revealed that IL-1α, local-delivered by thyroid follicular epithelial cells and monocytes, can negatively regulate the TJ complex and provoke paracellular flow in cultured thyrocytes [31]. Similarly, IL-1β has been confirmed a depressor of TJ proteins’ (Claudin and ZO-1) expression and may alter their sub-cellar distribution in the thyroid of AITDs patients [11]. In addition, Rebuffat et al. pointed out that the epithelium destruction or alteration of follicular tightness in AITDs may promote the contact of the autoantigen with immune system [11]. Based on the above-mentioned studies and consisted with our present experiment, we can make a reasonable assumption that the variants of MAGI2 could influence the lymphocyte trans-endothelial infiltration and contribute to the etiology of GD.
The important role of apoptosis in the occurrence and development of AITD are widely recognized, and MAGI2 dysfunction-induced cell apoptosis has been demonstrated in the previous literatures [32, 33]. Nevertheless, the effects of MAGI2 dysfunction-induced thyroid apoptosis have not been clearly established yet. There is a close functional relation between MAGI2 and PTEN [14, 27], one other TJ gene that is relevant to thyroid cell apoptosis [34]. Under normal conditions, MAGI2 upregulates PTEN expression by reducing protein degradation [26, 35], and improves PTEN stability [35]. PTEN, localized on chromosome 10q23.3, encodes a protective lipid phosphatase protein that deregulates the phosphatidylinositol 3-kinase (PI3K) [35]. PI3K is a ubiquitous and proapoptotic lipid kinase that plays a crucial role in cell apoptosis and inflammatory response through activating chemokine receptors and promoting leukocyte migration [36]. PTEN inactivation caused by the deletion or mutation of MAGI2 could activate the PI3K pathway, with consequent thyroid apoptosis and immune dysregulation, manifesting as autoimmune disorders and chronic inflammation [36]. In addition, DNA released from apoptotic cells stimulates the immune response, forming a positive feedback loop that further initiates and continues the autoimmune process [37]. Therefore, besides effects on junctional assembly, alterations in the balance of epithelial cell viability and apoptosis may represent a supplemental consequence of MAGI2 gene mutations associated with GD.
Our results first confirmed that the variants of MAGI2 gene were novel risk factors for GD and made a reasonable assumption for the pathophysiological mechanisms behind it. However, our research is limited to the Chinese Han population, and there may be racial bias. It is necessary to expand the scope of research to populations of different regions and races to get a more authoritative conclusion. Moreover, we need to conduct further researches about other TJ genes, so as to clarify the biological mechanism between TJ gene families and AITDs.
References
De Leo S, Lee SY, Braverman LE (2016) Hyperthyroidism. Lancet 388(10047):906–918. https://doi.org/10.1016/S0140-6736(16)00278-6
Marino M, Latrofa F, Menconi F, Chiovato L, Vitti P (2014) An update on the medical treatment of Graves’ hyperthyroidism. J Endocrinol Investig 37(11):1041–1048. https://doi.org/10.1007/s40618-014-0136-z
Effraimidis G, Wiersinga WM (2014) Mechanisms in endocrinology: autoimmune thyroid disease: old and new players. Eur J Endocrinol 170(6):R241–R252. https://doi.org/10.1530/EJE-14-0047
Smith TJ, Hegedus L (2016) Graves’ Disease. The New England journal of medicine 375(16):1552–1565. https://doi.org/10.1056/NEJMra1510030
Jabrocka-Hybel A, Skalniak A, Piatkowski J, Turek-Jabrocka R, Vyhouskaya P, Ludwig-Slomczynska A, Machlowska J, Kapusta P, Malecki M, Pach D, Trofimiuk-Muldner M, Lizis-Kolus K, Hubalewska-Dydejczyk A (2018) How much of the predisposition to Hashimoto’s thyroiditis can be explained based on previously reported associations? J Endocrinol Investig. https://doi.org/10.1007/s40618-018-0910-4 (Epub ahead of print)
Marino M, Latrofa F, Menconi F, Chiovato L, Vitti P (2015) Role of genetic and non-genetic factors in the etiology of Graves’ disease. J Endocrinol Investig 38(3):283–294. https://doi.org/10.1007/s40618-014-0214-2
Menconi F, Marcocci C, Marino M (2014) Diagnosis and classification of Graves’ disease. Autoimmun Rev 13(4–5):398–402. https://doi.org/10.1016/j.autrev.2014.01.013
Tomer Y (2014) Mechanisms of autoimmune thyroid diseases: from genetics to epigenetics. Annu Rev Pathol 9:147–156. https://doi.org/10.1146/annurev-pathol-012513-104713
Szklarczyk D, Franceschini A, Wyder S, Forslund K, Heller D, Huerta-Cepas J, Simonovic M, Roth A, Santos A, Tsafou KP, Kuhn M, Bork P, Jensen LJ, von Mering C (2015) STRING v10: protein-protein interaction networks, integrated over the tree of life. Nucleic Acids Res 43(Database issue):D447–D452. https://doi.org/10.1093/nar/gku1003
Tsukita S, Yamazaki Y, Katsuno T, Tamura A, Tsukita S (2008) Tight junction-based epithelial microenvironment and cell proliferation. Oncogene 27(55):6930–6938. https://doi.org/10.1038/onc.2008.344
Rebuffat SA, Kammoun-Krichen M, Charfeddine I, Ayadi H, Bougacha-Elleuch N, Peraldi-Roux S (2013) IL-1beta and TSH disturb thyroid epithelium integrity in autoimmune thyroid diseases. Immunobiology 218(3):285–291. https://doi.org/10.1016/j.imbio.2012.05.016
Fang TJ, Lin CH, Lin YZ, Li RN, Ou TT, Wu CC, Tsai WC, Yen JH (2016) F11R mRNA expression and promoter polymorphisms in patients with rheumatoid arthritis. Int J Rheum Dis 19(2):127–133. https://doi.org/10.1111/1756-185X.12663
Miyagawa H, Yamai M, Sakaguchi D, Kiyohara C, Tsukamoto H, Kimoto Y, Nakamura T, Lee JH, Tsai CY, Chiang BL, Shimoda T, Harada M, Tahira T, Hayashi K, Horiuchi T (2008) Association of polymorphisms in complement component C3 gene with susceptibility to systemic lupus erythematosus. Rheumatology 47(2):158–164. https://doi.org/10.1093/rheumatology/kem321
Noren E, Mellander MR, Almer S, Soderman J (2018) Genetic variation and gene expression levels of tight junction genes indicates relationships between PTEN as well as MAGI1 and microscopic colitis. Dig Dis Sci 63(1):105–112. https://doi.org/10.1007/s10620-017-4857-7
Noren E, Almer S, Soderman J (2017) Genetic variation and expression levels of tight junction genes identifies association between MAGI3 and inflammatory bowel disease. BMC Gastroenterol 17(1):68. https://doi.org/10.1186/s12876-017-0620-y
McGovern DP, Taylor KD, Landers C, Derkowski C, Dutridge D, Dubinsky M, Ippoliti A, Vasiliauskas E, Mei L, Mengesha E, King L, Pressman S, Targan SR, Rotter JI (2009) MAGI2 genetic variation and inflammatory bowel disease. Inflamm Bowel Dis 15(1):75–83. https://doi.org/10.1002/ibd.20611
Yan N, Meng S, Song RH, Qin Q, Wang X, Yao Q, Jiang Y, Jiang W, Shi L, Xu J, Zhang J (2015) Polymorphism of IL37 gene as a protective factor for autoimmune thyroid disease. J Mol Endocrinol 55(3):209–218. https://doi.org/10.1530/JME-15-0144
Yan N, Meng S, Zhou J, Xu J, Muhali FS, Jiang W, Shi L, Shi X, Zhang J (2014) Association between STAT4 gene polymorphisms and autoimmune thyroid diseases in a Chinese population. Int J Mol Sci 15(7):12280–12293. https://doi.org/10.3390/ijms150712280
Yang J, Qin Q, Yan N, Zhu YF, Li C, Yang XJ, Wang X, Pandey M, Hou P, Zhang JA (2012) CD40 C/T(−1) and CTLA-4 A/G(49) SNPs are associated with autoimmune thyroid diseases in the Chinese population. Endocrine 41(1):111–115. https://doi.org/10.1007/s12020-011-9510-1
Gabrielson AT, Sartor RA, Hellstrom WJG (2018) The impact of thyroid disease on sexual dysfunction in men and women. Sex Med Rev. https://doi.org/10.1016/j.sxmr.2018.05.002
De Leo S, Pearce EN (2018) Autoimmune thyroid disease during pregnancy. Lancet Diabetes Endocrinol 6(7):575–586. https://doi.org/10.1016/S2213-8587(17)30402-3
McLeod DS, Cooper DS (2012) The incidence and prevalence of thyroid autoimmunity. Endocrine 42(2):252–265. https://doi.org/10.1007/s12020-012-9703-2
Goldstein J, Goyal R, Roland JT, Gellert LL, Clark PE, Hameed O, Giannico GA (2016) MAGI-2 is a sensitive and specific marker of prostatic adenocarcinoma: a comparison with AMACR. Am J Clin Pathol 146(3):294–302. https://doi.org/10.1093/ajcp/aqw111
Hirao K, Hata Y, Ide N, Takeuchi M, Irie M, Yao I, Deguchi M, Toyoda A, Sudhof TC, Takai Y (1998) A novel multiple PDZ domain-containing molecule interacting with N-methyl-d-aspartate receptors and neuronal cell adhesion proteins. J Biol Chem 273(33):21105–21110. https://doi.org/10.1074/jbc.273.33.21105
Ingham RJ, Colwill K, Howard C, Dettwiler S, Lim CS, Yu J, Hersi K, Raaijmakers J, Gish G, Mbamalu G, Taylor L, Yeung B, Vassilovski G, Amin M, Chen F, Matskova L, Winberg G, Ernberg I, Linding R, O’Donnell P, Starostine A, Keller W, Metalnikov P, Stark C, Pawson T (2005) WW domains provide a platform for the assembly of multiprotein networks. Mol Cell Biol 25(16):7092–7106. https://doi.org/10.1128/MCB.25.16.7092-7106.2005
Nagashima S, Kodaka M, Iwasa H, Hata Y (2015) MAGI2/S-SCAM outside brain. J Biochem 157(4):177–184. https://doi.org/10.1093/jb/mvv009
Wu X, Hepner K, Castelino-Prabhu S, Do D, Kaye MB, Yuan XJ, Wood J, Ross C, Sawyers CL, Whang YE (2000) Evidence for regulation of the PTEN tumor suppressor by a membrane-localized multi-PDZ domain containing scaffold protein MAGI-2. Proc Natl Acad Sci USA 97(8):4233–4238. https://doi.org/10.1073/pnas.97.8.4233
Hu Y, Li Z, Guo L, Wang L, Zhang L, Cai X, Zhao H, Zha X (2007) MAGI-2 Inhibits cell migration and proliferation via PTEN in human hepatocarcinoma cells. Arch Biochem Biophys 467(1):1–9. https://doi.org/10.1016/j.abb.2007.07.027
Tedelind S, Ericson LE, Karlsson JO, Nilsson M (2003) Interferon-gamma down-regulates claudin-1 and impairs the epithelial barrier function in primary cultured human thyrocytes. Eur J Endocrinol 149(3):215–221. https://doi.org/10.1530/eje.0.1490215
Antonelli A, Ferrari SM, Corrado A, Franceschini SS, Gelmini S, Ferrannini E, Fallahi P (2014) Extra-ocular muscle cells from patients with Graves’ ophthalmopathy secrete alpha (CXCL10) and beta (CCL2) chemokines under the influence of cytokines that are modulated by PPARgamma. Autoimmun Rev 13(11):1160–1166. https://doi.org/10.1016/j.autrev.2014.08.025
Nilsson M, Husmark J, Bjorkman U, Ericson LE (1998) Cytokines and thyroid epithelial integrity: interleukin-1alpha induces dissociation of the junctional complex and paracellular leakage in filter-cultured human thyrocytes. J Clin Endocrinol Metab 83(3):945–952. https://doi.org/10.1210/jcem.83.3.4626
Shirata N, Ihara KI, Yamamoto-Nonaka K, Seki T, Makino SI, Oliva Trejo JA, Miyake T, Yamada H, Campbell KN, Nakagawa T, Mori K, Yanagita M, Mundel P, Nishimori K, Asanuma K (2017) Glomerulosclerosis induced by deficiency of membrane-associated guanylate kinase inverted 2 in kidney podocytes. J Am Soc Nephrol JASN 28(9):2654–2669. https://doi.org/10.1681/ASN.2016121356
Li X, Li Z, Li N, Qi J, Fan K, Yin P, Zhao C, Liu Y, Yao W, Cai X, Wang L, Zha X (2013) MAGI2 enhances the sensitivity of BEL-7404 human hepatocellular carcinoma cells to staurosporine-induced apoptosis by increasing PTEN stability. Int J Mol Med 32(2):439–447. https://doi.org/10.3892/ijmm.2013.1411
Eng C (2002) Role of PTEN, a lipid phosphatase upstream effector of protein kinase B, in epithelial thyroid carcinogenesis. Ann N Y Acad Sci 968:213–221
Larson SD, Jackson LN, Riall TS, Uchida T, Thomas RP, Qiu S, Evers BM (2007) Increased incidence of well-differentiated thyroid cancer associated with Hashimoto thyroiditis and the role of the PI3k/Akt pathway. J Am Coll Surg 204(5):764–773. https://doi.org/10.1016/j.jamcollsurg.2006.12.037
Guaraldi F, Di Nardo G, Tarani L, Bertelli L, Susca FC, Bagnulo R, Resta N (2017) Association of autoimmune thyroiditis and celiac disease with juvenile polyposis due to 10q23.1q23.31 deletion: Potential role of PI3K/Akt pathway dysregulation. Eur J Med Genet 60(7):380–384. https://doi.org/10.1016/j.ejmg.2017.04.010
Grossman L, Chang C, Dai J, Nikitin PA, Jima DD, Dave SS, Luftig MA (2017) Epstein-Barr virus induces adhesion receptor CD226 (DNAM-1) expression during primary B-cell transformation into lymphoblastoid cell lines. mSphere 2(6):115–123. https://doi.org/10.1128/msphere.00305-17
Acknowledgements
The present work was supported by grants from the National Natural Science Foundation of China (nos. 81670722 and 81471004).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The experiment was approved by the ethics committee of Jinshan Hospital of Fudan University.
Informed consent
Informed consent was signed in both the patient group and the control group. All subjects in this experiment were voluntary and did not receive any financial compensation.
Rights and permissions
About this article
Cite this article
Jia, X., Zhai, T., Wang, B. et al. The MAGI2 gene polymorphism rs2160322 is associated with Graves’ disease but not with Hashimoto’s thyroiditis. J Endocrinol Invest 42, 843–850 (2019). https://doi.org/10.1007/s40618-018-0990-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-018-0990-1