Abstract
Background
Autoimmune thyroid disease (ATD) patients may have a higher prevalence of anti-parietal cell antibodies (APCA) than normal population.
Objective
To study the prevalence of APCA in a cohort of ATD patients to know its association with patient’s clinical profile and gastrointestinal complaints.
Methods
APCA was sought for by indirect immunofluorescence test in 243 ATD patients: 136 (55.9%) with Graves’ disease and 107 (44.0%) with Hashimoto’s thyroiditis. A structured questionnaire for gastrointestinal symptoms, previous history of thrombosis, arthralgia and other autoimmune diseases in the patients and their families was applied. Positive and negative APCA individuals were compared. Positive patients were invited to perform upper gastrointestinal endoscopy and biopsy of duodenum segments. Sera from 100 healthy individuals from the same geographic area were used as controls.
Results
APCA was present in 20.1% (49/243) of ATD patients: 21.3% (29/136) in the Graves’ sample and 18.6% (20/107) in the Hashimoto’s sample (p = 0.61). Patients with positive APCA had more anemia (p = 0.03; OR = 2.89; 95% CI = 1.03–8.07) and less heartburn (p = 0.01; OR = 0.4; 95% CI = 0.20–0.83). Among the group of 49 APCA-positive patients, 24 agreed with upper endoscopy and it was found that 54.1% had atrophic gastritis.
Conclusions
There is a high prevalence of positive APCA in ATD patients. APCA are more common in those with anemia and less common in those with complaints of heartburn. Almost half of positive APCA patients had atrophic gastritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The hallmark of pernicious anemia (PA), a complication of autoimmune metaplastic atrophic gastritis (AMAG), is the anti-parietal cell antibody (APCA), considered to be highly sensible for this disease [1]. It is found in 85–90% of the pernicious anemia patients [2], but their presence is not enough for diagnosis, as they are not specific for this illness. These antibodies are also found in 7.8–19.5% of apparently healthy adult individuals [2]. There is a fascinating and not fully elucidated question on whether the infection by Helicobacter pylori is related to APCA presence [3]. APCA are found from 6.1% to up to 20.7% of these patients and this infectious agent has been proposed to be one of the etiologic agents of AMAG [2, 4]. The target for APCA is the H+/K + ATPase, a proton pump with two subunits: the alpha and beta. Both are targeted by this autoantibody, although the major antigen seems to be the alpha subunit [2]. It is proposed that molecular mimicry between H+/K + ATPase subunits and pathogen-derived peptides (such as those from H. pylori) stimulate autoreactive gastric CD4 + T cells. In this context, the loss of immunological tolerance is increased by genetic susceptibility, as T cells recognize antigen peptides bound to human leucocyte antigen (HLA) and HLA-DRB1*03 and DRB1*04 have been linked to the occurrence of PA [5].
Destruction of parietal cells in the stomach [2], atrophy of the mucosa, especially in the body and fundus, associated with hypo or achlorhydria, secondary hypergastrinemia, antral G-cell hyperplasia and low serum pepsinogen (PG) I concentrations are consequences of this reaction [2]. Thus, patients with AMAG are not only at increased risk for developing pernicious anemia but also neuroendocrine tumors of the gastric body and gastric cancer [5].
Autoimmune disorders may cluster in the same patient [6]. It is discussed if this clustering is due to a shared genetic background or to an exposure to a common triggering event. In this context, a high prevalence of AMAG in patients with type 1 diabetes mellitus, autoimmune thyroid diseases (ATD), vitiligo and celiac disease has been observed [6, 7]. Type 1 diabetes mellitus, ATD, and AMAG often occur together, forming the so-called autoimmune polyendocrine syndrome type 3 [7].
Gerenova et al. [8] found an APCA prevalence of 33.8% in Hashimoto’s thyroiditis and observed that the positive patients required treatment with a higher dose of levothyroxine than the negatives. Patients with gastric disorders such as chronic gastritis and H. pylori infection may need higher doses of oral thyroxine due to malabsorption [9].
Garcia et al. [10] found a prevalence of 20% of APCA positivity in patients with ATD and, in their study, the risk of APCA positivity was elevated in patients with high levels of anti-thyroglobulin and anti-peroxidase antibodies.
In the present study, we analyzed a cohort of patients with ATD (Hashimoto’s thyroiditis and Grave’s disease) for the presence of APCA, aiming to know their prevalence in our region and their association with epidemiologic data and clinical symptoms.
Methods
This study was approved by the local Ethics Research Committee and all participants signed a written consent. This is a cross-sectional study that included consecutively, from the years of 2007 to 2011, a non-probabilistic sample of previously diagnosed patients with ATD from a single adult Endocrinology Unit at the Clinics Hospital of the Federal University of Paraná. A total of 243 patients were investigated: 136 (55.9%) with Graves’ disease and 107 (44.0%) with Hashimoto’s thyroiditis; 213 (87.3%) were female and the mean age was 45.1 ± 13.4 years (range 15–79 years).
All patients were submitted to a structured questionnaire for gastrointestinal symptoms, previous history of thrombosis, arthralgia and history of other autoimmune diseases in the family and themselves (rheumatoid arthritis, systemic lupus, vitiligo, diabetes mellitus type 1, alopecia areata, psoriasis, myasthenia gravis, autoimmune hepatitis and celiac disease). Women were questioned about gynecological and obstetric history. Charts were reviewed for diagnosis, epidemiological data, information on body mass index, presence of anemia, TSH (thyroid stimulating hormone) and free T4 (thyroxine) levels, treatment and presence of osteoporosis. At the time of interview, 10 ml of venous blood sample was collected, aliquoted and stored at −80 °C until serological tests were performed.
As control group, one hundred healthy volunteers were studied from the same geographic area (93% female, 7% male, mean age 42 years, range 19–81 years), not related to the patients, with no digestive or extra-digestive symptoms, nor thyroid disease.
Serum levels of APCA were evaluated by indirect immunofluorescence (IFT) using FITC polyclonal anti-human globulin conjugate (GMK, Porto Alegre, Brazil) and cryostatic tissue sections of rat stomach as substrate, according to previously described [11]. APCA were reported as positive if there was cytoplasmic staining of parietal cells. A screening dilution of 1:40 was used. Titers up to 1:80 are considered low; until 1:160 as moderate and equal or over to 1:320 as high titers. All serologic examinations were blinded and done in the same laboratory. Positive samples were tittered up to the end point.
From 49 anti-parietal cell antibody-positive patients, 24 (47.0%) were clinically re-evaluated and submitted to upper gastric endoscopy and biopsy of oxyntic and angular/antral segments, to search for characteristics of atrophic gastritis. Fragments were fixed in formol and drenched in paraffin. Multiple histology sections (5 µm thick) were obtained from paraffin-embedded biopsies. Sections were stained using the hematoxylin–eosin technique (H&E), periodic acid–Schiff, and modified Giemsa for H. pylori. At each biopsy sample site, gastritis was distinguished in non-atrophic and atrophic. Mucosal atrophy was scored according to the Sydney system using a visual analogic scale (0 = absent; 1 = mild; 2 = moderate; 3 = severe), based on the topographic locations (oxyntic and angular/antral) of the histology changes [12].
Data were collected in frequency and contingency data. The distribution was evaluated by the Kolmogorov–Smirnov test; central tendency was expressed in median and interquartile range (IQR) and mean and standard deviation (SD). Patients were divided in APCA positive and negative and compared between themselves: the whole group as well as the groups of Graves’ patients and Hashimoto’s thyroiditis separately. Comparison of numeral data was done by Fisher’s and Chi-squared test and numerical data by Mann–Whitney and unpaired t test. The adopted significance was of 5%.
Results
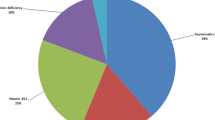
In the studied ATD patients, the prevalence of positivity for APCA was of 49/243 (20.1%), while in healthy controls it was of 1/100 (1%; p < 0.0001). In ATD patients, the titers of APCA positivity ranged from 1:80 to 1:20.480 and in this sample 6/49 (12.2%) had low titers; 11/49 (22.4%) had moderate and 32/49 (65.3%) had high titers. Graves’ patients had a prevalence of APCA of 29/136 (21.3%) and Hashimoto’s thyroiditis of 20/107 (18.6%; p = 0.61). Both groups had median titers of 1:320, without differences between them (p = 0.32).
Table 1 shows the sample description as well as the comparison of all ATD patients with and without APCA. It is possible to observe that APCA-positive patients had more anemia (p = 0.03; OR = 2.89; 95% CI = 1.03–8.07) and less complaints of heartburn (p = 0.01; OR = 0.4; 95% CI = 0.20–0.83) than that without this antibody.
In Table 2, there is the comparison between positive and negative APCA in the Graves’ disease and in the Hashimoto’s thyroiditis patients. Anemia was associated with APCA positivity just in the Graves’ patients (33.3%; p = 0.003; OR = 8.7; 95% CI = 2.1–35.6), while in either groups there was a negative association (Hashimoto’s group) or tendency to negative association (Graves’ group) of APCA presence with gastrointestinal symptoms.
From the group of 49 APCA-positive patients, 24 agreed with upper gastrointestinal endoscopy. It was found that 9/24 (37.5%) had H. pylori infection and 13/24 (54.1%) had signs of atrophic gastritis. In the group of patients with APCA positive and atrophic gastritis, 8/13 (61.5%) had Graves’ disease and 5/13 (38.4%) had Hashimoto’s thyroiditis (p = 0.43). About 6/13 (46.1%) patients with atrophic gastritis had also H. pylori infection, while 6/9 (66.6%) of H. pylori-infected patients had atrophic gastritis. The comparison of ACPA titers in H. pylori-positive (median 1:480; IQR 1:140–1:800) and negative patients (median 1:320; IQR = 1:120–1:640) showed no statistical difference (p = 0.48). The same was observed in the comparison of ACPA titers in patients with atrophic gastritis (median value of 1:640; IQR = 1:120–1:640) and without it (median 1:160; IQR 1:60–1:320) with p = 0.27. In the H. pylori-positive group, 2/9 (22.2%) had low titers of ACPA; 1/9 (11.1%) had moderate and 6/9 (66.6%) had high titers; the H. pylori negative had 2/15 (13.3%) with low, 3/15 (20%) with moderate and 10/15 (66.6%) with high titers (p = 0.76). In the atrophic gastritis, positive patients 3/13 (23.07%) had low titers; 1/13 (7.5%) had moderate and 9/13 (89.2%) had high titers; in the negative group 2/11 (18.1%) had low; 4/11 (36.3%) had moderate and 5/11 (45.4%) had high titers of APCA (p = 0.42).
Discussion
Currently, a high prevalence of APCA (almost 20%) was found in patients with ATD corroborating the statement that autoimmune disorders have a tendency to group in a single patient [13]. This statement was also supported by the high number of autoimmune diseases other than AMAG and ATD found to be associated not only in our group of patients (10%) but also in their relatives (almost 40%). Our ATD sample had a lower prevalence of APCA than those of Centanni et al. [14], that found 40% of positivity to APCA in their 62 ATD patients from Italy, but a similar prevalence to the 20% found by Garcia–Garcia et al. [10] studying 148 ATD patients from Spain. The association of thyroid disease with pernicious anemia is recognized since early 1960s; the expression ‘thyrogastric autoimmunity’ was used to point this combination of diseases [7, 15, 16].
No ethnic background was found to be more prevalent among the APCA-positive patients in this analysis. Pernicious anemia, once considered to be a disease of elderly females of Northern European ethnicity, has been subsequently detected in almost all ethnicities (White, Afrodescendants and non-white Hispanic) with equal prevalence [17].
The results of the present analysis showed, as expected, that patients with positive APCA had more anemia. Anemia shows up in this context because of these antibodies that can induce destruction of gastric parietal cells, resulting in failure of intrinsic factor production [18, 19]. Intrinsic factor deficiency may cause insufficient absorption of vitamin B12, that finally leads to the status of pernicious anemia [18]. In addition, iron deficiency may contribute to anemia in this situation, as iron is best absorbed in an acidic environment [20, 21]. Sibilla et al. [22], analyzing causes of chronic unexplained anemia in ATD individuals found that its prevalence was higher in those with ATD associated with other autoimmune disorders than in those with plain ATD. They also found that it was more prevalent in individuals with hypothyroidism. Interestingly, in the present analysis, when Graves’ patients were studied apart from those with Hashimoto’s thyroiditis, anemia could not be proven to be associated with APCA positivity in this last group. Maybe, if the number of Hashimoto’s patients were higher, we would have similar results. As in our country, most of the HT patients are treated by the general practitioner, we had, in the present sample, a higher number of Graves’ patients, that are usually sent to an university hospital.
Another remarkable finding of the current study was that patients with positive APCA had less gastrointestinal complaints than those with positivity for this autoantibody. The low prevalence of heartburn may be explained by the lower acidic environment seen in patients with atrophic gastritis. This finding is important for daily practice, as the clinician should not wait for gastrointestinal complaints to explore this diagnostic possibility. Our findings diverge from those of Carabotti et al. [23] that found a high prevalence of dyspepsia in their cohort of patients with AMAG. However, these authors studied only patients with AMAG, and not with positive APCA as we did. In addition, differences in the prevalence of co-existence of H. pylori infection may be a confusing factor.
Although APCA is considered a screening tool for AMAG, this autoantibody may be found in situations without known clinical meaning [2]. Only half of our APCA-positive patients had AMAG. However, it is possible that some of the individuals presently studied, still will develop the disease in the future. A careful follow-up of positive APCA patients will help to elucidate this aspect. Tozzoli et al. [24] followed prospectively 25 ATD patients that were APCA positive, and found that almost one-fourth of them (24%) developed autoimmune gastritis within 5 years.
The association between H. pylori infection and AMAG is debated. About 60% of our patients with biopsy-proven AMAG also had this infection. H. pylori infection has been implicated in the triggering of several autoimmune disorders such as systemic lupus, Sjögren syndrome, vasculitis, autoimmune skin conditions, idiopathic thrombocytopenic purpura, multiple sclerosis, neuromyelitis, among others [3]. In the context of AMGA, it has been found that there is antigen mimicry between H. pylori lipopolysaccharides and epitopes from beta subunit of the H+/K + ATPase of the parietal cells [2]. Other authors have noted that some H. pylori components, particularly urease, have been shown to stimulate B cells to produce IgM rheumatoid factor, anti-ds-DNA and anti-phospholipid choline antibodies [25]. Helicobacter pylori infection, by itself is associated with atrophic gastritis, and the association of atrophic gastritis and these infections increases the malignancy risk [2, 14].
Anemia was the main clinical sign that suggested that associated AMAG in an ATD patient. Another sign that this is happening is drug malabsorption [9, 26]; ATD patients with AMAG may have increased T4 requirement due to impairment of gastric secretion and motility [26]. This is very important as PA may develop unperceptively over many years, remaining undiagnosed [2]. However, these individuals have a heightened risk of irreversible neurologic disorders caused by B12 deficiency, such as numbness, paresthesia, weakness and ataxia. In addition, these patients have significantly higher risk of developing intestinal-type gastric adenocarcinoma, pyloric gland adenoma, squamous cell carcinomas and gastric carcinoid tumors [14]. According to a meta-analysis that included other 6 studies and 453 patients, the overall relative risk of gastric cancer in patients with pernicious anemia is 6.8 (95% CI 2.6–18.1) [14]. Thus, diagnosing atrophic gastritis is important to establish preventing measures in this context.
The limitations of our study are mainly its cross-sectional nature and the fact that only half of APCA-positive patients agreed with endoscopy. It is possible that this low number of patients with endoscopy did not allow correct observations on variation of ACPA titers in H. pylori-positive and -negative individuals as well as in those with and without atrophic gastritis. Nevertheless, it does highlight the need for and active search of AMAG in patients with ATD, despite presence of gastrointestinal complaints.
To summarize, it is possible to say that ATD patients have a 20% prevalence of APCA, equally distributed in Graves’ disease and Hashimoto’s thyroiditis. ATD patients with APCA had more anemia and less heartburn than those without it. AMAG was detected in almost half of positive APCA patients, but prospective studies with a long follow-up are needed for a better evaluation of atrophic gastritis occurrence in this context.
References
Minalyan A, Benhammou JN, Artashesyan A, Lewis MS, Pisegna JR (2017) Autoimmune atrophic gastritis: current perspectives. Clin Exp Gastroenterol 10:19–27
Rusak E, Chobot A, Krzywicka A, Wenzlau J (2016) Anti-parietal cell antibodies–diagnostic significance. Adv Med Sci 61:175–179
Smyk DS, Koutsoumpas AL, Mytilinaiou MG, Rigopoulou EI, Sakkas LI, Bogdanos DP (2014) Helicobacter pylori and autoimmune disease: cause or bystander. World J Gastroenterol 20:613–629
Šterzl I, Hrdá P, Matucha P, Čeřovská J, Zamrazil V (2008) Anti-Helicobacter pylori, anti-thyroid peroxidase, anti-thyroglobulin and anti-gastric parietal cells antibodies in Czech population. Physiol Res 57(S1):S135–S141
Lahner E, Annibale B (2009) Pernicious anemia: new insights from a gastroenterological point of view. World J Gastroenterol 15:5121–5128
Venerito M, Radünz M, Reschke K, Reinhold D, Frauenschläger K, Jechorek D et al (2015) Autoimmune gastritis in autoimmune thyroid disease. Aliment Pharmacol Ther 41:686–693
Cellini M, Santaguida MG, Virili C, Capriello S, Brusca N, Gargano L et al (2017) Hashimoto’s thyroiditis and autoimmune gastritis. Front Endocrinol (Lausanne) 26:8–92. doi:10.3389/fendo.2017.00092 (eCollection 2017)
Gerenova B, Manolova IM, Tzoneva VI (2013) Clinical significance of auto antibodies to parietal cells in patients with autoimmune thyroid diseases. Folia Med (Plovdiv) 55:26–32
Santaguida MG, Virili C, Del Duca SC, Cellini M, Gatto I, Brusca N, De Vito C, Gargano L, Centanni M (2015) Thyroxine softgel capsule in patients with gastric-related T4 malabsorption. Endocrine 49:51–57
García-García B, GimenoOrna JA, Aguillo GE, AltemirTrallero J, Cabrejas Gómez C, Ilundaín González A et al (2010) Prevalence and predictive factors of parietal cell antibody positivity in autoimmune thyroid disease. Endocrinol Nutr 57:49–53
Bigazzi PE, Rose NR (1984) Pruebas para anticuerpos contra antigenos tissulares especificos. In: Rose NR, Friedman H (eds) El laboratorio en inmunologia clínica, 2nd edn. Editorial Medica Pan Americana, Buenos Aires, pp 968–979
Neumann WL, Coss E, Rugge M, Genta RM (2013) Autoimmune atrophic gastritis-pathogenesis, pathology and management. Nat Rev Gastroenterol Hepatol 10:529–541
Fallahi P, Ferrari SM, Ruffilli I, Elia G, Biricotti M, Vita R et al (2016) The association of other autoimmune diseases in patients with autoimmune thyroiditis: review of the literature and report of a large series of patients. Autoimmun Rev 15:1125–1128
Centanni M, Marignani M, Gargano L, Corleto VD, Casini A, DelleFave G et al (1999) Atrophic body gastritis in patients with autoimmune thyroid disease: an underdiagnosed association. Arch Intern Med 159:1726–1730
Irvine WJ, Cullen DR, Mawhinney H (1974) Natural history of autoimmune achlorhydric atrophic gastritis. A 1–15-year follow-up study. Lancet 2:482–485
Singer W, Sahay BM (1966) Myasthenia gravis, Hashimoto’s thyroiditis, and pernicious anaemia. Br Med J 1(5492):904
Park JY, Lam-Himlin D, Vemulapalli R (2013) Review of autoimmune metaplastic atrophic gastritis. Gastrointest Endosc 77:284–292
Wu YH, Chang JYF, Wang YP, Wu YC, Chen HM, Sun A (2017) Anemia and hematinic deficiencies in anti-gastric parietal cell antibody-positive and -negative recurrent aphthous stomatitis patients with anti-thyroid antibody positivity. J Formos Med Assoc 116:145–152
Oh RC, Brown DL (2003) Vitamin B12 deficiency. Am Fam Phys 67:979e86
Lopez A, Cacoub P, Macdougall IC, Peyrin-Biroulet L (2016) Iron deficiency anaemia. Lancet 387(10021):907–916
Wang YP, Lin HP, Chen HM, Kuo YS, Lang MJ, Sun A (2014) Hemoglobin, iron, and vitamin B12 deficiencies and high blood homocysteine levels in patients with anti-thyroid autoantibodies. J Formos Med Assoc 113:155–160
Sibilla R, Santaguida MG, Virili C, Gargano L, Nardo S, Guardia MD et al (2008) Chronic unexplained anaemia in isolated autoimmune thyroid disease or associated with autoimmune related disorders. Clin Endocrinol (Oxf) 68:640–645
Carabotti M, Lahner E, Esposito G, Sacchi MC, Severi C, Annibale B (2017) Upper gastrointestinal symptoms in autoimmune gastritis: a cross-sectional study. Medicine (Baltimore) 96:e5784
Tozzoli R, Kodermaz G, Perosa AR, Tampoia M, Zucano A, Antico A et al (2010) Autoantibodies to parietal cells as predictors of atrophic body gastritis: a five-year prospective study in patients with autoimmune thyroid diseases. Autoimmun Rev 10:80–83
Yamanishi S, Iizumi T, Watanabe E, Shimizu M, Kamiya S, Nagata K et al (2006) Implications for induction of autoimmunity via activation of B-1 cells by Helicobacter pylori urease. Infect Immun 74:248–256
Lahner E, Virili C, Santaguida MG, Annibale B, Centanni M (2014) Helicobacter pylori infection and drugs malabsorption. World J Gastroenterol 20:10331–10337
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
This study was approved by the local Ethics Research Committee.
Informed consent
All participants signed a written consent.
Rights and permissions
About this article
Cite this article
Utiyama, S.R.R., De Bem, R.S., Skare, T.L. et al. Anti-parietal cell antibodies in patients with autoimmune thyroid diseases. J Endocrinol Invest 41, 523–529 (2018). https://doi.org/10.1007/s40618-017-0755-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-017-0755-2