Abstract
Introduction
Subclinical thyroid dysfunction is a possible risk factor for cognitive impairment in old age, but results are inconsistent. Aim of the present study was to evaluate the prevalence of thyroid dysfunction among older community-dwelling adults and to see whether thyroid function impacts the cognitive status of the elderly.
Methods
We included 1750 participants from the Study on Aging and Dementia in Mexico (SADEM). All subjects were evaluated clinically via specific interviews. TSH levels were analyzed by chemiluminescent immunometry assay. We classified participants into five thyroid state groups: (1) normal TSH levels (0.40–4.0 IU/L) were considered euthyroid; (2) Overt hyperthyroidism: TSH <0.3 IU/l and FT4 >23 pmol/l; (3) Overt hypothyroidism: TSH >4.8 IU/l, FT4 <13 pmol/l; (4) Subclinical hyperthyroidism: TSH <0.3 IU/l, FT4: 13–23 pmol/l; (5) Subclinical hypothyroidism: TSH >4.8 IU/l, FT4: 13–23 pmol/l.
Results
The overall estimated prevalence of thyroid dysfunction in Mexican population was 23.7% (95% CI, 22.66–26.77). Of these, 15.4% older adults were classified as subclinical hypothyroidism, 7.2% overt hypothyroidism, 0.5% subclinical hyperthyroidism, and 0.6% overt hyperthyroidism. The association of thyroid dysfunction with cognitive impairment was most evident in overt hypothyroidism OR = 1.261 (1.185–1.343).
Conclusions
The present study demonstrated a high prevalence of thyroid dysfunction in Mexican elderly people living in the community. A relationship between cognitive impairment and the presence of hypothyroidism was also shown, and to a lesser degree in hyperthyroidism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid disease is a common endocrine disorder whose prevalence of overt and subclinical hypothyroidism has been consistently reported, with frequencies ranging from 0.5 to 5% for overt hypothyroidism and from 5 to 20% for subclinical hypothyroidism [1–3]. However, only a limited number of studies have described thyroid disease in elderly patients and its impact on cognition. The thyroid, like other endocrine glands of the human body, has wide-ranging effects on nervous system, and overt thyroid dysfunctions are associated with several forms of cognitive impairment, peripheral neuropathies, and depressive or anxiety disorders [4]. Also, they act on muscular function, cardiovascular system [5], erythropoiesis, and oxidative stress [6], among other organic functions, as well as mobility [7], which is an important marker of independence for activities of daily living (ADLs) in old age.
The thyroid gland produces thyroid hormones thyroxine (T4) and triiodothyronine (T3) under the stimulation of pituitary secretion of thyrotrophin (TSH), and the diagnosis of hyperthyroidism is confirmed by demonstrating elevated free thyroxine (FT4) in conjunction with suppression of TSH via negative feedback to the pituitary. Conversely, hypothyroidism is characterized by reduced FT4 in the setting of elevated TSH. Subclinical hyperthyroidism is characterized by low TSH and normal free triiodothyronine (FT3) and free thyroid hormone (FT4) or thyroxine levels [8].
Primary hypothyroidism is the most prevalent thyroid dysfunction in elderly individuals, and subclinical hypothyroidism is found in almost 20% of the elderly population [9] (Biondi B 2008). Recent research has suggested that the upper reference value for serum TSH levels varies among age strata [10]. However, to date, there is no exact definition of these specific cut-offs, according to age, in our population [8].
A decline in cognitive function with aging may involve perception, memory, speech, judgment, and reasoning. Because thyroid hormone has profound effects on the central nervous system and modulates fetal and neonatal brain development, it affects cognition and may be important for optimal cognitive performance in adults [11]. Subclinical hyper- and hypothyroidism have been implicated as risk factors for cognitive impairment, risk for cardiovascular disease [12], and dementia [12–14], although the literature regarding these associations shows inconsistent results [15]. Some studies have reported a positive association [16–18], while others found no relationship between cognitive impairment and hypothyroidism [18, 19]. For these reasons, the association of clinical hypothyroidism with cognitive impairment is controversial and continues to be an issue for debate. Demographic change in aging populations is worldwide; this is a topical issue and likely to become an important area for future research, as dementia is a major health concern in older adults [20]. The aim of the present study was to evaluate the prevalence of thyroid dysfunction among older community-dwelling adults and to see whether thyroid function impacts the cognitive status of the elderly.
Materials and methods
Subjects
The population in this study came from the Study on Aging and Dementia in Mexico (SADEM study), held in 2009. This is a population-based study where men and women over 60 years of age who participated in the SADEM study were chosen at random from those insured by the Instituto Mexicano del Seguro Social (IMSS), residents of Mexico City. The SADEM study had a total of 3105 elderly; the objective of that study was to study the prevalence of dementia in Mexico City, and it has been described previously. Patients diagnosed with dementia were followed up to the present [21].
The participants in this cross-sectional study were selected at random from the 3105 older adults in the SADEM study, in order to estimate the prevalence of thyroid dysfunction and guarantee the extrapolation of the data to the elderly population in general, leading to a sample of 1750 elderly.
The exclusion criteria were as follows: being institutionalized, with brain tumor, iodine contrast use, unable to respond because of visual or severe hearing impairment, as well as presenting acute neurological diseases, and being unable to give informed consent. All criteria have been described previously [22].
In the present survey, we excluded subjects with a previous diagnosis of thyroid dysfunction and/or treated with drugs known to affect thyroid function. Patients affected by dementia were also excluded.
The research protocol was reviewed and approved by the National Commission of Scientific Research of the Mexican Institute of Social Security, as well as by the Institutional Ethics Committee (registration number R-2012-785-102). All participants agreed to be part of the study through a signed written informed consent.
Clinical evaluation
All included subjects were evaluated clinically via a specific interview. We collected information on age, education (years of schooling), marital status, and body mass index (measured weight/measured height2), cigarette smoking (current smoker), alcohol consumption (number of drinks/month). Comorbidity was evaluated using the Charlson Comorbidity Index. Waist circumference was measured at a level midway between the lower rib margin and iliac crest with the tape all around the body in horizontal position. Body weight was measured without shoes with a 0.1 kg precision. Systolic and diastolic blood pressures were measured using an automatic blood pressure monitor (Microfile BP A 100).
Body composition was assessed with a 353ioi JAWON body composition analyzer. Bioelectrical impedance was analyzed in the morning after a 12-h fast and adequate hydration, with the patient standing up and wearing light clothing, without shoes [23]. The analyzer measured weight with an accuracy of within 0.1 kg, as well as body impedance (in ohms), with calculation of the VAT value, percentage of total body fat (%BF).
The Mini-Mental State Examination (MMSE) [24] (Franco-Marina et al. 2010) was used to evaluate global cognitive function. The MMSE is a fully structured scale that consists of 30 points grouped into seven categories: orientation to place, orientation to time, registration, attention and concentration, language, and visual construction. In the Mexican population, 23/30 on the MMSE was found to be the optimal cut-off point to indicate cognitive impairment, with a sensitivity of 97% and specificity of 88% [25] The 1984 National Institute of Neurological and Communicative Disorders and the Alzheimer`s Disease and Related Disorders Association (NINCDS-ADRDA) recommended the MMSE as a screening test to detect cognitive impairment [26]. Nevertheless, care was taken due to the ceiling effect to which this test is subject [7].
Functional status was determined using the Katz basic activities of daily living (ADL) scale, where scores range from zero (all functions preserved) to six (all functions lost). This scale determines the level of personal independence in six activities: bathing, dressing, toileting, transferring from bed to chair, continence, and feeding [27]. The level of independence in executing tasks, such as using the telephone, shopping for personal items, preparing meals, doing light housework, and managing money or drugs, was assessed by the Instrumental ADL [28]. Scores range from zero (all functions preserved) to eight (all functions lost), and we used the SF-36 questionnaire used to evaluate the quality of life (QOL) of elderly. It measures the eight concepts of physical functioning, bodily pain, role limitations due to physical, personal, and emotional health problems, emotional well-being, social functioning, energy/fatigue, and general health perceptions. The total score is obtained by adding the items to create a score from zero to 100; higher scores indicate a better QOL. Scores of more than 117, 72–117, and less than 72 denote good, moderate, and negative QOL, respectively [29, 30].
Depressive symptoms. Depressive symptoms were assessed using the adapted Mexican version of the Center for Epidemiologic Studies Depression scale (CES-D 20-item version) [31, 32]. The final score ranged from zero to 60 points. Cut-off points for identifying depression were at >16 points.
Laboratory analysis
Blood samples were collected in the morning, after a fast equal to or greater than 10 h, and centrifuged at the clinical chemistry laboratory of the National Medical Center, IMSS. Glucose, total cholesterol, high-density lipoprotein cholesterol (HDL-chol), and triglyceride levels were determined in serum through the semiautomatic chemical analyzer Ekem Control Lab. Low-density lipoprotein cholesterol (LDL-chol) was calculated using the Friedewald formula.
TSH levels were analyzed by chemilluminescent immunometry assay, using IMMULITE by Diagnostic Products Corporation (Los Angeles, USA). The reference range was 0.4–4.0 mIU/L [33]. The limits of detection were 0.004 mIU/L for TSH, 0.28 ng/dL for free-T4 (FT4), and 1 pg/mL for free-T3 (FT3). TSH and FT4 levels were recoded based on the classification system for thyroid disorders, which includes clear definitions for subclinical thyroid disorders [34, 35]. Using this algorithm, we classified participants into five thyroid state groups: (1) participants with normal TSH levels (0.40–4.0 IU/L) were considered euthyroid; (2) Overt hyperthyroidism: TSH <0.3 IU/l and FT4 >23 pmol/l; (3) Overt hypothyroidism: TSH >4.8 IU/l, FT4 <13 pmol/l; (4) Subclinical hypothyroidism: TSH <0.3 IU/l, FT4: 13–23 pmol/l; and (5) Subclinical hyperthyroidism was defined as TSH >4.8 IU/l, FT4: 13–23 pmol/l.
Statistical analyses
Statistical analyses were performed using the Statistical Package for Social Sciences [36]. Means and standard deviation (SD) were calculated for continuous variables, and significance differences evaluated using one-way analysis of variance (ANOVA) in the four groups (Euthyroid, Overt hyperthyroidism, Overt hypothyroidism, Subclinical hypothyroidism, and Subclinical hyperthyroidism). Descriptive characteristics of categorical variables were summarized as frequencies, and comparisons among the groups performed using Chi square tests. Based on low to high serum TSH, all participants were divided into five groups, and logistic regression analyses performed using the fifth quintile as the reference. Logistic regression was used to evaluate the association of thyroid dysfunction with MCI (crude analysis and multivariate adjustment for age, sex and education). All calculated P values were unpaired and two-tailed, and differences were considered statistically significant at P < 0.05. Bonferroni correction was applied to adjust for multiple comparisons.
Results
Prevalence of thyroid dysfunction
Of the 1750 participants, 1276 (76.3%) had normal thyroid function, 256 (15.4%) had subclinical hypothyroidism, 121 (7.2%) had overt hypothyroidism, 9 (0.5%) had subclinical hyperthyroidism, and 10 (0.6%) had overt hyperthyroidism. Table 1 shows thyroid dysfunction prevalence. The prevalence was not affected by age or education. 78 participants were excluded for being under treatment for thyroid disorders. Subjects with hypothyroidism have a higher prevalence of metabolic syndrome as compared with subjects with hyperthyroidism.
Alteration in thyroid was associated with lower education (4.0 for overt hyperthyroidism vs 60.3 to euthyroidism; p = 0.026), BMI (24.8 subclinical hypertyriodism vs 25.8 euthyroidism; p < 0.000), percent body fat (PBF) (subclinical hypertyriodism 29.0 vs 31.9% euthyroidism; p < 0.000), visceral fat area (subclinical and overt hypertyriodism 107.1 vs 157.0 cm2 euthyroidism; p < 0.000), abdominal circumference (subclinical and overt hypertyriodism 80.1 vs 86.6 cm euthyroidism; p < 0.000), total cholesterol (subclinical hypertyriodism 168.2 vs 203.3 mg/dL euthyroidism; p < 0.000), LDL-chol (106.9 vs 116.7 mg/dL euthyroidism; p < 0.000), triglycerides (149.4 vs 166.6 mg/dL euthyroidism; p = 0.008), and albumin (4.3 vs 4.4 g/dL euthyroidism; p < 0.000) when compared to euthyroid participants. Glucose was higher in participants with subclinical hypothyroidism compared to those with euthyroidism (120.8 vs 113.9 mg/dL euthyroidism; p = 0.000).
Thyroid status and other geriatric assessment
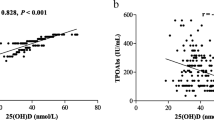
Table 2 shows associations of serum TSH levels with cognitive function test scores with MMSE. Based on serum TSH, all patients were divided into five groups. Compared with the fifth quintile, participants in the lowest and second lowest quintiles of TSH presented odds ratio (OR) for Cognitive Impairment of 2.50 [95% confidence interval (95% CI), 1.01–7.02] and 2.23 (95% CI, 1.05–6.35), respectively. All analyses were adjusted for age, sex, and years of education.
Thyroid dysfunction and cognitive impairment
The association of thyroid status and cognitive performance is presented in Table 3. There was a significant difference in MMSE between participants with hyperthyroidism and hypothyroidism when compared to participants with euthyroidism (all p < 0.05). Compared with the normal thyroid function group, we found significant association between MCI and thyroid dysfunction after adjusting the model for covariates of age, sex, and education years. In patients with hypothyroidism, the association was significant, while patients with hyperthyroidism did not reach statistical significance. (OR, 1.23, 95% CI, 1.28–5.69; OR, 1.23, 95% CI,) 1.39–5.42; OR, 1.23, 95% CI, 0.19–5.56; OR, 1.03, 95% CI, 0.69–8.69, respectively.
Discussion
The prevalence of thyroid disease in this study was similar to that reported in previous studies [2] (Robles-Osorio 2014). Given the known effects of thyroid hormone on brain function, it is reasonable to ask whether altered thyroid status is a risk factor for the cognitive impairment. The results of the present study showed the risk effect of thyroid dysfunction on cognitive performance in elderly people, reflecting a global decline related to aging. Similarly hypothyroidism and subclinical hypothyroidism were associated with cognitive dysfunction, but only the former was statistically significant [37]. This result set is contrary to that reported in other large studies which indicate that subjects with subclinical hypothyroidism do not have major cognitive impairments. However, the administered tests were often designed to screen large numbers of subjects and might not have detected subtle deficits. The association between subclinical hypothyroidism and cognitive impairment has not been completely clarified, especially in the elderly, where the assessment of neurological function is more challenging [38].
Some studies have assessed whether there are significant differences in cognitive function in elderly subjects affected by subclinical hypothyroidism. Cook et al. [39], studying 15 subjects of a mean age of 74 years, have noted that patients with subclinical hypothyroidism had significantly lower MMSE scores compared with euthyroid controls. In another report [40] in 425 subjects aged between 65 and 85 years, verbal fluency, an aspect of cognitive status, was found to be significantly impaired in subclinical hypothyroidism. Wijsman et al. [41], studying 161 participants, found no consistent association of subclinical hyper- or hypothyroidism with altered cognitive performance compared to euthyroid. The same thing was observed in a subsample of 62 participants aged 67 years and over at baseline from the NuAge study (Quebec longitudinal study). In conditional regression logistic models, there was no significant association between any thyroid function indices and the 3-year risk of cognitive impairment, as measured with the Modified Mini-Mental State [42]. The underlying causes of this discrepancy could be related to different exclusion criteria, age, or other confounding conditions.
However, other cross-sectional or longitudinal studies performed in this area are consistent with our results and observed an association between subclinical hypothyroidism and cognitive performance.
In a recent meta-analysis, a relationship was observed between subclinical hypothyroidism and cognitive impairment only in individuals younger than 75 years and those with higher TSH concentrations. No correlation was found when considering all the studies as a whole. Nonetheless, in this systematic review, none of the meta-analyzed studies used age-adjusted expected ranges, leading to the possible misclassification of older subjects as having subclinical hypothyroidism. Other limitations of this meta-analysis were dissimilar data collection and marked heterogeneity in the definition of hypothyroidism and cognitive scales [38].
Hogervorst et al. [16] reported that high log-transformed TSH levels were associated with lower MMSE performance, independent of FT4, age, sex, education, and mood. However, the analysis in that study focused on the level of TSH, in contrast to our study, where the objective was to evaluate cognitive state with the different categories of thyroid dysfunction. Although the concentration of TSH may be a reflection of the intracellular amount of thyroid hormones, it has been observed that the circulating level of these thyroid hormones is associated with oxidative stress and neuronal damage in elderly patients. Moreover, other studies in elderly participants have found that low thyroid hormone (T4, but not TSH level) predicted low baseline cognitive performance. In addition, the Hogervorst study included patients with known diagnosis of thyroid disease, in spite of which in the present study, it is noteworthy that the frequency of patients with hypothyroidism, both clinical and subclinical, was elevated.
The present study data were adjusted for age, sex, and education, and the MMSE scale has been previously reported [25]. Considering the high prevalence of subclinical hypothyroidism, additional studies using more specific methodologies to examine cognitive function in elderly patients with subclinical hypothyroidism are needed; also, knowing the practical repercussions of any such association is needed.
The results of our study indicate that in elderly people, cognitive impairment is evidently associated with overt hypothyroidism. Recent research has suggested that thyroid status varies among age strata. However, thyroid biology itself partly argues against the delineation of universal TSH cut-off points, since each individual appears to have a specific cut-point set by the hypothalamic–pituitary–thyroid axis [43]. To date, there is no exact definition of these specific cut-offs, according to age, in our population.
In this study, there was also a significant association between hyperthyroidism and cognitive impairment, although to a lesser degree. These results are consistent with previous studies reporting associations between hyperthyroidism and cognitive impairment [44]. Several plausible mechanisms for these associations have been suggested, including thyroid hormones inducing deposition of β-amyloid changes, and higher thyroid hormone levels have been found to be associated with a higher count of neocortical neuritic plaque and smaller hippocampal volume [44, 45].
Despite these limitations, our data suggest that even in relatively healthy elderly participants, thyroid dysfunction is associated with low cognitive function. Moreover, thyroid screening of cases with cognitive impairment may be important, as one prospective study found that levothyroxine prescribed to patients with hypothryoidism improved their affected memory performance significantly [25].
Strengths of the present study are that the sample was drawn from a community-dwelling population, and that important factors potentially affecting the thyroid function were considered. The well-known limitations of cross-sectional studies apply to the present study. Therefore, it is difficult to determine whether thyroid dysfunction was present before cognitive impairment. The major limitation to the study is that the chosen measures cover a broad range of cognitive domains. However, the MMSE is a screening test to detect gross impairment, as the authors point out. It is possible that subtle defects in specific cognitive domains may have been missed in this study. The valid counter-argument is that such subtle defects may not be clinically significant, at least in otherwise healthy elderly subjects. Further research is needed to elucidate causality and directions of these associations across the life course.
Conclusions
The present study demonstrates a high prevalence of thyroid dysfunction in adult population, as well as a relationship between cognitive impairment and the presence of hyperthyroidism and hypothyroidism. We have shown that overt hypothyroidism, whether clinical or subclinical, is associated with poorer cognitive performance in elderly people. Thyroid dysfunction and cognitive impairment are common problems in older individuals. The possible association of thyroid dysfunction with cognitive impairment is very important, because management of thyroid dysfunction is likely to have beneficial effects on mental health and quality of life. Better knowledge of this and other aspects in the elderly population is urgently needed. More thorough studies are needed to assess these findings and their impact on quality of life, hospitalization, and mortality in this specific population.
References
Grossman A, Weiss A, Koren-Morag N et al (2016) Subclinical thyroid disease and mortality in the elderly: a retrospective cohort study. Am J Med 129:423–430
Robles-Osorio ML, Zacarías-Rangel V, García-Solís P (2014) Prevalence of thyroid function test abnormalities and anti-thyroid antibodies in an open population in Central México. Rev Invest Clin 66:113–120
Canaris GJ, Manowitz NR, Mayor G et al (2000) The Colorado thyroid disease prevalence study. Arch Intern Med 160:526–534
Smith JW, Evans AT, Costall B et al (2002) Thyroid hormones, brain function and cognition: a brief review. Neurosci Biobehav. 26:45–60
Moura Neto A, Parisi MC, Tambascia MA et al (2013) Relationship of thyroid hormone levels and cardiovascular events in patients with type 2 diabetes. Endocr 45:84–91
Vitale G, Fatti LM, Prolo S, Girola A et al (2010) Screening for hypothyroidism in older hospitalized patients with anemia: a new insight into an old disease. J Am Geriatr Soc 58:1825–1827
Simonsick EM, Newman AB, Ferrucci L et al (2009) Subclinical hypothyroidism and functional mobility in older adults. Arch Intern Med 169:2011–2017
Cooper DS, Halpern R, Wood LC, Levin AA, Ridgway EC (1984) L-thyroxine therapy in subclinical hypothyroidism. A double-blind, placebo-controlled trial. Ann Intern Med 101:18–24
Biondi B, Cooper DS (2008) The clinical significance of subclinical thyroid dysfunction. Endocr Rev 29:76–131
Benseñor IM, Goulart AC, Lotufo PA et al (2011) Prevalence of thyroid disorders among older people: results from the Sao Paulo Ageing and Health Study. Cad Saude Publ 27:155–161
Di Liegro I (2008) Thyroid hormones and the central nervous system of mammals (Review). Mol Med Rep 1:279–295
Dorr M, Volzke H (2005) Cardiovascular morbidity and mortality in thyroid dysfunction. Min Endocrinol 30:199–216
Kalmijn S, Mehta KM, Pols HA et al (2000) Subclinical hyperthyroidism and the risk of dementia. The Rotterdam study. Clin Endocrinol (Oxf) 53:733–737
van Boxtel MP, Menheere PP, Bekers O et al (2004) Thyroid function, depressed mood, and cognitive performance in older individuals: the Maastricht Aging Study. Psychoneuroendocrinology 29:891–898
Parsaik AK, Singh B, Roberts RO et al (2014) Hypothyroidism and risk of mild cognitive impairment in elderly persons: a population-based study. JAMA Neurol 71:201–207
van Osch LA, Hogervorst E, Combrinck M et al (2004) Low thyroid-stimulating hormone as an independent risk factor for Alzheimer disease. Neurology 62:1967–1971
Roberts LM, Pattison H, Roalfe A et al (2006) Is subclinical thyroid dysfunction in the elderly associated with depression or cognitive dysfunction? Ann Int Med 145:573–581
Park YJ, Lee EJ, Lee YJ et al (2010) Subclinical hypothyroidism (SCH) is not associated with metabolic derangement, cognitive impairment, depression or poor quality of life (QoL) in elderly subjects. Arch Gerontol Geriatr 50:e68–e73
Kramer CK, von Muhlen D, Kritz-Silverstein D et al (2009) Treated hypothyroidism, cognitive function, and depressed mood in old age: the Rancho Bernardo Study. Eur J Endocrinol 161:917–921
Tan ZS, Vasan RS (2009) Thyroid function and Alzheimer’s disease. J Alzheimer’s Dis 16:503–507
Juarez-Cedillo T, Sanchez-Arenas R, Sanchez-Garcia S et al (2012) Prevalence of mild cognitive impairment and its subtypes in the Mexican population. Dement Geriatr Cogn Disord 34:271–281
Juárez-Cedillo T, Basurto-Acevedo L, Vega-García S et al (2014) Prevalence of anemia and its impact on the state of frailty in elderly people living in the community: SADEM study. Ann Hematol 93:2057–2062
Fernandez MJ, Basurto L, Córdova N et al (2014) Epicardial adipose tissue is associated with visceral fat, metabolic syndrome, and insulin resistance in menopausal women. Rev Esp Cardiol 67:436–441
Franco-Marina F, García-González JJ, Wagner-Echeagaray F et al (2010) The Mini-mental State Examination revisited: ceiling and floor effects after score adjustment for educational level in an aging Mexican population. Int Psychogeriatr 22:72–81
Reyes-Beaman S, Beaman PE, García-Peña C et al (2004) Validation of a modified version of the Minimental State Examination (MMSE) in Spanish. Aging Neuropsychol Cognit 11:1–11
McKhann G, Drachman D, Folstein M et al (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 34:939–944
Katz S, Akpom CA (1976) A measure of primary sociobiological functions. Int J Health 6:493–507
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Zúniga MA, Carrillo-Jiménez GT, Fos PJ (1999) Evaluation of health status using survey SF-36: preliminary results in Mexico. Salud Publica Mex 41:110–118
Brazier E, Harper R, Jones NMB et al (1992) Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 305:160–164
Eaton W, Muntaner C, Smith C (1998) Revision of the Center for epidemiologic studies depression (CES-D) Scale. John Hopkins University Prevention Center, Baltimore
Reyes M, Soto AL, Milla JG et al (2003) Actualización de la Escala de Depresión del Centro de Estudios Epidemiológicos (CES-D). Estudio piloto en una muestra geriátrica mexicana. Salud Ment 26:59–68
Garber JR, Cobin RH, Gharib H et al (2012) Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract 18:989–1028
Gussekloo J, van Exel E, de Craen AJ (2004) Thyroid status, disability and cognitive function, and survival in old age. JAMA 292:2591–2595
Medrano ME, Santillana-Hernández SP, Torres-Arreola LP et al (2012) Diagnóstico y tratamiento del hipotiroidismo primario en adultos. Rev Med Inst Mex Seguro Soc 50:71–80
SPSS Inc (2015) SPSS Base 23.0 for Windows User’s Guide. SPSS Inc., Chicago
Samuels MH (2010) Cognitive function in subclinical hypothyroidism. J Clin Endocrinol Meta 95:3611–3613
Pasqualetti G, Pagano G, Rengo G et al (2015) Subclinical hypothyroidism and cognitive impairment: a systematic review and meta-analysis. J Clin Endocrinol Metab 25:2046
Cook SE, Nebes RD, Halligan EM et al (2002) Memory impairment in elderly individuals with mildly elevated serum TSH: the role of processing resources, depression and cerebrovascular disease. Aging 9:175–183
Manciet G, Dartigues JF, Decamps A (1995) The PAQUID survey and correlates of subclinical hypothyroidism in elderly community residents in the southwest of France. Age Aging 24:235–241
Wijsman LW, de Craen AJ, Trompet S, Gussekloo J et al (2013) Subclinical thyroid dysfunction and cognitive decline in old age. PLoS One 8:e59199
Castellano CA, Laurin D, Langlois MF, Fortier M et al (2013) Thyroid function and cognition in the euthyroid elderly: a case-control study embedded in Quebec longitudinal study - NuAge. Psychoneuroendocrinology 38:1772–1776
Coene KL, Demir AY, Broeren MA et al (2015) Subclinical hypothyroidism: a “laboratory-induced” condition? Eur J Endocrinol 173:499–505
Ceresini G, Lauretani F, Maggio M (2009) Thyroid function abnormalities and cognitive impairment in elderly people: results of the Invecchiare in Chianti study. J Am Geriatr Soc 57:89–93
Kim JM, Stewart R, Kim SY et al (2010) Thyroid Stimulating Hormone, cognitive impairment and depression in an older Korean population. Psychiatry Investig 7:262–269
Acknowledgements
This study was supported by grants from SEP-CONACYT CB-2012-01-183700 (México). The original SADEM STUDY was supported by SSA/IMSS/ISSSTE-CONACYT (México) Salud-2007-01-69842 and the Fund for the Promotion of Health Research, Mexican Institute of Social Security, FIS/IMSS/PROT/G09/772.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors have no conflict of interest to declare. No competing financial interests exist. The funders had no role in analysis and interpretation of the data or in writing and publishing of the manuscript. There are no patents, and products in development to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Juárez-Cedillo, T., Basurto-Acevedo, L., Vega-García, S. et al. Prevalence of thyroid dysfunction and its impact on cognition in older mexican adults: (SADEM study). J Endocrinol Invest 40, 945–952 (2017). https://doi.org/10.1007/s40618-017-0654-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-017-0654-6