Abstract
Background
This study assessed the difference in 3-, 5-, and 10-year relative survival rates (RSRs) for female breast cancer between White and Black patients across the levels of year, tumor stage, age, and marital status at diagnosis. Confounding factors and effect modifiers were considered.
Methods
Analyses were based on 17 population-based tumor registries in the Surveillance, Epidemiology, and End Results (SEER) Program. Cases were diagnosed in 2000–2017 and followed through 2020.
Results
Three-, 5-, and 10-year female breast cancer RSRs significantly improved for White and Black patients during the years 2000–2020, more so for Blacks than Whites. Three-, 5-, and 10-year estimated annual percent changes in trends were 0.09%, 0.16%, and 0.29% for Whites and 0.36%, 0.49%, and 0.86% for Blacks, respectively. However, a large difference in RSRs for White and Black patients persists, 4.2% for three-year RSRs, 5.7% for five-year RSRs, and 7.5% for 10-year RSRs, after adjusting for year, tumor stage, age, and marital status at diagnosis. The difference in RSRs between White and Black patients differs by tumor stage at diagnosis. For example, higher five-year RSRs in Whites than Blacks were 2.6% for local, 9.3% for regional, 10.4% for distant, and 6.2% for unknown/unstaged tumors at diagnosis.
Conclusion
Improvement in 3-, 5-, and 10-year female breast cancer RSRs occurred for both White and Black patients, albeit more so for Blacks. Yet the poorer RSRs for Blacks remain large and significant, increasingly so with later staged disease at diagnosis and as we move from 3- to 5- to 10-year RSRs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Poorer female breast cancer survival rates in Black women compared with White women in the United States have been tracked for decades [1,2,3,4]. These poorer rates in Black women may be because they are more likely affected by aggressive subtypes of breast cancer (i.e., triple-negative breast cancer and inflammatory breast cancer, both of which are harder to treat); less likely to undergo mammography screening because of factors like differences in access to care, education, and health literacy; and more likely to dismiss or ignore cancer symptoms, or view cancer as a taboo subject [5,6,7]. In addition, data have shown that female breast cancer survival rates are significantly influenced by calendar year, tumor stage, age, and marital status at diagnosis [8,9,10].
The relative survival rate (RSR) is a measure that removes competing causes of death. Five-year RSRs have remained consistently lower for Black compared with White women during 2010 through 2020 [11]. However, it is not clear whether this difference varies across the levels of years, tumor stage, age, or marital status at diagnosis. It is important to consider differences in RSRs between White and Black women that are adjusted for potential confounding effects of year, tumor stage, age, and marital status at diagnosis to provide a more complete perspective on the state of breast cancer inequality between racial/ethnic groups. In addition, differences in RSRs may vary between 3-, 5-, or 10-years of survival.
The current study assessed breast cancer incidence data according to year, tumor stage, age, and marital status, which may provide new insights into differential screening between White and Black women and indicate the need for variable adjustment in our assessment of race differences in RSRs. The primary purpose of the study was to provide a unique assessment of differences in 3-, 5-, and 10-year RSRs between White and Black female breast cancer patients across the levels of year, tumor stage, age, and marital status at diagnosis. In addition, differences in RSRs between White and Black women were adjusted for potential confounders and effect modifiers. Consideration of these potential confounders and effect modifiers on 3-, 5-, and 10-year RSRs can provide meaningful clinical insights that have not been addressed in previous studies.
Materials and Methods
Study Population
We assessed retrospective cohort data on breast cancer patients diagnosed in 17 population-based tumor registries in the Surveillance, Epidemiology, and End Results (SEER) Program of the United States National Cancer Institute [12]. The SEER Program provides a comprehensive system for tracking cancer incidence and survival in the United States. It collects and reports information on tumor characteristics (e.g., stage and grade at diagnosis), patient characteristics (e.g., age and race), and first course of cancer-directed therapy [13]. Cancer characteristics and treatment information are abstracted from the records of hospitals, clinical and nursing homes, private pathology laboratories, radiotherapy units, and from death certificates.
The SEER registries include San-Francisco-Oakland, Connecticut, Detroit (metropolitan), Hawaii, Iowa, New Mexico, Seattle (Puget Sound), Utah, Atlanta (metropolitan), San Jose-Monterey, Los Angeles, Rural Georgia, California (excluding the three other California areas listed), Kentucky, Louisiana, New Jersey, and Rural Georgia. The SEER program began on January 1, 1973, with five states and two metropolitan areas participating. Since then, it has expanded to include additional registries, as described elsewhere [14]. This program is the gold standard of cancer data quality, with almost complete case identification and regular quality control measures [15, 16].
Breast cancer incidence, prevalence, and survival is determined in the SEER Program by the International Classification of Diseases for Oncology, 3rd Edition (ICD-O-3), code C50.0-C50.9 [17, 18].
Data
There were 920,467 (819,188 White and 101,279 Black) cases of malignant breast cancer with known age diagnosed during 2000–2017. Exclusions were made in the survival analysis for all cases known by death certificate only, autopsy only, and for patients still alive with no survival time, leaving 749,676, for inclusion in the survival analysis. Of these 665,097 represented White patients and 84,579 represented Black patients. Cases were followed up through 2020.
The SEER program uses national life tables to estimate expected mortality for individuals in a study population when calculating RSRs for cancer patients. National life tables were calculated using population estimates from the U.S. Census Bureau and birth and death records from the National Center for Health Statistics, National Vital Statistics System. We also derived female breast cancer incidence rates in this paper. Annual mid-year population estimates for the denominators of the estimated breast cancer incidence rates were obtained from the U.S. Census Bureau.
Statistical Techniques
Numbers, percentages, incidence rates (age-adjusted to the 2000 U.S. standard population), and RSRs described the data. The chi-square test of independence was used to assess whether distributions of incident cases of breast cancer significantly differed between White and Black patients. Relative survival is a net survival measure of cancer survival in the absence of other causes of death. It is defined as the ratio of the proportion of observed survivors in a cohort of cancer patients to the proportion of expected survivors in a comparable set of people without cancer [19]. Three-, 5-, and 10-year RSRs were derived. RSRs and corresponding 95% confidence intervals were generated in SEER*Stat 8.4.2 [12]. Non-overlapping 95% confidence intervals for the relative survival rate estimates denoted statistical significance. Multiple regression with RSRs regressed on race and year, tumor stage, age, and marital status at diagnosis, were weighted by the number in each race, stage, age, marital status, and year classification. Interaction terms involving race were assessed. Statistical significance was based on two-sided hypothesis tests, at the 0.05 level of significance. Statistical analyses were derived from Statistical Analysis System (SAS) software, version 9.4 (SAS Institute Inc., Cary, NC, USA, 2012).
Results
The estimated annual percent change in age-adjusted female malignant breast cancer incidence rates from 2000 through 2017 was -0.2% (t p = 0.0913) for Whites and 0.5% (t p = 0.0002) for Blacks. In general, the age-adjusted incidence rates are approximately 4% higher for White women than for Black women, with the difference falling from 10% in 2000–2005 to 1% in 2012–2017 (Table 1). The higher rates in White women are reflected in cases diagnosed with localized staged disease and in older age groups. Age-adjusted rates in White women (vs. Black women) are 11% lower for regional cases, 36% lower for distant cases, and 17% lower for ages < 40 years. White women are significantly more likely than Black women to be married and less likely to have never been married.
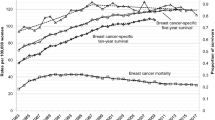
Three-, 5-, and 10-year malignant female breast cancer RSRs are shown for White and Black women in Fig. 1. The rates consistently significantly improved with later calendar year at diagnosis, more so for Black women. For 3-year RSRs the estimated annual percent increase in trend is 0.09 for White women and 0.36 for Black women; for 5-year RSRs the estimated annual percent increase in trend is 0.16 for White women and 0.49 for Black women; and for 10-year RSRs the estimated annual percent increase in trend is 0.29 for White women and 0.86 for Black women. Thus, improvement in RSRs appears for both White and Black women, though it is more pronounced in Black women. The RSRs remain significantly better for White women, especially for 10-year survival versus 5-year survival and 5-year survival versus 3-year survival. Improvements in survival for both White and Black women increase with more years of survival (i.e., 10- vs. 5- vs. 3-year RSRs).
Five years after diagnosis the average female breast cancer patient was 9.1% less likely to survive than a White woman without breast cancer (Table 2). The corresponding value for Black women is 19.1%. Five-year RSRs for breast cancer are consistently significantly greater for White women than Black women across the levels of each variable. The difference in rates is less pronounced for those diagnosed in more recent years. In addition, the higher five-year RSRs in White versus Black women are greatest in those diagnosed with regional or distant disease, in the younger and older age groups, and in those who are not married.
Multiple regression models estimating female breast cancer RSRs according to race and year, tumor stage, age, and marital status at diagnosis through 3, 5, and 10 years appear in Table 3. Each variable significantly contributes to variation in breast cancer RSRs except age, which is not significant in the first model. White women experience higher RSRs than Black women in each of the adjusted models. Better RSRs are also seen in those with local tumor stage, in the age group 40–79 years, and married at diagnosis. The estimated differences tend to become more extreme as we move from 3-, to 5-, to 10-year RSRs. For example, 3-, 5-, and 10-year breast cancer RSRs for White women are 4.2%, 5.7%, and 7.5% greater than for Black women, respectively.
Interaction terms were assessed in each of the models between race and year, tumor stage, age, and marital status at diagnosis. Race by tumor stage was the only interaction found to be significant. Interaction terms involving stage at diagnosis and each of the other variables in the models were also significant. Hence, the models were each reassessed according to tumor stage at diagnosis. The results for 5-year RSRs by tumor stage at diagnosis are shown in Table 4.
Higher female breast cancer RSRs in White women compared with Black women are increasingly pronounced with higher stage, after adjusting for year, age, and marital status at diagnosis. For local staged cases RSRs are significantly lower for those aged < 40 years at diagnosis, and for regional staged cases RSRs are significantly lower in those aged < 40 and 80 +. On the other hand, the RSRs for distant staged cases significantly fell with older age. The benefit of marriage on RSRs is significant in each stage category, but more so in later staged cases.
Discussion
This study assessed the difference in 3-, 5-, and 10-year RSRs for female breast cancer between Whites and Blacks across the levels of year, tumor stage, age, and marital status at diagnosis. Differences in RSRs were adjusted for potential confounders. In addition, effect modifiers of the differences in RSRs were evaluated.
The distribution of breast cancer cases across calendar years indicated a greater proportion of White women compared with Black women were diagnosed with breast cancer in earlier years, but the converse is true in later years. This may reflect a concerted effort to improve breast cancer screening among Black women; that is, increased breast cancer screening can result in more cases being identified [20]. Literature in recent years reflects this increased effort to improve screening among Black women through greater awareness of the barriers for screening among Black women (e.g., inadequate health insurance or access to health care facilities) and higher levels of recommended mammography screening by primary care clinicians [7, 21,22,23]. A report from the American Cancer Society shows that since 2008 the prevalence of mammography screening has been similar or higher for Black than White women [24]. In 2021, the report showed that the prevalence of mammography screening in the past two years in ages ≥ 45 years is 69% for non-Hispanic (NH) Black women and 65% for NH White women. Corresponding estimates for ages 50–74 years are 82% and 76%, respectively. In general, better screening practices have proven beneficial in decreasing mortality in breast cancer patients [25].
Despite an improved effort to screen Black women for breast cancer, White women were more likely to be diagnosed with early staged disease, suggesting more aggressive screening overall in White women than Black women. A previous study examined an HMO that screened for breast cancer at no-cost to the patient [26]. Although screenings were more frequently recommended to Black women, White women were more likely to undergo mammogram screening. Compared with Black women, White women were also more likely diagnosed at an older age, which is consistent with their having an older age distribution in general in the United States [27].
Most White women included in this study were married, while most Black women were single. This is consistent with research showing that Black women tend to marry later in life or are less likely to get married at all in comparison to their White counterparts [28, 29].
Trends in 3-, 5-, and 10-year RSRs improved for both White and Black women over the study period, more so for Black women. This is consistent with national data showing that breast cancer mortality rates for Black women have consistently fallen since the mid-1990s and for White women since the early-1990s [30]. Similar improvements have been found internationally, attributed to earlier cancer detection and personalized treatment plans [31].
Although RSRs improved for both White and Black women (albeit more so for Black women), the difference in RSRs remains large and statistically significant in the adjusted models, increasingly so as we move from 3- to 5- to 10-year RSRs. Nevertheless, increasing improvement of longer-term survival is seen for both White and Black women. The greater improvement in longer-term survival is consistent with advances in screening and treatment for breast cancer. The greater improvement in survival for Black women compared with White women may be related to more concerted screening and treatment efforts in these women.
Five-year RSRs for breast cancer are consistently significantly greater for White women compared with Black women across the levels of stage, age, and marital status, more so for regional or distant disease, in the younger and older age groups, and in singles. Greater screening and treatment efforts are needed for Black women across all levels of stage, age, and marital status, especially in later stages, young and old ages, and among singles.
Research shows that Black women have poorer breast cancer mortality than other racial groups at younger ages, and, thus, it is recommended that they should start screening 8 years earlier than White women (i.e., at age 42 rather than 50) [32]. In addition, studies show that Black women are less likely than White women with breast cancer to receive minimum expected therapy [33] and are more likely to delay treatment [34, 35]. Higher treatment delay for Black versus White women with breast cancer has been seen across all levels of socioeconomic status [35]. In a 2018 study looking at women aged 18–64 diagnosed with early staged breast cancer, four key factors accounted for 76.3% of total excess death risk in Black women: 37% private health insurance, 23.2% tumor characteristics, 11.3% comorbidities, and 4.8% treatment [36]. Treatment differences related to when they started or stopped and what they received. Poorer treatment patterns among Black women compared with White women may be the result of their having more comorbid disease (like diabetes, heart disease, and obesity), lower income, employment, and private health insurance that limits access to healthcare; lower education, health literacy, and recognition of the importance responding to cancer symptoms; and lower marriage rates [7, 28, 34].
Our finding that being married is associated with significantly better breast cancer RSRs for both White and Black women is consistent with another study [37]. Research has shown that married patients receive more mental and financial support, are diagnosed with earlier staged disease, get more appropriate treatment, and ultimately have better survival [38,39,40]. The benefit of marriage may be even more pronounced for Black women, possibly because marital status is more likely associated with screening and treatment resources for Black than White women.
Differences in breast cancer RSRs between Black and White women continue after adjustment for tumor stage, age, and marital status at diagnosis. Further, the estimated differences increase as we move from 3-, to 5-, to 10-year RSRs. This is consistent with Black women being more likely than White women to receive minimum expected therapy [33] or delay treatment [34, 35], which is explained by the factors already mentioned [7, 28, 34]. The effect of older age on lower breast cancer RSRs does not become significant until 5- and 10-years of follow-up.
The difference in breast cancer RSRs between White and Black women differs by tumor stage at diagnosis. For example, higher 5-year RSRs in White women compared with Black women are 2.6% for local, 9.3% for regional, 10.4% for distant, and 6.2% for unknown/unstaged tumors at diagnosis. It may be that Blacks who aggressively pursue mammography screening are more likely to be diagnosed at an earlier stage and less likely to delay receiving adequate treatment. Research suggests that more educated women are screen detected for breast cancer at an earlier stage and that higher education is also related to receiving appropriate treatment [41, 42].
Tumor stage at diagnosis also interacted with year, age, and marital status at diagnosis. RSRs improved with later years at diagnosis for local, regional, and distant stages. The improvement was more pronounced in later stages. These findings are consistent with previous research [43], with improvements being made in treating later stage breast cancer.
For local staged disease at diagnosis, the RSRs were significantly lower in those aged < 40 years, and for regional staged disease at diagnosis RSRs were significantly lower in those aged < 40 and 80 + . This may suggest that breast cancer at a younger age tends to be more biologically aggressive [44]. Further research needs to be conducted to better understand localized breast cancer in women aged < 40. Similarly, those who are aged < 40 and receive a regional stage diagnosis may have a more aggressive tumor biology and require further study. Those aged ≥ 80 are less likely to have their breast cancer screen detected. This makes the cancer first detectable when it is at a later stage. Moreover, elderly patients are often given alternative treatment plans based on personal choice and what their body can undergo given their age, leading to a less-favorable prognosis [45].
RSRs for distant staged cases consistently significantly fell with older age. At older ages there are fewer clinical options due to potential comorbid conditions (e.g., arthritis, hypertension, heart disease, diabetes, and osteoporosis) that are more likely to exist and decrease 5-year RSRs [46, 47]. Moreover, the literature suggests that older patients may face complications because clinical trials in younger populations are unable to be extrapolated and applied to older patients because of differences in breast cancer tumor pathology by age. Older aged patients may also be more likely to opt for palliative care as opposed to a more aggressive treatment approach relative to younger populations [48]. Limited treatment options, comorbid health problems, and increased likelihood of electing for palliative-care would all lead to lower RSRs in older ages.
Black women were significantly less likely to be married or ever married. This is consistent with other research showing that Black women compared with White women are more likely to marry later in life, are less likely to ever marry, and have higher rates of marital instability [29]. The benefit of marriage on RSRs was significant in each stage category, but more so in later staged cases. Research shows that social structures such as marriage or having a cohabitating partner can help reduce the risk of depression in breast cancer patients [49]. Moreover, those that have depression experience worse outcomes while undergoing cancer treatments such as chemotherapy, which is the more common treatment used in later staged breast cancer [49]. Therefore, those who are married or have a cohabitating partner may be less likely to experience depression, which is a condition that may compromise the efficacy of treatments used in later staged breast cancer.
The 17 tumor registries used for the current analysis represents 26.5% of the total U.S. population (22.4% for Whites and 23.1% for Blacks). Although the registries were selected to be representative of the U.S. population and represent high quality population-based data [50], there may be some limitations in external validity (generalizability). Further, assessing RSRs for some combinations of year, tumor stage, age, and marital status at diagnosis involved small numbers and unstable estimates. Marital status was available at the time of diagnosis only. Marital status after diagnosis was not tracked. We assume there was little change with years of follow-up. In addition, about 5% of White and Black women had unknown marital status at the time of diagnosis. Unknown stage or unstaged disease involved about 3% of Whites and 4% of Blacks. The database did not include information on all potential confounders of the relationships considered in this study, such as lifestyle and environmental factors. The study’s conclusions are limited to associations and do not imply any casual relationships.
Conclusion
The current study shows that 3-, 5-, and 10-year female breast cancer RSRs for White and Black women significantly improved during the years 2000–2020, more so for Black women than for White women. This suggests more concerted efforts for screening and treating breast cancer in Black women in recent years. However, a large difference in RSRs persists between White and Black patients, with the difference increasing with time from diagnosis. The relationship between race and RSRs is also impacted by tumor stage at diagnosis, with Black women having increasingly poorer prognosis compared with White women with later staged disease. Further research may explore other potential confounders and effect modifiers.
The relationship between race and RSRs also depends on marital status; the difference in RSRs is less pronounced between White and Black women who are married at the time of diagnosis. Understanding the effect of marital status on the relationship between race and RSRs requires further study.
Both White and Black women under the age of 40 with a malignant breast cancer diagnosis have lower RSRs than older women with the same diagnosis. One reason suggested in the literature for this is infrequent screening in this younger population.
Data Availability
The data were obtained from the National Cancer Institute’s SEER Program, which is freely accessed through the public domain.
References
Yedjou CG, Sims JN, Miele L, et al. Health and racial disparity in breast cancer. Adv Exp Med Biol. 2019;1152:31–49. https://doi.org/10.1007/978-3-030-20301-6_3.
Giaquinto AN, Miller KD, Tossas KY, Winn RA, Jemal A, Siegel RL. Cancer statistics for African American/Black people 2022. CA Cancer J Clin. 2022;72(3):202–29. https://doi.org/10.3322/caac.21718.
Baquet CR, Mishra SI, Commiskey P, Ellison GL, DeShields M. Breast cancer epidemiology in blacks and Whites: Disparities in incidence, mortality, survival rates and histology. J Natl Med Assoc. 2008;100(5):480–8. https://doi.org/10.1016/s0027-9684(15)31294-3.
Abraham HG, Xia Y, Mukherjee B, Merajver SD. Incidence and survival of inflammatory breast cancer between 1973 and 2015 in the SEER database. Breast Cancer Res Treat. 2021;185(1):229–38. https://doi.org/10.1007/s10549-020-05938-2.
George P, Chandwani S, Gabel M, et al. Diagnosis and surgical delays in African American and white women with early-stage breast cancer. J Womens Health (Larchmt). 2015;24(3):209–17. https://doi.org/10.1089/jwh.2014.4773.
Mayo Clinic Comprehensive Cancer Center Blog. What black women need to know about breast cancer. https://cancerblog.mayoclinic.org/2022/02/24/what-black-women-need-to-know-about-breast-cancer/#:~:text=But%20the%20longer%20cancer%20goes,would%20be%20a%20big%20advance.%22. Accessed 19 July 2024
Breast Cancer Research Foundation. Black women and breast cancer: why disparities persist and how to end them. https://www.bcrf.org/blog/black-women-and-breast-cancer-why-disparities-persist-and-how-end-them/#:~:text=Through%20continued%20research%2C%20it's%20clear,advanced%20stages%20of%20the%20disease. Accessed 19 June 2024
Fontein DB, de Glas NA, Duijm M, et al. Age and the effect of physical activity on breast cancer survival: A systematic review. Cancer Treat Rev. 2013;39(8):958–65. https://doi.org/10.1016/j.ctrv.2013.03.008.
Li X, Yang J, Peng L, et al. Triple-negative breast cancer has worse overall survival and cause-specific survival than non-triple-negative breast cancer. Breast Cancer Res Treat. 2017;161(2):279–87. https://doi.org/10.1007/s10549-016-4059-6.
Adekolujo OS, Tadisina S, Koduru U, Gernand J, Smith SJ, Kakarala RR. Impact of marital status on tumor stage at diagnosis and on survival in male breast cancer. Am J Mens Health. 2017;11(4):1190–9. https://doi.org/10.1177/1557988316669044.
SEER*Explorer: An interactive website for SEER cancer statistics [Internet]. Surveillance Research Program, National Cancer Institute; 2023 Apr 19. [updated: 2023 Nov 16; cited 2024 Jan 23]. Available from: https://seer.cancer.gov/statistics-network/explorer/. Data source(s): SEER Incidence Data, November 2022 Submission (1975–2020), SEER 22 registries (excluding Illinois and Massachusetts). Expected Survival Life Tables by Socio-Economic Standards.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER Research Data, 17 Registries, Nov 2022 Sub (2000–2020) - Linked To County Attributes - Time Dependent (1990–2021) Income/Rurality, 1969–2021 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2023, based on the November 2022 submission.
Hankey BF, Ries LA, Edwards BK. The surveillance, epidemiology, and end results program: a national resource. Cancer Epidemiol Biomarkers Prev. 1999;8(12):1117–21.
National Cancer Institute. About the Seer Registries. https://seer.cancer.gov/registries/. Accessed 18 Dec 2023.
National Cancer Institute. Quality Improvement. https://seer.cancer.gov/about/uses.html. Accessed 18 Dec 2023.
Zippin C, Lum D, Hankey BF. Completeness of hospital cancer case reporting from the SEER Program of the National Cancer Institute. Cancer. 1995;76(11):2343–50 https://doi.org/10.1002/1097-0142(19951201)76:11<2343::AID-CNCR2820761124>3.0.CO;2-%23.
Fritz A, Percy C, Jack A, et al. International classification of diseases for oncology, 3rd ed. World Health Organization; 2000. https://iris.who.int/handle/10665/42344.
Adamo MB, Johnson CH, Ruhl JL, Dickie LA. SEER Program Coding and Staging Manual 2012. National Cancer Institute; 2012. NIH Publication number 12–5581. https://seer.cancer.gov/archive/manuals/2012/SPCSM_2012_maindoc.pdf.
Mariotto AB, Noone AM, Howlader N, et al. Cancer survival: an overview of measures, uses, and interpretation [published correction appears. J Natl Cancer Inst Monogr. 2014;2014(49):145–86. https://doi.org/10.1093/jncimonographs/lgu024.
Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367(21):1998–2005. https://doi.org/10.1056/NEJMoa1206809.
Mitchell EP. Cancer in African Americans: Screening can make a difference. J Natl Med Assoc. 2021;113(4):365. https://doi.org/10.1016/j.jnma.2021.07.001.
Aleshire ME, Adegboyega A, Escontrías OA, Edward J, Hatcher J. Access to care as a barrier to mammography for Black women. Policy Polit Nurs Pract. 2021;22(1):28–40. https://doi.org/10.1177/1527154420965537.
Oppong BA, Obeng-Gyasi S, Relation T, Adams-Campbell L. Call to action: breast cancer screening recommendations for Black women. Breast Cancer Res Treat. 2021;187(1):295–7. https://doi.org/10.1007/s10549-021-06207-6.
American Cancer Society. Cancer Prevention & Early Detection Facts & Figures 2023–2024.
Coleman C. Early detection and screening for breast cancer. Semin Oncol Nurs. 2017;33(2):141–55. https://doi.org/10.1016/j.soncn.2017.02.009.
Reisch LM, Barton MB, Fletcher SW, Kreuter W, Elmore JG. Breast cancer screening use by African Americans and Whites in an HMO. J Gen Intern Med. 2000;15(4):229–34. https://doi.org/10.1111/j.1525-1497.2000.01339.x.
GBD Us Health Disparities Collaborators. Life expectancy by county, race, and ethnicity in the USA, 2000–19: a systematic analysis of health disparities. Lancet. 2022;400(10345):25–38. https://doi.org/10.1016/S0140-6736(22)00876-5.
Zubizarreta D, Beccia AL, Chen JT, Jahn JL, Austin SB, Agénor M. Structural racism-related state laws and healthcare access among Black, Latine, and White U.S. adults. J Racial Ethn Health Disparities. 2024. https://doi.org/10.1007/s40615-024-01976-4.
Raley RK, Sweeney MM, Wondra D. The growing racial and ethnic divide in U.S. marriage patterns. Future Child. 2015;25(2):89–109. https://doi.org/10.1353/foc.2015.0014.
Giaquinto AN, Sung H, Miller KD, et al. Breast Cancer Statistics, 2022. CA Cancer J Clin. 2022;72(6):524–41. https://doi.org/10.3322/caac.21754.
Nardin S, Mora E, Varughese FM, et al. Breast cancer survivorship, quality of life, and late toxicities. Front Oncol. 2020;10:864. https://doi.org/10.3389/fonc.2020.00864. Published 2020 Jun 16.
Chen T, Kharazmi E, Fallah M. Race and ethnicity-adjusted age recommendation for initiating breast cancer screening. JAMA Netw Open. 2023;6(4):e238893. https://doi.org/10.1001/jamanetworkopen.2023.8893.
Breen N, Wesley MN, Merrill RM, Johnson K. The relationship of socio-economic status and access to minimum expected therapy among female breast cancer patients in the National Cancer Institute Black-White Cancer Survival Study. Ethn Dis. 1999;9(1):111–25.
Reeder-Hayes KE, Mayer SE, Olshan AF, et al. Race and delays in breast cancer treatment across the care continuum in the Carolina Breast Cancer Study. Cancer. 2019;125(22):3985–92. https://doi.org/10.1002/cncr.32378.
Emerson MA, Golightly YM, Aiello AE, et al. Breast cancer treatment delays by socioeconomic and health care access latent classes in Black and White women. Cancer. 2020;126(22):4957–66. https://doi.org/10.1002/cncr.33121.
Jemal A, Robbins AS, Lin CC, et al. Factors that contributed to Black-White disparities in survival among nonelderly women with breast cancer between 2004 and 2013. J Clin Oncol. 2018;36(1):14–24. https://doi.org/10.1200/JCO.2017.73.7932.
Ding W, Ruan G, Lin Y, Zhu J, Tu C, Li Z. Dynamic changes in marital status and survival in women with breast cancer: a population-based study. Sci Rep. 2021;11(1):5421. https://doi.org/10.1038/s41598-021-84996-y.
Chang SM, Barker FG II. Marital status, treatment, and survival in patients with glioblastoma multiforme: a population-based study. Cancer. 2005;104:1975–84. https://doi.org/10.1002/cncr.21399.
Cohen SD, et al. Social support and chronic kidney disease: An update. Adv Chronic Kidney Dis. 2007;14:335–44. https://doi.org/10.1053/j.ackd.2007.04.007.
Liu Y, Zhang J, Huang R, Feng WL, Kong YN, Xu F, Zhao L, Song QK, Li J, Zhang BN, Fan JH, Qiao YL, Xie XM, Zheng S, He JJ, Wang K. Influence of occupation and education level on breast cancer stage at diagnosis, and treatment options in China: A nationwide, multicenter 10-year epidemiological study. Medicine (Baltimore). 2017;96(15):e6641. https://doi.org/10.1097/MD.0000000000006641.
Chung HW, Noh SH, Lim JB. Analysis of demographic characteristics in 3242 young age gastric cancer patients in Korea. World J Gastroenterol. 2010;16:256–63.
Baade PD, Aitken JF, Ferguson M, et al. Diagnostic and treatment pathways for men with prostate cancer in Queensland: investigating spatial and demographic inequalities. BMC Cancer. 2010;10:452.
Guo F, Kuo YF, Shih YCT, Giordano SH, Berenson AB. Trends in breast cancer mortality by stage at diagnosis among young women in the United States. Cancer. 2018;124(17):3500–9. https://doi.org/10.1002/cncr.31638.
Tesch ME, Partridge AH. Treatment of breast cancer in young adults. Am Soc Clin Oncol Educ Book. 2022;42:1–12. https://doi.org/10.1200/EDBK_360970.
Crivellari D, Aapro M, Leonard R, et al. Breast cancer in the elderly. J Clin Oncol. 2007;25(14):1882–90. https://doi.org/10.1200/JCO.2006.10.2079.
Chagpar AB. Distant metastasis in elderly patients with breast cancer: Prognosis with Nodal Status. In: Hayat MA, editor. Methods of cancer diagnosis, therapy and prognosis. Methods of cancer diagnosis, therapy and prognosis, vol. 1. Dordrecht: Springer,; 2008. https://doi.org/10.1007/978-1-4020-8369-3_42.
Crivellari D, Spazzapan S, Puglisi F, Fratino L, Scalone S, Veronesi A. Hormone therapy in elderly breast cancer patients with comorbidities. Crit Rev Oncol Hematol. 2010;73(1):92–8. https://doi.org/10.1016/j.critrevonc.2009.02.003.
Rubens M, Ramamoorthy V, Saxena A, et al. Palliative care consultation trends among hospitalized patients with advanced cancer in the United States, 2005 to 2014. Am J Hosp Palliat Care. 2019;36(4):294–301. https://doi.org/10.1177/1049909118809975.
Zamanian H, Amini-Tehrani M, Jalali Z, et al. Perceived social support, coping strategies, anxiety and depression among women with breast cancer: Evaluation of a mediation model. Eur J Oncol Nurs. 2021;50:101892. https://doi.org/10.1016/j.ejon.2020.101892.
Merrill RM, Dearden KA. How representative are the surveillance, epidemiology, and end results (SEER) program cancer data of the United States. Cancer Cause Control. 2004;15:1027–34.
Funding
No funding was used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
This study did not require ethical review because it is based on data that are freely available in the public domain and the data are properly anonymized and informed consent was obtained at the time of original data collection.
Disclosure
The study was performed as part of the employment of the principal investigator at Brigham Young University. The institution did not provide funding and was not involved with drafting the manuscript or making the decision to publish.
Conflicts of Interest
The authors declare that they have no conflicting/competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Merrill, R.M., Gibbons, I.S. Inequality in Female Breast Cancer Relative Survival Rates between White and Black Women in the United States. J. Racial and Ethnic Health Disparities (2024). https://doi.org/10.1007/s40615-024-02079-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-024-02079-w