Abstract
Black individuals have been disproportionately affected by the COVID-19 pandemic, likely due in part to historically rooted stressors that lie at the intersection of the COVID-19 pandemic and racism. We used secondary data from The Association of Black Psychologists’ multi-state needs assessment of 2480 Black adults to examine the link between race-related COVID stress (RRCS) and mental health outcomes. We also examined the moderating roles of everyday discrimination, cultural mistrust, Black activism, Black identity, and spirituality/religiosity in these associations. T-tests revealed that several demographic and cultural factors are associated with RRCS endorsement. A series of regression analyses showed that endorsement of RRCS is associated with higher psychological distress and lower well-being, above and beyond several sociodemographic characteristics. While traditional cultural protective factors did not buffer against the effects of RRCS on mental health, cultural mistrust strengthened the positive association between RRCS and psychological distress; nonetheless, the association of cultural mistrusts with psychological distress was only seen in those who endorsed RRCS. We provide recommendations for policymakers, clinicians, and researchers to consider the impact of RRCS when addressing Black mental health and well-being in the age of COVID-19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
It is well-known that Black individuals in the USA have disproportionately suffered from the COVID-19 pandemic due to higher risk, mortality, and inequitable treatment [1]. Emerging research suggests that the disparate health impact is not only physical, but mental as well. Kujawa et al. found that Black people have significantly higher pandemic-related stress than any other demographic group and that this pandemic-related stress is positively associated with anxiety and depression [2]. Black individuals are more fearful of contracting COVID-19 than White Americans, likely due to disproportionate exposure to the virus [3]. Researchers have speculated that repeated and persistent exposure to the suffering of other Black individuals, by means of the pandemic, may lead to a vicarious trauma response and secondary emotional and physical symptoms [4]. Communities of color experience secondary trauma during times of national distress [5, 6], and COVID-19 is no exception. Black individuals are more likely to experience COVID-related post-traumatic stress symptoms [7].
The disproportionate impact of the COVID-19 pandemic on the mental health of Black individuals within the USA may be exacerbated by the preexisting pandemic of racism [5, 8]. The Black community has faced historical racial injustices and trauma, which has led to heightened awareness of racism’s interaction with the existing pandemic [9]. Events such as the Tuskegee Syphilis Study and the HIV/AIDS epidemic, both examples of systemic failure to provide proper treatment to Black individuals with ailments due to underlying medical racism, have resulted in lingering cultural mistrust of American institutions and historically rooted worry regarding the treatment of Black people during the COVID-19 pandemic [10]. As a result, Black individuals fear racial bias in disease testing and treatment [4].
To our knowledge, very few studies have directly and empirically examined the intersecting effects of racism in the context of the COVID-19 pandemic on Black mental health [11,12,13]. Cokley and colleagues found that race-related concerns about COVID-19 are associated with increased depression and anxiety, and that this association is partially mediated by perceived discrimination [12]. Fisher et al. demonstrated that Black individuals are more likely to experience racial bias associated with the coronavirus, and this bias was positively associated with depressive and anxiety symptoms [13]. Greater perceptions of COVID-19 as a health threat and beliefs about racial discrimination in medical settings were shown to have a synergistic effect such that their interaction is associated with greater psychological distress than either stressor alone [11]. Other studies have examined Black mental health during the COVID-19 pandemic alone [14] and the impact of either COVID-19 stress or racial stress on mental health during COVID-19 [15], but not examined how these two pandemics intersect to produce unique COVID-19 racial stressors impacting Black mental health. Given the dearth of research in this area, additional research regarding the impact of COVID-19 race-related concerns on mental health is needed to inform policy and prevention efforts addressing vaccination outreach, healthcare services, and racial healing efforts both now as it pertains to the current COVID-19 pandemic and in preparation for future pandemics and other public health crises.
In this study, we investigated the link between mental health and stressors at the intersection of racism and COVID-19. To do so, we operationalized race-related COVID stress (RRCS) as stressors faced by Black individuals specifically due to being Black during the COVID-19 pandemic; such stressors include things like worry about being Black and contracting COVID-19 and the pandemic eliciting reminders of race-related, historical medical trauma. We hypothesized that higher levels of RRCS would be associated with greater psychological distress and decreased subjective well-being.
Risk Factors
In addition to RRCS, Black individuals face pre-existing everyday injustices, due to their race, known as everyday discrimination [16]. Everyday discrimination has consistently been shown to have negative impacts on both positive and negative aspects of mental health across the lifespan, such as anxiety, depression, and life-satisfaction [17, 18]. Everyday discrimination is particularly relevant in the acute context of COVID-19 due to increased awareness of racial discrimination after the murder of George Floyd in 2020 [19]. Thus, everyday discrimination’s salience makes it likely to have worsened the already negative impact of RRCS on mental health.
Unlike everyday discrimination which captures direct experiences of racism, cultural mistrust is a byproduct of historical racism. Cultural mistrust refers to the mistrust an individual holds towards societal institutions (e.g., healthcare, criminal justice system) due to historical and continuous mistreatment [20, 21]. Cultural mistrust is generally high within the Black community and has been shown to have significant impacts on mental health [22, 23]. Thus, as general cultural mistrust outside of the context of COVID-19 has impacts on one’s mental health and well-being, it may also exacerbate the impacts of acute RRCS [24]. Therefore, we hypothesized that cultural mistrust would exacerbate the negative impacts of RRCS on mental health outcomes.
Protective Factors
Despite the greater burden of COVID-19 on the Black community, Black individuals have been shown to have higher levels of resilience than White individuals [25]. Religion, physical activity, and hope have been facilitators of coping during the COVID-19 pandemic [26]. However, little research has examined additional protective factors for the Black community during COVID-19, especially in relation to race-related COVID stress.
According to the African-centered worldview, culturally specific protective factors are most likely to be responsible for a large part of Black resilience as they have a greater impact than traditional protective factors [27]. Three evidence-based cultural protective factors are positive Black identity, Black activism, and spirituality/religiosity. Black identity, the meaning a Black individual gives to their racial group membership [28], is predictive of decreased psychological distress and increased well-being [29, 30]. Black activism is a natural coping response to oppressive racism [31,32,33] and is associated with higher subjective well-being, empowerment, and social support, especially in times of grief and pain [34, 35]. Religiosity/spirituality is known to be especially protective within the Black community [36], and is associated with increased psychological well-being, mental health, and social functioning [30, 37]. In addition to their direct relationships with positive mental health, Black identity, Black activism, and spirituality/religiosity are all protective factors against the effects of race-related stressors on psychological distress, anxiety, depression [29, 38, 39].
Of note, there is also some conflicting literature that counters the protective role of Black identity and activism. For activism, Hope and colleagues found that higher activism exacerbates the association between microaggressions and resulting anxiety and stress [40]. As for racial identity, Ashburn-Nardo and colleagues identified three conflicting models of the role racial identity may play in the relation between discrimination and mental health: (1) Black identity as a buffer against the psychological distress occurring with discrimination, (2) Black identity as an antecedent to discrimination, and later leading to distress, and (3) Black identity as a consequence of discrimination, and later leading to distress [41]. While they found support for all three models, they noted that the benefits of Black identity outweigh the negatives [41]. Similarly, Sellers and Shelton showed that while racial centrality was associated with perceived discrimination, public regard buffered discrimination’s negative impacts on mental health [29]. Generally, the majority of research involving these constructs supports Black identity and activism as beneficial [29,30,31,32,33,34,35, 39], supporting the rationale for their use as protective factors against race-related stress. Because less is known about these evidence-based protective factors in the context of COVID-19, we examined the impact of Black identity, Black activism, and spirituality/religiosity on the relationship between RRCS and mental health.
The Current Study
In sum, the purpose of this study was to examine the impact of RRCS on the mental health of Black individuals in the USA. Moreover, we also examined the role of culturally specific risk (i.e., everyday discrimination) and protective factors (e.g., religious involvement, Black identity, and Black activism) in this relation. We proposed the following model (see Fig. 1):
We hypothesized:
-
1.
Endorsement of RRCS would be associated with increased psychological distress and lower well-being.
-
2.
Everyday discrimination and cultural mistrust would moderate the relation between RRCS and mental health, such that they would strengthen this association (i.e., even greater psychological distress and lower well-being).
-
3.
Black identity, Black activism, and spirituality/religiosity would moderate the relation between RRCS and mental health, such that they would weaken this association (i.e., less psychological distress and greater well-being).
Racial trauma seems to be a critical factor facing communities of color during the pandemic [5]. Understanding the impact of RRCS and its moderating factors may contribute to the development of effective multilevel interventions addressing racial trauma. Thus, we aim to empirically examine the importance of considering racial stress in the disproportionate impact of COVID-19 on Black mental health.
Methods
Study Design
Data were collected from The Association of Black Psychologists’ (ABPsi) COVID-19 Needs Assessment of the Mental Health Impact of COVID-19 on Blacks living in the USA, which was commissioned by the Congressional Tri-Caucus. Additional details about the dataset may be found in the Needs Assessment study report [42]. The Association surveyed a cross-sectional sample of Black/Africana adults drawn from a multi-state Qualtrics panel.
Participants
The total sample consisted of 2480 participants that self-identified as Black/Africana (e.g., Black, Black American, African American, African, Afro-Caribbean, Afro-Latinx). All participants were 18 years or older and had been living in the USA at least since the last quarter of 2019 (prior to declaration of the pandemic in the USA). Participants were primarily sampled from California, Washington D.C., Louisiana, Maryland, Michigan, Texas, and the Mississippi Delta. These states/regions were selected for their inclusion of cities/counties containing COVID-19 hotspots, a high concentration of Black residents, and/or to diversify the types of regions chosen (e.g., rural, urban), based on location and population size. Respondents were also sampled from three convenience states: Georgia, Florida, and Ohio. Participant characteristics are shown in Table 1.
Measures
Race-Related COVID Stress (RRCS)
Race-related COVID stress (RRCS) was measured using eight conceptually similar items that examined participants’ worries, stressors, and thoughts at the intersection of COVID-19 and racism. A checklist of items was given in which each item captured a different type/source of RRCS experienced during the pandemic (e.g., “COVID-19 was like the Tuskegee (syphilis) Experiment”). RRCS was categorized and analyzed in two ways: (a) as a dichotomous variable indicating whether an individual endorsed any type of RRCS or not and (b) as a continuous variable indicating the number of RRCS sources one endorsed. The dichotomous version of the variable was used to conduct all the main analyses, such that participants who endorsed at least one RRCS were coded as 1 and those who did not endorse any stressors were coded as 0. The continuous measure of the scale was only used in one post-hoc exploratory analysis to examine whether the number of sources of RRCS was a significant predictor of the outcome variables—all the items were summed to produce scores ranging from 0 to 8, with higher scores indicating greater RRCS. The scale showed adequate internal reliability (α=.63).
Psychological Distress
The 4-item version of the Patient Health Questionnaire (PHQ-4) was used to measure psychological distress [43]. Participants were asked how often they have been bothered by specific depression or anxiety symptoms within the past 2 weeks. Response options ranged from 0- Not at all to 3- Nearly every day, such that higher scores indicated more frequently occurring symptoms. Overall scale scores were calculated by summing all four items, resulting in an overall range of 0–12. The PHQ-4 is a well-validated measure of depression and anxiety with good construct and factorial validity [43, 44]. and good internal consistency [44]. In this study, the internal consistency was good (α =.88).
Subjective Well-Being
Subjective well-being was measured using two items from the Medical Outcomes Study (MOS) 20-Item Short Form Health Survey (SF-20) [45]. Participants were asked how much of the time they felt like (1) a happy person and (2) calm and peaceful since COVID-19 began. Response options ranged from 1- All of the time to 6- None of the time. Items were reverse coded, rescaled to range from 0 to 100, and averaged so that higher scores indicated greater well-being. Though these two items alone have not been previously validated, the scale was internally consistent within this study (α=.82).
Everyday Discrimination
Everyday discrimination was measured using the 10-item expanded version of the Everyday Discrimination Scale [16]. The scale measures experiences of everyday discrimination by asking participants to indicate how often they have experienced various examples of discrimination in their day-to-day life (e.g., being followed in stores). Response options ranged from 0- Never to 5- Almost every day. The items were averaged across the scale so that overall scale scores range from 0 to 5, with higher scores indicating more frequent experiences of discrimination. The Everyday Discrimination Scale has been shown to demonstrate good internal consistency and construct validity [46, 47]. In this study, the Everyday Discrimination Scale showed high internal consistency (α=.92).
Cultural Mistrust
Cultural mistrust was measured using the Revised Cultural Mistrust Inventory (CMI) [48], which was adapted from the original Cultural Mistrust Inventory [49]. The scale consisted of 10 items assessing participants’ beliefs, opinions, and attitudes regarding mistrust towards the dominant culture (i.e., White individuals) in a variety of domains (e.g., “White teachers teach subjects so that it favors Whites”). Participants indicated the extent to which they agree or disagree with each statement, with responses ranging from 1-Strongly Disagree to 7- Strongly Agree. Responses were summed so the overall scale scores ranged from 10 to 70, with higher scores indicating higher levels of mistrust. The factorial validity [46], criterion-related validity [49], and internal [48, 49] have all previously been demonstrated to be adequate or better. In this study, Cronbach’s alpha for this scale was .81, indicating good reliability.
Black Identity
The Centrality and Private Regard subscales of the Multidimensional Inventory of Black Identity (MIBI) Short Form were used to measure Black identity [28; Wout et al. (unpublished manuscript), 2020] by identifying the extent to which participants agreed with certain statements regarding Black identity. The Centrality subscale measures the extent to which an individual holds their race as a strong part of their self-concept (e.g., “In general, being Black is an important part of my self-image”). Private Regard measures how favorably an individual views their race, specifically, other Black individuals and their own membership (e.g., “I am proud to be Black.”). Responses ranged from 1-Strongly disagree to 7- Strongly agree. Responses were averaged across items, and higher scores indicated higher levels of centrality or private regard. Previous studies have demonstrated the internal reliability of the MIBI [28; Wout et al. (unpublished manuscript), 2020] and in this study, the internal consistency was adequate-good with a Cronbach’s alpha of .70 for Centrality and .84 for Private Regard.
Black Activism
Black activism was measured using four items adapted from the Multidimensional Measure of Black Activism scale (MMBA) [50]. Participants were asked to what extent they were involved in a variety of activities related to involvement in the Black community and issues within the past year (e.g., “Been involved in a program, project, group, and/or organization geared towards helping or uplifting the Black community?”) Response options ranged from 1- Frequently to 4- Never. Responses were reverse coded and averaged so that higher responses on the scale indicated greater Black involvement. Previous research has demonstrated that the MMBA has excellent internal reliability (α = .95), and in this study, the Cronbach’s alpha was .83, indicating good internal reliability.
Spirituality/Religiosity
Engagement in spirituality/religiosity was measured using five conceptually similar items that assessed spiritual and/or religious coping strategies, thoughts, and activities during the COVID-19 pandemic (e.g., Religious or spiritual practices [praying, reading religious texts] [to cope with COVID-19]). Each item endorsed was coded as 1 then dichotomized into groups of 1 or greater and 0. The Cronbach’s alpha was .63, demonstrating adequate reliability.
Demographic Variables
All binary variables were dummy coded (0 or 1) and used within the analyses as categorical variables. Given the low response rates, “transgender” and “non-binary” responses were coded as missing and gender was dummy coded (0- Man, 1= Woman). Income and education level were both used as continuous variables within the analysis, in the order/categories shown within Table 1. This was done in order to increase the interpretability of the results and is acceptable due to the ordinal nature of these variables [51]. “Prefer not to answer” and non-responses were both treated as missing data.
Procedures
The University of Cincinnati’s IRB deemed this study non-human subjects research due to our use of deidentified secondary data. The original study protocol was approved by The MayaTech Corporation’s IRB, Protocol No. 2020-001. Participants were recruited through Qualtrics LLC’s survey panel. Prior to completing the survey, participants provided informed consent to be a part of the study and confirmed eligibility. The survey was conducted from February 1, 2021 to March 31, 2021 (approximately 1 year after the declaration of COVID-19 as a pandemic in the USA). The survey collected information regarding a variety of indicators. For the purposes of this study, we extracted data regarding RRCS, perceived discrimination, cultural mistrust, spirituality/religiosity, Black activism, Black identity, subjective well-being, psychological distress, and participant demographics.
Data Management and Statistical Analysis
The data were analyzed using the Statistical Package for the Social Sciences (SPSS), version 28. We screened the data for missing cases and normality. Although Little’s MCAR Test was significant, indicating the data were not missing completely at random, χ2(238) = 432.26, p<.001, further examinations were conducted. The additional analyses revealed minimal levels (<6%) and monotone patterns of missingness, indicating that the data were missing at random and that mean imputation could be used [52,53,54]. Thus, we used mean imputation for all multi-item variables. However, we could not impute any single-item categorical variables or sociodemographic covariates due to the nature of these variables, resulting in varied sample sizes across analyses.
Assumptions of univariate normality were met for skewness and kurtosis (skewness < 3, kurtosis < 10). The data met the assumption of independent residuals, multivariate normality, linearity, homoscedasticity, and no multicollinearity. We detected that less than 0.5% of the data fell outside of the typical range of data; however, due to desired response variability and the tolerability of minimal outliers within large sample sizes [55], we retained all cases.
Descriptive statistics were conducted by calculating frequencies and proportions for categorical variables and means and standard deviations for continuous variables. Preliminary analyses, namely Pearson Chi-Square Tests for categorical variables and independent samples T-tests for continuous variables, were conducted to determine differences in participant characteristics of those who endorsed RRCS as compared to those who did not endorse this stress.
We hypothesized that RRCS would be positively associated with psychological distress and negatively associated with subjective well-being. To test this hypothesis, we conducted independent regression analyses between (1) RRCS and psychological distress and (2) RRCS and subjective well-being. These analyses were conducted with the dichotomous RRCS variable. Age, gender, household income, education level, essential worker status, and partner status were included as covariates in both analyses at the second step. Due to missing covariate data, the sample size for this analysis was 2320. We also conducted additional post-hoc analyses to determine whether the number of sources of RRCS (as opposed to dichotomous endorsement or non-endorsement) was uniquely associated with the mental health outcomes. We used linear regression to examine the relation between a continuous measure of RRCS and the mental health outcomes (psychological distress and well-being) for those who had experienced at least one stressor, while controlling for the covariates.
To detect whether the proposed moderators moderate the relation between the dichotomous RRCS variable and the mental health outcomes, we conducted moderation analyses using the PROCESS Macro by Hayes in SPSS [56]. To complete the moderation, we entered RRCS as the X variable in all analyses. We also entered psychological distress and well-being as the Y variable in subsequent analyses, and we entered each previously defined moderator variables into the moderator variable field, in subsequent analyses, for a total of 10 moderator analyses. We conducted our moderation analyses using a 95% confidence interval and 5000 bootstrap resamples. We entered significant covariates from the analyses testing hypothesis 1, reducing the sample size to 2328 for psychological distress and 2461 for well-being.
Results
Sample Characteristics and Associations with RRCS
About 40% of the participants met criteria for a clinically significant level of depression (40.9%) and anxiety (40.2%) symptoms. About one quarter (24.3%) of participants had been previously diagnosed with a depression, anxiety, or substance use disorder; and 63.1% of the sample endorsed at least one stressor. The remaining statistics regarding sample characteristics may be found in Table 1. Those who endorsed RRCS tended to be older in age and had higher levels of cultural mistrust, everyday discrimination, racial centrality, and participation in activism (see Table 2). Those who endorsed RRCS were also more likely to be essential workers (X2 [1, N = 2480] = 7.04, p < .01), to have previously attended an HBCU (X2 [1, N = 2448] = 45.84, p < .001), and to have engaged in spiritual/religious practices during the pandemic (X2 [1, N = 2480] = 64.41, p < .001).
RRCS, Psychological Distress, and Subjective Well-Being
Race-related COVID stress was positively associated with psychological distress, β= .18, t(2312)=9.10, p<.001, such that those who experienced stressors at the intersection of racism and the COVID-19 pandemic (M=5.17, SD=3.86) had higher levels of psychological distress than those who did not (M=3.47, SD=4.01). The full model accounted for 14% of the variance in psychological distress, with RRCS accounting for 4% of the variance in psychological distress alone. Further analyses showed that this effect was also significant for both the depression, β= .15, t(2312)=7.57, p<.001, and anxiety subscales, β= .18, t(2312)=9.22, p<.001. As for significant covariates in this relationship, younger age, β= −.28, t(2312)= −14.25, p<.001, identification as a woman (as opposed to men), β=.06, t(2312)=3.10, p<.01, lower education levels, β= −.06, t(2312)= −2.79, p<.01, and lower income levels, β= −.07, t(2312)= −3.08, p<.01 were associated with greater psychological distress.
RRCS was negatively associated with well-being, β= −.05, t(2312)= −2.31, p<.05. Participants who endorsed RRCS (M=55.49, SD=26.55) had significantly lower levels of well-being than those who did not endorse RRCS (M=57.87, SD= 27.09). The full model accounted for 1% of the variance in well-being while RRCS accounted for 0.2% of the variance. Gender was the only significant covariate in this analysis β= −.08, t(2312)= −4.01, p<.001, such that women had significantly lower levels of well-being than men.
Post-hoc examination of the number of sources of RRCS’ relation to mental health outcomes determined that for those who experienced at least one stressor, higher endorsement of RRCS was associated with higher levels of psychological distress, β = .12, t(1459) = 4.74, p <.001. However, this relation was not significant when well-being was used as the outcome variable, p>.05.
Moderators of RRCS
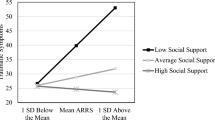
Cultural mistrust significantly moderated the association between RRCS and psychological distress (see Table 3). Post-hoc simple slope analyses showed a significant positive relation between cultural mistrust and psychological distress for those who endorsed RRCS, β = .079, t(1465) = 3.13, p<.01 (See Fig. 2). There was no significant association between cultural mistrust and psychological distress for those who did not endorse RRCS, β = −.021, t(851) = −0.652, p>.05. As indicated by insignificant interaction terms, none of the other proposed moderators (i.e., everyday discrimination, Black identity, Black activism, and spirituality/religiosity) significantly moderated the association between RRCS and well-being nor the association between RRCS and psychological distress, p>.05.
Discussion
The COVID-19 pandemic has been shown to widen physical and mental health inequities affecting Black individuals. Researchers have theorized that stress from the COVID-19 pandemic may interact with historical and present-day race-related stressors facing the Black community to present a unique experience of stress fueling these health disparities [5, 6]. In this study, we examined how stress at the intersection of racism and the COVID-19 pandemic impacted the mental health of Black individuals during the pandemic. Our first hypothesis was supported as results showed that positive endorsement of RRCS was predictive of higher psychological distress and lower well-being, above and beyond significant sociodemographic characteristics (gender, race, education, and income for psychological distress; gender for well-being). For those who endorsed at least one stressor, the amount of RRCS was positively associated with psychological distress, but not well-being. Regarding our second and third hypotheses on the moderation of race-related COVID stress’ association with mental health, only cultural mistrust was shown to be significant. Cultural mistrust strengthened the existing association between RRCS and mental health outcomes, posing further risk to one’s mental health. No other risk and protective factors, including everyday discrimination, Black activism, Black identity, and spirituality/religiosity exacerbated or buffered these associations.
As one of the first studies to empirically examine RRCS’ associations with mental health, our findings demonstrate the importance of considering how racism and COVID-19 interact to create a synergistic form of stress that may impact mental health. Furthermore, RRCS’ associations with psychological distress and well-being above and beyond sociodemographic characteristics demonstrate that mental health inequities during COVID-19 extend beyond socioeconomic lines. Racism is a hierarchical social system which ranks certain racial groups as inferior, thus manifesting through the very structure of institutions (e.g., residential segregation), mass culture (e.g., persistent negative stereotypes within media), and acts of discrimination (e.g., unjust police stops) [57]. Our measure of RRCS captured racial stressors in the context of COVID-19 that are linked to historical and present-day institutional racism and discrimination. For example, worry about COVID-19 mirroring the Tuskegee syphilis study captures multiple aspects of racism and its effects (i.e., fear of discrimination and the use of institutional systems to exploit Black individuals). Thus, RRCS may be attributed to a combination of a longstanding history of racism in the USA and a recent increase in its awareness along with the simultaneous rise of the COVID-19 pandemic [12, 19]. Our results are consistent with theory that describes race-related stress as a significant factor in the mental health of Black individuals during times of national distress, including the COVID-19 pandemic [5, 6].
Our findings showed that for those who endorsed at least one stressor, the number of RRCS was still positively associated with psychological distress, but not well-being. These findings indicate that in addition to whether one endorses RRCS or not, the number of sources of RRCS is also predictive of psychological distress, suggesting a potential compounding effect as the number of sources of RRCS experienced rises. However, the number of stress sources endorsed does not play a role in impacting well-being, only whether one endorses RRCS or not. Our observation of these differential associations is consistent with existing literature as well-being and psychological distress have been shown to have unique drivers and differential consequences [58]. Tests of discriminant validity have also shown that psychological well-being and psychological distress are distinct indicators of mental health, rather than opposite ends of a spectrum, as the absence of psychopathology does not indicate optimal functioning and vice versa [59]. Though RRCS was associated with overall mental health (both well-being and distress), it had the greatest impacts on psychological distress. Overall, the more pervasively Black individuals experience stress around racism and COVID, the more distress they feel.
Whereas the majority of the sample endorsed at least one RRCS stressor, a large group of individuals still did not endorse any RRCS (36.9%). As indicated in our analyses of sample characteristics, older individuals, individuals who have previously attended an HBCU, and essential workers are more likely to report RRCS. As curriculum at HBCUs promotes the development of Black identity and a detailed understanding of Black history, including racism, HBCU attendance may make it more likely for Black individuals to be aware of the ways in which COVID-19 interacts with race-related stressors [60]. In addition, a variety of cultural factors seem to be positively associated with endorsement of RRCS, including engagement in spirituality/religiosity and higher cultural mistrust, everyday discrimination, racial centrality, and activism participation. One reason for these positive associations may be that individuals who endorse these cultural factors tend to engage more with their community and value their race as central to their identity. We infer that these individuals’ investment in their racial identity increases their propensity to experience concern for their community and detect discrimination, resulting in distress. These findings are consistent with previous research that immersion in Black culture, private regard, and racial centrality are all associated with racial discrimination and psychological distress [61], and ethnic group membership is predictive of higher race-related stress [62], likely due to a greater ability to perceive discrimination [29].
Contrary to our hypotheses, racial centrality, private regard, Black activism, and spirituality/religiosity did not buffer the associations between RRCS and psychological distress or well-being. Given our previous findings that these cultural factors are associated with increased RRCS, these results are not surprising. There have been mixed results as to whether the discrimination-distress relation is buffered by several of these factors, including Black identity [29, 41, 63] and activism [40, 64]. Our findings show that traditional protective factors may not have the same buffering impact against racism’s effects in the context of the COVID-19 pandemic.
At first glance, our findings may seem to suggest that the “cultural buffers” have a deleterious impact on mental health. However, these cultural buffers have an extensive amount of literature supporting their utility for positive outcomes, including self-esteem, well-being, and social functioning [35, 37]. It is rather more likely that individuals with high endorsement of these buffers may be more aware of discrimination and distressed by its implications. Thus, these associations capture the distress that accompanies being Black in America where systematic racism and injustice are ever-present. As the majority of our sample has experienced at least some form of RRCS, the implications of these results are far-reaching and do not suggest individual pathology but rather a systemic challenge affecting the Black community.
On the other hand, cultural mistrust moderated the association between RRCS and psychological distress, such that cultural mistrust was associated with higher levels of psychological distress, only for those who experienced RRCS. Thus, cultural mistrust exacerbates the deleterious associations between RRCS and psychological distress. Cultural mistrust has been shown to be associated with perceived racism [65] and can be conceptualized as a byproduct of historical and present-day institutional racism [20]. It may be that persistent cultural mistrust elevates awareness of RRCS towards the point of symptom exacerbation. These findings also demonstrate that chronic forms of racism may exacerbate the impact of acute manifestations of racism [24].
Of note, cultural mistrust was not associated with psychological distress at low levels of RRCS. Despite the majority of research on cultural mistrust being aimed towards examining its associations with reduced help-seeking behaviors and health, cultural mistrust was originally purported by theorists to be a healthy “cultural paranoia” as a result of historical and continuous racism [20, 21]. One study found that cultural mistrust holds a curvilinear relation with psychological well-being, such that both low and high levels were associated with lower well-being, and moderate levels were deemed to be optimal [23]. Our findings suggest that cultural mistrust’s impacts are nuanced and sometimes innocuous. In this case, whether one experiences RRCS is the defining factor to whether cultural mistrust results in psychological distress. Furthermore, though cultural mistrust and RRCS share some conceptual similarities, their moderating relation and absence of collinearity indicate that they are distinct constructs. This highlights the unique nature of RRCS and warrants further research into its impact on Black individuals during COVID-19.
Limitations
There are a few limitations to acknowledge within this study. These data were collected 1 year into the COVID-19 pandemic, prior to universal distribution of the vaccine in the USA, yet after the early stages of the pandemic in which there was greater uncertainty about COVID. Thus, these results represent a time-limited snapshot of the potential impact of RRCS on mental health, as there may have been other points of the pandemic in which this stress may have had greater or lesser impacts on mental health. Relatedly, the police-involved or race-based deaths of George Floyd, Breonna Taylor, Ahmaud Arbery, and many other Black individuals in 2020 also increased racial tension and awareness of racism at the time of the survey. It was not possible to isolate the co-occurring stress of this racial climate, which also may have exacerbated the negative impacts on mental health, from that of RRCS. Future studies should examine how the mental health of Black individuals has progressed throughout the COVID-19 pandemic, using longitudinal data, while considering how it relates to both stressors of RRCS and increased racial tension. Finally, some of our measures were limited as the original survey was aimed to cover a wide variety of topics. For example, the well-being measure contained only two items adapted from a longer scale. Furthermore, although significant, RRCS only accounted for 4% of the variance of psychological distress and 1% of well-being alone. As racism is a multidimensional construct that includes many covert sources with cascading effects, there are likely other important racism-related factors within the context of COVID-19 that impact mental health. For example, due to structural racism Black individuals are overrepresented in essential worker jobs which involve unique COVID-19 stressors, such as increased COVID exposure and reduced occupational resources (e.g., paid sick leave, ability to work remotely) [66]. To better identify RRCS and its impacts on mental health, researchers should develop expanded measures of RRCS that may capture multiple aspects of racism (i.e., institutional, cultural, and discrimination). Moreover, although we established face validity and internal reliability of RRCS, the full psychometric properties of this scale are unknown, and future researchers should aim to validate this measure.
Conclusions and Implications
Overall, our research demonstrates that stress at the intersection of racism and COVID-19 has negative implications for the mental health of Black individuals. In the early stages of COVID-19, COVID-19 was described as an equal opportunity disease in that it was thought to equally impact individuals beyond sociodemographic characteristics such as race and class [1]. Since then, an aggregation of research has shown that this is not the case, and in fact, COVID-19 seems to widen existing disparities [1, 67]. Our results show that RRCS is associated with negative impacts on mental health and thus may contribute to these disparities. Though the landscape of COVID-19 is continuously changing, these results will continue to bear relevance well-beyond the end of the pandemic. COVID-19 is projected to have long-term impacts on physical and mental health due to both the biomedical impacts of COVID-19 and stressors experienced during the pandemic [68], making relevant the role of RRCS for years to come. In addition, our results provide further support that Black mental health is at risk during times of national distress, due to the preexisting pandemic of racism [5, 6]. Therefore, our examination of RRCS provides a framework for how racism may interact with future pandemics or national stressful events. As cultural mistrust strengthened the positive association between RRCS and psychological distress, chronic impacts of racism interact with acute racial stressors to further worsen Black mental health. Nevertheless, cultural mistrust’s association with mental health only for those who endorsed RRCS also demonstrates that cultural mistrust is more nuanced than existing empirical literature has suggested. There may in fact be an adaptive “healthy paranoia” that only has negative impacts when it is associated with stress.
Our results bear implications for how researchers, clinicians, and policymakers should approach Black mental health in the age of COVID-19 and beyond. Policymakers should continue to address structural racism, which lies at the core of RRCS. Greater funding for public health research examining structural racism and its manifestations as a social determinant of health is needed [69]. Policies that focus on expansion of access to mental health services, such as by expanding financial support for community-level programing, insurance coverage, and school-based services [70], will help to reduce these disparities. Furthermore, organizations involved in health research should uphold an antiracist stance through commitment to examine and ameliorate the intersection of racism and chronic and acute stressors [69].
Since psychological distress and well-being are both indicative of other outcomes, such as physical health, productivity, and pro-social behavior, the negative implications of RRCS may extend beyond the constructs measured in this study [58]. In particular, individuals with lower psychological well-being are more likely to contract viral infection, less likely to develop antibodies from a vaccine, and less likely to survive overall [58]. Thus, researchers should examine the impact of RRCS on physical health, its relations to COVID-19 morbidity, and mortality disparities. Researchers should also examine other protective factors not assessed in this study (e.g., formal and informal support) in order to identify mutable factors that may help to buffer RRCS. Although our findings suggest that RRCS must be addressed on a systemic level, mechanisms to foster Black resilience in the present-day are still needed. Finally, as the literature on cultural mistrust is sparse, researchers should further explore its associations with both positive and negative aspects of mental health.
Mental health practitioners must consider RRCS within their case conceptualization for Black clients and should also be open to discussion about racism [5, 6]. Given how cultural mistrust exacerbated the impacts of RRCS, clinicians must acknowledge their position in the institution of healthcare which has historically marginalized and harmed the Black community, fostering mistrust [6]. Therefore, if a client is expressing mistrust, clinicians should refrain from invalidating this “healthy paranoia” and openly discuss how the client and clinician can collaborate to build trust [6]. They should also take a culturally informed approach by relying on the use of cultural humility and applying culturally adapted treatments, when necessary [5]. Finally, clinicians should also aim to foster individual client strengths to help the client manage their RRCS [5]. By employing these recommendations, mental health professionals and advocates may begin to challenge RRCS and its impacts on mental health, which is necessary to fully improve Black mental health outcomes in the age of COVID-19.
Data Availability
The COVID-19 Communities of Color Needs Assessment Phase 1 data are available on the National Urban League website at https://nul.org/sites/default/files/2022-03/21.35.NUL_.Covid_.Layout.D9_v9.pdf (Executive Summary) and https://nul.org/sites/default/files/2022-03/21.35.NUL_.Covid_.ABPsi_.D3.2_v3.pdf (Association of Black Psychologists).
Change history
24 July 2023
A Correction to this paper has been published: https://doi.org/10.1007/s40615-023-01726-y
References
Mein SA. COVID-19 and health disparities: the reality of “the great equalizer”. J Gen Intern Med. 2020;35(8):2439–40. https://doi.org/10.1007/s11606-020-05880-5.
Kujawa A, Green H, Compas BE, Dickey L, Pegg S. Exposure to COVID-19 pandemic stress: associations with depression and anxiety in emerging adults in the United States. Depress Anxiety. 2020;37(12):1280–8. https://doi.org/10.1002/da.23109.
Pew Research Center. Health concerns from COVID-19 much higher among Hispanics and Blacks than Whites. Pew Research Center; 2020. https://www.pewresearch.org/politics/2020/04/14/health-concerns-from-covid-19-much-higher-among-hispanics-and-blacks-than-whites/. Accessed 10 Jan 2023
Sneed RS, Key K, Bailey S, Johnson-Lawrence V. Social and psychological consequences of the COVID-19 pandemic in African-American communities: lessons from Michigan. Psychol Trauma. 2020;12(5):446–8. https://doi.org/10.1037/tra0000881.
Liu SR, Modir S. The outbreak that was always here: racial trauma in the context of COVID-19 and implications for mental health providers. Psychol Trauma. 2020;12(5):439–42. https://doi.org/10.1037/tra0000784.
Novacek DM, Hampton-Anderson JN, Ebor MT, Loeb TB, Wyatt GE. Mental health ramifications of the COVID-19 pandemic for Black Americans: clinical and research recommendations. Psychol Trauma. 2020;12(5):449–51. https://doi.org/10.1037/tra0000796.
Shigemoto Y. Exploring state-level variabilities between perceived community resilience and posttraumatic stress symptoms during the COVID-19 pandemic: multilevel modeling approach. Traumatology. 2021;27(1):98–106. https://doi.org/10.1037/trm0000303.
Laurencin CT, Walker JM. A pandemic on a pandemic: racism and COVID-19 in Blacks. Cell Syst. 2020;11(1):9–10. https://doi.org/10.1016/j.cels.2020.07.002.
Loeb TB, Ebor MT, Smith AM, Chin D, Novacek DM, Hampton-Anderson JN, Norwood-Scott E, Hamilton AB, Brown AF, Wyatt GE. How mental health professionals can address disparities in the context of the COVID-19 pandemic. Traumatology. 2021;27(1):60–9. https://doi.org/10.1037/trm0000292.
Thompkins F, Goldblum P, Lai T, Hansell T, Barclay A, Brown LM. A culturally specific mental health and spirituality approach for African Americans facing the COVID-19 pandemic. Psychol Trauma. 2020;12(5):455–6. https://doi.org/10.1037/tra0000841.
Cobb RJ, Erving CL, Byrd WC. Perceived COVID-19 health threat increases psychological distress among Black Americans. Ethn Racial Stud. 2021;44(5):806–18. https://doi.org/10.1080/01419870.2021.1867216.
Cokley K, Krueger N, Cunningham SR, Burlew K, Hall S, Harris K, Castelin S, Coleman C. The COVID-19/racial injustice syndemic and mental health among Black Americans: the roles of general and race-related COVID worry, cultural mistrust, and perceived discrimination. J Community Psychol. 2021;50(6):2542–61. https://doi.org/10.1002/jcop.22747.
Fisher CB, Tao X, Yip T. The effects of COVID-19 victimization distress and racial bias on mental health among AIAN, Asian, Black, and Latinx young adults. Cultur Divers Ethnic Minor Psychol. Advance online publication. https://doi.org/10.1037/cdp0000539.
Chae DH, Yip T, Martz CD, Chung K, Richeson JA, Hajat A, Curtis DS, Rogers LO, LaVeist TA. Vicarious racism and vigilance during the COVID-19 pandemic: mental health implications among Asian and Black Americans. Public Health Rep. 2021;136(4):508–17. https://doi.org/10.1177/00333549211018675.
Dush CMK, Manning WD, Berrigan MN, Hardeman RR. Stress and Mental Health: A Focus on COVID-19 and racial trauma stress. RSF. 2022;8(8):104–34. https://doi.org/10.7758/RSF.2022.8.8.06.
Williams DR, Yan Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2(3):335–51. https://doi.org/10.1177/135910539700200305.
Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, Gupta A, Kelaher M, Gee G. Racism as a determinant of health: a systematic review and meta-analysis. PloS One. 2015;10(9):e0138511. https://doi.org/10.1371/journal.pone.0138511.
Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc Sci Med. 2013;95:115–27. https://doi.org/10.1016/j.socscimed.2012.11.031.
Lipscomb AE, Ashley W. Surviving being Black and a clinician during a dual pandemic: personal and professional challenges in a disease and racial crisis. Smith Coll Stud Soc Work. 2020;90(4):221–36. https://doi.org/10.1080/00377317.2020.1834489.
Grier WH, Cobbs PM. Black rage. New York, NY: Basic Books; 1968.
White JL. Toward a Black psychology. In: Jones RL, editor. Black psychology. New York, NY: Harper & Row; 1980. p. 1–12.
Alang S, McAlpine DD, Hardeman R. Police brutality and mistrust in medical institutions. J Racial Ethn Health Disparities. 2020;7(4):760–8. https://doi.org/10.1007/s40615-020-00706-w.
Bell TJ, Tracey TJ. The relation of cultural mistrust and psychological health. J Multicult Couns Dev. 2006;34(1):2–14. https://doi.org/10.1002/j.2161-1912.2006.tb00022.x.
Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93(2):200–8. https://doi.org/10.2105/ajph.93.2.200.
Riehm KE, Brenneke SG, Adams LB, Gilan D, Lieb K, Kunzler AM, Smail EJ, Holingue C, Stuart EA, Kalb LG, Thrul J. Association between psychological resilience and changes in mental distress during the COVID-19 pandemic. J Affect Disord. 2021;282:381–5. https://doi.org/10.1016/j.jad.2020.12.071.
Bateman LB, Schoenberger YMM, Hansen B, Osborne TN, Okoro GC, Speights KM, Fouad MN. Confronting COVID-19 in under-resourced, African American neighborhoods: a qualitative study examining community member and stakeholders’ perceptions. Ethn Health. 2021;26(1):49–67. https://doi.org/10.1080/13557858.2021.1873250.
Utsey SO, Bolden MA, Lanier Y, Williams O. Examining the role of culture-specific coping as a predictor of resilient outcomes in African Americans from high-risk urban communities. J Black Psychol. 2007;33(1):75–93. https://doi.org/10.1177/0095798406295094.
Sellers RM, Smith MA, Shelton JN, Rowley SAJ, Chavous TM. Multidimensional model of racial identity: a reconceptualization of African American racial identity. Pers Soc Psychol Rev. 1998;2(1):18–39. https://doi.org/10.1207/s15327957pspr0201_2.
Sellers RM, Shelton JN. The role of racial identity in perceived racial discrimination. J Pers Soc Psychol. 2003;84(5):1079–92. https://doi.org/10.1037/0022-3514.84.5.1079.
Mushonga DR, Henneberger AK. Protective factors associated with positive mental health in traditional and nontraditional Black students. Am J Orthopsychiatry. 2020;90(1):147–60. https://doi.org/10.1037/ort0000409.
Krueger NT, Garba R, Stone-Sabali S, Cokley KO, Bailey M. African American activism: the predictive role of race related stress, racial identity, and social justice beliefs. J Black Psychol. 2021;48(3–4):273–308. https://doi.org/10.1177/0095798420984660.
Prosper T, Gushue GV, Lee TR. Promoting African American activism: experiences of racism-related stress and spirituality. J Black Psychol. 2021;47(8):657–68. https://doi.org/10.1177/00957984211034949.
Szymanski DM, Lewis JA. Race-related stress and racial identity as predictors of African American activism. J Black Psychol. 2015;41(2):170–91. https://doi.org/10.1177/0095798414520707.
Al’Uqdah S, Adomako F. From mourning to action: African american women’s grief, pain, and activism. J Loss Trauma. 2017;23(2):91–8. https://doi.org/10.1080/15325024.2017.1393373.
Grayman-Simpson N. Black community involvement and subjective well-being. Pan Afr. 2012;5(3):26–42.
Hackney CH, Sanders GS. Religiosity and mental health: a meta–analysis of recent studies. J Sci Study Relig. 2003;42(1):43–55. https://doi.org/10.1111/1468-5906.t01-1-00160.
Taylor RJ, Chatters LM, Levin J. Religion in the lives of African Americans: social, psychological, and health perspectives. Thousand Oaks, CA: Sage Publications; 2003.
Bierman A. Does religion buffer the effects of discrimination on mental health? Differing effects by race. J Sci Study Relig. 2006;45(4):551–65. https://doi.org/10.1111/j.1468-5906.2006.00327.x.
Watson-Singleton NN, Mekawi Y, Wilkins KV, Jatta IF. Racism’s effect on depressive symptoms: examining perseverative cognition and Black Lives Matter activism as moderators. J Couns Psychol. 2021;68(1):27–37. https://doi.org/10.1037/cou0000436.
Hope EC, Velez G, Offidani-Bertrand C, Keels M, Durkee MI. Political activism and mental health among Black and Latinx college students. Cultur Divers Ethnic Minor Psychol. 2018;24(1):26–39. https://doi.org/10.1037/cdp0000144.
Ashburn-Nardo L, Monteith MJ, Arthur SA, Bain A. Race and the psychological health of African Americans. Group Process Intergroup Relat. 2007;10(4):471–91. https://doi.org/10.1177/1368430207081536.
Randolph Cunningham SM, Burlew AK, Jackson-Lowman H, Golden A, Cokley KO, Lowe T, Ramsey L, Barnes O, Harris M, Castelin S, Jackson T. The Association of Black Psychologists’ (ABPsi) COVID-19 needs assessment report: mental health and other impacts of the pandemic on Blacks/Africanas living in the U.S. National Urban League; 2021. https://nul.org/sites/default/files/2022-03/21.35.NUL_.Covid_.ABPsi_.D3.2_v3.pdf. Accessed 28 Apr 2023
Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. 2009;50(6):613–21. https://doi.org/10.1176/appi.psy.50.6.613.
Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, Schneider A, Brähler E. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122(1-2):86–95. https://doi.org/10.1016/j.jad.2009.06.019.
Ware JE, Sherbourne CD, Davies AR. Developing and testing the MOS 20-item short-form health survey: a general population application. In: Stewart AL, Ware JE, editors. Measuring functioning and well-being: the medical outcomes study approach. Durham and London: Duke University Press; 1992. p. 277–90.
Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40(3):208–30. https://doi.org/10.2307/2676349.
Taylor TR, Kamarck TW, Shiffman S. Validation of the Detroit area study discrimination scale in a community sample of older African American adults: the Pittsburgh healthy heart project. Int J Behav Med. 2004;11(2):88–94. https://doi.org/10.1207/s15327558ijbm1102_4.
Irving MA. Oppositional identity and academic achievement among African American males (Publication No. 3055998) [Doctoral Dissertation]. Santa Barbara, CA: University of California, Santa Barbara; 2002.
Terrell F, Terrell S. An inventory to measure cultural mistrust among Blacks. West J Black Stud. 1981;5(3):180–4.
Thomas ON. Collective action, socio-political attitudes, and social change preference: a multidimensional measure of African American activism. [Master’s thesis]. East Lansing: Michigan State University; 2001.
Robitzsch A. Why ordinal variables can (almost) always be treated as continuous variables: clarifying assumptions of robust continuous and ordinal factor analysis estimation methods. Front Educ. 2020;5(589965)
Montelpare WJ, Read EA, McComber T, Mahar A, Ritchie K. Applied statistics in healthcare research. Pressbooks; date unknown.
Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7(2):147–77. https://doi.org/10.1037/1082-989X.7.2.147.
Peugh JL, Enders CK. Missing data in educational research: a review of reporting practice and suggestions for improvement. Rev Educ Res. 2004;74(4):525–56. https://doi.org/10.3102/00346543074004525.
Pallant J. SPSS Survival manual. 6th ed. London: McGraw-Hill Education; 2016.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression based approach. 3rd ed. New York, NY: The Guilford Press; 2017.
Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health. 2019;40:105–25. https://doi.org/10.1146/annurev-publhealth-040218-043750.
Huppert FA. Psychological well-being: evidence regarding its causes and consequences. Appl Psychol Health Well Being. 2009;1(2):137–64. https://doi.org/10.1111/j.1758-0854.2009.01008.x.
Lamers SM, Westerhof GJ, Bohlmeijer ET, ten Klooster PM, Keyes CL. Evaluating the psychometric properties of the mental health continuum-short form (MHC-SF). J Clin Psychol. 2011;67(1):99–110. https://doi.org/10.1002/jclp.20741.
Lee DL, Ahn S. The relation of racial identity, ethnic identity, and racial socialization to discrimination–distress: a meta-analysis of Black Americans. J Couns Psychol. 2013;60(1):1–14. https://doi.org/10.1037/a0031275.
Utsey SO, Chae MH, Brown CF, Kelly D. Effect of ethnic group membership on ethnic identity, race-related stress, and quality of life. Cultur Divers Ethnic Minor Psychol. 2002;8(4):366–77. https://doi.org/10.1037/1099-9809.8.4.367.
Banks KH, Kohn-Wood LP. The influence of racial identity profiles on the relationship between racial discrimination and depressive symptoms. J Black Psychol. 2007;33(3):331–54. https://doi.org/10.1177/0095798407302540.
Mekawi Y, Carter S, Packard G, Wallace S, Michopoulos V, Powers A. When (passive) acceptance hurts: race-based coping moderates the association between racial discrimination and mental health outcomes among Black Americans. Psychol Trauma. 2021;14(1):38–46. https://doi.org/10.1037/tra0001077.
Thompson CE, Neville H, Weathers PL, Poston WC, et al. Cultural mistrust and racism reaction among African-American students. J Coll Stud Dev. 1990;31(2):162–8.
University of Illinois School of Public Health. Black, Hispanic Americans are overrepresented in essential jobs. 2021. https://publichealth.uic.edu/news-stories/black-hispanic-americans-are-overrepresented-in-essential-jobs/Accessed 10 Jun 2023.
Roebuck JB, Murty KS. Historically Black colleges and universities: their place in American higher education. Westport: Praeger; 1993.
Saltzman LY, Lesen AE, Henry V, Hansel TC, Bordnick PS. COVID-19 mental health disparities. Health Secur. 2021;19(S1):S5–S13. https://doi.org/10.1089/hs.2021.0017.
Higgins V, Sohaei D, Diamandis EP, Prassas I. COVID-19: From an acute to chronic disease? Potential long-term health consequences. Crit Rev Clin Lab Sci. 2021;58(5):297–310. https://doi.org/10.1080/10408363.2020.1860895.
Churchwell K, Elkind M, Benjamin RM, Carson AP, Chang EK, Lawrence W, Mills A, Odom TM, Rodriguez CJ, Rodriguez F, Sanchez E, Sharrief AZ, Sims M, Williams O, American Heart Association. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation. 2020;142(24):e454–68. https://doi.org/10.1161/CIR.0000000000000936.
Shim RS, Starks SM. COVID-19, structural racism, and mental health inequities: policy implications for an emerging syndemic. Psychiatr Serv. 2021;72(10):1193–8. https://doi.org/10.1176/appi.ps.202000725.
Acknowledgements
We would like to acknowledge the Association of Black Psychologists (ABPsi), ABPsi's National Office staff, organizational partners in The Alliance of National Psychological Associations for Racial and Ethnic Equity, and the 18 participating community partner orgnizations for their work in conducting the COVID-19 Communities of Color Needs Assessment Phase 1. We would also like to acknowledge the individual contributions of Huberta Jackson-Lowman, PhD and Cheryl Grills, PhD in conducting the Needs Assessment and Paula Silva, PhD; Monica Mitchell, PhD; Julia Rabin, M.A.; and Savanha Renald, B.A. in preparing this manuscript.
Funding
This research study is supported by the National Urban League and the Congressional Tri-Caucus. Funding was provided for The Needs Assessment Phase 1 through grants to the National Urban League, and subawards were distributed to members and partners organizations of the Alliance of National Psychological Associations for Racial and Ethnic Equity, Dr. Cheryl Grills- principal investigator. The National Urban League secured funding with grants from The W. K. Kellogg Foundation, JPB Foundation, Ford Foundation, The California Endowment, Weingart Foundation, and The California Wellness Foundation. The Association of Black Psychologists also provided funds beyond the grant for data management and statistical support. This material is based upon work supported by the National Science Foundation Graduate Research Fellowship under Grant No. 2035701. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the National Science Foundation. The work in this study was also supported by the Albert C. Yates Fellowship Program.
Author information
Authors and Affiliations
Contributions
The study conception and design for this secondary study were led by SC and FJ. All authors contributed to revisions of the study design and analysis plan. Study design and data collection for the original primary study was performed by SRC and KB. The data analysis was performed by SC, and all authors contributed to interpretation of the data. The first draft of the manuscript was written by SC. All authors provided edits on previous versions of the manuscript as well as read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This research involved the use of human participants. The University of Cincinnati’s IRB deemed this study non-human subjects research due to our use of deidentified secondary data. The original study protocol was approved by The MayaTech Corporation’s IRB, Protocol No. 2020-001.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The surname of coauthor Farrah Jacquez was misspelled (as “Jaquez”) in the article as originally published.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Castelin, S., Jacquez, F., Burlew, A.K. et al. Dual Pandemics: Race-Related COVID Stress and Mental Health Outcomes in Black Individuals. J. Racial and Ethnic Health Disparities 11, 2141–2153 (2024). https://doi.org/10.1007/s40615-023-01683-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-023-01683-6