Abstract
Racial and ethnic disparities in birth outcomes have persisted in the United States for decades, though the causes remain poorly understood. The life course perspective posits that poorer outcomes of Black birthing people stem from heightened exposure to stressors early in life and cumulative exposure to stressors over time. Despite its prominence, this perspective has seldom been investigated empirically. We analyzed longitudinal data gathered from 1319 women in low-income households in Wisconsin who received perinatal home visiting services. Variable- and person-centered analyses were performed to assess whether 15 adverse childhood experiences (ACEs) and 10 adverse adult experiences (AAEs) were associated, alone and in combination, with pregnancy loss, preterm birth, and low birth weight among Hispanic (i.e., Latinx) and non-Hispanic Black and White participants. As expected, there were disparities in preterm birth and low birth weight, and both ACEs and AAEs were linked to poorer pregnancy and birth outcomes. Unexpectedly, bivariate and multivariate analyses showed that the associated effects of ACEs and AAEs were most robust for non-Hispanic White women. A latent class analysis produced four patterns of life course adversity, and multigroup latent class analyses confirmed that, compared to White women, higher-adversity class assignments were associated with less robust effects for Hispanic women, and even less robust effects for Black women. We discuss interpretations of the paradoxical findings, including the possibility that alternative sources of stress such as interpersonal and structural racism may better account for the reproductive disparities that disproportionately affect Black birthing people.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pregnancy loss, preterm birth (PTB), and low birth weight (LBW) are major public health issues in the United States (US) given their incidence and impact on maternal and infant health. It is estimated that 15–25% of recognized pregnancies end in miscarriage, a life event that has been linked to significant psychosocial consequences and economic burden [72, 73]. Of all infants born in the US, about 10.5% are premature and 8.2% are below normal birthweight [68]. PTB and LBW are leading causes of infant mortality and, for surviving infants, they forecast long-term health and development concerns that pass on substantial economic costs to society [2, 4, 22, 71, 89].
The development of strategies to prevent unwanted pregnancy and birth outcomes hinges partly on understanding their etiologies. The list of risks for pregnancy loss, PTB, and LBW is long and includes genetic and epigenetic influences, maternal and paternal age, placental insufficiency, infection, cervical length, hypertension, diabetes, obesity, smoking, alcohol and substance use, low health care access and quality, chronic stress, violence, discrimination, and racism [30, 35, 45, 74, 77, 81, 91]. Collectively, these and other complex processes contribute to pregnancy loss, PTB, and LBW, though their influence may not manifest equally across outcomes or population subgroups.
To illustrate, there are stark racial and ethnic differences in pregnancy and birth outcomes among American women [2, 65, 75, 76, 82]. For example, Black women are 50–60% more likely than White women to give birth prematurely [8, 68]. Many risks for poor pregnancy and birth outcomes are correlated with race and ethnicity but have not been shown to fully account for racial/ethnic variation. Due partly to their heterogeneous and multifactorial origins, these disparities have proven difficult to explain and redress.
To improve the prediction and prevention of health disparities, scholars have called for approaches that account for the cumulative impact of adverse and inequitable experiences from conception through adulthood [26, 41]. One prominent example is the life course perspective [50, 51], which posits that disparities in birth outcomes partly result from exposure to harmful experiences and conditions during sensitive developmental periods early in life (i.e., early programming) and cumulative stress over time that leads to allostatic load and physiological wear and tear (i.e., cumulative pathways). This model has been widely disseminated, and it serves as a framework that guides federal maternal and child health priorities [3, 26, 28]. Yet, surprisingly few studies have examined whether racial and ethnic disparities in pregnancy and birth outcomes are associated with exposure to stressful life events over the life course [7, 69].
Partial support for the life course perspective can be found in research indicating that poor pregnancy and birth outcomes are associated with increased exposure to adverse childhood experiences (i.e., ACEs), which include harmful events and conditions such as child abuse and neglect, domestic violence, and incarceration of a parent or caregiver [14, 46, 60, 85]. ACEs are more prevalent in the US among non-Hispanic Black than non-Hispanic White individuals [52, 56], and it is plausible that differential exposure to early adversity contributes to disparities in pregnancy and birth outcomes. On the other hand, a series of recent studies have found that ACEs are more prevalent among low-income White adults than low-income Black adults [58, 61, 80]. There also is some evidence to suggest that socioeconomic disparities in birth outcomes vary by race and ethnicity (see [7] for review), though a recent analysis of nearly two million births in California over a 10-year period showed that racial/ethnic disparities in birth outcomes were present across the income distribution [42].
These nuanced findings underscore the point that empirical applications of the life course model should aim to disentangle outcome variance explained by adversity from socioeconomic differences that prevail among racial/ethnic groups [10]. While it is standard practice to account for socioeconomic confounds at the study design phase or through the use of statistical controls, there is growing interest in applying variable- and person-centered techniques to explore between- and within-group heterogeneity [20, 24]. In addition to the use of novel statistical techniques, scholars have attempted to strengthen the ecological and cross-cultural validity of ACE assessments by incorporating indicators of socioeconomic risk [17, 27, 57].
Alongside novel approaches to measuring and modeling ACEs, recent research has drawn attention to adverse adult experiences (AAEs) and their deleterious effects within and across generations [59, 63, 87, 92]. Poor pregnancy and birth outcomes are associated with many adult adversities, including intimate partner violence [35], community violence [29, 54], residential segregation [55], housing insecurity and homelessness [19, 47], and discrimination and racism [1, 45]. Studies have also found that cumulative exposure to AAEs increases the risk of poor physical and mental health above and beyond the effects of ACEs [62, 83]. Yet, no known studies have examined whether the accumulation of adverse experiences throughout childhood and adulthood result in disparate pregnancy and birth outcomes. Research along these lines is needed to further develop life course models of adversity and reproductive health.
Study Aims
To better understand the relationship between life course adversity and disparities in pregnancy and birth outcomes, this study analyzes longitudinal data collected from a sample of 1319 racially and ethnically diverse women from low-income households in Wisconsin who received perinatal home visiting services. The aims of the study are twofold. First, bivariate and multivariate analytic approaches are conducted to test whether ACEs and AAEs are associated with pregnancy loss, PTB, and LBW overall and whether associations differ between self-identified Black, White, and Hispanic (i.e., Latina; Latine; Latinx) participants. Second, latent class analysis is used to identify subgroups that share similar patterns of exposure to life course adversity, and multigroup latent class regressions are performed to explore whether different patterns are linked to pregnancy and birth outcomes within each racial/ethnic group.
Methods
Sample and Data
Data for the current study were collected from participants in the Families and Children Thriving (FACT) Study, an ongoing longitudinal investigation of Wisconsin households that received perinatal home visiting services. All families were served by agencies that are subsidized by the federal Maternal, Infant, and Early Childhood Home Visiting (MIECHV) Program, which allocates funds to states, territories, and tribal communities to support evidence-based programs for priority populations at risk of poor maternal and child health outcomes [25]. In Wisconsin, MIECHV supports four home visiting models: Early Head Start, Healthy Families America, Nurse-Family Partnership, and Parents as Teachers. Illustrating the socioeconomic composition of the sample, 98.3% of participating households were at or below 200% of federal poverty line or eligible for means-tested public benefits.
Launched in August 2015, the FACT Study tracks a cohort of 1967 primary caregivers who completed a baseline survey after the birth of a child associated with a home visiting episode (response rate = 62.8%). Approximately 97.9% of respondents self-identified as women (n = 1923). For the present study, 90 women were removed from the analytic sample because they were less than 19 years old at baseline. Another 234 participants who self-identified as American Indian or Alaska Native, Asian or Pacific Islander, multiracial, or other race/ethnicity were omitted from the sample because their group sample sizes were too small to make valid statistical comparisons.
Another 280 eligible participants were omitted from the analysis via listwise deletion due to missing or incomplete data on adverse experiences or study outcomes. Compared to the 280 participants who were removed from the sample, the analytic sample of 1319 participants was less likely to be Black than White or Hispanic and more likely to live with spouse or partner (p < 0.05); there were no differences in maternal age, number of children, or educational attainment.
Following a data sharing agreement, program records used to create measures of pregnancy loss, PTB, LBW, and ACEs were obtained from an administrative database managed by the Wisconsin Department of Children and Families. Survey data were collected by mail or phone after completing an informed consent procedure. Baseline surveys from the FACT Study supply primary data on participant demographics and AAEs along with supplemental data on pregnancy losses. All study protocols were approved by the instiutional review board at the University of Wisconsin-Milwaukee (FWA00006171).
Measures
Pregnancy and Birth Outcomes
Administrative data were used to create dichotomous measures indicating if participants had ever given birth prematurely (i.e., < prior to 37th week of pregnancy) or to a low birthweight infant (i.e., < 2500 g or 5.5 pounds). Primary data used to create a dichotomous measure of pregnancy loss were drawn from archival program records. A total of 235 participants were missing pregnancy loss data, largely because the information was collected by home visiting staff during a prenatal assessment, meaning that the information was not recorded for most program participants who enrolled postnatally. Missing cases were imputed using data from a baseline survey item from the FACT Study that asked participants to report the number of pregnancy losses since turning age 18.
Adverse Childhood Experiences
Home visiting providers assessed participant ACEs using the Childhood Experiences Survey, an expanded ACE assessment that has demonstrated good internal consistency, test–retest reliability, and criterion validity [13, 57]. Ten conventional ACEs were coded dichotomously, including five forms of child maltreatment (physical abuse,sexual abuse; emotional abuse; physical neglect; emotional neglect) and five forms of household dysfunction (mental illness; substance use; incarceration/jail; domestic violence; prolonged absence of a parent). The 10 items were summed to create a cumulative score. In addition to the 10 conventional ACEs, five novel adversities were measured dichotomously, including three socioeconomic indicators (frequent financial problems; food insecurity; homelessness) and two extrafamilial indicators of victimization (bullying; crime). These five items were summed with the 10 conventional ACEs to create a 15-item score. For further information about item language and scoring as well as the prevalence of ACEs in the FACT Study, see [57].
Adverse Adult Experiences
At baseline, FACT Study participants completed the Adult Experiences Survey, a measure of AAEs that has demonstrated good internal consistency, test–retest reliability, and criterion validity (for information about item language, scoring, and prevalence, see [62]). Ten adversities that occurred after the respondent’s 18th birthday were assessed, five of which were associated with a spouse, partner, or household member: physical or emotional abuse, sexual abuse, substance use, mental health problem, and incarceration or jail. The remaining five AAEs were sexual assault, crime victimization, frequent financial problems, homelessness, and discrimination. The 10 items were coded dichotomously and summed to create a cumulative score.
Race and Ethnicity
The race and ethnicity of study participants was self-reported and coded into three mutually exclusive categories: non-Hispanic Black, non-Hispanic White, and Hispanic.
Covariates
Survey data from the FACT Study were used to construct four demographic measures that served as model covariates. At baseline, a continuous measure of participant age was calculated along with a categorical measure of educational attainment with the following values: (1) less than high school, (2) some high school, (3) high school diploma or General Educational Development certificate, (4) some college credit, no degree, (5) associate degree, (6) bachelor’s (4-year) degree or higher. Participant responses also yielded a dichotomous variable indicating if they were cohabitating with a partner or spouse as well as a count measure denoting their number of biological children.
Analysis Plan
A descriptive analysis of data was performed, followed by bivariate logistic regressions tests of association between adversity measures and study outcomes for the full sample and for racial/ethnic subgroups. Controlling for covariates, multivariate logistic regressions were performed to examine main effects associated with ACE and AAE scores. Interaction terms were added to a second set of multivariate analyses to test whether race and ethnicity moderated the estimated effects of ACEs and AAEs. The preceding analyses were conducted in IBM SPSS 28.
Mplus 8.8 was used to complete a latent class analysis (LCA) of heterogeneous patterns in adverse childhood and adult experiences while adjusting for covariates. Model fit was judged based on a lower Bayesian information criterion, a significant Lo-Mendell-Rubin adjusted LRT test, and practical significance [67]. Missing data were handled via full information maximum likelihood estimation. Once an optimal number of adversity classes was identified, the LCA was transformed into a multigroup latent class regression with a model constraint command and model test statement [66], which yielded within-group comparisons for Black, White, and Hispanic women in their predicted probabilities of pregnancy and birth outcomes based on their exposure to lifetime adversity.
Results
Table 1 describes the sample demographic characteristics and key study variables. Participants’ mean age was 27.4 years, and their mean level of educational attainment was 3.3; 41.5% had a high school diploma or equivalent, and 40.5% had obtained some postsecondary education (not shown). More than half (57.2%) of participants were living with a partner/spouse, and they averaged 2.0 biological children. There were significant differences among racial/ethnic groups for each demographic indicator.
On average, participants reported 3.5 adversities on the 10-item ACE score and 4.7 adversities on the 15-item ACE score. The sample mean on the 10-item AAE score was 3.4. Significant racial/ethnic differences in ACEs and AAEs were observed, with White women reporting the highest scores and Hispanic women reporting the lowest scores.
Approximately 31.1% of participants experienced a pregnancy loss, 19.5% experienced a PTB, and 14.4% gave birth to a LBW infant. The prevalence of pregnancy loss did not differ significantly among racial/ethnic groups (Black = 32.2%; Hispanic = 30.2%; White = 31.2%). The prevalence of PTB did vary significantly by race/ethnicity (p < 0.05), with higher rates reported by Black women (26.7%) than White women (18.3%) and Hispanic women (17.0%). LBW also varied by race/ethnicity, with higher rates for Black women (20.1%) than Hispanic women (13.7%) and White women (12.7%).
Study Aim 1
Table 2 presents unadjusted bivariate associations between ACEs and study outcomes in the full sample and by racial/ethnic subgroup. Pregnancy loss was significantly correlated with all ACEs except for indicators of socioeconomic concern (financial problems; food insecurity; homelessness). Associations with PTB and LBW were less robust; only sexual abuse was significantly correlated with all three outcomes. The 10-item and 15-item ACE scores were associated with an increased odds of pregnancy loss, but not PTB and LBW. Descriptively, patterns of association between ACEs and study outcomes varied by race and ethnicity. For instance, pregnancy loss was correlated with 11 out of 15 ACEs for White women and 8 out of 15 ACEs for Hispanic women, but for Black women no ACEs correlated with pregnancy loss in the expected direction. The 10-item and 15-item ACE scores were associated with a greater likelihood of pregnancy loss in White and Hispanic women but not Black women.
As shown in Table 3, there were significant unadjusted associations between pregnancy loss and all AAEs except for partner/spouse mental health problems. Associations between AAEs and PTB and LBW were less consistent. Only incarceration/jail of a partner or spouse was significantly associated with all three outcomes. The 10-item AAE score was associated with all three outcomes in the full sample.
Model 1 coefficients in Table 4 are from multivariate logistic regressions that estimate associated effects of ACE scores and AAE scores on pregnancy and birth outcomes. Controlling for demographic characteristics, participant ACE scores were significantly associated with an increased risk of having had a pregnancy loss (b = 0.13, SE = 0.02; p < 0.001) and a LBW infant (b = 0.06, SE = 0.03; p = 0.048), but not PTB (b = 0.05, SE = 0.03; p = 0.104). The 10-item AAE score also was significantly associated with pregnancy loss (b = 0.13, SE = 0.03; p < 0.001) and LBW (b = 0.08, SE = 0.03; p = 0.020), but not PTB (b = 0.05, SE = 0.03; p = 0.117).
Table 4 also presents coefficients from tests of interaction effects between race/ethnicity and adversity scores (model 2). Results indicated that the strength of association between ACEs and pregnancy loss was significantly greater for White and Hispanic women than for Black women. Moderation test results trended in the same direction for other outcomes, but no other statistically significant differences were present.
Study Aim 2
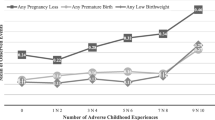
Figure 1 displays results from a latent class analysis of 15 ACEs and 10 AAEs. Four classes were identified (sample percentages in parentheses): (1) low life course adversity (32.8%), (2) moderately high childhood adversity and moderately low adult adversity (22.1%), (3) moderately low childhood adversity and moderately high adult adversity (27.5%); (4) high life course adversity (17.6%). Results (not shown) from an analysis of the full sample indicated that, when compared to women who experienced low life course adversity (class 1), women in classes 2, 3, and 4 were more like to have had a pregnancy loss, and women in classes 3 and 4 also were more likely to have had a PTB and LBW infant.
Results shown in Table 5 are from multigroup latent class regressions that generated within-group comparisons for Black, Hispanic, and White women. The coefficients represent the predicted probability that an adversity class was associated with a poor outcome, with low life course adversity (class 1) serving as the reference group. One pairwise difference was observed among Black women: Compared to participants assigned to class 1, participants in class 3 had a significantly higher probability of having had a pregnancy loss. To illustrate for ease of interpretation, Black women in class 1 had a 27% chance of having had a pregnancy loss whereas Black women in class 3 had a 51% chance of having had a pregnancy loss. For further context, adjusted probabilities shown in Table 5 can be compared to unadjusted outcome means in Table 1. For instance, the unadjusted prevalence of pregnancy loss among all Black women was 32% (Table 1), which was comparable to the adjusted probability of pregnancy loss among Black women who were exposed to high life course adversity (Table 5).
For Hispanic women, high life course adversity (class 4) was significantly associated with a greater risk of ever having a pregnancy loss, while adversity class 2 was marginally associated with an increased risk of prior pregnancy loss. For White women, assignment to classes 2, 3, and 4 was significantly associated with a higher risk of pregnancy loss; class 3 assignment was marginally associated with a higher risk of PTB; class 4 assignment was significantly associated with a higher risk of PTB; class 3 and 4 assignments were marginally associated with a higher risk of LBW.
Discussion
Informed by the life course perspective [50, 51], the primary aim of this study was to assess whether exposure to childhood and adult adversity contributed to pregnancy and birth outcome disparities among Black, White, and Hispanic women. Basic and advanced statistical methods were used to analyze data collected from a racially and ethnically diverse sample of low-income women who received perinatal home visiting services. What follows is a brief summary of key findings, a discussion of study implications and limitations, and a set of future directions for research on life course adversity and reproductive disparities.
Summary of Key Findings
Most ACEs and AAEs were correlated with at least one pregnancy or birth outcome in the full sample, but there was marked variation by race/ethnicity. For example, risk of pregnancy loss was correlated with 11 ACEs for White women, eight ACEs for Hispanic women, and no ACEs for Black women in the expected direction. Higher ACE scores were linked to some outcomes in White and Hispanic women but not Black women. Higher AAE scores were associated with all three outcomes in White women, pregnancy loss and LBW in Hispanic women, and only pregnancy loss in Black women. Interaction tests revealed that the association between ACE scores and pregnancy loss was greater for White and Hispanic women than for Black women; moderation effects trended in the same direction for PTB and LBW but were not statistically significant. Four latent classes of life course adversity were identified, and within-group contrasts showed that, compared to White women who experienced low lifetime adversity, White women in higher-adversity classes were often at risk of poorer pregnancy and birth outcomes. Comparatively, the estimated effects of assignment to higher-adversity classes were not as robust for Hispanic women, and they were even less robust for Black women.
Implications
Corroborating disparities that have been documented in the US for over a century [79], we found that Black women were at an elevated risk of PTB and LBW. By a mean age of 27, 1 in 5 Black women had given birth prematurely and more than 1 in 4 had given birth to a LBW infant. Comporting with population estimates [8, 68], the unadjusted prevalence of PTB and LBW in this sample was anywhere from 46 to 58% higher for Black women than White and Hispanic women. Yet, pregnancy loss rates did not differ significantly by race/ethnicity, contradicting the findings of Mukherjee et al. [65] that showed Black women were 1.57 times more likely than White women to have had a miscarriage. Our findings more closely align with results from the National Survey of Family Growth [75], which indicated that the percentage of pregnancies ending in loss were similar among Black and White women (20.7% vs. 21.3%) but lower among Hispanic women (15.0%). Unlike PTB and LBW, racial/ethnic differences in the epidemiology of pregnancy loss have received limited attention and deserve further investigation.
Although racial/ethnic differences in reproductive outcomes are well known, the causes remain incompletely understood. The life course perspective posits that these disparities result from differential exposure to stressors during developmentally sensitive periods and ongoing stressors that increase allostatic load and cumulative wear and tear. We found little support for this conceptual model in this analysis of 25 major life stressors. Paradoxically, both early adversity and cumulative pathways of adversity better explained poor pregnancy and birth outcomes for non-Hispanic White and Hispanic women than Black women. These findings were robust across basic and advanced statistical analyses of between- and within-group differences.
Specific explanations are not readily apparent, but generally the findings imply that the observed disparities in pregnancy and birth outcomes are due to influences that went unmeasured in this study. Pregnancy loss, PTB, and LBW are correlated with many environmental risks that are experienced unequally by racial/ethnic groups in the US, including inadequate prenatal and preconception care, low social support, and stressful neighborhood conditions to name but a few (for review, see [8]. Moreover, a rapidly growing body of research suggests that health disparities are rooted in exposure to racism, a chronic stressor facing Black, Indigenous, and other People of Color [32, 70, 86]. Racism, manifested interpersonally through racial discrimination and structurally through intersecting and mutually reinforcing systems and policies (e.g., housing,employment; criminal justice), has been shown in most studies to be strongly associated with adverse pregnancy and birth outcomes [1, 12, 39, 45, 84]. There is a need to further specify the causal pathways that link racism to disparities while moving toward consensus on definitions and measures of racism along with methods for differentiating the effects of racism from the effects of other adverse conditions and social determinants [31, 33, 40, 53]. Toward that end, there is a commensurate need to explore alternative measures of ACEs and AAEs that incorporate experiences of discrimination and racism [6].
Unmeasured biological and genetic processes that contribute to health disparities also may have attenuated the effects associated with adversity on pregnancy and birth outcomes in Black women. Downstream correlates of discrimination and racism such as hypertension, obesity, and infection and associated biological processes such as immune response and inflammation are plausible sources of reproductive disparity [8, 15, 18, 88]. In addition, while the amount of variance explained by genetics is thought to be small, theory and evidence suggest that epigenetic changes affecting fetal programming are likely to contribute more substantially to differential outcomes [8, 44, 53, 93]. Research on transgenerational epigenetic inheritance indicates that the effects of historical traumatic events, including ACEs, can be passed across generations [48]. Thus, inquiries informed by the life course perspective may be complemented by epigenetic studies that identify modifiable mechanisms of intergenerational transmission.
Taken together, all signs point to the conclusion that reproductive inequities stem from highly complex, syndemic origins. Although the adversities we measured did not help to explain why unwanted pregnancy and birth outcomes disproportionately affect Black women, it must be emphasized that exposure to early adversity and cumulative life course adversity increased the risk of poor outcomes in the full sample and in each racial/ethnic group. Thus, the fact that ACEs and AAEs were not linked to racial/ethnic disparities should not be misconstrued as implying that these events and conditions lacked predictive validity. Rather, we verified that adverse experiences are associated with poorer pregnancy and birth outcomes (e.g., [1, 15, 35, 46, 55, 60, 85]). Pending replication, our results suggest that widespread prevention of ACEs and AAEs may reduce pregnancy loss, preterm birth, and low birth weight overall but may not mitigate the persistent disparities that continue to plague the population and puzzle the field.
Study Limitations
Results should be interpreted while considering the study’s selective sample of women from low-income households receiving perinatal home visiting services in Wisconsin. Although there is little evidence to suggest that home visiting programs enhance pregnancy and birth outcomes [37, 64], the data are from a selective sample and should be compared with caution against populations with dissimilar characteristics. Along with questions of generalizability, home visiting enrollment may have corresponded with unmeasured differences between racial/ethnic groups (i.e., selection effects). Another limitation is the study’s modest sample size, which restricted statistical power and likely increased the Type-II error rate. Future studies with larger and more diverse samples are needed to assess reproductive disparities in other racial/ethnic groups, especially American Indian and Alaska Native populations given their elevated rates of PTB and LBW [9]. In addition, data on adverse experiences were drawn from retrospective assessments that may have introduced recall biases. Finally, while racial/ethnic disparities are of great importance, it is well understood that race and ethnicity are socially constructed phenomena that may be misclassified or oversimplified when they are operationally defined as mutually exclusive, binary categories.
Conclusion and Future Directions
Compared to other high-income countries, the US has higher rates of pregnancy loss, PTB, and LBW [21, 23], and it is also home to unrelenting disparities in reproductive health. In the interest of developing prevention and intervention strategies to remediate these disparities, there is a need to better understand the root causes of these complex outcomes. Two decades ago, Lu and Halfon [50] put forward a life course perspective that links health disparities to early and ongoing environmental stressors. This model has helped to shape maternal and child health policy in the US, though empirical studies of its assumptions are in short supply. The current study aimed to help fill this gap.
In this study of women from low-income households, we confirmed that greater exposure to early adversity and cumulative life course adversity increased the risk of poor pregnancy and birth outcomes. However, instead of contributing to disparities that disproportionately affect Black women and children, early and ongoing exposure to adverse experiences better explained pregnancy loss, PTB, and LBW among non-Hispanic White and Hispanic participants. We look forward to replication studies with larger and more representative samples in the US and worldwide given that similar racial/ethnic disparities have been observed in many high- and middle-income countries [78]. Bearing in mind that socioeconomic inequalities often correlate with race and ethnicity, researchers who interrogate nationally representative datasets are encouraged to unpack racial/ethnic differences across socioeconomic strata.
Further progress toward understanding how adverse environments affect reproductive health may be possible through advances in measurement and modeling. Future work should explore additional perinatal outcomes such as small for gestational age, recurrent pregnancy loss, timing and type of pregnancy loss, and various birth weight thresholds. The study of life course adversity can be enriched by extending recent efforts to develop ACE measures that are chronologically specific and more ecologically and cross-culturally valid [6, 34, 57] while also employing complementary, broad-based assessments of adverse adult experiences. We encourage scholars to push beyond the limits of the current study by measuring other factors that may increase allostatic load and contribute to physiological wear and tear, including conditions that affect the developing fetus. Along with everyday discrimination, racial discrimination, institutional racism, and structural racism warrant special attention, as do processes that may contribute to intergenerational transmission [31, 33, 88].
Finally, while there are many known correlates of reproductive health disparities, longitudinal studies into causal mechanisms have great potential to inform prevention efforts. Considerable funding and industry has been put toward improving pregnancy and birth outcomes via medical and clinical intervention, producing many practice recommendations [16, 38, 90] but no appreciable impact on population-level disparities. Less attention has been paid to psychosocial interventions that may improve pregnancy and birth outcomes overall and reduce disparities. Research has linked continuous support from health providers (e.g., nurses; midwives; doulas) to many benefits for birthing people [36], and one observational study found that doula care was associated with a lower rate of PTB [43]. Group-based models of care show some promise, though the evidence to date has not been uniform [11, 49]. Further trials are needed to examine the effects of these alternative and complementary health practices on pregnancy and birth outcomes, as are policy solutions that remove cost barriers to bringing these models to scale [5, 43]. Yet, if reproductive disparities are borne out of stress-related processes from conception to birth, as the life course perspective suggests, preconception and prenatal interventions may be necessary but insufficient remedies. Thus, we call for research on large-scale programs, policies, and systems change initiatives that may reduce inequities wholesale among disadvantaged and marginalized groups that bear the brunt of this wicked problem.
Data Availability
The authors do not have permission to share the source data.
Code Availability
The authors may provide syntax upon request.
References
Alhusen JL, Bower KM, Epstein E, Sharps P. Racial discrimination and adverse birth outcomes: an integrative review. Journal of Midwifery & Women’s Health. 2016;61(6):707–20.
Almeida J, Bécares L, Erbetta K, Bettegowda VR, Ahluwalia IB. Racial/ethnic inequities in low birth weight and PTB: the role of multiple forms of stress. Matern Child Health J. 2018;22(8):1154–63.
Alvidrez J, Castille D, Laude-Sharp M, Rosario A, Tabor D. The national institute on minority health and health disparities research framework. Am J Public Health. 2019;109(S1):S16–20.
Beam AL, Fried I, Palmer N, Agniel D, Brat G, Fox K, … & Armstrong J. Estimates of healthcare spending for preterm and low-birthweight infants in a commercially insured population: 2008–2016. J Perinatol. 2020;40(7), 1091–1099
Bellerose M, Rodriguez M, Vivier PM. A systematic review of the qualitative literature on barriers to high-quality prenatal and postpartum care among low-income women. Health Serv Res. 2022;57(4):775–85.
Bernard DL, Calhoun CD, Banks DE, Halliday CA, Hughes-Halbert C, Danielson CK. Making the “C-ACE” for a culturally-informed adverse childhood experiences framework to understand the pervasive mental health impact of racism on Black youth. J Child Adolesc Trauma. 2021;14:233–47.
Blumenshine P, Egerter S, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic disparities in adverse birth outcomes: a systematic review. Am J Prev Med. 2010;39(3):263–72.
Braveman P, Dominguez TP, Burke W, Dolan SM, Stevenson DK, Jackson FM, Collins JW, Driscoll DA, Haley T, Acker J, Shaw GM, McCabe ERB, Hay WW, Thornburg K, Acevedo-Garcia D, Cordero JF, Wise PH, Legaz G, Rashied-Henry K, … Waddell L. Explaining the Black-White disparity in PTB: a consensus statement from a multi-disciplinary scientific work group convened by the March of Dimes. Front Reprod Health. 2021;3
Brown CC, Moore JE, Tilford JM. Rates of preterm birth and low birthweight: an analysis of racial and ethnic populations: Study examines preterm birth and low birthweight rates among racial and ethnic populations. Health Aff. 2023;42(2):261–7.
Burris HH, Hacker MR. Birth outcome racial disparities: a result of intersecting social and environmental factors. In Seminars Perinatol. 2017; (Vol. 41, No. 6, pp. 360–366). WB Saunders
Buultjens M, Farouque A, Karimi L, Whitby L, Milgrom J, Erbas B. The contribution of group prenatal care to maternal psychological health outcomes: a systematic review. Women and Birth. 2021;34(6):e631–42.
Chambers BD, Baer RJ, McLemore MR, Jelliffe-Pawlowski LL. Using index of concentration at the extremes as indicators of structural racism to evaluate the association with PTB and infant mortality—California, 2011–2012. J Urban Health. 2019;96(2):159–70.
Choi C, Mersky JP, Janczewski CE, Lee CTP, Davies WH, Lang AC. Validity of an expanded assessment of adverse childhood experiences: a replication study. Child Youth Serv Rev. 2020;117:105216.
Christiaens I, Hegadoren K, Olson DM. Adverse childhood experiences are associated with spontaneous PTB: a case–control study. BMC Med. 2015;13(1):1–9.
Christian LM. Psychoneuroimmunology in pregnancy: immune pathways linking stress with maternal health, adverse birth outcomes, and fetal development. Neurosci Biobehav Rev. 2012;36(1):350–61.
Coomarasamy, A., Dhillon-Smith, R. K., Papadopoulou, A., Al-Memar, M., Brewin, J., Abrahams, V. M., … & Quenby, S. Recurrent miscarriage: evidence to accelerate action. Lancet. 2021;397(10285), 1675–1682.
Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, … & Fein JA. Adverse childhood experiences: expanding the concept of adversity. Am J Prevent Med. 2015;49(3), 354–361.
Culhane JF, Goldenberg RL. Racial disparities in preterm birth. In Seminars Perinatol. 2011;(Vol. 35, No. 4, pp. 234–239). WB Saunders.
Cutts DB, Coleman S, Black MM, Chilton MM, Cook JT, de Cuba SE, … & Frank DA. Homelessness during pregnancy: a unique, time-dependent risk factor of birth outcomes. Maternal Child Health J. 2015;19(6), 1276–1283.
Deichen Hansen ME. Predictors of preterm birth and low birth weight: a person-centered approach. SSM-Population Health. 2021;15:100897.
Dubay L, Hill I, Garrett B, Blavin F, Johnston E, Howell E, … & Cross-Barnet C. Improving birth outcomes and lowering costs for women on Medicaid: impacts of ‘Strong Start For Mothers And Newborns’. Health Affairs. 2020;39(6), 1042–1050.
Ely DM, Driscoll AK. Infant mortality in the United States, 2019: data from the period linked birth/infant death file. Natl Vital Stat Rep: From Centers Dis Control Prevent, Natl Center Health Stat, Natl Vital Stat Syst. 2021;70(14):1–18.
Emanuel EJ, Gudbranson E, Van Parys J, Gørtz M, Helgeland J, Skinner J. Comparing health outcomes of privileged US citizens with those of average residents of other developed countries. JAMA Intern Med. 2021;181(3):339–44.
Evans CR, Williams DR, Onnela JP, Subramanian SV. A multilevel approach to modeling health inequalities at the intersection of multiple social identities. Soc Sci Med. 2018;203:64–73.
Fernandes-Alcantara AL. Maternal, infant, and early childhood home visiting (MIECHV) program: background and funding. Congression Res Service. 2018;18:1–51.
Fine A, Kotelchuck M Rethinking MCH: the life course model as an organizing framework. US Department of Health and Human Services, Health Resources and Services Administration. Maternal Child Health Bureau. 2010;1–20.
Finkelhor D, Shattuck A, Turner H, Hamby S. A revised inventory of adverse childhood experiences. Child Abuse Negl. 2015;48:13–21.
Foney DM, DiBari J, Li R, Kogan M. Life course investments at the Maternal and Child Health Bureau. Pediatrics. 2022;149(Supplement 5):e2021053509B.
Goin DE, Gomez AM, Farkas K, Zimmerman S, Matthay EC, Ahern J. Exposure to community homicide during pregnancy and adverse birth outcomes: a within-community matched design. Epidemiology (Cambridge, Mass). 2019;30(5):713–22.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of PTB. The Lancet. 2008;371(9606):75–84.
Groos M, Wallace M, Hardeman R, Theall KP. Measuring inequity: a systematic review of methods used to quantify structural racism. J Health Disparities Res Pract. 2018;11(2):13.
Hailu EM, Maddali SR, Snowden JM, Carmichael SL, Mujahid MS. Structural racism and adverse maternal health outcomes: a systematic review. Health Place. 2022;78:102923.
Hardeman RR, Murphy KA, Karbeah JM, Kozhimannil KB. Naming institutionalized racism in public health literature: a systematic literature review. Public Health Rep. 2018;133(3):240–9.
Hawes DJ, Lechowicz M, Roach A, Fisher C, Doyle FL, Noble S, Dadds MR. Capturing the developmental timing of adverse childhood experiences: the Adverse Life Experiences Scale. Am Psychol. 2021;76(2):253–67.
Hill A, Pallitto C, McCleary-Sills J, Garcia-Moreno C. A systematic review and meta-analysis of intimate partner violence during pregnancy and selected birth outcomes. Int J Gynecol Obstet. 2016;133(3):269–76.
Hodnett ED, Gates S, Hofmeyr GJ, & Sakala C. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2013;7.
Issel LM, Forrestal SG, Slaughter J, Wiencrot A, Handler A. A review of prenatal home-visiting effectiveness for improving birth outcomes. J Obstet Gynecol Neonatal Nurs. 2011;40(2):157–65.
Jacobsson B, Simpson JL, FIGO Working Group for Preterm Birth, Jacobsson B, Simpson JL, Norman J, ... & Shennan A. FIGO good practice recommendations for reducing preterm birth and improving child outcomes. Int J Gynecol Obstet. 2021; 155(1), 1-4.
Janevic T, Zeitlin J, Egorova NN, Hebert P, Balbierz A, Stroustrup AM, Howell EA. Racial and economic neighborhood segregation, site of delivery, and morbidity and mortality in neonates born very preterm. J Pediatr. 2021;235:116–23.
Jeffers NK, Berger BO, Marea CX, Gemmill A. Investigating the impact of structural racism on black birthing people-associations between racialized economic segregation, incarceration inequality, and severe maternal morbidity. Soc Sci Med. 2023;317:115622.
Jones NL, Gilman SE, Cheng TL, Drury SS, Hill CV, Geronimus AT. Life course approaches to the causes of health disparities. Am J Public Health. 2019;109(S1):S48–55.
Kennedy-Moulton K, Miller S, Persson P, Rossin-Slater M, Wherry L, & Aldana G Maternal and infant health inequality: new evidence from linked administrative data (No. w30693). National Bureau of Economic Research. 2022.
Kozhimannil KB, Hardeman RR, Alarid-Escudero F, Vogelsang CA, Blauer-Peterson C, Howell EA. Modeling the cost-effectiveness of doula care associated with reductions in preterm birth and cesarean delivery. Birth. 2016;43(1):20–7.
Kuzawa CW, Sweet E. Epigenetics and the embodiment of race: developmental origins of US racial disparities in cardiovascular health. Am J Human Biol: Off J Human Biol Assoc. 2009;21(1):2–15.
Larrabee Sonderlund A, Schoenthaler A, Thilsing T. The association between maternal experiences of interpersonal discrimination and adverse birth outcomes: a systematic review of the evidence. Int J Environ Res Public Health. 2021;18(4):1465.
Leeners B, Rath W, Block E, Görres G, Tschudin S. Risk factors for unfavorable pregnancy outcome in women with adverse childhood experiences. J Perinat Med. 2014;42(2):171–8.
Leifheit KM, Schwartz GL, Pollack CE, Edin KJ, Black MM, Jennings JM, Althoff KN. Severe housing insecurity during pregnancy: association with adverse birth and infant outcomes. Int J Environ Res Public Health. 2020;17(22):8659.
Leimert KB, Olson DM. Racial disparities in pregnancy outcomes: genetics, epigenetics, and allostatic load. Curr Opin Physio. 2020;13:155–65.
Liu Y, Wang Y, Wu Y, Chen X, Bai J. Effectiveness of the CenteringPregnancy program on maternal and birth outcomes: a systematic review and meta-analysis. Int J Nurs Stud. 2021;120:103981.
Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7(1):13–30.
Lu MC, Kotelchuck M, Hogan V, Jones L, Wright K, Halfon N. Closing the Black-White gap in birth outcomes: a life-course approach. Ethnicity Dis. 2010;20(1 0 2):S2.
Maguire-Jack K, Lanier P, Lombardi B. Investigating racial differences in clusters of adverse childhood experiences. Am J Orthopsych. 2020;90(1):106–20.
Martin CL, Ghastine L, Lodge EK, Dhingra R, Ward-Caviness CK. Understanding health inequalities Through the lens of social epigenetics. Annu Rev Public Health. 2022;43(1):235–54.
Masho SW, Cha S, Chapman DA, Chelmow D. Understanding the role of violence as a social determinant of PTB. Am J Obstet Gynecol. 2017;216(2):183-e1.
Mehra R, Boyd LM, Ickovics JR. Racial residential segregation and adverse birth outcomes: a systematic review and meta-analysis. Soc Sci Med. 2017;191:237–50.
Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of adverse childhood experiences from the 2011–2014 behavioral risk factor surveillance system in 23 states. JAMA Pediatr. 2018;172(11):1038–44.
Mersky JP, Janczewski CE, Topitzes J. Rethinking the measurement of adversity: Moving toward second-generation research on adverse childhood experiences. Child Maltreat. 2017;22(1):58–68.
Mersky JP, Janczewski CE. Racial and ethnic differences in the prevalence of adverse childhood experiences: Findings from a low-income sample of US women. Child Abuse and Neglect. 2018;76:480–7.
Mersky JP, Janczewski CE, Nitkowski JC. Poor mental health among low-income women in the US: The rolesof adverse childhood and adult experiences. Soc Sci Med. 2018;206:14–21.
Mersky JP, Plummer Lee C. Adverse childhood experiences and poor birth outcomes in a diverse, low-income sample. BMC Preg Child. 2019;19(387):1–7.
Mersky JP, Choi C, Lee CP, Janczewski CE. Disparities in adverse childhood experiences by race/ethnicity, gender, and economic status: Intersectional analysis of a nationally representative sample. Child Abuse & Neglect. 2021;117:105066.
Mersky JP, Plummer Lee C, Janczewski CE. Toward the assessment of adverse adult experiences: An initial validation study of the Adult Experiences Survey. Psychol Trauma: Theory, Res Prac Pol. 2021;13(5):528–36.
Mersky JP, Plummer Lee C, Janczewski CE. Adverse adult experiences and health outcomes: Racial and ethnic differences in a low-income sample. Stress & Health. 2023 (Advance online publication). https://doi.org/10.1002/smi.3212
Moniz MH, Low LK, Stout MJ. Intensive nurse home visiting program and adverse birth outcomes. JAMA. 2022;328(1):23–4.
Mukherjee S, Velez Edwards DR, Baird DD, Savitz DA, Hartmann KE. Risk of miscarriage among black women and white women in a US prospective cohort study. Am J Epidemiol. 2013;177(11):1271–8.
Muthén LK and Muthén BO (1998–2017). Mplus User’s Guide. Eighth Edition. Los Angeles, CA: Muthén & Muthén
Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model. 2007;14(4):535–69.
Osterman MJK, Hamilton BE, Martin JA, Driscoll AK, Valenzuela CP. Births: Final data for 2020. National Vital Statistics Reports. 2022;70(17), 1–50. https://www.cdc.gov/nchs/data/nvsr/nvsr70/nvsr70-17.pdf
Osypuk TL, Slaughter-Acey JC, Kehm RD, Misra DP. Life-course social mobility and reduced risk of adverse birth outcomes. Am J Prev Med. 2016;51(6):975–82.
Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, ... & Gee G. Racism as a determinant of health: a systematic review and meta-analysis. PloS one. 2015;10(9), e0138511
Petrou S, Yiu HH, Kwon J. Economic consequences of PTB: a systematic review of the recent literature (2009–2017). Arch Dis Child. 2019;104(5):456–65.
Practice Committee of the American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012;98(5):1103–11.
Quenby S, Gallos ID, Dhillon-Smith RK, Podesek M, Stephenson MD, Fisher J, ... & Coomarasamy A. Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss. Lancet. 2021;397(10285), 1658–1667
Reno R, Hyder A. The evidence base for social determinants of health as risk factors for infant mortality: a systematic scoping review. J Health Care Poor Underserved. 2018;29(4):1188–208.
Rossen LM, Ahrens KA, Branum AM. Trends in risk of pregnancy loss among US women, 1990–2011. Paediatr Perinat Epidemiol. 2018;32(1):19–29.
Schaaf JM, Liem SM, Mol BWJ, Abu-Hanna A, Ravelli AC. Ethnic and racial disparities in the risk of PTB: a systematic review and meta-analysis. Am J Perinatol. 2013;30(06):433–50.
Shah PS, Shah J. Maternal exposure to domestic violence and pregnancy and birth outcomes: a systematic review and meta-analyses. J Womens Health. 2010;19(11):2017–31.
Sheikh J, Allotey J, Kew T, Fernández-Félix BM, Zamora J, Khalil A, ... & van Gelder M. Effects of race and ethnicity on perinatal outcomes in high-income and upper-middle-income countries: an individual participant data meta-analysis of 2 198 655 pregnancies. Lancet. 2022;400(10368), 2049–2062.
Singh GK, Stella MY. Infant mortality in the United States, 1915–2017: large social inequalities have persisted for over a century. Int J Maternal Child Health AIDS. 2019;8(1):19.
Slopen N, Shonkoff JP, Albert MA, Yoshikawa H, Jacobs A, Stoltz R, Williams DR. Racial disparities in child adversity in the US: interactions with family immigration history and income. Am J Prev Med. 2016;50(1):47–56.
Staneva A, Bogossian F, Pritchard M, Wittkowski A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on PTB: a systematic review. Women and Birth. 2015;28(3):179–93.
Strutz KL, Hogan VK, Siega-Riz AM, Suchindran CM, Halpern CT, Hussey JM. Preconception stress, birth weight, and birth weight disparities among US women. Am J Public Health. 2014;104(8):e125–32.
Stumbo SP, Yarborough BJH, Paulson RI, Green CA. The impact of adverse child and adult experiences on recovery from serious mental illness. Psychiatr Rehabil J. 2015;38(4):320.
Su D, Samson K, Hanson C, Berry ALA, Li Y, Shi L, Zhang D. Racial and ethnic disparities in birth outcomes: a decomposition analysis of contributing factors. Prevent Med Rep. 2021;23:101456.
Testa A, Jackson DB. Maternal adverse childhood experiences, paternal involvement, and infant health. J Pediatr. 2021;236:157–63.
van Daalen KR, Kaiser J, Kebede S, Cipriano G, Maimouni H, Olumese E, ... & Oliver-Williams C. Racial discrimination and adverse pregnancy outcomes: a systematic review and meta-analysis. BMJ Glob Health. 2022;7(8), e009227
van der Feltz-Cornelis C, Bakker M, van der Sluijs JVE. Four clinical profiles of adult outpatients with somatic Symptom Disorders and Related Disorders (SSRD) A latent class analysis. J Psychosom Res. 2022;156:110775.
Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health. 2019;40(1):105–25.
Wolke D, Johnson S, Mendonça M. The life course consequences of very PTB. Ann Rev Develop Psychol. 2019;1:69–92.
World Health Organization. WHO recommendations on interventions to improve preterm birth outcomes: highlights and key messages from the World Health Organization's 2015 global recommendations (No. WHO/RHR/15.16). World Health Organization. 2015
Zhang G, Srivastava A, Bacelis J, Juodakis J, Jacobsson B, Muglia LJ. Genetic studies of gestational duration and PTB. Best Pract Res Clin Obstet Gynaecol. 2018;52:33–47.
Zhang L, Mersky JP, Lee CP. Intergenerational pathways linking mothers’ adverse childhood experiences and children’s social-emotional problems. Child Maltreat. 2023;28(1):107–18.
Zuccarello D, Sorrentino U, Brasson V, Marin L, Piccolo C, Capalbo A, ... & Cassina M. Epigenetics of pregnancy: looking beyond the DNA code. J Assist Reprod Gene. 2022;39(4), 801–816
Funding
This work was supported by grants from the U.S. Department of Health and Human Services, Health Resources Services Administration (X10MC43618; X10MC33618).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by JM and CPL. The first draft of the manuscript was written by JM and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board (FWA00006171) of the University of Wisconsin-Milwaukee (14.286; 3/27/14).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent to Publish
Not applicable. Study participants were informed at the time of consent that their data would be deidentified and used for research.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mersky, J.P., Jeffers, N.K., Lee, C.P. et al. Linking Adverse Experiences to Pregnancy and Birth Outcomes: A Life Course Analysis of Racial and Ethnic Disparities Among Low-Income Women. J. Racial and Ethnic Health Disparities 11, 1741–1753 (2024). https://doi.org/10.1007/s40615-023-01647-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-023-01647-w