Abstract
This study examined how a racially and socioeconomically diverse group of caregivers of children with autism spectrum disorder (ASD) responds to national standard measures of family-centered care (FCC) and care coordination (CC) and what aspects of quality care are missing from these measures. Based on survey and interview data collected from 70 caregivers who have a child with ASD that receive services at a community-based autism clinic located in Atlanta, GA, we compared proportions of answers to FCC and CC questions to national and state representative data using chi-square analyses and contextualized our findings through a thematic analysis of qualitative interviews. Compared to national- and state-level data, the Atlanta autism clinic data had a higher percentage of participants who identified as Black, relied on public health insurance, and lived below 200% of the federal poverty line. The Atlanta autism clinic responses were significantly more positive in four measures of FCC but significantly less effective in two CC measures, including a lower reported percentage who received CC and greater reported percentage who needed extra help. Qualitative data revealed a range of positive meanings and challenges associated with FCC and identified areas of help needed beyond CC, including physical and mental health care and emotional connection, especially for low-income single Black female caregivers. Our mixed-method approach identified strengths in FCC, barriers to CC, and suggestions for developing more pragmatic questions in national surveys that address experiences of quality-of-care among low-income, racial minority families of children with ASD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Families who have a child with autism spectrum disorder (ASD) face unique challenges in navigating multiple complex systems of care due to the range and severity of symptoms and co-occurring conditions associated with ASD [1]. As such, there is an increasing focus on carefully measuring how health care is delivered to children with autism who are unique even among larger groups of children with special needs [2,3,4]. Large-scale, nationwide surveys have been used to gather quantitative data to identify how caregivers of children with ASD seek medical care, at what age they are first diagnosed, and their overall experience with providers [2, 3, 5]. Subsequently, this data has been used to compare costs, outcomes, and autism service access across the USA and to identify the importance of certain aspects of high-quality care such as family-centered care and care coordination [6,7,8,9]. However, the understanding of quality-of-care measures is limited among racially and socioeconomically diverse families who have a child with ASD.
Although the Center for Disease Control and Prevention (CDC) surveillance data from 2016 estimates that the difference in prevalence of ASD among 8-year olds is closing among white and Black children (1 in 54 compared to 1 in 55 children diagnosed with an ASD, respectively), prevalence disparities continue to persist for Hispanic children (1 in 65) and for those with lower socioeconomic status (SES) [10]. For example, population-based research in the USA indicates that prevalence of ASD is higher among higher SES groups, even within racial and ethnic groups [11]. Furthermore, low-income families who have children with ASD are less likely to have initial concerns, and receive early, continuous care, while proximal social factors like marital status and distance from clinics elevate risk for disrupted care [3, 12, 13].
Existing literature largely recognizes that children and families who face racial, ethnic, and/or socioeconomic biases likely face disparities beyond diagnostic rates, extending into differences in age at diagnosis, ability to access services, and overall quality of health care received [11,12,13,14,15,16,17,18,19]. The cumulative stress of discrimination based on race and ethnicity may also serve as an additive factor to any aspect of a disability that extend to other domains of life such as living, working, and/or educational conditions [20]. Within the clinical context, studies have found that Black and Latino parents are less likely to report that they experienced quality indicators of family-centered care, which highlights the need for research that offers a deeper understanding how families of color experience the diagnosis and treatment of ASD [19, 21]. Importantly, a few studies indicate that adequate family-centered care indicators, such as spending enough time with families or engaging parents as partners, could potentially mediate the negative health outcome effect of race and ethnicity such as the ability to access, monitor, and implement an effective ASD treatment plan [18, 22].
Qualitative data and analysis offer the ability to inform why minority and impoverished families report worse experiences and differential outcomes. Qualitative and mixed-method approaches have been implemented to better understand the underpinnings of families’ experiences that are often quantified through standard validated questionnaires [22,23,24,25]. A recent review of qualitative research on autism disparities identified interacting familial, cultural, and structural barriers, as well as gaps in the literature such as the effects of accessing autism services for low-income and single-parent households or the unequal autism services available through public health insurance [26]. Thus, qualitative research has the potential to uncover underlying social phenomenon that may explain observed disparities in quantitative data based on race, ethnicity, and/or SES, which can better inform the use of such quality measures across diverse demographic groups.
Current Study
This study is a mixed-method approach designed to answer the following exploratory research questions: (1) How does a racially and socioeconomically diverse population respond to measures of family-centered care (FCC) and care coordination (CC) compared to national- and state-level data? and (2) What are the experiences of and barriers and facilitators to FCC and CC among racially and socioeconomically diverse populations? The goals of this study are to better understand the social and structural context that inform the reporting of quantitative quality-of-care measures, and to offer suggestions on how to develop and design questions that more appropriately measure the contours of quality-of-care for underserved minority children with autism, and ultimately improve services.
Methods
We conducted a convergent mixed-method study, which is a design that blends quantitative and qualitative data together as they are both gathered and analyzed at the same time [27]. The strengths of this approach allowed us to converge closed and open-ended questions and conduct statistical and thematic analysis across different sets of data [27]. For this study, we utilized three sets of data: (1) quality-of-care survey responses from caregivers whose children receive services at an urban autism clinic on FCC and CC measures; (2) open-ended interview responses collected concurrently to FCC and CC measures from the same caregivers; and (3) National Survey of Children with Special Health Care Needs (NS-CSHCN) demographic, FCC, and CC data from 2009 to 2010 [2, 28].
Participants and Procedures
Individuals who participated in the quality-of-care survey and interview were recruited from the autism clinic at Hughes Spalding Hospital of Children’s Healthcare of Atlanta, a public non-profit hospital in downtown Atlanta, GA, that serves patients who rely primarily on Medicaid health insurance. The autism clinic was established in 2002 to respond to the needs of low-income minority children with ASD who had limited access to diagnostic and/or therapeutic services. At a typical initial visit to the clinic, children and their caregivers receive services from an interdisciplinary team, including a developmental pediatrician; a nurse practitioner; an occupational therapist; a speech therapist; and as needed, a nutritionist, social worker, and education consultant. The clinic operates 3 days a month and offers diagnostic and referral services as well as medical management.
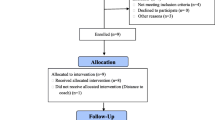
Study participants included English-speaking primary caregivers who were receiving services at the autism clinic for their children at least one time before they participated in the study. Caregivers were recruited between September 2016 and December 2018 based on selective referral by the developmental pediatrician running the clinic. Eighty-six caregivers were recruited and 70 were ultimately surveyed and interviewed (Table 1). Caregivers who agreed to participate were administered a structured survey and responded to open-ended questions about their survey responses either in person (N = 20) or over the phone (N = 50). The mean length of the survey and interview was 60 min, and all the participants were compensated with a $55 gift card. This study received IRB approval from Children’s Healthcare of Atlanta (#16-099), and all the participants were given a pseudonym in the presentation of our findings to protect their identity.
Study Data
The quantitative data consisted of self-reported answers to a survey that was designed to document extensive demographic data and measure quality-of-care experienced at the autism clinic. The survey questions were derived from the 2009–2010 NS-CSHCN, which is a validated survey administered by the CDC [2, 28]. At the time of this study’s design, the 2009–2010 NS-CSHCN was the most updated survey with available data for analysis, although similar surveys continue to be conducted by the CDC. For this study, we are reporting on participant demographics and self-reported measures related to the quality of FCC and CC. Demographic characteristics were based on caregiver participant report including age at diagnosis, current age of child, household income, mother’s education, insurance status, and child’s race/ethnicity. To better understand the quality of FCC during the first visit to the autism clinic, the prompt and response options on the FCC portion of the survey were changed from the NS-CSHCN questions, which asks about the experience of FCC over the last 12 months using a Likert scale, to questions that ask about the first experience at the clinic using a yes or no response. We made these changes since the survey was designed in conjunction with autism clinic staff who felt the first visit was the most significant time of care we were assessing. We also wanted to keep the responses the same to limit the complexity of the survey and burden on our participants. Similarly, the prompt to the CC measures of the survey were designed to assess the first visit (as opposed to the last 12 months) but we used the same response options as the NS-CSHCN (e.g., yes, no, don’t know, or refuse to answer). A total of 78 questions were included in the survey, with this analysis focusing on a specific subset of 10 NS-CSHCN questions on family-centered care and care coordination.
To compare our quantitative survey data, we used national and state levels of FCC and CC items from the publicly available 2009–2010 NS-CSHCN dataset, inclusive of data collected from July 2009 to March 2011 and specified to children with a diagnosis of autism [28].
The qualitative data consisted of responses to follow-up questions that were asked throughout the autism clinic survey. For this study, we analyzed qualitative data provided by the caregiver participants who were asked to elaborate on their survey responses to FCC and CC measures. For example, we asked, “can you elaborate your response or give me an example based on your experience?” The responses to the entire survey and open-ended questions were audio-recorded, transcribed, and uploaded into a qualitative research software [29].
Quantitative Data Analysis
To compare the demographic data, the means and 95% confidence intervals were calculated for continuous variables and income was used to calculate relationship to 200% of the Federal Poverty Line based on federal guidelines for the poverty line for a participant’s reported household size [30]. This demographic comparison allowed us to characterize how our clinic sample represents a distinct subset of the autism population typically underrepresented in large-scale surveys (Table 1).
A statistical comparison of responses to FCC and CC measures was conducted to identify possible disparities and differences between the autism clinic population compared to the state and national sample, which we hypothesized may be likely given the level of complexity involved in delivering family-centered care and aiding in care coordination for clinic patients. All NS-CSHCN comparative analyses were completed using SAS complex survey design analyses and appropriate weights as advised by survey documentation guidelines to obtain nationally and state representative proportions of demographic variables and survey questions of interest [31]. Proportions of answers to family-centered care and care coordination questions from the autism clinic were compared to the national and state representative standards using chi-square test of proportions; for questions where expected values were less than five, the chi-square exact test of proportions was used, with p < 0.05 as the significance level for both tests. Where response options differed in FCC questions due to the clinic focusing on the first visit, positive responses of “yes” were compared to national responses of “usually” or “always,” which is a conventionally collapsed response category for dichotomous analysis as done in other studies using NS-CSHCN data [18, 22]. Quantitative data analyses were performed using SAS Software version 9.4 [32]
Qualitative Data Analysis
We conducted a thematic analysis of qualitative data collected from open-ended follow-up questions to the structured survey to identify central themes related to the strengths, weaknesses, barriers, and facilitators to FCC and CC. Following the steps in the coding process of qualitative data [27], we read all the transcriptions, identified salient ideas, and then carefully analyzed all the interviews for key themes and subthemes until we reached saturation. A preliminary codebook was developed and refined after multiple data inspections by the principal investigator who collected all the data (author 3). We used HyperRESEARCH to aid in coding segments of qualitative data to specific themes and categories (Table 3) and in writing detailed memos to capture the data conceptually [29]. All the data was coded by the principal investigator.
Validity
The principal investigator conducted all the interviews and coded the qualitative data for this analysis. She did not know the participants before conducting the interview and only met them at the time of recruitment. We minimized bias and established validity of the data generated from the closed- and open-ended responses to the FCC and CC measures through triangulation, a common validity procedure that converges multiple and different sources of information to form themes or categories in a study [33]. In addition to the survey responses to FCC and CC, the open-ended responses to these measures were also contextualized with the extensive demographic data collected, the detailed memos taken after each survey and interview, and the fieldnotes taken during prolonged participant observation at the autism clinic from September 2016 through December 2018 (approximately 250 h). The post survey/interview memos highlighted the primary concerns of the caregiver, strengths and weaknesses of the autism clinic, and areas of need to access autism services. The detailed ethnographic fieldnotes helped the principal investigator continuously document the different processes of FCC and CC that corresponded to survey responses and categories saturated in the thematic analysis of the interview data. The participant observation also helped the PI establish and build trust with the clinical team; nursing staff; affiliated clinical support; and most importantly, the caregivers who utilized the autism clinic for their child. This enabled a more credible account from the study participants of their experience of FCC and CC. The triangulation of these different sources of data allowed us to validate how accurately the thematic accounts we identified in the FCC and CC open-ended responses represented participants’ realities and credibility of the observed and measured quality-of-care processes [33].
Results
Quantitative Findings
The total study sample size included 70 participants and differed demographically from the national- and state-level samples in several ways (Table 1). The study had more participants who identified as Black or African American (72.5% vs. national: 11.3%, state: 24.1%) in addition to having a higher percentage of solely publicly insured patients (61.4% vs. national: 32.7%, state: 31.3%) and those below 200% of the federal poverty line (64.3% vs. national: 40.0%, state: 41.3%). Additionally, there were fewer study participants who identified as married (42.9% vs. national: 69.4%, state: 75.2%). Finally, overall, autism clinic patients generally had a lower mean age of first diagnosis (4.9 years, 95% CI: 2.4, 5.5) compared to the national- (6.4 years, 95% CI: 5.9, 6.9) and state-level data (6.8 years, 95% CI: 4.7, 8.9).
Results on seven items of FCC were reported and compared to national- and state-level data (Table 2). Of these seven questions, autism clinic data significantly differed on four items, including more frequent reports by caregivers that providers at the autism clinic spent enough time (91.4% vs. national: 67.4%, state: 78.9%), listened carefully (98.6% vs. national 80.0%, state: 91.0%), provided specific information needed (94.3% vs. national: 67.3%, state: 80.9%), and discussed a range of options for their child’s treatment (77.1% vs. national: 67.4%, state: 76.5%).
Results on three items of care coordination were reported and compared to national and state-level data (Table 2). Two of these items significantly differed from both national and state reports, including a lower proportion of caregivers who reported that providers at the autism clinic helped them coordinate care (29.4% vs. national: 57.1%, state: 75.3%) and a higher proportion reported the need for extra help in arranging or coordinating services (64.7% vs. national: 40.1%, state: 33.9%).
Qualitative Findings—Family-Centered Care
The responses to follow-up and open-ended questions to FCC survey items demonstrate that the meanings attached to spending enough time, listening carefully, and providing specific information that was needed during the visit are more nuanced and overlap with one another (Table 3). These three measures were the focus in this analysis because they were among the top three positive responses that were significantly higher compared to both national- and state-level means for the same measures. We also highlight both the strengths and the challenges of these processes of FCC.
Spending Enough Time
First, caregivers who felt that enough time was spent during their first visit with the autism clinic indicated that the visit was thorough, allowed all questions to be answered, and involved a team of professionals. For example, Lydia, a married mother of three children, one diagnosed with ASD, felt that enough time was spent to really get an understanding of her son’s situation. She stated,
They spent a good amount of time. I did feel it was beneficial because it felt like they were actually taking the time to understand what the issues were.
The caregivers also acknowledged that not only was the time spent sufficient, but it allowed for a two-way conversation of understanding to be accomplished. This was very important to caregivers as it allowed for ample time to ask questions. The length of time was also viewed positively within the context of being able to see multiple clinical providers in one visit. For example, Shauna, a single mother with two teenage boys, one diagnosed with ASD, appreciated the amount of time spent during her son’s initial visit and viewed her interactions with different providers as an essential component. Shauna especially appreciated how the providers worked together to develop a plan of action for her and her son.
Listening Carefully
Relative to other items of FCC, the ability of the providers at the autism clinic to listen carefully to caregiver’s needs and concerns was reported most frequently as “yes” by the respondents. This is reflected in the caregiver’s own words to mean that the clinic providers did not rush the appointment, took a genuine interest in all their questions, and valued the expertise they brought to the conversation. For example, Sharon, a single mother of four children, one diagnosed with ASD, felt that a key component of listening was the feeling that they were never rushed through the appointment. This was particularly important to Sharon, because as she states it, they are “dealing with your child’s mental health at this point.”
Creating an environment that allowed for the time and opportunity to ask questions and express concerns to providers who are willing to listen established not only a safe space for caregivers and their children but also signaled that caregiver input was valued. For example, Erika who is married and had two daughters with special needs, one with ASD, felt the providers at the autism clinic listened to what parents had to offer. She stated,
They’re really good about listening …and helping you coordinate what’s best for your child, based on what they know as clinicians, and what you know as a parent… So, I feel comfortable voicing my concerns. I feel like I’m being listened to.
One other element of listening was the autism clinics’ ability to provide referrals or recommendations to issues that were the most concerning to the caregivers, whether it be addressing sleeping or eating issues, behavioral concerns at school, or finding other appropriate providers like a dentist. Pamela, for example, who is married with five children and has an 11-year-old diagnosed with ASD recalled how the clinic went beyond what she was expecting during her first visit, including “Little things that most physicians don’t pay attention to, they really homed in on.”
These responses indicate that listening processes at that autism clinic involved a two-way interaction between the providers and the caregivers, a genuine interest in the primary concerns of the caregiver, and a safe and open environment that allowed caregivers to voice their concerns. In essence, from the perspective of the caregivers, the autism clinic providers asked a lot of questions and carefully listened to parents in order to get a sense of not only the specific needs of the child but also the family situation before setting a comprehensive plan in motion.
Providing Needed Information
At the end of each visit, caregivers are given many different kinds of information depending on the primary concerns of the caregivers and the needs identified by the providers after the evaluation. This ranged from a diagnosis of ASD and a thorough and understandable explanation of symptoms associated with it, to a list of referrals for therapy or treatment, as well as other kinds of services that the children and/or caregivers needed.
For example, Felicia, a single grandmother who was the primary caregiver of her 2-year-old grandson with ASD, felt more assured and less alone after the clinic diagnosed her grandson and provided pertinent information as a result of their first visit. She stated,
I left with the diagnosis and …. I felt like they cared …. and I felt that I was given a lot of good information and some tools to use…. I felt like I wasn’t really alone in this.
The caregivers also noted that the range of referrals were not only limited to the child with ASD but also focused on the needs of the caregivers. As Sylvia, a single mother with one child diagnosed with autism, recalled,
Even though [the appointment] wasn’t for me, the doctor was like, “this is so much about you too because [your son] is with you on a day-to-day basis.”
Thus, the clinic offered information that was useful for the child with ASD and their caregivers such as information to connect with other parents who were going through the same challenges or resources to access respite care. Family-centered resources like these helped caregivers not feel so alone in this journey, which was especially important for single parents.
Caregivers were also appreciative that the clinic explained everything in simple terms, something that is a challenge especially for ASD, which has multiple symptoms, trajectories, and treatments. For example, Kiara, another single grandmother, who took care of her adolescent daughter and three young grandchildren, one who was diagnosed with autism, was very appreciative of the way the information was communicated. She stated,
[The doctor] gave me like everything that he wanted him to do and broke everything down [about autism] to me….. It’s just not one thing you diagnose; you have a high and a low.
The resources provided were also directly related to the primary concerns of the parent, which for this sample often meant issues associated with limited resources like insurance coverage; income; housing; transportation; and, in some cases, legal or child protective services. Thus, the range of resources provided to families spread out to other areas of life beyond the immediate needs of the child with ASD.
Limitations of Family-Centered Care
While these three categories (e.g., spending enough time, listening carefully, and providing needed information) ranked high in positive responses, these family-centered practices also evoked a lot of overwhelming emotions by the parents. First, the significant amount of time spent during the initial clinic appointment made it challenging for children to stay occupied over the duration of several hours and engage with multiple clinical providers. Caregivers also discussed that although they agreed that enough time was spent during the initial visit, they also experienced a lot of repetitive questions being asked by the different providers. For example, Patricia, a single mother to a 4-year-old boy diagnosed with ASD, felt that the clinic spent enough time, but found it “very tiring” to be asked the same questions over and over again, every time a new clinical provider came into their exam room. Patricia also had a hard time keeping her son occupied during the 3-h duration of the visit in such a small room. We should also note that the size of the exam rooms in the autism clinic were designed for individual patients and not for families, which is another limitation in FCC.
Second, the amount of information received was in several cases a stressful experience especially for caregivers who were not prepared for an autism diagnosis. For example, Allison, a divorced mother of two children, one diagnosed with autism, recalled how overwhelmed she was during her initial visit. She stated,
It was so much information for somebody like me… It was overwhelming because you have all those people come in and trying to explain stuff to you and you don’t know. That was my first time being in a special-needs world. I had no idea what to expect.
Allison recalled that she also came to the point where she could no longer process the information anymore, especially the complexity of the autism diagnosis and the range of therapies she was going to have to seek for her son.
Qualitative Findings—Care Coordination
The survey data showed that significantly fewer caregivers reported that they received any type of care coordination from the autism clinic compared to federal- and state-level means. Furthermore, significantly fewer caregivers in this study received additional help from anyone else beyond the autism clinic (Tables 2 and 3). This finding reflects the limited resources outside of the clinic either in the hospital or the community that are available to caregivers to help coordinate their child’s care. In the survey, we defined care coordination as “anyone who helps make sure that their child gets all the medical, educational, therapeutic, or social services that he/she needs, that doctors and therapist share information, and that these services fit together and are paid for in a way that works for caregivers.”
Initial and Continued Path Toward Services
Care coordination provided from the autism clinic typically did not move beyond providing a list of referrals, which caregivers used to find needed services. One caregiver, Dominique, who was separated at the time of the interview and managed the care of her son with little help from her son’s father, recalled the minimal care coordination she received after her first visit to the autism clinic. She stated,
I had to contact Amerigroup to find out what services where in my area; what offices to go to. The only thing [the clinic] told me was to …. do the evaluation for his hearing and his speech evaluation. So, I needed that first, [before] I can start any services.
Like many participants, the autism clinic offered Dominique an initial path toward services providing mainly referrals to the types of evaluations and/or services needed to get caregivers started in the right direction. This may consist of a list of referrals for behavioral, occupational, or speech therapy, or specific recommendations to get a psychological evaluation, or in some cases a prescription for medication to address associated behavioral, mental health, and physical symptoms. However, the responsibility to follow-up on these referrals was left mainly to the caregivers alone.
The social and economic situation these caregivers faced also made the challenge and responsibility of coordinating care more difficult. As Makayla, who is a single mother of a 4-year-old boy diagnosed with autism and navigates autism services through Medicaid boundaries, stated,
They just gave me information and I use what was given to me…. (extra help) would be nice, but I never really thought about it that way…because I’m responsible for him, that’s what I’m supposed to do.
The responsibility Makayla places on herself is situated in the fact that she does not receive any help from her immediate family. As a single parent, she views her situation as a mother who takes on full responsibility to “work and make a living” for her family while at the same time continues her education to improve her future income potential. The social and economic context of Makayla’s life makes it very challenging to meet the demands of coordinating care for her son, which usually falls short because of her demanding schedule. Like Makayla, many of our respondents viewed it as their responsibility to make the connections between different providers, and in the process sacrificed their own personal lives (health, employment, etc.) to meet the needs of this demanding situation.
Help Needed
Another component of measuring care coordination in the NS-CSHCN is whether caregivers needed extra help arranging or coordinating their child’s care. Our sample of caregivers reported that that they needed significantly more help in this area compared to national- and state-level means. When asked to elaborate, the caregivers described that they needed help finding services for their child, whether it be certain therapies, special educational services, or appropriate daycare. Above all, these families needed help connecting these different services to meet the needs of their children; a realization that was especially evident for caregivers who were new to systems of care in Georgia. For example, Erika, who we mentioned earlier, reflected how difficult it was to coordinate both of her daughter’s care when she moved to Georgia. She stated, “In Maine, you don’t go to your services, they come to you. So, there’s kind of no issue of figuring out how to coordinate so many different appointments into a week.” Since moving to Georgia, Erika described her experience as “a whole new ballgame” that “feels really overwhelming,” mainly because services are not centrally located, difficult to access, and very limited.
The lack of services in certain areas of Atlanta also prompted parents to respond that they needed help coordinating care, simply because the different therapies they needed were not available where they lived. For example, Sharise, a single parent of four children with a 14-year-old daughter diagnosed with ASD, described her need for help in the following way,
I know they are trying their best, but there so many resources on that side and then on our side of town, the south side, there’s not a lot of resources. I feel like sometimes we are getting left behind because we are not able to get that information and I have to try to find it on my own.
Several caregivers mentioned scarcity of resources with regard to finding daycare or afterschool programs for their children and indicated that they simply could not find these types of services for children with special healthcare needs, which had both personal (emotional and physical stress on caregivers) and economic (unable to work after school hours, etc.) consequences.
The second most common request for help expressed by the caregivers was the need for self-care and emotional connection. Typically, this is not the core part of the definition of coordinating care, but when the primary caregiver is simultaneously the primary care coordinator, the need for respite and emotional connection with others needs to be part of the equation, otherwise caregivers have the potential for neglecting their own needs. For example, Alicia, a caregiver to five children, one diagnosed with ASD, was suffering from a painful auto-immune disorder when we met. She stated, “I put myself on the back burner all the time and if I am sick today, I am going to just have to deal with it and try and do what I have to do and take care of my daughter.”
Caregivers also needed emotional connection with other parents who are experiencing similar situations. One single mother, Melinda, who had twins diagnosed with ASD, felt extremely isolated in her situation and needed help connecting with other people. She stated, “I do need the setting where I’m talking to somebody that knows what I’m going through because I don’t have anybody to discuss that with.” Other caregivers expressed this emotional and supportive need, an opportunity to link up with other parents especially after their child received an initial diagnosis.
Discussion
This study offers important insights into a known gap in research by offering a mixed-method analysis of quality-of-care measures and experiences in an autism clinic composed of primarily low-income, Black, single-parent households. The results demonstrate that self-reported receipt of family-centered care and care coordination for the autism clinic differ from the national and state samples, while the qualitative results underscore how current measures may fail to capture the experiences of households who lie at the intersection of poverty, racial discrimination, and inadequate public resources.
First, our study should be framed by the demographic differences in the caregivers we surveyed with those sampled by the NS-CSCHCN. In comparison to their national- and state-level counterparts, our sample was predominantly African American, accessed healthcare through public insurance, and from single-parent households. Our caregivers had a similar distribution of education level as the national and state survey’s distribution. These differences and similarities in demographics carry implications for the interpretation of our results, particularly highlighting how our sample addresses caregivers at the intersection of many socioeconomic factors including poverty, fewer familial resources, and the various impacts of race. Of note, nine caregiver participants identified as grandparents, while the other 61 identified as the child’s mother. Understanding the social and economic context of this demographic is important since a high percentage of female African Americans 45 years and older are raising grandchildren (7%) and, compared to Black non-caregivers, are more likely to be less educated, living in poverty and receiving public assistance [34]. Another important comparison was that the mean age that the child was first told of an autism diagnosis was actually younger than the national- and state-level average, which may be on track with previous study results that document rates and pathways to diagnosis for minority and underserved populations are improving [10, 12]. It also underscores the importance of community-based clinics that offer diagnostic services to underserved minority populations.
Insights on Family-Centered Care and Care Coordination Experiences
The quantitative results of our study indicate that there are significant differences in the reported receipt of family-centered care when compared to the national- and state-level results of the NS-CSHCN. The caregivers surveyed were significantly more likely to report that providers spent enough time with them, listened carefully to them, gave them the specific information needed, and discussed a range of options for their child’s treatment. In contrast, the caregivers we surveyed largely reported that they did not receive help from the autism clinic with care coordination and needed extra help in coordinating their child’s care. While the clinic staff are experienced in serving children with ASD and their families and provide good diagnostic and referral services, a major limitation is the absence of a dependable infrastructure that includes coordination of care. This restriction is a factor of the incomplete resources available in the hospital where the clinic is based, as well as inadequate community resources. The existing community-based family support groups, including Parent to Parent of Georgia, do provide some support to families but there is no dedicated coordinator to connect the families directly with the needed services, nor to monitor the uses and efficiency and effectiveness of the community services.
The qualitative results help us to further contextualize our quantitative findings to confirm that the family-centered care measurements did in fact capture the experience of the participants: that they felt heard and appreciated the time spent with multiple providers who shared a genuine interest in their child. Importantly, these aspects of family-centered care empowered caregivers to feel capable of asking questions and voicing concerns. Our results also highlight that while many caregivers rated these family-centered care measure positively based on their experiences, there is a balance that needs to be made between having enough time for the providers to evaluate, understand, and develop a plan of action, with the time caregivers and their children are able to manage in one visit. However, the alternative to a single multi-disciplinary visit is to have multiple visits to see the different providers, which could potentially be more straining on families and their children with autism and limit continuity of care. The amounts and type of information provided also has to be carefully calibrated with caregiver’s knowledge of ASD, level of acceptance, and emotional consequences of being told their child has autism. As we observed in the clinic, this is also where cultural sensitivity becomes essential, as well as the appreciation, understanding, and comprehension of the family’s situation and health literacy levels. Although we did not measure the likelihood of receiving FCC by race or ethnicity, 72.5% of our sample identified as Black or African American, which would suggest that our study results differ from other studies that show Black families with ASD are less likely to receive family-centered care [21, 22], which can significantly affect therapeutic outcomes [18, 35]. Within this context, the positive FCC measures also suggest mutual respect and acceptance between the autism clinic providers and the diverse caregiver population. This is certainly an area that deserves future investigation.
The positive findings of FCC identified in both the survey and interview data might also be due to the differences in NS-CSHCN data that asks caregivers about FCC and CC generally, whereas our study generated data from a specialty autism clinic, that might dedicate more time to spend with families, ask thorough questions, and identify specific needs. The autism clinic also has a long-term dedicated team, including a developmental pediatrician and a pediatric nurse practitioner who have been part of the clinic since 2002, as well as a speech pathologist and occupational therapist. These long-term relationships with caregivers offer the continuity of care that families need over the duration of their child’s development, especially for children with autism because of their constant changing and shifting needs and priorities. Further, the multi-disciplinary team approach allows for a comprehensive initial visit, which typically involves assessment, diagnosis, and referrals for appropriate therapeutic, educational and social interventions. The reported earlier age of diagnosis in our sample in comparison to the national and state-level means also suggests that the existence of the clinic over the last two decades has raised awareness of the clinic and encouraged earlier referrals.
The qualitative analysis of experiences with care coordination also offered a complex and multi-layered description of disparities that are evident in receiving autism services based on race, ethnicity, and socioeconomic status [26, 36, 37]. We learned that caregivers in our study had to do most of the care coordination of their child’s care on their own, which was often inhibited by caregiver time, financial resources, knowledge, and access to different services as similarly noted in previous research [38, 39]. Perhaps most revealing were the types of help needed that the caregivers expressed in addition to help with coordinating care, namely social and emotional support. This is not surprising given the plethora of research that identifies significant effects on maternal psychological wellbeing due to the frustration and stress of navigating systems of care [1, 40] and the need for respite care [41].
Taken together, our findings offer insight into specific ways in which we can begin to take into account compounding social and economic factors that shape the experience of family-centered care and care coordination. First, although caregivers in our study indicated that enough time was spent during their initial visit to the autism clinic, the way in which caregivers perceive time needs to be further explored. Important time factors highlighted by caregivers included whether they have daycare support for other children, flexible employment schedules, or other logistic preparations needed to dedicate a significant amount of time during initial and/or follow-up visits, findings that align with priorities identified in previous studies [18, 42]. Furthermore, questions about experiencing a multi-disciplinary team approach, which our data demonstrates can be both beneficial and overwhelming, can offer better insight on how to make the best use of time, especially for caregivers who experience multiple resource constraints.
Our data also suggests that an oversimplified view of care coordination services is counterproductive, both in the measurement and the delivery of the help that caregivers of children with autism need. An autism diagnosis often comes with multiple referrals that are dependent on the specific and unique needs of each child, the social and economic resources available to families, and the availability of services in relation to where people live [43]. This variation in the needs and severity of the individual child requires care coordination to be highly personalized, and even the frameworks provided by the American Academy of Pediatrics note that effective care coordination should be viewed as expansive and covering multiple systems and societal structures, making it even more difficult to achieve for children with autism who face multiple structural, familial, and healthcare barriers [38, 43, 44]. In fact, previous work notes that parents of children with autism historically have higher rates of dissatisfaction with care coordination services and more unmet care needs than parents of children without ASD [45, 46]; our study suggests this previously noted disparity is further amplified for our caregivers who have fewer resources to navigate the complex autism care network. Furthermore, the lack of care coordination available beyond the in-house clinical services demonstrates the need to integrate more care coordination services into the autism clinic as well as extending to other clinical services in the hospital.
Insights on Measurement of Care Coordination
The questions from the NS-CSHCN attempt to quantify the reception of care coordination services by simply using the term “care coordination,” but based on the caregiver’s open-ended responses, many participants viewed this term only in the context of receiving referrals. It was not clear that patients expected or understood that support can be provided beyond making referrals, extending to tracking the outcomes of those referrals, developing communication between the providers of those services, and facilitating transitions in their child’s care [44]. Our qualitative responses demonstrate that the standard questions may assume a scope of care coordination that families are not necessarily aware of, leading us to suggest that further care coordination questions should address specific components of care coordination, in particular social, economic and family resources, as well as geographic location of autism services.
The standard care coordination questions fail to assess the pragmatic issues that families face that often lead to care coordination failure, in particular for our families who face layers of inequity. We suggest asking questions on the geographic and financial feasibility of referrals to multiple services and the practicality of having transportation to those services. How far, on average, are services from our caregiver’s home and work? How are families transporting their child to services? What is the flexibility of the caregiver’s work schedule and what format of services would blend following optimal treatment recommendations and feasibility for the family? Questions could ask families directly about any challenges they face in familial and social support, in an effort to better tailor recommendations. Furthermore, quality assessments of care coordination should focus on how useful referrals are and how often resources recommended were used by families. Assessing the context in which care is coordinated is even more vital for caretakers who face multiple barriers to autism services.
The final care coordination question that our study highlighted was the high number of caregivers in our sample who indicated a greater need for help with their child’s autism care. We suggest that care coordination questions should follow-up to ask what kind of help is needed. In the case of our particularly low-resourced families who were trying to navigate challenges on multiple fronts, the caregivers in our study often reported a need for emotional and social support. In the past, the autism clinic in fact did have a parental support team member who was part of the clinic, but this position was lost because of a lack of funding. By including a question designed to understand the type of help needed, providers and systems can better assess and legitimize the need for interventions that may not seem valuable to other stakeholders.
Study Limitations
Our study has several limitations. First, this is a cross-sectional analysis of data from one clinic, and it is limited by the use of a convenience sample of caregivers who were able to participate in a lengthy survey and interview. Additionally, our data was collected from 2016 to 2018, and compared to the national sample from 2009 to 2010, leading to a comparison of responses across two different time periods. Second, the unique attributes of the autism clinic and the patients they serve make it hard to generalize our findings. In addition, for the purposes of clinic usability, our question prompt and response options were slightly modified to focus on the first patient experience at the autism clinic versus the 12-month period specified by the national survey questions. However, the similarity of the question structure still provides an opportunity to compare the autism clinic to national- and state-level data. Third, quantitatively, the sample size was insufficient to perform statistical analysis of the differences of FCC and CC based on race and/or SES. However, the quantitative comparison between the autism clinic using the same FCC and CC measures with national and state levels provides an important initial comparative analysis. Finally, the data relied on caregiver report only without correlation with medical record data, which could provide insight into complexity of each child’s care coordination and number of referral services recommended.
Conclusions
The autism clinic we examined was designed to meet the needs of underserved families in Georgia, who historically have struggled to access diagnostic and therapeutic services for autism [47]. Our results support that providing community-based autism services that directly serve low-income and racial and ethnically diverse families in an urban center can provide beneficial access to a family-centered, multi-disciplinary diagnostic service. But this study also underscores that to bring family-centered care beyond the diagnostic phase into prioritizing effective receipt of treatments and services, we must more effectively assess and address the multi-level and complex layers of inequity within care coordination of different services that families face. Although the autism clinic we evaluated demonstrates the strengths (and potential) of what quality family-centered care can look like, the limitations in care coordination highlight systemic inequities within the hospital system where the clinic is based, within the communities where services are lacking, and within a healthcare delivery system that systematically limits access to services for low-income and predominantly minority populations [26, 38]. These structural inequities are part of a larger history of various forms of racism that affect health, such as racial segregation and the production of the concentration of poverty, social disorder, and social isolation, which can have long-standing negative impacts on accessing medical, educational, and material resources [48]. We are hopeful that further research into delivering family-centered care and care coordination to families who have an excess of challenges and priorities to negotiate will reveal innovative and more accurate needs assessments that can be utilized as clinics and health systems build more comprehensive and equitable models for autism care.
References
Karst JS, Van Hecke AV. Parent and family impact of autism spectrum disorders: a review and proposed model for intervention evaluation. Review Clin Child Fam Psychol Rev. 2000;15:247–77. https://doi.org/10.1007/s10567-012-0119-6.
Bramlett MD, Blumberg SJ, Ormson AE, George JM, Williams KL, Frasier AM, et al. Design and operation of the National Survey of Children with Special Health Care Needs, 2009-2010. Vital Health Stat 1. 2014;57:1–271.
The Child and Adolescent Health Measurement Initiative, Johns Hopkins Bloomberg School of Public Health. Experience matters: a view into the health and wellbeing of US children and families with autism spectrum disorder (ASD). 2016. https://childhealthdata.org/docs/default-source/cahmi/asdchartbookfinal.pdf?sfvrsn=2. Accessed 23 May 2020.
Vanegas SB, Abdelrahim R. Characterizing the systems of support for families of children with disabilities: a review of the literature. J Fam Soc Work. 2016;19:286–327. https://doi.org/10.1080/10522158.2016.1218399.
Benevides TW, Carretta HJ, Lane SJ. Unmet need for therapy among children with autism spectrum disorder: results from the 2005-2006 and 2009-2010 National Survey of Children with Special Health Care Needs. Matern Child Health J. 2016;20:878–88. https://doi.org/10.1007/s10995-015-1876-x.
Austin J, Manning-Courtney P, Johnson ML, Weber R, Johnson H, Murray D, et al. Improving access to care at autism treatment centers: a system analysis approach. Pediatrics. 2016;137:S149–57. https://doi.org/10.1542/peds.2015-2851M.
Buescher AVS, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014;168:721–8. https://doi.org/10.1001/jamapediatrics.2014.210.
Christon LM, Myers BJ. Family-centered care practices in a multidisciplinary sample of pediatric professionals providing autism spectrum disorder services in the United States. Res Autism Spectr Disord. 2015;20:47–57. https://doi.org/10.1016/j.rasd.2015.08.004.
Zhang W, Baranek G. The impact of insurance coverage types on access to and utilization of health services for US children with autism. Psychiatr Serv. 2016;67:908–11. https://doi.org/10.1176/appi.ps.201500206.
Maenner MJ, Shaw KA, Bak J, Washington A, Patrick M, DiRienzo M, et al. Prevalence of autism spectrum disorder among children aged 8 years-autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveill Summ. 2020. https://doi.org/10.15585/mmwr.ss6904a1.
Durkin MS, Maenner MJ, Baio J, Christensen D, Daniels J, Fitzgerald R, et al. Autism spectrum disorder among US children (2002-2010): socioeconomic, racial, and ethnic disparities. Am J Public Health. 2017;107:1818–26. https://doi.org/10.2105/AJPH.2017.304032.
Bishop-Fitzpatrick L, Kind AJH. A scoping review of health disparities in autism spectrum disorder. J Autism Dev Disord. 2017;47:3380–91. https://doi.org/10.1007/s10803-017-3251-9.
Kalb LG, Freedman B, Foster C, Menon D, Landa R, Kishfy L, et al. Determinants of appointment absenteeism at an outpatient pediatric autism clinic. J Dev Behav Pediatr. 2012;33:685–97. https://doi.org/10.1097/DBP.0b013e31826c66ef.
Constantino JN, Abbacchi AM, Saulnier C, Klaiman C, Mandell DS, Zhang Y, et al. Timing of the diagnosis of autism in African American children. Pediatrics. 2019;146:e20193629. https://doi.org/10.1542/peds.2019-3629.
Bilaver LA, Havlicek J. Racial and ethnic disparities in autism-related health and educational services. J Dev Behav Pediatr. 2019;40:501–10. https://doi.org/10.1097/DBP.0000000000000700.
Daniels AM, Mandell DS. Explaining differences in age at autism spectrum disorder diagnosis: a critical review. Autism. 2014;18:583–97. https://doi.org/10.1177/1362361313480277.
Longtin SE, Principe GM. The relationship between poverty level and urban African American parents’ awareness of evidence-based interventions for children with autism spectrum disorders: preliminary data. Focus on Autism and Other Dev Disabl. 2016;31:83–91. https://doi.org/10.1177/1088357614522293.
Magnusson DM, Mistry KB. Racial and ethnic disparities in unmet need for pediatric therapy services: the role of family-centered care. Acad Pediatr. 2017;17:27–33. https://doi.org/10.1016/j.acap.2016.06.010.
Zuckerman KE, Mattox KM, Sinche BK, Blaschke GS, Bethell C. Racial, ethnic, and language disparities in early childhood developmental/behavioral evaluations: a narrative review. Clin Pediatr. 2014;53:619–31. https://doi.org/10.1177/0009922813501378.
Williams DR. Stress and the mental health of populations of color: advancing our understanding of race-related stressors. J Health Soc Behav. 2018;59:466–85. https://doi.org/10.1177/0022146518814251.
Magana S, Parish SL, Son E. Have racial and ethnic disparities in the quality of health care relationships changed for children with developmental disabilities and ASD? Am J Intellect Dev Disabil. 2015;120:504–13. https://doi.org/10.1352/1944-7558-120.6.504.
Montes G, Halterman JS. White-black disparities in family-centered care among children with autism in the United States: Evidence from the NS-CSHCN 2005-2006. Acad Pediatr. 2011;11:297–304. https://doi.org/10.1016/j.acap.2011.02.002.
Bromley J, Hare DJ, Davison K, Emerson E. Mothers supporting children with autistic spectrum disorders-social support, mental health status and satisfaction with services. Autism. 2004;8:409–23. https://doi.org/10.1177/1362361304047224.
Hodgetts S, Nicholas D, Zwaigenbaum L, McConnell D. Parents’ and professionals’ perceptions of family-centered care for children with autism spectrum disorder across service sectors. Soc Sci Med. 2013;96:138–46. https://doi.org/10.1016/j.socscimed.2013.07.012.
Pearson JN, Meadan H, Malone KM, Martin BM. Parent and professional experiences supporting African-American children with autism. J Racial Ethn Health Disparities. 2020;7:305–15. https://doi.org/10.1007/s40615-019-00659-9.
Singh JS, Bunyak G. Autism disparities: a systematic review and meta-ethnography of qualitative research. Qual Health Res. 2019. https://doi.org/10.1177/1049732318808245.
Creswell J, Creswell J. Research design: qualitative, quantitative, and mixed methods approaches. 5th ed. Los Angeles, CA: Sage; 2018.
Centers for Disease Control and Prevention National Center for Health Statistics. (2011). 2009-2010 National Survey of Children with Special Health Care Needs Questionnaire Version: December 14, 2011. https://www.cdc.gov/nchs/slaits/cshcn.htm. Accessed 25 May 2020.
HyperRESEARCH 3.7.5. Computer Software. Researchware, Inc. 2015.
Department of Health and Human Services Office of the Secretary. Annual update of the HHS poverty guidelines: a notice by the Health and Human Services Department on 01/18/2018. In Department of Health and Human Services (Ed.). 2018. Federal Register. https://www.federalregister.gov/documents/2018/01/18/2018-00814/annual-update-of-the-hhs-poverty-guidelines. Accessed 25 May 2020.
Centers for Disease Control and Prevention National Center for Health Statistics State and Local Area Integrated Telephone Survey. 2009-2010 National Survey of Children with Special Health Care Needs Frequently Asked Questions. https://www.cdc.gov/nchs/slaits/cshcn.htm. Accessed on 28 May 2020.
SAS Software Version 9.4. Copyright © 2013. SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA.
Creswell JW, Miller DL. Determining validity in qualitative inquiry. Theory Pract. 2000;39:124–30. https://doi.org/10.1207/s15430421tip3903_2.
Minkler M, Fuller-Thomson E. African American grandparents raising grandchildren: a national study using the Census 2000 American Community Survey. J Gerontol Ser B-Psychol Sci Soc Sci. 2005;60:S82–92. https://doi.org/10.1093/geronb/60.2.s82.
Denboba D, McPherson MG, Kenney MK, Strickland B, Newacheck PW. Achieving family and provider partnerships for children with special health care needs. Pediatrics. 2006;118:1607–15. https://doi.org/10.1542/peds.2006-0383.
Debabanah S, Shaia WE, Campion K, Nichols HM. “We had to keep pushing”: Caregivers’ perspectives on autism screening and referral practices of Black children in primary care. Intellect Dev Disabil. 2018. https://doi.org/10.1352/1934-9556-56.5.321.
Burkett K, Morris E, Manning-Courtney P, Anthony J, Shambley-Ebron D. African American families on autism diagnosis and treatment: the influence of culture. J Autism Dev Disord. 2015;45:3244–54. https://doi.org/10.1007/s10803-015-2482-x.
Hong A, Singh JS. Contextualizing the social and structural constraints of accessing autism services among single Black female caregivers in Atlanta, Georgia. Int J Child Health Hum Dev. 2019;12(4):365–378.
Pearson JN, Meadan H. African American parents’ perceptions of diagnosis and services for children with autism. Educ Train Autism Dev Disabil. 2018. https://doi.org/10.2307/26420424.
Hodgetts S, McConnell D, Zwaigenbaum L, Nicholas D. The impact of autism services on mothers’ psychological wellbeing. Child Care Health Dev. 2017;43:18–30. https://doi.org/10.1111/cch.12398.
Hodgetts S, Zwaigenbaum L, Nicholas D. Profile and predictors of service needs for families of children with autism spectrum disorders. Autism. 2015;19:673–83. https://doi.org/10.1177/1362361314543531.
Carr T, Lord C. A pilot study promoting participation of families with limited resources in early autism intervention. Res Autism Spectr Disord. 2016;25:87–96. https://doi.org/10.1016/j.rasd.2016.02.003.
Hyman SL, Levy SE, Myers SM, Kuo DZ, Apkon S, Davidson LF, et al. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics. 2020;145:e20193447. https://doi.org/10.1542/peds.2019-3447.
Council on Children with Disabilities and Medical Home Implementation Project Advisory Committee. Patient- and family-centered care coordination: a framework for integrating care for children and youth across multiple systems. Pediatrics. 2013. https://doi.org/10.1542/peds.2014-0318.
Cheak-Zamora NC, Farmer JE. The impact of the medical home on access to care for children with autism spectrum disorders. J Autism Dev Disord. 2015;45:636–44. https://doi.org/10.1007/s10803-014-2218-3.
Carbone PS, Behl DD, Azor V, Murphy NA. The medical home for children with autism spectrum disorders: parent and pediatrician perspectives. J Autism Dev Disord. 2010;40:317–24. https://doi.org/10.1007/s10803-009-0874-5.
Jarquin VG, Wiggins LD, Schieve LA, Van Naarden-Braun K. Racial disparities in community identification of autism spectrum disorders over time; metropolitan Atlanta, Georgia, 2000-2006. J Dev Behav Pediatr. 2011;32:179–87. https://doi.org/10.1097/DBP.0b013e31820b4260.
Williams DR, Sternthal M. Understanding racial-ethnic disparities in health: sociological contributions. J Health Soc Behav. 2010;51:S15–27. https://doi.org/10.1177/0022146510383838.
Acknowledgements
We would like to express our gratitude to all the women in this study who contributed their valuable time and energy of telling their stories about navigating ASD services, as well as the staff and clinical professionals at the Autism Clinic at Hughes Spalding Children’s Hospital.
Availability of Data and Material
Not available
Code Availability
Not applicable
Funding
This study was supported by a research partnership between Children’s Healthcare of Atlanta and the Georgia Institute of Technology. Funding was also provided by the Ivan Allen College of Liberal Arts, Georgia Institute of Technology.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Jennifer S. Singh (qualitative) and Stephanie Wagner (quantitative). The first draft of the manuscript was written by Stephanie Wagner and Jennifer S. Singh, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Approval was obtained from the Institutional Review Boards of Children’s Healthcare of Atlanta (#16-099), Georgia Institute of Technology, and Morehouse School of Medicine, as well as the Grady Research Oversight Committee. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Participants signed informed consent regarding publishing their data. All the participants were given a pseudonym in the presentation of our findings to protect their identity.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wagner, S., Rubin, I.L. & Singh, J.S. Underserved and Undermeasured: a Mixed-Method Analysis of Family-Centered Care and Care Coordination for Low-Income Minority Families of Children with Autism Spectrum Disorder. J. Racial and Ethnic Health Disparities 9, 1474–1487 (2022). https://doi.org/10.1007/s40615-021-01086-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-021-01086-5