Abstract
Colorectal cancer, the second leading cause of mortality in the USA, can be prevented with colorectal cancer screening. However, many people who should receive the screening do not get screened. To learn more, this study estimated the prevalence of up-to-date colorectal cancer (CRC) screening and examined the relationship between CRC knowledge and screening compliance among Asian Americans living in the Baltimore-Washington Metropolitan area. The study included a cross-sectional sample of 274 Chinese, Korean, and Vietnamese Americans aged 50–75 years old. Participants completed a questionnaire regarding CRC knowledge in either their preferred native language or in English, and data were collected in person. The percentage of total participants with up-to-date overall CRC screening was 52.9%. Up-to-date fecal occult blood test (FOBT) screening was 15.0% and colonoscopy was 50.7%. The average CRC knowledge score was 6.10 out of 9 (SD = 2.91). Those with high education, high English proficiency, married, health insurance, and good physical health ratings had higher CRC knowledge. In multivariate analysis, CRC knowledge was significantly correlated with increasing up-to-date colonoscopy (aOR = 2.74, 1.13–6.64). Having health insurance (aOR = 4.40, 2.33–8.32) was another predictor of up-to-date colonoscopy. These findings suggest that CRC knowledge is a strong predictor of CRC screening behavior in Asian American populations. Lack of CRC screening knowledge still remains an important barrier to screening, and increased public awareness is necessary to achieve greater screening compliance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the second most common cause of cancer-related death in the USA [1]. Among Asian American men and women, CRC is the third leading malignant neoplasm and one of the top causes of cancer-related mortality [2, 3]. In recent years, CRC incidence and mortality have increased among three of the largest Asian American subgroups: Chinese, Korean, and Vietnamese Americans. From 1990 to 2008, the incidence of CRC in Asian Americans, particularly Vietnamese and Korean Americans increased, with Korean Americans having higher than or comparable rates to those of non-Hispanic whites [3]. A study conducted in California reflected similar patterns in Korean and Vietnamese American populations [4]. Furthermore, Chinese American adults in California had higher CRC incidence rates, while Chinese and Korean American adults in California had higher CRC mortality rates than the total Asian/Pacific Islander population [5].
To reduce the risk of CRC incidence and mortality, the US Preventive Services Task Force (USPSTF) has recommended that all adults aged 50 to 75 should be screened for CRC using stool-based tests, such as fecal occult blood test (FOBT) yearly, or direct visualization tests, such as colonoscopy, every 10 years [1]. Both FOBT and colonoscopic screening have been shown to significantly reduce the risk of CRC death in a cost-effective manner [6, 7]. However, previous studies have shown that Asian Americans as a whole have lower screening rates than all other racial groups, including non-Hispanic Whites (46.8 vs 57.7%, respectively) [8, 9]. When separated into ethnic subgroups, Korean and Vietnamese Americans self-reported the lowest CRC screening rates [8]. Chinese American populations in Chicago were less likely to undergo CRC screening compared to Vietnamese, and both groups had lower rates of CRC screening than the national average [10]. The National Colorectal Cancer Roundtable has established a nationwide movement of “80% by 2018,” which aims to raise the screening rate among the general American population to 80%, but Asian American screening rates are not on track to reach this goal [9, 11]. Therefore, increased screening for CRC among Asian Americans may be a critical step in reducing CRC incidence and mortality.
In a cross-sectional study of 815 Korean, Vietnamese, and Chinese Americans, it was determined that factors associated with decreased likelihood of CRC screening included lower education levels, lack of health insurance, lack of employment, and decreased English proficiency [12]. Another study of 205 Korean Americans showed that CRC screening is correlated with marital status, general physical health, and time spent in the USA [13]. English proficiency and time spent in the USA, also known as proxy measure of acculturation, are powerful predictors of screening likelihood, as well [12, 13].
Knowledge about CRC is one of the most important factors to affect a person’s inclination to undergo screening [14]. In African-American populations, participants who were more informed about CRC were more likely to perceive the benefits of screening as outweighing the barriers [12]. In addition, lower CRC knowledge was associated with less education, lack of employment/health insurance, and lower income among African Americans and Whites living in the Kentucky; these factors lead to low CRC screening rates [15]. CRC knowledge, attitude, and behavior questionnaires administered to Japanese Americans and Asian American populations in Michigan yielded similar results [16, 17]. These studies showed that mailing educational pamphlets and using Asian-language media could increase CRC knowledge, educate the public, and help decrease barriers to screening [16, 17].
Previous studies investigating CRC screening in Asian Americans have been conducted in areas with dense Asian American populations, such as California, New Jersey, New York, and Philadelphia [8, 9, 12, 18]. To learn more about factors affecting CRC screening among Asian Americans, we studied another area with a dense Asian American population, the Baltimore-Washington Metropolitan areas (BWMA) [19]. The purposes of this paper are as follows: (1) to report the rates of up-to-date overall CRC screening and test-specific CRC screening (e.g., FOBT, colonoscopy) among Asian Americans in the BWMA and compare those rates with national data on Asian Americans from the 2009 California Health Interview Survey (CHIS); (2) to examine the CRC knowledge scores and correlates of CRC knowledge; and (3) to examine the relationship between CRC knowledge and up-to-date colonoscopy in Asian American populations residing in the BWMA.
Methods
This is a secondary data analysis of data collected as a part of the Asian American Liver Cancer Prevention Program (hereinafter the Program) for our paper. Using a non-probability sampling method, foreign-born Asian American adults, aged 18 years and older, were recruited from the community in the BWMA. One or two weeks before the Program, we had a pre-screening event to recruit eligible participants. Of the 645 eligible volunteer participants, 30 did not show up for the program. Of the 615 who attended the program, 15 did not complete the initial survey. A total of 600 Asian Americans aged 18 and older completed the survey [20]. From this cohort of 600, this paper included 274 respondents between 50 and 75 years of age in the analysis.
Recruitment Procedure
We recruited participants who expressed interest in participating. They were screened for eligibility and invited to participate in the study through local community-based events and through other connections made through a community advisory board (CAB) that was established in 2008. The members of CAB were critical sources for obtaining the referred locations for recruitment. Three major recruitment strategies adopted were as follows: (1) advertisements that described the study were placed in local Chinese, Korean, and Vietnamese newspapers and in local Asian grocery stores, and individuals who responded to the advertisements were screened for eligibility and invited to participate in the study; (2) community announcements of upcoming screening events by lay health workers (LHWs); and (3) contact with church and temple leaders to arrange recruitment days where church and temple members were invited to participate in the study on the spot. Most participants were recruited directly by LHWs or learned about screening events through word-of-mouth.
Data Collection Procedure
After obtaining informed consent, all of the participants were asked to complete a self-administered questionnaire in English, Chinese, Korean, or Vietnamese, with the assistance of a bilingual interviewer when necessary. The data collection period was from April 2013 to March 2014. This study was approved by the Committee of Human Research at Johns Hopkins Bloomberg School of Public Health.
Measures
The questionnaire was translated into respective ethnic languages by bilingual research assistants and back-translated into English by different bilingual research assistants. The translated questionnaire was compared and discussed to reach to a consensus of the best wording choice in each ethnic language. Then, the questionnaire was pilot tested and reviewed by community advisory board members.
CRC screening behaviors included FOBT and colonoscopy. Participants were first asked if they had undergone each of these screening tests. For instance, participant utilization of the colonoscopy was assessed first by asking whether they had ever had colonoscopy (yes, no, not sure), and if yes, when they had their most recent colonoscopy (<a year ago; 1–5 years ago; 5–10 years ago; more than 10 years ago). Then, the measure of up-to-date colonoscopy was categorized into 0 = no/had more than 10 years; 1 = had less than 10 years.
CRC knowledge was adapted from the instrument of 17 knowledge questions in our recent CRC study of Chinese and Korean Americans [21] (see Table 3). Our knowledge measure consisted of nine questions covering topics such as CRC risk factors (e.g., “Risk of CRC becomes greater as a person gets older”), symptoms (e.g., “Bleeding is a symptom to report to your doctor”), screening knowledge (e.g., “CRC screening is not necessary if there are no symptoms”), and treatment knowledge (e.g., “The treatment for CRC may not be as bad if the cancer is found early”). Each correctly answered question was given a point; scores were summed to yield the final knowledge composite score ranged from 0 to 9. The composite score of CRC knowledge was highly skewed to the high end and was converted to a three category ordinal variable denoting low (0–6), medium (7–8), and high (9). The internal reliability of the instrument in this study was good (Cronbach alpha = .87).
Control Variables
Demographic information included in the analysis were age, gender (0 = male; 1 = female), ethnicity (0 = Chinese; 1 = Korean; 2 = Vietnamese), marital status (0 = no; 1 = yes), employment (0 = no; 1 = yes), and having health insurance (0 = no; 1 = yes). Education was categorized into 3 categories: <high school, high school graduate+, or >college graduate. As a proxy measure of acculturation, spoken English proficiency was measured on a 5-point scale ranging from not at all (=1) to fluent like a native speaker (=5). Participants rated their current health on a 5-point ordinal scale ranging from poor (=1) to excellent (=5).
Data Analysis
Three sets of analyses were conducted. First, descriptive analyses were performed to provide background information on the sample. We reported the rate of CRC screening by subgroups of Asian Americans in our study population as well as in the 2009 CHIS data which consists of a sample population containing high percentages of Asian American. For the CHIS data, we conducted weighted descriptive analysis by using command of svy in STATA [22] to account for the design of the complex and multistage sample by using the jackknife method to compute standard error estimates. Second, we examined the percent of correct CRC knowledge and identified the correlates of CRC knowledge using zero order correlations. Finally, we conducted logistic regression analysis to examine factors associated with up-to-date colonoscopy. All analyses were performed with STATA version 13 software.
Results
Sample Characteristics
Characteristics of the 274 Asian Americans are shown in Table 1. Participant average age was 57 years (range 50–75, SD 5.21), and more than half were female (58.8%). About two-thirds were employed (63.7%). More than four-fifths were married or living with a partner (84.2%). Mean score of self-rated physical health was 2.95 (SD: 1.02) on a scale of 1 (poor) to 5 (excellent). About half reported having no or poor proficiency with spoken English (47.8%). About half had health insurance.
Rate of Up-to-Date CRC Screening
Table 2 compared the rate of up-to-date CRC screening among our participants with the rate of up-to-date CRC screening among 23,837 adults aged 50 and 75 years old in the 2009 CHIS. When the CHIS data were disaggregated by race, rates of up-to-date overall CRC screening were higher among Whites (70.1%) than among Asians (64.7%), African Americans (63.9%), and Latino (53.4%). When the CHIS data were disaggregated by Asian American ethnicity, Chinese Americans had a higher rate of up-to-date overall screening (66.5%, 95% CI: 59.3, 73.0) than Korean Americans (62.0%, 95% CI: 50.8, 72.1) and Vietnamese Americans (59.0%, 95% CI: 46.3, 70.6). Compared to the CHIS data, our participants had similar rates of up-to-date overall screening: Chinese Americans (64.4%, 95% CI: 53.4, 74.4) had the highest rate followed by Vietnamese Americans (52.5%, 95% CI: 41.0, 63.8) and Korean Americans (43.9%, 95% CI: 34.3, 53.9). The differences between the CHIS data and our data were not statistically significant based on overlapping 95% CI.
In test-specific CRC screening, African Americans (36.9%) had high FOBT followed by Asian Americans (34.4%), Whites (33.9%), and Latino (33.3%). When the CHIS data were disaggregated by Asian American ethnicity, Vietnamese Americans had a higher rate of up-to-date FOBT (30.9%, 95% CI, 22.1, 41.4) than Chinese Americans (30.4%, 95% CI: 24.5, 37.1) and Korean Americans (27.2%, 95% CI 19.1, 37.2). Compared to the CHIS data, our participants had much lower rates of up-to-date FOBT: about 15% reported having up-to-date FOBT. Vietnamese had the highest rate of up-to-date FOBT (21.3%, 95% CI: 12.9, 31.8) followed by Chinese (13.8%, 95% CI: 7.3, 22.9) and Korean (11.2%, 95% CI: 5.9, 18.8). These differences between our study sample and the CHIS data among Chinese and Koreans were statistically significant based on no overlapping 95% CI.
Rates of up-to-date of colonoscopy among the participants in the CHIS and our study were also compared (Table 2). In the CHIS, the rate of up-to-date colonoscopy was lower among Asian Americans (47.0%) than Whites (55.4%). When the CHIS data were disaggregated by Asian American ethnicity, Chinese Americans had the highest rates of having colonoscopy less than 10 years ago (53.3%, 95% CI: 45.8, 60.7) followed by Korean Americans (49.9%, 95% CI: 38.4, 61.5) and Vietnamese Americans (42.1%, 95% CI: 30.6, 54.6). In our study of Asian Americans, Chinese had a higher rate of up-to-date colonoscopy (63.2%, 95% CI: 52.2, 73.3) than Vietnamese (47.5%, 95% CI: 36.2, 58.9) and Korean (42.9%, 95% CI: 33.5, 52.9). These differences between our study samples and the CHIS population were not statistically significant based on overlapping confidence interval.
CRC Knowledge
CRC knowledge scores ranged from 0 to 9 with a mean score of 6.10 (SD = 2.91) (Table 3). The percentage of correct answers per question ranged from 47.0 to 79.3%. Fewer than half of participants (47.0%) answered correctly that “CRC begins as a growth in the colon or rectum.” Participants also had low screening knowledge (59.6%) that “CRC screening is not necessary if there are no symptoms.”
Correlates of CRC Knowledge
Zero-order correlations were computed across all variables including CRC knowledge to assess overlapping variance. Education, marital status, English proficiency, having health insurance, and self-rated health were significantly associated with CRC knowledge (Table 4). Education was significantly related to self-rated physical health (r = .38, p < .001) and having health insurance (r = .29, p < 001). English proficiency was also highly correlated with education (r = .53, p < .001), having health insurance (r = .41, p < .001), and physical health (r = .45, p < .001). In consideration of multicollinearity of these measures and English proficiency, we decided to have final model of CRC screening without English proficiency.
Factors Associated with Having Up-to-Date Colonoscopy
The results of the bivariate and the multivariate logistic regression analyses are shown in Table 5. In bivariate analysis, ethnicity, self-reported physical health, having health insurance, and CRC knowledge were associated with having up-to-date colonoscopy (p < .05). Education was marginally significant at p < .10. In multivariate analysis, education, health insurance, and CRC knowledge were significantly related to having colonoscopy. Those with high CRC knowledge were more likely to have colonoscopy than those with low knowledge (aOR = 2.74, CI, 1.13, 6.64). Those who had health insurance had higher likelihood of having colonoscopy than those without health insurance (aOR = 4.40, CI, 2.33, 8.32). Those more than high school education were less likely to have colonoscopy than those with less than high school education (aOR = 0.37, CI, 0.16, 0.84).
Discussion
This study reported the prevalence of up-to-date CRC screening and the predictors of CRC knowledge and CRC screening behaviors in Chinese, Korean, and Vietnamese populations residing in the Baltimore-Washington Metropolitan areas. The results of the data allow us to make several key points regarding how CRC knowledge and other factors affect CRC screening.
Although regular CRC screening is advised for all people ages 50 to 75, participants in this study appeared to have the low rates of up-to-date FOBT among Chinese and Korean Americans, consistent with previous studies [7, 21]. The rates of up-to-date colonoscopy were higher than those reported in previous studies from data on Asian American [13, 21]. Overall, these up-to-date CRC screening rates still lag significantly behind screening rates of the general American population, further supporting the need to focus on increasing screening among Asian Americans in order to meet the national CRC screening goal of 80% by 2018 [11].
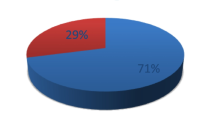
Our findings also indicate that more study participants had colonoscopy screening than FOBT screening (50.7 vs 15.0%). Colonoscopy is becoming the test of choice in the general population and in minority groups [23]. It may be because primary care physicians are recommending colonoscopy, since a majority of physicians think that colonoscopy is more accurate than FOBT. Although primary screening through FOBT may be much cheaper on a population basis [24], it is difficult for participants to follow up annually with FOBT screening, causing lower rates of up-to-date screening. In addition, even though patients may have received the FOBT kit from their doctor, they may forget to mail in the test or return it to their doctor.
Interestingly, our study showed that Chinese Americans in the targeted area have higher rates of up-to-date colonoscopy screening compared to those in the 2009 CHIS (63.2 vs 53.3%). This may be due to their higher education. We found that the Chinese in the sample had a significantly higher level of education compared to the Koreans and Vietnamese in the sample (51% of Chinese had more than college education compared to 39% of Korean and 10% of Vietnamese). The disparity between our finding and previous results could indicate significant differences in demographic variables of Asian Americans living in the BMWA.
In terms of any previous up-to-date CRC screening, Korean Americans had the lowest rates for overall CRC screening and test-specific CRC screening (e.g., FOBT, colonoscopy) compared to Chinese and Vietnamese Americans. This observation is consistent with findings from Hwang et al. that Korean Americans had the lowest CRC screening rates among Asian American subgroups [13]. Future research studies could further examine the relationship between screening likelihood and certain demographic variables within Asian American ethnic subgroups.
The average CRC Knowledge score among our survey participants was slightly lower than those reported from similar quizzes administered to Asian American and White populations [14]. While greater than 90% of participants from these earlier studies answered certain questions correctly, the question with the highest percentage correct in our study was much lower at 79.3% [21]. Less than half of our survey participants answered the question, “CRC begins as a growth in the colon or rectum,” correctly. In comparison, in studies by Lu et al., 70% of participants answered the same question correctly [21]. This result may suggest that Chinese, Korean, and Vietnamese American populations in the BMWA are much less informed about CRC than Whites, African Americans, and Asian Americans living in other regions of the USA, and because knowledge is correlated to screening behavior, we must focus on educating Asian American populations about CRC in order to increase screening.
CRC knowledge and health insurance status were two important predictors of CRC screening behavior in this study. Consistent with previous findings [16, 17], knowledge of CRC is the strongest predictor of CRC screening behaviors among Asian Americans. These findings also verify previous studies that lack of health insurance is a consistent barrier to screening [12, 13, 15]. Interestingly, individuals with greater than high school education level were less likely to undergo screening compared to those without a high school diploma. It might be assumed that those with higher education and employed had no time to have up-to-date colonoscopy even if they had health insurance.
There were several limitations in this study. First, our sampling method was based on convenience and lacked randomization. Therefore, results from this study cannot be generalized to all Asian Americans living in the USA. Second, our data were self-reported by participants and were not verified through outside sources. This may result in recall bias and incorrect answering of survey questions. Third, we used weighted data analysis to consider oversampling of Asian Americans in the CHIS. Nevertheless, there are many methodological differences between our Program and the CHIS. In order to properly contextualize observed differences, we need to consider the following: sampling strategy (convenience sampling vs random sampling), mode of administration (personal interview vs phone interview), geographic location (Baltimore-Washington Metropolitan areas vs California), and year of data collection (2013–2014 vs 2009).
Despite these limitations, the findings of this study are an important reminder that CRC knowledge and screening behaviors in Asian American populations still lag behind those of the general American population, and future strategies and interventions to educate Asian Americans on CRC are still much needed areas of improvement. This result again reflects the idea that increasing the understanding of the general public on CRC and its preventability are of utmost importance in increasing screening compliance.
References
US Preventive Services Task Force. Screening for colorectal cancer: Us preventive services task force recommendation statement. JAMA. 2016;315(23):2564–75.
Rahman R, Schmaltz C, Jackson CS, et al. Increased risk for colorectal cancer under age 50 in racial and ethnic minoritis living in the United States. Cancer Med. 2015;4(12):1863–70.
Gomez SL, Noone A-M, Lichtensztajn DY, et al. Cancer incidence trends among Asian American populations in the United States, 1990–2008. J Natl Cancer Inst. 2013;105(15):1096–110.
Giddings BH, Kwong SL, Parikh-Patel A, Bates JH, Snipes KP. Going against the tide: Increasing incidence of colorectal cancer among Koreans, Filipinos, and south Asians in California, 1988–2007. Cancer Causes Control. 2012;23(5):691–702.
Bates JH, Kwong SL, Hofer BM, et al. Colorectal cancer among Californians, 1988–2007. Sacramento, CA: California Department of Public Health, Cancer Surveillance Section; 2010.
Jung MY, Holt CL, Ng D, et al. The Chinese and Korean American immigrant experience: a mixed-methods examination of facilitators and barriers of colorectal cancer screening. Ethn Health. 2017: 1–20.
Ryu SY, Crespi CM, Maxwell AE. Colorectal cancer among Koreans living in South Korea versus California: Incidence, mortality and screening rates. Ethn Health. 2014;19(4):406–23.
Trinh QD, Li H, Meyer C, et al. Determinants of cancer screening in Asian-Americans. Cancer Causes Control. 2016;27:989–98.
Lee HY, Lundquist M, Ju E, et al. Colorectal cancer screening disparities in Asian Americans and Pacific islanders: Which groups are most vulnerable? Ethn Health. 2011;16(6):501–18.
Kim K, Chandrasekar E, Lam H. Colorectal cancer screening among Chinese, Cambodian, and Vietnamese immigrants in Chicago. J Racial Ethn Health Disparities. 2015;2(4):473–80.
80% by 2018 | National Colorectal Cancer Roundtable [Internet]. [cited 2016 Jul 5]. Available from: http://nccrt.org/tools/80-percent-by-2018/
Ma GX, Wang MQ, Toubbeh J, et al. Factors associated with colorectal cancer screening among Cambodians, Vietnamese, Koreans and Chinese living in the United States. N Am J Med Sci (Boston). 2012;5(1):1–8.
Hwang H. Colorectal cancer screening among Asian Americans. Asian Pac J Cancer Prev. 2013;14(7):4025–32.
Sentnell T, Braun KL, Davis J, et al. Colorectal cancer screening: Low health literacy and limited English proficiency among Asians and whites in California. J Health Commun. 2013;18(Suppl 1):242–55.
Knight JR, Kanotra S, Siameh S, et al. Understanding barriers to colorectal cancer screening in Kentucky. Prev Chronic Dis. 2015;12(E95):1–9.
Wu T-Y, Kao JY, Hsieh H-F, Tang Y-Y, Chen J, Lee J, et al. Effective colorectal cancer education for Asian Americans: A Michigan Program. J Canc Educ. 2010;25(2):146–52.
Lau DT, Machizawa S, Demonte W, Cameron KA, Muramatsu N, Henker RD, et al. Colorectal cancer knowledge, attitudes, screening, and intergenerational communication among Japanese American families: An exploratory, community-based participatory study. J Cross Cult Gerontol. 2013;28(1):89–101.
Lee S, Chen L, Jung MY, et al. Acculturation and cancer screening among Asian Americans: Role of health insurance and having a regular physician. J Community Health. 2014;39(2):201–12.
Population estimates, July 1, 2015 [Internet]. [cited 2016 Jul 6]. Available from: http://www.census.gov/quickfacts/table/PST045215/11
Juon HS, Strong C, Kim F, et al. Lay health worker intervention improved compliance with hepatitis B vaccination in Asian Americans: Randomized controlled trial. PLoS One. 2016;11(9):1–14.
Lu X, Holt CL, Chen JC, et al. Is colorectal cancer a western disease? Role of knowledge and influence of misconception on colorectal cancer screening among Chinese and Korean Americans: A mixed methods study. Asian Pac J Cancer Prev. 2016;17(11):4885–92.
Korn EL, Graubard BI. Simultaneous testing of regression coefficients with complex survey data: Use of Boferroni t statistics. Am Stat. 1990;44(4):270–6.
Meissner HI, Breen N, Klabunde CN, et al. Patterns of colorectal cancer screening uptake among men and women in the United States. Cancer Epidemiol Biomark Prev. 2006;15(2):389–94.
Fisher JA, Fikry C, Troxel AB. Cutting cost and increasing access to colorectal cancer screening: Another approach to following the guidelines. Cancer Epidemiol Biomark Prev. 2006;15(1):108–13.
Acknowledgements
We thank all the participants of this study. We also appreciate the dedicated work of the members of the research team.
Contribution
HS Juon and S Lee conceptualized the study. J Guo and J Kim did literature review and wrote introduction. HS Juon wrote the first draft. HS Juon devised the analysis plan and conducted the analyses. All authors edited the final draft of the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the National Cancer Institute (grant number: R01CA163805).
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study and all the procedures were approved by the Committee of Human Research at Johns Hopkins Bloomberg School of Public Health.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Juon, HS., Guo, J., Kim, J. et al. Predictors of Colorectal Cancer Knowledge and Screening Among Asian Americans Aged 50–75 years old. J. Racial and Ethnic Health Disparities 5, 545–552 (2018). https://doi.org/10.1007/s40615-017-0398-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-017-0398-1