Abstract
Background
Copper is associated with mild cognitive impairment (MCI). However, there is a lack of relevant population studies with large sample sizes.
Aims
This study used baseline data from a cohort study to determine the distribution characteristics of MCI in the elderly and to estimate the association between whole blood copper concentrations and MCI.
Methods
MCI status was screened by the Mini-Mental State Examination (MMSE) scale and Activities of Daily Living (ADL) scale. The concentration of copper in whole blood was determined by Inductively Coupled Plasma Mass Spectrometer (ICP-MS).
Results
A total of 1057 subjects with an average age of 71.82 ± 6.45 years were included in this study. There were 215 patients with MCI, and the prevalence of MCI was 20.34%. After adjusting for general demographic variables, logistic regression analysis showed that the risk of MCI in the elderly with high copper level was 1.354 times higher than that in the elderly with low copper level (OR 1.354, 95% CI 1.047–1.983, P = 0.034).
Conclusion
In this study, it was found that the prevalence of MCI was different in gender, age, education level and other aspects, and a higher copper level in the elderly was significantly related to the occurrence of MCI. The association was stronger in older adults and men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mild cognitive impairment (MCI) is a clinical transition state between normal aging and dementia, and is a cognitive disorder syndrome [1, 2]. Its main characteristics are cognitive decline, including memory impairment and learning or concentration difficulties, and objective cognitive function tests can detect abnormalities, but do not meet the criteria for dementia [3, 4]. With the increase in the aging population, the incidence and prevalence of MCI in China are increasing year by year. The annual incidence of MCI ranges from 1 to 6%, while the annual prevalence estimates range from 3 to 22% [5], which is much higher than in developed countries such as Germany (3.1%) and Canada (1.03%) and Finland (5.3%) [6]. Studies have shown that most patients with MCI would convert to Alzheimer’s disease (AD) without any intervention within 4–6 years [7]. Its rate of onset was 10 times that of healthy elderly people. If a patient with MCI converts to AD, it would cause irreversible damage to the patient, severely reduce their quality of life, and bring a huge burden of disease to the family and society[8, 9]. To date, no monocausal treatment has reached its primary clinical endpoints [10], and its pathogenesis is not yet clear [11,12,13]. Therefore, understanding the epidemiological characteristics and influencing factors of MCI, early intervention and control or delay of the development of MCI and its conversion to AD will help improve the quality of life of the elderly, and reduce the burdens on the family and social economy. This has important practical significance for achieving healthy aging.
Copper is one of the earliest metals used by humans and has had a profound impact on the progress of human civilization. In 1996, the World Health Organization listed copper as a basic element and recommended that the minimum intake for preventing copper deficiency is 0.9 mg/day [14]. However, with the acceleration of industrialization and urbanization, the health threat caused by metals has attracted increasing attention. Although the geological background of heavy metals in the soil in China is relatively low, they are widely distributed in the environment due to the rise of mining, the development of the smelting industry and the large-scale use of metal-containing compounds in daily life and production industries, and most of them are discharged into the environment. Internationally, the results of studies on the impact of copper on cognitive function are also different. A cohort study showed that subjects with MCI who had a serum copper level above 1.6 mmol/L were three times more likely to convert to AD than normal subjects after 4 years of follow-up.[15]. Another large community prospective study showed that there was an association between copper intake and mental decline in healthy people whose diets were rich in saturated fats and trans fats. For example, people who consumed an average of 2.75 mg of copper a day had more than a 50% decrease in intelligence compared to those who consumed 0.88 mg of copper a day [16]. A case–control study showed that serum nonceruloplasmin nonalbumin copper was elevated in MCI and dementia due to AD [17]. High dietary intake of copper in conjunction with a diet high in both saturated and trans fats may be associated with accelerated cognitive decline [16]. However, there are some different voices about whether copper intake is related to cognitive function [18]. The reason for this different conclusion may be that the human body’s absorption rate of copper changes with increasing in intake [19]. There have been a number of studies showing that an imbalance of copper in AD can be improved, and genes that control the copper pathway play an important role in the development of AD [10, 20, 21]. Population studies are also needed to confirm these observations.
To further understand and explore the association between cognitive function and copper, the research group collected data from a baseline survey of the Elderly Health and Environment Risk Factor Cohort (EHERFC), which was conducted in Lu’an, Anhui Province, China. A total of 1080 whole blood samples were collected, the copper content was determined by inductively coupled plasma mass spectrometer (ICP-MS), and the association between whole blood copper levels and cognitive function was estimated.
Materials and methods
Study population
The data reported in this article were from a baseline survey of the EHERFC, in Lu’an city, Anhui Province, China, carried out from June 2016 to September 2016. A cluster sampling method was used to identify the samples to explore the health and environmental factors of the elderly. Two administrative districts were selected, and a community was randomly selected. All respondents who met the inclusion criteria in the community completed a household questionnaire survey and were admitted to a designated hospital for physical examination. The investigator determined whether the survey object met the inclusion criteria. The inclusion criteria were as follows, (1) age over 60 years old, (2) living in the local area for more than 6 months, (3) consciously and abled to complete the questionnaire, (4) voluntarily participated in the study and signed the informed consent form, and (5) a clear consciousness, no serious neuropsychiatric disease, and sufficient understanding and expression skills to complete the investigation. The exclusion criteria were as follows, (1) communication barriers, (2) poor compliance, or (3) groups with severe brain diseases or taking drugs containing related trace elements (such as copper gluconate, copper acetate, copper citrate, etc.). The investigator introduced the research purpose and research content in detail to the survey subjects who met the inclusion criteria after respondents signed the informed consent form launching an investigation. A total of 1080 pieces of information were collected. According to the purpose of this study, 23 people in whom blood samples were not collected were excluded, the detection rate of copper was 93.80%, and 1013 blood samples were finally included in the correlation analysis.
The diagnostic criteria of MCI
ADL (activity of daily living scale) scale [22] was used to assess the ability of the elderly performing activities of daily living. The scale includes 10 items for eating, bathing, grooming, dressing, stool control, urination control, toileting, transfer, walking on level ground and going up and downstairs. Each item is divided into 0, 5, and 10 points, with a full score of 100 points. If the score is greater than 60 points, it will be regarded as basic self-care, a score of 40–60 is judged that needed help in life, a score of 20–40 is judged to be dependent on others for life, and scores less than 20 are divided into living completely dependent on others.
The mini-mental state examination (MMSE) scale [23] was currently one of the most influential and popular cognitive impairment screening tools in the world. The scale includes orientation, immediate memory, attention and calculation, short-term memory, language and visual space structure ability, a total of 30 items. The correct answer or operation is given a score of one, whereas the opposite is given a score of zero. The standard for dividing the normal threshold were, when the score of illiteracy ≤ 17 points, the score of the education level of primary school ≤ 20 points and middle school education or above ≤ 24points [24]. Those who meet the following conditions were judged as MCI [25], (1) respondents or family members reported clues to memory impairment in the past year, (2) basically take care of their own daily life, ADL scale score was greater than 60 points, (3) MMSE score, illiteracy ≤ 17 points, elementary school ≤ 20 points, middle school and above ≤ 24 points, (4) not meet the diagnostic criteria for dementia.
Collection of whole blood samples
The subjects were required to take blood samples in the morning in a designated hospital. Before that they should fast for up to 8 h. Medical staff used two types of anticoagulant and non-anticoagulant vacuum blood-collecting vessels to collect peripheral venous blood. Centrifuged the blood in the non-anticoagulated blood collection tube at 4000 rpm for 5 min, and taken the upper layer of serum to detect various blood biochemical indicators. The blood in the anticoagulated blood collection tube is transferred into a 2 mL polypropylene tube after routine blood testing, each sample was stored in 3 tubes, and sent to Lu'an City Center for Disease Control and Prevention – 80 ℃ refrigerator for storage immediately. Finally, the cold chain was used to transport samples to the laboratory of Anhui Medical University.
Laboratory analysis
Experimental apparatus
Inductively coupled plasma-mass spectrometer (Perkin Elmer NexION 350X, Shelton, CT, USA), Ultrapure water meter (Cascada 1, Pall Corporation, USA), Electronic analytical balance (AB265-S, METTLER TOLEDO, Switzerland).
Experimental reagent
Up-S grade nitric acid (Jingrui Corporation, China), TritonX-100 (Sigma Corporation, USA), 25% Tetramethyl Hydroxyl Ammonia Solution (Gelinda Corporation, China), 10 µg/mL copper standard solution (PerkinElmer Corporation, USA) and 10 µg/mL internal standard mixed standard solution (PerkinElmer Corporation, USA) are prepared.
Sample processing
Removed the blood sample from the – 80 ℃ refrigerator and thaw it in the 4 ℃ refrigerator. Taken 1 mL blood sample in 50 mL disposable centrifuge tube, weigh it as M, then diluted the weight to 25 M with No. 1 solution (mix 7.4 mL of 68% concentrated nitric acid, 25 mL of TMAH and 5 mL of 5% tritonX-100 solution, and dilute to 500 mL). After mixing thoroughly, wait for 5 min for testing.
Instrument related parameters
Instrument parameters were shown in Table 1.
Sample determination
-
1.
Turned on the argon gas and the cooling circulating water, wait for the instrument to stabilize for 15–20 min, then started the torch.
-
2.
Measure blank control, 10 μg/L, 25 μg/L, 50 μg/L, 100 μg/L standard solution in sequence, the correlation coefficients of the standard curve were all greater than 0.999, Otherwise, the standard curve needs to be re-tested until the requirement was met.
-
3.
After each batch of samples was measured, clean the instrument with No. 1 solution for 30 min, and then rinsed with ultrapure water for 15 min.
Quality control
Quality control of field investigation
All survey subjects were required fasting blood sampling, no food after 20:00 one day before the examination, no water after 22:00, and avoided staying up late or greasy food. Registered the detailed home address on the cover of the questionnaire, mobile phone number or fixed telephone of the respondent and other contact methods to ensure that problems encountered can be returned and resolved in time. A quality control team was set up to supervise and guide the survey respondents to fill out the questionnaire, and quality check on the questionnaire.
Quality control of laboratory testing
-
1.
Elimination of pollution during the experiment
As the experimental utensils made of glass were easy to adsorb metal ions, which would affect the results of the experiment, so plastic products made of polypropylene were used in this experimental.
-
2.
Reducing instrument interference
At the end of each test the instrument was cleaned by No. 1 solution for 20 min. Before measuring the sample next day, washed the instrument again to ensure that the background signal value reached the minimum and remains stable.
-
3.
Sample quality control
After every 20 samples were tested, the whole blood metal element quality control standard of Seronorm Company was used for quality control. If it was found that the measured value of the quality control sample exceeded the given standard range, stopped the test and investigate the cause in time.
-
4.
Linear relationship, blank detection limit, instrument detection limit, quantification limit, spike recovery rate, intra-day precision and inter-day precision
In order to reducing the interference of the whole blood matrix in the detection process, the standard curve was prepared with the whole blood diluted 25 times as the matrix solution. The spiked concentrations of copper in the above-mentioned matrix solution were 10 μg/L, 25 μg/L, 50 μg/L, and 100 μg/L, respectively. Within this concentration range, the signal value (y) of the copper element had a good linear relationship with the concentration (x) (r ≥ 0.999). The relative precision of the instrument is shown in Table 2. Specific methods were shown in references [26, 27].
Statistical analysis
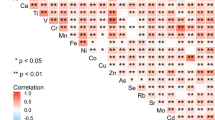
Pearson’s chi-square test was used to evaluate the significance of the difference in the prevalence of MCI among different population characteristics. Normal tests showed that the blood copper concentration did not conform to a normal distribution. After converting the logarithm of the whole blood copper concentration, the t-test or variance was used to compare the distribution differences in general demographic data, health-related behaviors, and chronic diseases. Spearman's rank correlation analysis was used to evaluate the association of the whole blood copper concentration with the MMSE score. A logistic regression model was used to evaluate the relationship between copper concentration and MCI risk. The copper concentration of the population was divided into three groups of high, middle and low according to tertiles. A stratified analysis was conducted for age and gender (The subjects were divided into three age groups: 60–69, 70–79, 80 years old and above).
The SPSS statistical software package (version 23.0) was used for all statistical analyses. All reported p values were bilateral, and p < 0.05 was considered statistically significant.
Ethical basis
The EHERFC strictly followed ethically related procedures. Before the investigation, relevant information, such as research purpose and research content was introduced to the respondents, and the investigation began only after the respondents signed the informed consent form. The research scheme was verified by the Ethics Committee of Anhui Medical University.
Results
Characteristics of the study population
A total of 1057 subjects were included in this study. Among them, 481 subjects (45.5%) were males and 576 subjects (54.5%) were females; 500 people (47.3%) were aged 60–69, 420 people (39.7%) were aged 70–79, and 137 people (13.0%) were aged 80 and above; 486 people (46.0%) were illiterate, 257 people (24.3%) were in elementary school, and 314 people (29.7%) were in junior high school and above; 148 persons (14.0%) lived alone and 909 persons (86.0%) did not live alone; 750 subjects (71.0%) were married and 307 subjects (29.0%) were unmarried or widowed; 294 people (27.8%) participated in physical exercise and 763 (72.2%) did not participate in physical exercise. See Table 3 for detailed demographic information.
The prevalence and influencing factors of mild cognitive impairment
In the study, 215 people were assessed as having MCI, and 842 people were classified as the normal population. The results of this study showed that the distribution of MCI was statistically significant with regard to gender, age, education level, region, residence status, marital status, physical exercise, and family monthly income (p < 0.05). There was no statistically significant difference in smoking or drinking (Table 4).
Distribution of blood copper levels and influencing factors
A total of 1057 whole blood samples were tested, and the detection rate was 100%. The geometric mean copper concentration in whole blood was 0.910 μg/mL, the standard deviation was 0.115 μg/mL, the median was 0.772 μg/mL, the minimum was 0.5391 μg/mL, and the maximum was 1.1824 μg/mL. The total blood copper concentration of the elderly had statistically significant differences in relation to the distributions of gender, age, education level, region, marital status, smoking, drinking, physical exercise and family monthly income (all p < 0.05) Table 5).
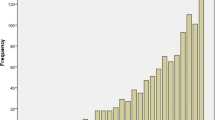
Correlation analysis between blood copper level and MMSE score
Figure 1 shows the MMSE scores of the study subjects. Spearman's rank correlation analysis was used to analyze the correlation between whole blood copper concentration and the MMSE score. The scatter diagram is shown in Fig. 2. The results of Spearman's rank correlation analysis showed that the correlation coefficient r = − 0.189 (p < 0.001).
Association between the blood copper level of the general population and the risk of mild cognitive impairment
Univariable logistic regression analysis showed that compared with low levels of copper, elderly people with high levels of copper had 1.566 times the risk for MCI (OR 1.566, 95% CI 1.075–2.281, p < 0.05) (Table 6).
After adjusting for gender, age, area of residence, education level, smoking, drinking, depression, physical exercise, income status, and marital status, the risk of MCI for the elderly with a high level of copper was 1.354 times that of the elderly with a low level of copper (OR 1.354, 95% CI 1.047–1.983, p < 0.05).
At the same time, the results of the multivariate analysis showed that elderly people with advanced age (OR 2.192, 95% CI 1.382–3.475, p < 0.001; OR 4.113, 95% CI 1.382–3.475, p < 0.001), living in a city (OR 1.690, 95% CI 1.007–2.835, p = 0.047), smoking (OR 1.651, 95% CI 1.053–2.581, p = 0.029), depressive symptoms (OR 1.478, 95% CI 1.027–2.58, p = 0.036), and high monthly household income (OR 1.575, 95% CI 1.002–2.478, p = 0.049) were at higher risk for MCI (Table 6).
Association between the whole blood copper level of the elderly of different genders and the risk of mild cognitive impairment
The univariate logistic regression analysis of male results showed that the risk of MCI in the elderly with high levels of copper was 1.888 times that in the elderly with low levels of copper (OR1 1.888, 95% CI 1.117–3.191, p = 0.018) (Fig. 3). After adjusting for age, area of residence, education level, smoking, drinking, depression, physical exercise, income status, and marital status, the risk of MCI in the elderly with a high copper level was 1.429 times that of those with a low copper level (OR2 1.429, 95% CI 1.058–2.501, p = 0.039) (Fig. 4).
Logistic regression analysis of correlation between whole blood copper concentrations (μg/mL) and MCI stratify by gender. OR1: crude odds ratio; OR2: adjusted the OR value of gender, age, area of residence, education level, smoking, drinking, depression, physical exercise, income status, marital status
Association between the whole blood copper level of the elderly of different ages and the risk of mild cognitive impairment
The results of the univariable logistic regression analysis of 60–69 years old people showed that before and after the adjustment of related variables, the risk of MCI in the elderly with moderate and high copper levels was not statistically correlated with that in the elderly with low copper levels.
The results of univariable logistic regression analysis of 70–79 years old people showed that the risk of MCI in the elderly with a high level of copper was 1.842 times that in the elderly with a low level of copper (OR 1.842, 95% CI 1.040–3.263, p = 0.036). After adjusting for related variables, the risk of MCI in the elderly with a high level of copper was 1.330 times that in the elderly with a low level of copper, but there was no statistical association (OR 1.330, 95% CI 0.704–2.514, p = 0.380) (Fig. 6).
The results of univariable logistic regression analysis of elderly people aged 80 years and above showed that the risk of MCI in elderly people with high levels of copper was 2.052 times that in elderly people with low levels of copper (OR1 2.052, 95% CI 1.297–3.756, p = 0.018) (Fig. 5). After adjusting for related variables, the incidence of MCI in the elderly with a high level of copper levels was 1.983 times that in the elderly with low copper levels (OR2 1.983, 95% CI 1.156–3.545, p = 0.024) (Fig. 6).
Discussion
With the aging of the Chinese population, the incidence of MCI is increasing gradually. This study shows that the overall prevalence of MCI in the elderly over 60 years old is 20.34%. In the largest epidemiological study to date in China, a survey of 10,276 community populations aged 65 and over found that the total prevalence of MCI in China was approximately 20.8% (95% CI 20.0–21.6%) [28].
Another community study of elderly people over 60 years old in Shanghai also showed that the prevalence of MCI was 20.1% [29]. The prevalence of MCI reported in other countries varies widely, ranging from 1.74 to 45.5% [30,31,32]. Representative research results have shown a 9.8% prevalence of MCI in the United States, and a study from Saudi Arabia showed that a prevalence of MCI as high as 38.6%. The main reasons for the large difference in prevalence may be as follows:
-
1.
The criteria for judging MCI are inconsistent. Studies have shown that the prevalence of MCI varies greatly across criteria [33].
-
2.
There are differences in research methods. Some studies are retrospective studies, using MCI diagnostic criteria to identify previously collected data, while prospective studies first identify diagnostic criteria and then collect and identify data for newly enrolled patients.
-
3.
Because MCI is highly correlated with age [31], the prevalence of MCI varies greatly among people of different ages.
-
4.
The choice of study subjects can also affect the prevalence of MCI. The prevalence of MCI in the community population was lower but higher than that in the hospital population [30].
At present, there are few reports on the association between whole blood copper concentration and MCI in the elderly. A case–control study showed significantly higher concentrations of copper in the red blood cells of patients with dementia when compared to that in the normal control group (p < 0.0001) [34]. Another cross-sectional study showed that older adults with high levels of copper in their nails had a 1.275 times greater risk of cognitive impairment than those with low levels of copper (OR 1.275, 95% CI 1.047–1.552, p < 0.05) [35].
The main sources of copper in the human body are food and drinking water. The elderly surveyed in this study had lived in the local area for many years, and the exposure source was relatively stable. The relationship between copper levels and MCI was analyzed by measuring copper concentrations in the whole blood of older adults using baseline data from a cohort study. The results showed that older adults with higher copper levels had a higher incidence of MCI, and men and the elderly had a higher risk of MCI. Many epidemiological studies and animal experiments have shown that copper affects cognitive function [36, 37], and hypothetical mechanisms of the effect of copper on cognition have been summarized and preliminarily established[38]. The formation of insoluble fibrils as a result of amyloid β-protein (Aβ) aggregation is the main pathological incident in AD [39,40,41]. Aβ first forms dimers and oligomers and then forms aggregates, leading to neurodegeneration. At the same time, it accumulates phosphorylated tau protein in cells to form neurofibrillary tangles [42]. Normally, excess Aβ in the brain is eliminated by lipoprotein receptor-related protein-1. Singh [43] found that low-dose copper can destroy the function of lipoprotein receptor-associated protein-1 through oxidation and regulate the Aβ to cross the blood–brain barrier, which ultimately leads to the formation of Aβ plaques and neurotoxicity. Reports show that Aβ aggregation is a consequence of the interactions of Aβ and metals, such as copper [44]. It is important to maintain the balance of all metal ions, especially copper, which has redox activity and can produce reactive oxygen species (ROS) involved in oxidative damage. It has been proven that copper plays a critical role in the formation of β-sheet structures, which are considered to be an initial step of the formation of toxic aggregates of the Aβ fibrillar form. Therefore, copper binding to Aβ has been recognized to play an important role in the neurotoxicity of the Aβ [45, 46]. In addition, recent research shows that the amyloid hypothesis is strongly intertwined with copper imbalance because the Aβ precursor (AβPP)/Aβ are probable copper/zinc-binding proteins with a potential role as natural copper/zinc buffering proteins (loss of function), and via the plausible pathogenic role of copper-Aβ [38]. Another genetic theory is further perfecting the generation of the AD copper subtype theory. The study points out that patients with AD fail to maintain a copper metabolic balance and reveals the presence of a percentage of patients with AD carrying the ATP7B AG haplotype and presenting Non-Cp copper excess, which suggests that a subset of subjects with AD is prone to copper imbalance [10].
There is strong evidence tying the ingestion of inorganic copper as a causal factor in AD, and includes AD animal model data where trace amounts of inorganic copper in the drinking water markedly worsened AD. Human studies where the ingestion of copper supplements, along with a high-fat diet, are associated with a marked loss of cognition [47]. Reducing dietary and environmental copper intake is of great significance to prevent the occurrence and development of AD. Numerous animal studies have shown that adding copper to the diet results in significant reductions in memory and cognitive function [48,49,50,51].
In a nutritional study of people in a large Chicago population, the intake of nutrients was studied while cognition was measured over time. It was found that those in the highest quintile of copper intake if they also ate a high-fat diet as many Americans do, lost cognition at several times the rate of other groups [49]. A paper showed that almost all food copper is copper-1; that is, the copper-2 of foods reverts to the reduced copper-1 form at death or harvest. The body has an intestinal transport system for copper-1 and Ctr1, which channels copper-1 through the liver and into safe channels. Ctr1 cannot absorb copper-2, and some copper-2 bypasses the liver, ends up in the blood quickly, and is toxic to cognition. Humans have evolved to handle copper-1 safely, but not copper-2. AD is, at least in part, a copper-2 toxicity disease [52]. The two sources of copper-2 ingestion are drinking water and multimineral supplement pills containing copper. It has been shown that enough copper is leached from copper plumbing in most households to cause AD, using AD animal model studies as a guide to toxic levels [53]. Therefore, the copper content in drinking water and food should be valued.
Air pollution is another important factor contributing to increased copper intake [54]. Copper is one of the main metal elements of the air pollutant PM2.5 [55]. With the increase in environmental pollution, the passive intake of copper from the air has gradually increased [56]. We should pay attention to air pollution and reduce the concentration of heavy metals in the air, as well as reduce the body's excessive intake of copper from the environment.
In this study, the association between whole blood copper levels and the risk of MCI was assessed. The research object was the elderly in the community, whose exposure source was stable and more representative. This study also conducted a stratified analysis to further analyze and explain the association between the whole blood copper levels and the occurrence of MCI in the elderly of different ages and genders. However, this study also has shortcomings. Because the baseline data of the cohort study were used, the causal association between copper exposure and MCI could not be determined. The sample size is still not large, and it is not ruled out that found associations may be accidental. Extrapolation from other populations requires careful interpretation. This result has not yet been validated in a large sample cohort study.
Conclusions
This study shows that the prevalence rate of MCI among the elderly in Lu'an was 20.36%. The geometric mean, standard deviation, median, minimum, and maximum values of copper concentrations in the whole blood of subjects were 0.910 μg/mL, 0.115 μg/mL, 0.772 μg/mL, 0.5391 μg/mL, and 1.1824 μg/mL, respectively. Gender, age, area of residence, education level, smoking, drinking, dysfunction of daily activities, and family income can affect the whole blood copper level of the elderly. The prevalence of MCI was different with regard to gender, age, education level, etc., and a higher copper level in the elderly was significantly related to the occurrence of MCI. The association was stronger in older adults and men.
Availability of data and material
Research data are not shared.
Code availability
Not applicable.
References
Rocca WA, Petersen RC, Knopman DS et al (2011) Trends in the incidence and prevalence of Alzheimer’s disease, dementia, and cognitive impairment in the United States. Alzheimers Dementia 7:80–93
Yamaguchi T, Tabuchi H, Ito D et al (2021) Effect of different parietal hypoperfusion on neuropsychological characteristics in mild cognitive impairment. Psychogeriatrics 21(4):618–626. https://doi.org/10.1111/psyg.12723
Petersen RC, Doody R, Kurz A et al (2001) Current concepts in mild cognitive impairment. Arch Neurol 58:1985–1992
Langa KM, Levine DA (2014) The diagnosis and management of mild cognitive impairment: a clinical review. JAMA 312:2551–2561. https://doi.org/10.1001/jama.2014.13806
Geda YE (2012) Mild cognitive impairment in older adults. Curr Psychiatry Rep 14:320–327. https://doi.org/10.1007/s11920-012-0291-x
Xu S, Xie B, Song M et al (2014) High prevalence of mild cognitive impairment in the elderly: a community-based study in four cities of the Hebei province, China. Neuroepidemiology 42:123–130
Isaacson RS, Hristov H, Saif N et al (2019) Individualized clinical management of patients at risk for Alzheimer’s dementia. Alzheimer’s Dementia 15:1588–1602
Gu L, Yu J, Fan Y et al (2021) The association between trace elements exposure and the cognition in the elderly in China. Biol Trace Elem Res 199:403–412
Tang Z, Chen X, Zhang W et al (2021) Association between gamma-glutamyl transferase and mild cognitive impairment in Chinese women. Front Aging Neurosci 13:630409
Squitti R, Ventriglia M, Simonelli I et al (2021) Copper imbalance in Alzheimer's disease: meta-analysis of serum, plasma, and brain specimens, and replication study evaluating ATP7B gene variants. Biomolecules 11:960. https://doi.org/10.3390/biom11070960
Wang Z, Li N, Heizhati M et al (2021) Association between 24-h urinary sodium to potassium ratio and mild cognitive impairment in community-based general population. Public Health Nutr 24:5795–5804. https://doi.org/10.1017/S1368980021001452
Bai A, Xu W, Sun J et al (2021) Associations of sarcopenia and its defining components with cognitive function in community-dwelling oldest old. BMC Geriatr 21:292
Yee A, Tsui NBY, Kwan RYC et al (2021) Apolipoprotein E gene revisited: contribution of rare variants to Alzheimer's disease susceptibility in Southern Chinese. Curr Alzheimer Res. https://doi.org/10.2174/1567205018666210324111401
Squitti R, Mendez AJ, Simonelli I et al (2017) Diabetes and Alzheimer’s disease: can elevated free copper predict the risk of the disease? J Alzheimers Dis 56:1055–1064
Squitti R, Polimanti R (2013) Copper phenotype in Alzheimer's disease: dissecting the pathway. Am J Neurodegener Dis 2(2):46–56
Morris MC, Evans DA, Tangney CC et al (2006) Dietary copper and high saturated and trans fat intakes associated with cognitive decline. Arch Neurol 63:1085–1088
Rozzini L, Lanfranchi F, Pilotto A et al (2018) Serum non-ceruloplasmin non-albumin copper elevation in mild cognitive impairment and dementia due to Alzheimer’s disease: a case control study. J Alzheimers Dis 61:907–912
Kessler H, Bayer TA, Bach D et al (2008) Intake of copper has no effect on cognition in patients with mild Alzheimer’s disease: a pilot phase 2 clinical trial. J Neural Transm 115:1181–1187
Turnlund JR, Keyes WR, Kim SK et al (2005) Long-term high copper intake: effects on copper absorption, retention, and homeostasis in men. Am J Clin Nutr 81:822–828
Bucossi S, Polimanti R, Mariani S et al (2012) Association of K832R and R952K SNPs of Wilson’s disease gene with Alzheimer’s disease. J Alzheimers Dis 29:913–919
Squitti R (2012) Copper dysfunction in Alzheimer's disease: from meta-analysis of biochemical studies to new insight into genetics. J Trace Elem Med Biol 26(2–3):93–96. https://doi.org/10.1016/j.jtemb.2012.04.012
Wade DT, Collin C (1988) The Barthel ADL Index: a standard measure of physical disability? Int Disabil Stud 10(2):64–67. https://doi.org/10.3109/09638288809164105
Schultz-Larsen K, Lomholt RK, Kreiner S (2007) Mini-Mental Status Examination: a short form of MMSE was as accurate as the original MMSE in predicting dementia. J Clin Epidemiol 60:260–267
Li H, Jia J, Yang Z (2016) Mini-mental state examination in elderly Chinese: a population-based normative study. J Alzheimers Dis 53:487–496
Petersen RC, Smith GE, Waring SC et al (1999) Mild cognitive impairment: clinical characterization and outcome. Arch Neurol 56:303–308
Armbruster DA, Pry T (2008) Limit of blank, limit of detection and limit of quantitation. Clin Biochem Rev 29(Suppl 1):S49–S52
Liang C, Li Z, Xia X et al (2017) Determine multiple elements simultaneously in the sera of umbilical cord blood samples—a very simple method. Biol Trace Elem Res 177:1–8
Jia J, Zhou A, Wei C et al (2014) The prevalence of mild cognitive impairment and its etiological subtypes in elderly Chinese. Alzheimers Dementia 10:439–447
Ding D, Zhao Q, Guo Q et al (2015) Prevalence of mild cognitive impairment in an urban community in China: a cross-sectional analysis of the Shanghai Aging Study. Alzheimers Dementia 11:300–309
Pan Y, Shea YF, Li S et al (2021) Prevalence of mild behavioural impairment: a systematic review and meta-analysis. Psychogeriatrics 21:100–111
Trittschuh EH, Crane PK, Larson EB et al (2011) Effects of varying diagnostic criteria on prevalence of mild cognitive impairment in a community based sample. J Alzheimers Dis 25:163–173
Khedr E, Fawi G, Abbas MAA et al (2015) Prevalence of mild cognitive impairment and dementia among the elderly population of Qena governorate, upper Egypt: a community-based study. J Alzheimers Dis 45:117–126
Pusswald G, Moser D, Gleiss A et al (2013) Prevalence of mild cognitive impairment subtypes in patients attending a memory outpatient clinic-comparison of two modes of mild cognitive impairment classification. Results of the Vienna Conversion to Dementia Study. Alzheimers Dementia 9:366–376
Coelho Vaz FN, Fermino BL, Loch Haskel MV et al (2018) Langoni de Freitas GB, Fabbri R, Montagna E, Teixeira Rocha JB, Bonini JS: the relationship between copper, iron, and selenium levels and Alzheimer disease. Biol Trace Elem Res 181:185–191
Meramat A, Rajab NF, Shahar S et al (2017) DNA damage, copper and lead associates with cognitive function among older adults. J Nutr Health Aging 21:539–545
Zhang Y, Chen Y, Lin Z et al (2014) Ultrasonic oscillation dialysis-graphite furnace atomic absorption spectrometer method for determination of “free” copper and exchangeable copper in serum. Clin Lab 60:543–551
Pal A (2014) Copper toxicity induced hepatocerebral and neurodegenerative diseases: an urgent need for prognostic biomarkers. Neurotoxicology 40:97–101. https://doi.org/10.1016/j.neuro.2013.12.001
Squitti R, Faller P, Hureau C et al (2021) Copper imbalance in Alzheimer’s disease and its link with the amyloid hypothesis: towards a combined clinical, chemical, and genetic etiology. J Alzheimers Dis 83:23–41
Kulichikhin KY, Fedotov SA, Rubel MS et al (2021) Development of molecular tools for diagnosis of Alzheimer’s disease that are based on detection of amyloidogenic proteins. Prion 15:56–69
Yepes M (2021) The plasminogen activating system in the pathogenesis of Alzheimer's disease. Neural Regen Res 16(10):1973–1977. https://doi.org/10.4103/1673-5374.308076
Pannuzzo M (2021) Beta-amyloid pore linked to controlled calcium influx into the cell: a new paradigm for Alzheimer's Disease. Alzheimers Dement. https://doi.org/10.1002/alz.12373
Hung YH, Bush AI, Cherny RA (2010) Copper in the brain and Alzheimer’s disease. J Biol Inorg Chem 15:61–76
Singh I, Sagare AP, Coma M et al (2013) Low levels of copper disrupt brain amyloid-beta homeostasis by altering its production and clearance. Proc Natl Acad Sci USA 110:14771–14776
Johnstone EM, Chaney MO, Norris FH et al (1991) Conservation of the sequence of the Alzheimer’s disease amyloid peptide in dog, polar bear and five other mammals by cross-species polymerase chain reaction analysis. Brain Res Mol Brain Res 10:299–305
Cherny RA, Atwood CS, Xilinas ME et al (2001) Treatment with a copper-zinc chelator markedly and rapidly inhibits beta-amyloid accumulation in Alzheimer’s disease transgenic mice. Neuron 30:665–676
Bush AI (2002) Metal complexing agents as therapies for Alzheimer's disease. Neurobiol Aging 23(6):1031–1038. https://doi.org/10.1016/s0197-4580(02)00120-3
Brewer GJ (2012) Copper toxicity in Alzheimer's disease: cognitive loss from ingestion of inorganic copper. J Trace Elem Med Biol 26(2–3):89–92. https://doi.org/10.1016/j.jtemb.2012.04.019
Sparks DL, Friedland R, Petanceska S et al (2006) Trace copper levels in the drinking water, but not zinc or aluminum influence CNS Alzheimer-like pathology. J Nutr Health Aging 10:247–254
Schreurs BG, Sparks DL (2016) Dietary high cholesterol and trace metals in the drinking water increase levels of ABCA1 in the rabbit hippocampus and temporal cortex. J Alzheimers Dis 49(1):201–209. https://doi.org/10.3233/JAD-150601
Quinn JF, Harris CJ, Cobb KE et al (2010) A copper-lowering strategy attenuates amyloid pathology in a transgenic mouse model of Alzheimer’s disease. J Alzheimers Dis 21:903–914
Yao D, Jing T, Niu L et al (2018) Amyloidogenesis induced by diet cholesterol and copper in a model mouse for Alzheimer’s disease and protection effects of zinc and fluvastatin. Brain Res Bull 143:1–8
Brewer GJ (2015) Copper-2 ingestion, plus increased meat eating leading to increased copper absorption, are major factors behind the current epidemic of Alzheimer's disease. Nutrients 7(12):10053-10064. https://doi.org/10.3390/nu7125513. Erratum in: Nutrients. 2016;8(4). pii:E194. https://doi.org/10.3390/nu8040194
Brewer GJ (2017) Copper-2 hypothesis for causation of the current Alzheimer's disease epidemic together with dietary changes that enhance the epidemic. Chem Res Toxicol 30(3):763–768. https://doi.org/10.1021/acs.chemrestox.6b00373
Fu P, Yung KKL (2020) Air pollution and Alzheimer's disease: a systematic review and meta-analysis. J Alzheimers Dis 77(2):701–714. https://doi.org/10.3233/JAD-200483
Wang X, Nie Y, Chen H et al (2016) Pollution characteristics and source apportionment of PM2.5, in Lanzhou City. Huan jing ke xue Huanjing kexue 37:1619–1628
Xiong QL, Zhao WJ, Guo XY et al (2015) Dustfall heavy metal pollution during winter in North China. Bull Environ Contam Toxicol 95:548–554
Acknowledgements
Thanks to the following people for their contributions to this article, who were key members of the cohort and participated in the survey. School of Public Health, Anhui Medical University: Fangbiao Tao, Sufang Wang, Linsheng Yang, Kaiyong Liu, Qunan Wang, Xiude Li; School of Health Management, Anhui Medical University: Guimei Chen, Dongmei Zhang, Ying Ma, Li Wang; School of Nursing, Anhui Medical University: Annuo Liu; Lu'an Center of Disease Control and Prevention: Hongjuan Cao, Kaichun Li.
Funding
Grants for Major Projects on College Leading Talent Team Introduced of Anhui (0303011224) and National Natural Science Foundation of China (81872662).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The Elderly Health and Environment Risk Factor Cohort strictly followed ethically related procedures. The research scheme was verified by the Ethics Committee of Anhui Medical University. This study was approved by the biomedical ethical committee of Anhui Medical University (No.2017028).
Statements on human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent to participate
All subjects signed informed consent forms to participate in the survey.
Consent for publication
All authors have agreed to be published.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gu, L., Yu, J., He, Y. et al. Blood copper excess is associated with mild cognitive impairment in elderly Chinese. Aging Clin Exp Res 34, 1007–1019 (2022). https://doi.org/10.1007/s40520-021-02034-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-021-02034-3