Abstract
Objective
Our aim was to measure the prevalence of delirium, its clinical features, and outcomes in older patients referred to a memory clinic.
Methods
A retrospective cohort study of 109 older outpatients with delirium referred to a memory clinic with a home care service. Delirium was diagnosed using the confusion assessment method and dementia with the DSM-5 criteria. We collected information on cognitive and functional status, mortality, institutionalization, and hospitalization during 6 months following the delirium episode.
Results
Delirium prevalence was 3.6%, mostly of hyperactive type. Delirium worsened functional (ADL 2.95 ± 1.95 vs. 2.16 ± 1.84) and cognitive (MMSE 13.88 ± 8.96 vs.11.0 ± 9.49) status after 6 months compared to the baseline. The mortality rate was 29.4%, and 28.3% were admitted to a long-term facility after the episode of delirium. Of these patients, more than half were hospitalized during the follow-up. Of the 109 patients with delirium, 85 were managed at home and 24 were hospitalized. Patients who were hospitalized had more severe behavioral symptoms during the delirium episode. There was no difference in mortality and institutionalization according to the home or hospital management.
Conclusions
This retrospective cohort study adds novel information to the existing literature of an understudied setting and population. The study supports the need to further investigate the feasibility and efficacy of the hospital at home models for the prevention and management of delirium in a high-risk population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Delirium is defined as an acute disturbance in attention and cognition that develops over a short period of time and is caused by an underlying clinical condition. Delirium prevalence in the acute hospital ranges from 17 to 50% according to the settings [1]. The occurrence of delirium is associated with adverse outcomes including increased hospital costs, mortality, dementia and worsening of dementia and functional decline [2,3,4,5]. Additionally, it has been shown that delirium is a stressful event for the patients and the caregivers, also in the context of dementia [6,7,8,9].
However, little is known on delirium in the community, with a prevalence ranging from 0.50 to 22% according to the presence of dementia [10,11,12,13]. The largest prospective cohort study included 261 outpatients with dementia followed up in a memory clinic and reported a delirium prevalence of 19.4% at the time of the follow-up visit [12]. Additionally, to date, it is unclear what are the outcomes related to delirium in community settings, how delirium is actually managed and which would be the best approach especially in the context of dementia.
Increasing the knowledge about delirium in the community may be relevant to further develop and test interventions. For example, a recent study reported the feasibility and the acceptability of a nursing intervention to detect and reduce delirium incidence among older adults with mild cognitive impairment discharged from an acute hospital [14].
The aims of this study include: (1) to assess the prevalence of delirium in older outpatients referring to a memory clinic with a home care service; (2) to investigate the clinical characteristics of patients with delirium; (3) to study the association between delirium and negative outcomes at 6-month follow-up including hospitalization, mortality and institutionalization; and (4) to compare clinical characteristics and 6-month outcomes between patients managed at home and in the hospital.
Materials and methods
Setting and patients
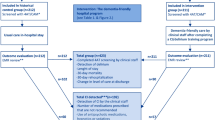
This is a retrospective cohort a study of 109 older patients with cognitive impairment and delirium assessed in a memory clinic with a home care service, Cognitive Disorders and Dementia Unit, Primary Care of Health Authority and Services in Modena (Italy) in 2017. Patients are referred to the memory clinic by a general practitioner as first visit or are evaluated by a geriatrician during a follow-up visit. Moreover the memory clinic can accept General Practitioner’s (GP) fast evaluation request in case of severe cognitive/behavioural changes. After the GP refers the patient to the memory clinic a nurse case manager organizes the evaluation within a maximum of 10 days. A total of 2995 patients with dementia were referred to this service in 2017. We included all older patients who received a diagnosis of delirium detected by a geriatrician in an outpatient clinic consultation or home visits; 76 of these where referred by a GP as fast evaluation or re-evaluation. The Health Trust (AUSL) of Modena approved the study. Informed consent was waved due to the retrospective nature of the study.
Delirium and dementia evaluation
The presence of delirium was diagnosed by trained geriatricians of the memory clinic using the confusion assessment method (CAM) at the moment of the outpatient or at home visit, before administering the cognitive tests [15]. The CAM is a widely used tool with high sensitivity and specificity for delirium detection. The administration takes about 5–10 min. Psychomotor delirium subtypes (i.e. hyperactive, hypoactive, and mixed) were categorized according to the geriatric clinical evaluation.
Cognitive assessment and/or diagnosis of dementia, severity and type of dementia, behavioral symptoms of dementia within 6 months before the occurrence of delirium, at the time of delirium onset and at 6 months were collected using the clinical records of the memory clinic. The presence of dementia was defined according to the DSM-5 criteria [16]. It was possible to ascertain—via the medical records—the cognitive, functional and behavioral measures before the delirium episode only for patients in charge of the memory clinic. The mini-mental state examination, a cognitive screening test that ranges from a minimum of 0 (cognitive functions completely lost) to a maximum of 30 (normal cognitive performances), was collected before the delirium onset, and at 6-month follow-up [17]. The severity of dementia was graded using the Clinical Dementia Rating Scale (CDR) a 3-point scale that ranks different level of dementia with a score of 0 indicative of normal cognitive, 1 questionable cognitive impairment, 1 mild cognitive impairment, 2 moderate cognitive impairment, 3 severe cognitive impairment [18]. CDR were obtained from clinical and anamnestic interview with caregiver. Behavioral and psychological symptoms of dementia were assessed with the neuropsychiatric inventory (NPI) from 0 (absence of behavioral symptoms) to 144 points (maximum severity of behavioral symptoms) [19]. At the time of delirium and at 6-month follow-up were recorded the score of each NPI items, while before the index delirium evaluation it was collected only the total NPI score.
Each patient at every follow-up visit was always evaluated with the CDR and the NPI but the MMSE was not always administered.
Clinical evaluation and management
For every patient, we collected demographic information including age and gender, comorbidity using the CIRS severity index [20]. Functional status was evaluated with the activities of daily living (ADLs) before the occurrence of delirium, at delirium onset and at 6 months [21]. The ADL score ranges from 0 (all functions lost) to 6 (all functions maintained). ADLs before delirium were collected with main caregiver. Delirium etiology was ascertained via the clinical evaluation performed during the geriatric evaluation. We recorded if the patient, after the delirium diagnosis, was managed at home or if the patient was hospitalized.
After the home or clinic evaluation, the geriatrician can order fast-track laboratory exams or instrumental evaluations using a day service. The geriatrician suggests the caregivers a non-pharmacological intervention (e.g., cognitive stimulation and mobilization; support the use of hearing aids or eye glasses) for the patients. The caregiver is sustained by a phone contact with a psychologist for a psychological support, training about delirium and psychosocial intervention. A pharmacological therapy is prescribed only in case of symptoms distressing for patients and when the safety of the patients and other is compromised, as indicated by the most recent guidelines [22, 23]. After the clinical evaluation, the geriatrician plans for a short-, middle- or long-term follow-up according to the complexity and the severity of the clinical situation. The final decision to manage the patient at home or to admit the patient to the hospital was based according to type of clinical problem underlining the occurrence of delirium, unsuccessful therapy or poor caregiver compliance.
Finally, we collected information on mortality status, institutionalization, and hospitalization after the episode of delirium at 6 months via phone interview or in person evaluation at the memory clinic.
Statistical analysis
Continuous variables are presented as mean ± standard deviation, while categorical data as number and proportions. Differences in the NPI items score during and after delirium episode were tested with ANOVA test as the differences in the MMSE, NPI, CDR and ADLs before, during and after the resolution of delirium. Comparison between home and hospital delirium management was performed with Pearson’s Chi-squared test χ2 for categorical data and ANOVA test for continuous data. Differences were assumed to be significant at p < 0.05. Analysis were performed using SPSS (Statistical Package for Social Sciences) version 24.
Results
Out of 2995 patients evaluated in the memory clinic in 2017, 109 (3.64%) were diagnosed with delirium. The mean age was 84.6 ± 7.74 years old, most of them were women and had a moderate comorbidity (Table 1). At the baseline, most of the patients had a dementia diagnosis (86.24%) and 13.76% had mild cognitive impairment. Only 17.4% of patients did not have any previous diagnosis of cognitive impairment at the time of the home or clinic assessment. The mean CDR was 2.36 ± 1.47, indicative of moderate dementia and with relatively minor behavioral symptoms.
Most of the patients had hyperactive delirium (N = 84, 77.1%), followed by the hypoactive (N = 14, 12.8%), and mixed (N = 11, 10.1%) delirium subtypes.
At the moment of delirium, patients worsened the behavioral symptoms of dementia and functional status, as measured with the NPI and ADL, respect to the baseline (Table 1). The precipitating factors were mainly infections or sepsis, followed by pain, respiratory distress or heart failure and multifactorial causes. At the 6-month follow-up, we observed a worsening of the cognitive performance (MMSE before delirium 13.88 ± 8.96; after delirium MMSE 11.0 ± 9.49; CDR before delirium 2.36 ± 1.47 and after delirium 2.73 ± 1.33) and functional performance (ADL before delirium 2.95 ± 1.95; after delirium 2.16 ± 1.84). However, the difference in the ADLs between the time of delirium and after delirium was not statistically significant (Table 2).
Behavioral symptoms improved after the resolution of delirium but the severity was higher compared to the pre-delirium evaluation (NPI before delirium 9.26 ± 9.39; during delirium 34.99 ± 15.91; after delirium 15.82 ± 13.18). The severity of each behavioral symptoms was lower after delirium except for euphoria (Table 3). The mortality rate was 29.36% and 28.3% were admitted to a long-term facility after the episode of delirium. Of these patients more than half were hospitalized in the 6 months after delirium.
Of the 109 patients with delirium, 85 (78%) were managed at home and 24 (22%) were hospitalized (Table 4). In both groups, there was a high prevalence of hyperactive delirium but it was much higher in those hospitalized. We did not detect any statistically significant differences between these two groups regarding the clinical, cognitive and behavioral characteristics before the onset of delirium. Moreover, the two groups did not differ for the type of dementia, neither for precipitant factors for delirium. Patients who were hospitalized had more severe behavioral symptoms compared to those managed at home (NPI 44.04 ± 15.81 vs. 32.44 ± 15.07). We did not find any difference between the groups in the rate of mortality and institutionalization after six months but people with delirium managed at home had higher rates of hospital access after 6 months respect to people managed in the hospital.
Discussion
This is the first study to combine the evaluation of delirium prevalence and outcomes with a longitudinal follow-up in a relatively large sample of older patients referred to a memory clinic with a home care service. We found a relatively low prevalence of delirium with a higher proportion of hyperactive delirium subtype. Behavioral symptoms worsened during the delirium episode and at 6-month follow-up, we detected a decline in cognitive and functional performance compared to the pre-delirium evaluation, although the difference in the functional performances between delirium and delirium resolution was not statistically significant. More than half of these patients were hospitalized in the 6 months after the occurrence of delirium. The majority of the patients were managed at home and only 22% were hospitalized. Those who were hospitalized had significant more severe behavioral symptoms and higher comorbidity, compared to those managed at home. Additionally, those who were hospitalized even at 6-month follow-up still had more severe behavioral symptoms.
To date, relatively few studies have been carried out to investigate the occurrence of delirium at home and its management [10,11,12,13,14]. Two studies were retrospective [10, 13] and one study was prospective [12]. In the retrospective studies, delirium prevalence range from 13.3 to 22%. In the prospective cohort study delirium prevalence was 19.4%. The prevalence in our study is in line with other studies enrolling patients without dementia [11]. However, the lower prevalence of delirium in the population included in our study might also be related to the nature of the study. Indeed the patients referred to our memory clinic were either sent by the primary care physicians or were follow-up visits. Previous reports have underlined how delirium is often underdiagnosed by primary care physicians in home settings due to the possible confusion with dementia, behavioral symptoms of dementia or ageing [11]. It is uncommon for primary care physician to use delirium tools to diagnose delirium. Additional difficulties are related to the ability to diagnose delirium in the advanced stages of dementia [24]. It is well known how the presence of dementia is a significant risk factor for the underdiagnosis of delirium [25]. In the home setting, additional tools might be useful to increase delirium detection. Indeed in patients with advanced dementia functional changes might be an important trigger for a more detailed assessment of the presence of delirium. Previous studies underlined how, especially in the context of dementia, the occurrence of delirium is associated with significant functional changes [26,27,28,29].
Only one study reported the actual prevalence of delirium according to the type of dementia with a higher prevalence in vascular dementia, followed by Lewy body dementia and Alzheimer dementia [12]. In our study, we found a similar pattern though we also detected cases of delirium in patients with fronto-temporal dementia and Parkinson dementia.
The findings of a higher severity of behavioral symptoms in delirious patients have also been described in previous reports [12, 30]. Indeed during the delirium phase, patients with delirium and dementia have a greater severity of behavioral symptoms. However, in our study, we were also able to detect the changes in the severity of behavioral symptoms before and after the delirium episodes showing that indeed patients who experience delirium, worsen their behavioral symptoms, and their cognitive functions after the delirium resolution. The worsening of cognitive performances after an episode of delirium has been previously described and it should not be underestimated even in the context of home settings [3]. A recent trial has been carried out to evaluate the feasibility and acceptability of a nursing intervention to reduce the burden of delirium in the home settings [14]. Several studies have now been published in the acute settings and there is a strong evidence of the possibility to prevent delirium [31]. However, no data are currently available in the home settings and future studies are required in high-risk population. For instance, a novel and integrative approach involves occupational therapists. Indeed occupational therapy interventions have been proven to be effective in improving behavioral symptoms of dementia in home settings and are feasible for the management of patients with delirium and dementia in nursing homes [32,33,34].
To the best of our knowledge, our study is the first one to investigate the etiology of delirium and to study the characteristics and the outcomes of patients managed at home vs. those hospitalized. Patients hospitalized had a higher severity of behavioral symptoms, greater comorbidity and probably a greater clinical instability given the higher prevalence of infection and sepsis and mortality. However, this is a speculation since we do not have measure of clinical instability to support this hypothesis. On another note, it might be that these patients have been delirious for a longer period of time and that delirium was misdiagnosed as dementia or as a behavioral symptoms of dementia leading to a delayed treatment. Delirium is considered a medical emergency since often, especially in frail patients, is the only manifestation of a serious underlying clinical condition and a misdiagnosis can lead to increase mortality [35]. It should also be noticed that the majority of patients were managed at home leading us to consider potential different approaches for the prevention and management of delirium in home settings in high-risk patients. For instance, a previous study reported how patients in whom delirium was not detected during an emergency department (ED) visit had higher 6-month mortality [36]. We do not know if patients with more severe symptoms had for example a recent hospitalization or ED visit. Therefore, studies are required to further understand the applicability and efficacy on delirium detection and management of patients with moderate–severe dementia with the new models of the hospital at home given the current preliminary evidences [37,38,39].
Our study has important strength along with limitations. This is the first study to combine the evaluation of delirium prevalence, outcomes with a longitudinal follow-up in a relatively large sample of older patients referred to a memory clinic with a home care service. The limitations include the possible bias in the diagnosis of delirium due to the retrospective nature of the study and the limited information on previous access to hospitalization or emergency visit wards before the delirium episode. Additionally, it is possible that cases of delirium were not referred to the memory clinic by the general practitioner since they were considered as behavioral symptoms of dementia. Finally, we did not include a cohort of patients with dementia but without delirium. Future prospective studies are necessary to elucidate the effect of delirium and its management in this frail population.
Conclusions
This retrospective cohort study adds novel information to the existing literature of an understudied setting and population. We found a relatively low prevalence of delirium compared to other studies. Patients with delirium after the delirium episode had lower cognitive and functional performances with worse behavioral symptoms than before the delirium episode. Patients managed at home had a lower mortality after the delirium episode although non-statistically significant and higher rate of hospitalization at 6-month follow-up. The study provides initial insights on the possible role of home management of delirium superimposed on dementia. Future studies are warranted to investigate the feasibility and efficacy of the hospital at home models for the prevention and management of delirium in a high-risk population.
References
Inouye SK, Westendorp RG, Saczynski JS (2014) Delirium in elderly people. Lancet 383:911–922
Eeles EM, Hubbard RE, White SV et al (2010) Hospital use, institutionalisation and mortality associated with delirium. Age Ageing 39:470–475
Davis DH, Muniz Terrera G, Keage H et al (2012) Delirium is a strong risk factor for dementia in the oldest-old: a population-based cohort study. Brain J Neurol 135:2809–2816
Morandi A, Davis D, Fick DM et al (2014) Delirium superimposed on dementia strongly predicts worse outcomes in older rehabilitation inpatients. J Am Med Dir Assoc 15:349–354
Morandi A, Di Santo SG, Zambon A et al (2019) Delirium, dementia, and in-hospital mortality: the results from the Italian Delirium Day 2016, a national multicenter study. J Gerontol Ser Biol Sci Med Sci 74:910–916
Morandi A, Lucchi E, Turco R et al (2015a) Delirium superimposed on dementia: a quantitative and qualitative evaluation of informal caregivers and health care staff experience. J Psychosom Res 79:272–280
Morandi A, Lucchi E, Turco R et al (2015b) Delirium superimposed on dementia: a quantitative and qualitative evaluation of patient experience. J Psychosom Res 79:281–287
Fong TG, Racine AM, Fick DM et al (2019) The caregiver burden of delirium in older adults with Alzheimer disease and related disorders. J Am Geriatr Soc 67:2587–2592
Grossi E, Lucchi E, Gentile S et al (2019) Preliminary investigation of predictors of distress in informal caregivers of patients with delirium superimposed on dementia. Aging Clin Exp Res 32:339–344
Lerner AJ, Hedera P, Koss E et al (1997) Delirium in Alzheimer disease. Alzheimer Dis Assoc Disord 11:16–20
de Lange E, Verhaak PF, van der Meer K (2013) Prevalence, presentation and prognosis of delirium in older people in the population, at home and in long term care: a review. Int J Geriatr Psychiatry 28:127–134
Hasegawa N, Hashimoto M, Yuuki S et al (2013) Prevalence of delirium among outpatients with dementia. Int Psychogeriatr IPA 25:1877–1883
Addesi D, Maio R, Smirne N et al (2018) Prevalence of delirium in a population of elderly outpatients with dementia: a retrospective study. J Alzheimer’s Dis 61:251–257
Verloo H, Goulet C, Morin D et al (2016) Nursing intervention versus usual care to improve delirium among home-dwelling older adults receiving homecare after hospitalization: feasibility and acceptability of a randomized controlled trail. BMC Nurs 15:19
Inouye SK, van Dyck CH, Alessi CA et al (1990) Clarifying confusion: the confusion assessment method A new method for detection of delirium. Ann Intern Med 113:941–948
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Hughes CP, Berg L, Danziger WL et al (1982) A new clinical scale for the staging of dementia. Br J Psychiatry J ment Sci 140:566–572
Cummings JL, Mega M, Gray K et al (1994) The neuropsychiatric inventory: comprehensive assessment of psychopathology in dementia. Neurology 44:2308–2314
Parmelee PA, Thuras PD, Katz IR et al (1995) Validation of the Cumulative Illness Rating Scale in a geriatric residential population. J Am Geriatr Soc 43:130–137
Katz S (1983) Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc 31:721–727
Bellelli G, Morandi A, Trabucchi M et al (2018) Italian intersociety consensus on prevention, diagnosis, and treatment of delirium in hospitalized older persons. Intern Emerg Med 13:113–121
Network SIG: Risk reduction and management of delirium. https://www.sign.ac.uk/sign-157-delirium.html.
Morandi A, Davis D, Bellelli G et al (2017) The diagnosis of delirium superimposed on dementia: an emerging challenge. J Am Med Dir Assoc 18:12–18
Inouye SK, Foreman MD, Mion LC et al (2001) Nurses’ recognition of delirium and its symptoms: comparison of nurse and researcher ratings. Arch Intern Med 161:2467–2473
Gual N, Richardson SJ, Davis DHJ, Bellelli G, Hasemann W, Meagher D, Kreisel SH, MacLullich AMJ, Cerejeira J, Inzitari M, Morandi A (2019) Impairments in balance and mobility identify delirium in patients with comorbid dementia. Int Psychogeriatr. 31(5):749–753. https://doi.org/10.1017/S1041610218001345
Richardson SJ, Davis DHJ, Bellelli G et al (2017) Detecting delirium superimposed on dementia: diagnostic accuracy of a simple combined arousal and attention testing procedure. Int Psychogeriatr 29(10):1585–1593
Morandi A, Han JH, Meagher D et al (2016) Detecting delirium superimposed on dementia: evaluation of the diagnostic performance of the Richmond Agitation and Sedation Scale. J Am Med Dir Assoc 17:828–833
Bellelli G, Speciale S, Morghen S et al (2011) Are fluctuations in motor performance a diagnostic sign of delirium? J Am Med Dir Assoc 12:578–583
Landreville P, Voyer P, Carmichael PH (2013) Relationship between delirium and behavioral symptoms of dementia. Int Psychogeriatr IPA 25:635–643
Siddiqi N, Harrison JK, Clegg A et al (2016) Interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev 3:5563
Pozzi C, Tatzer VC, Alvarez EA et al (2020) The applicability and feasibility of occupational therapy in delirium care. Eur Geriatr Med 11:209–216
Pozzi C, Lanzoni A, Lucchi E et al (2020) Activity-based occupational therapy intervention for delirium superimposed on dementia in nursing home setting: a feasibility study. Aging Clin Exp Res 32:827–833
Pozzi C, Lanzoni A, Lucchi E et al (2018) A pilot study of community-based occupational therapy for persons with dementia (COTID-IT Program) and their caregivers: evidence for applicability in Italy. Aging Clin Exp Res 31(9):1299–1304
Holtta E, Laakkonen ML, Laurila JV et al (2011) The overlap of delirium with neuropsychiatric symptoms among patients with dementia. Am J Geriatr Psychiatry 19:1034–1041
Kakuma R, du Fort GG, Arsenault L et al (2003) Delirium in older emergency department patients discharged home: effect on survival. J Am Geriatr Soc 51:443–450
Caplan GA, Coconis J, Board N et al (2006) Does home treatment affect delirium? A randomised controlled trial of rehabilitation of elderly and care at home or usual treatment (The REACH-OUT trial). Age Ageing 35:53–60
Tibaldi V, Aimonino N, Ponzetto M et al (2004) A randomized controlled trial of a home hospital intervention for frail elderly demented patients: behavioral disturbances and caregiver’s stress. Arch Gerontol Geriatr Suppl 9:431–436
Chia J, Eeles EM, Tattam K et al (2020) Outcomes for patients with delirium receiving hospital-in-the-home treatment: an Australian perspective. Australas J Ageing 39(2):e215–e219
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The Health Trust (AUSL) of Modena approved the study.
Statement of human and animal rights
The study was conducted in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Manni, B., Federzoni, L., Zucchi, P. et al. Prevalence and management of delirium in community dwelling older people with dementia referred to a memory clinic. Aging Clin Exp Res 33, 2243–2250 (2021). https://doi.org/10.1007/s40520-020-01753-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01753-3