Abstract
Background
The management of older and multimorbid patients with complex care requires a personalised and comprehensive approach. The main diagnosis is often registered as the cause of hospitalisation, yet poor health-related quality of life (HRQoL) as well as multimorbidity may represent the underlying cause and markedly influence prognosis.
Aims
To analyse the association of HRQoL and clinical prognosis over time as assessed by a Comprehensive Geriatric Assessment (CGA)-based Multidimensional Prognostic Index (MPI) in older patients admitted to the emergency department (ED).
Methods
We used data from the prospective MPI–HOPE (Influence of the MPI on the Hospitalisation of Older Patients admitted to the Emergency department) study. Data from 165 patients (≥ 75 years) admitted to the ED of the University Hospital of Cologne, Germany, between Oct 2017 and Jan 2018 were included. Clinical prognosis was calculated by the MPI and HRQoL by the EQ5D-5L. Follow-up interviews assessed HRQoL up to 6 months after discharge.
Results
Most patients were multimorbid and presented with several geriatric syndromes. At admission, HRQoL was highest in patients with the best clinical prognosis. The MPI showed a negative correlation with the EQ-Index at admission (rs(86) = − 0.50, p < 0.0001) and follow-up assessments after 3 and 6 months (rs(86) = − 0.55 and rs(86) = − 0.47, p < 0.0001).
Discussion
Our results suggest that patients’ self-perceived HRQoL in the ED is related to functional health status and clinical prognosis.
Conclusion
The MPI as a multidimensional snapshot provides information on clinical health indicators and informs about subjective HRQoL, thereby helping in identifying patients who would benefit from a specific treatment within the frame of a patient-centered, value-based care strategy geriatric treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
One of the biggest challenges for worldwide healthcare systems is the ongoing demographic change, with the increase in older patients with complex care needs requiring personnel and economic resources [1]. Older patients in the emergency department (ED) tend to present with typically multifactorial conditions. These are often related to underlining frailty in domains beyond the physical. Multifactoriality and frailty in multiple domains often do escape organ medicine-related usual care, particularly in settings like EDs where high-performance actions are in high demand [2, 3]. Psychiatric, social and functional deficits may accompany patients’ trajectories, influencing post-ED management and outcomes [4,5,6]. One way to fill the gap between management needs in advanced age and optimal care efficiency is the use of the Comprehensive Geriatric Assessment (CGA) [7, 8]. This, however, poses important organisational issues [9] and to date the CGA is largely underused in EDs, including those in Germany [5]. Furthermore, the effectiveness of recommended screening instruments for older patients in the ED like the Identification of Seniors at Risk Score (ISAR) is currently under debate [4, 5]. As a consequence of the traditional “one cause-one disease-one treatment” approach [10, 11], the main diagnosis of older adults is therefore still often registered as the cause of hospitalisation.
Health-related quality of life (HRQoL) [12] measured by the European Quality of life-5 Dimensions (EQ5D) by the EuroQol group [13] is well established in geriatric populations and shows good interaction and discriminative ability of geriatric conditions [14, 15]. Considering HRQoL could strengthen the personalised approach recognising both health and well-being.
The present study was designed to evaluate the long-term relationship between multidimensional health measured by means of a CGA-based prognosis evaluation and HRQoL measured by the EQ5D in older patients admitted to the ED of a large German metropolitan hospital.
Patients and methods
Study design and participants
The observational longitudinal study “Influence of the Multidimensional Prognostic Index (MPI) on the Hospitalisation of Older Patients admitted to the Emergency department—The MPI_HOPE study”, registered at the German Clinical Trials Register (DRKS00012694) complies with the ethical rules for human experimentation that are stated in the Declaration of Helsinki (1983). The study was approved by the Ethical Committee of the University Hospital of Cologne, Germany. Inclusion criteria were age 75 years and older, willingness/ability to consent and admission during the quartile between 18 October 2017 and 17 January 2018. Patients aged less than 75 years, visited outside the above cited time window and those unwilling/unable to consent were excluded from the study. All patients or proxy respondents gave written informed consent to participate after a personal conversation with the study doctor and adequate time for questions and decision-making.
Of the 1071 older patients admitted during the recruitment window, an average of 2–3 patients per recruitment day formally agreed to participate. Out of 215 consecutive participants who signed the informed consent, 165 with complete datasets were included in the present analysis.
Assessment
After giving informed consent, patients underwent a CGA-based calculation of the MPI [16,17,18,19], chosen for its clinimetric properties and its correlation to several key performance indicators [20, 21]. HRQoL was measured by the German 5-level EQ5D version. The first part provides a questionnaire addressing five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) that are rated on a Likert scale for this particular day (1 = no problems, 2 = slight problems, 3 = moderate problems, 4 = severe problems and 5 = extreme problems/unable to do). The dimensions can be analysed separately or combined into an index, using population-based preference weights. This study used the German value set from Ludwig et al. [22], which allows for the calculation of an index score that ranges from − 0.66 over 0 (death) to 1 (full health). Negative index values are rated as a health state being worse than death. The second part consists of a visual analogue scale (VAS), giving the interviewees the opportunity to estimate their current overall health status that day on a scale from 0 to 100 (0 = worst and 100 = best imaginable health).
The MPI combines information of eight different domains from widely used assessments: daily dependence by Katz’s Activities of Daily Living (ADL) [23], the Lawton’s Instrumental Activities of Daily Living (IADL) [24], comorbidities by the Cumulative Illness Rating Scale (CIRS) [25], pressure ulcer risk by the Exton-Smith Scale (ESS) [26], nutrition by the Mini Nutritional Assessment Short Form (MNA-SF) [27], cognition by the Short Portable Mental Status Questionnaire (SPMSQ) [28] and additional information on social living conditions and number of prescribed drugs. The summarised MPI ranges from 0 indicating the lowest risk of mortality to 1 indicating the highest risk. It can additionally be classified into three risk groups: low risk MPI-1 (0–0.33), moderate risk MPI-2 (0.34–0.66) and high risk MPI-3 (0.67–1). For the assessment and definition of geriatric syndromes, liberal criteria were applied to reflect common clinical conditions in geriatric patients in line with previous literature [29, 30]
Follow-up
In follow-up interviews via phone three and six months after recruitment, the EQ5D was applied to measure changes in HRQoL. Additionally, information about the length of the initial hospital stay (LHS) after the ED visit was obtained.
Registration, participant consent and ethics
Statistical analysis
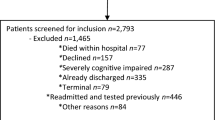
In the present analysis, we included n = 165 patients with complete assessments of both MPI and EQ5D-5L assessment at recruitment. Patients with incomplete HRQoL follow-up assessment were excluded from the follow-up analysis. Lost to follow-up was defined as participants who died during the follow-up, refused to continue participation or were not contactable via phone. A study patient flow chart is shown in Fig. 1.
Study flow chart. Out of n = 215 patients who were enrolled in the MPI_HOPE study, a subsample of n = 165 patients with complete MPI and HRQoL assessment was used for analysis at baseline. The flow chart illustrates the number of patients included in the analysis at the three different time points and provides information about the number and reasons for exclusions
All statistical analyses were performed with SPSS Statistics 25.0 (IBM Corp., Armonk, NY) for Windows. General characteristics are expressed using absolute numbers and relative frequencies for description of categorial variables. The Kolmogorov–Smirnov test was used to test for normal distribution and indicated that all variables used in this analysis were non-normally distributed. Therefore, the median (Mdn) and interquartile range (IQR) were reported for ordinal and continuous variables. We tested for differences between MPI risk groups and compared characteristics of patients who were lost to follow-up with those who remained in the study using nonparametric methods. Pairwise comparisons were carried out using Bonferroni-corrected post hoc tests.
To analyse the differences in HRQoL ratings over the study observation time (Admission, FU1 after three months, FU2 after 6 months), the Friedman test was carried out. Partial Spearman correlations were calculated to analyse the relationship between the MPI score on admission and EQ-Index score as well as the VAS score at different time points. To further analyse the association, linear regression analyses were carried out using the MPI score as the predictor for EQ-Index score and VAS score after adjusting for age and sex at admission, FU1 and FU2. To create an integer scale, the MPI score was multiplied by 10. In addition, the relationship between the geriatric syndromes assessed at admission with HRQoL was analysed. The analyses were adjusted for sex and age. We corrected for multiple testing using Bonferroni correction.
Results
Characteristic of study population
The demographic and clinical characteristics of the sample at admission and categorised by MPI groups are described in Table 1.
Eighty-four patients were classified into the low-risk (MPI-1), 70 into the moderate-risk (MPI-2) and 11 into the high-risk group (MPI-3). The majority of patients was male (59.4%) and only MPI-2 group had significantly fewer male than female patients in comparison with the MPI-1 group (p = 0.016). The median age was 80 (IQR = 77.5–84) years, the MPI risk groups did not differ significantly in age. The mean number of diagnoses was 8 (IQR = 5–11); the number of diagnoses was significantly associated with the MPI group (p < 0.01). The number of geriatric syndromes at admission (Mdn = 4, IQR = 3–5) was significantly associated with the MPI group (p < 0.001). The most frequent geriatric syndromes were sensorial impairment (81.7%), polypharmacy (77.6%) and fluid or electrolyte imbalance (37.2%).
The length of hospital stay after ED admission was Mdn = 4 days (IRQ = 4–11.5), the MPI groups did not differ significantly in the number of in-hospital days (p = 0.07). In total, 13.9% of the patients were discharged home.
The most frequent main diagnoses given at the ED concerned diseases of the heart (33.9%), followed by neurological (13.9%) and musculoskeletal (13.3%) disorders.
Follow-up results
When comparing admission characteristics of the subjects who were lost to follow-up with those who underwent all FU assessments, the former displayed a significantly higher MPI (Mdn = 0.38, IQR = 0.31–0.5 vs. Mdn = 0.31, IQR = 0.25–0.38; U = 4527.50, p < 0.001) and older age (Mdn = 81 years, IQR = 78–86 years vs. Mdn = 79.5 years, IQR = 77–82.3 years; U = 4094.50, p < 0.05) than the latter group.
HRQoL analysis
The EQ-Index and the VAS score were non-normally distributed according to Kolmogorov–Smirnov test. Therefore, a nonparametric Friedman test was carried out to analyse the progression over time and revealed that both scores differed between the measurement time points (EQ-Index: χ2(2) = 6.96, p < 0.05; VAS score: χ2(2) = 14.37, p < 0.001). Post hoc testing indicated that the VAS score after 6 months (FU2) was significantly higher compared to admission (p = 0.001), but not to FU1 after 3 months; there was no significant difference between admission and FU1. The results were similar for the EQ-Index at 6 months compared to admission (p < 0.05). The results are presented in Fig. 2. The number of geriatric syndromes correlated negatively with the EQ-Index [rs(149) = − 0.35, p < 001] and the VAS [rs(149) = − 0.17, p < 0.05] at admission. However, the correlation between the number of geriatric syndromes and the VAS missed significance level after Bonferroni correction.
Boxplot of the self-reported HRQoL as reported on EQ5D Index (a) and visual analogue scale (VAS) (b) over the course of the study visits (admission, FU1 after 3 months, FU2 after 6 months), showing the median. Whiskers extend 1.5 times the interquartile range from the 25th and 75th percentiles, and outliers are represented by dots. Higher scores on EQ5D Index and VAS indicate higher self-reported HRQoL. Patients reported significantly higher HRQoL at FU2 compared to admission on the EQ-Index and the VAS
Associations of HRQoL and MPI
The Kruskal–Wallis test used to assess differences in HRQoL at admission between MPI risk groups revealed that groups differed significantly in self-reported HRQoL as reported on the VAS (H = 13.17, p = 0.001) and measured with the EQ-Index (H = 34.45, p < 0.001). Dunn–Bonferroni post hoc tests showed that self-reported HRQoL was lower in the MPI-2 group compared to the MPI-1 group (p < 0.01). There was a trend for a lower self-reported HRQoL in the MPI-3 group compared to the MPI-1 group; however, this difference did not reach statistical significance after correcting for multiple testing (p = 0.073). For the EQ-Index, the measured HRQoL was higher in MPI-1 in comparison with both the MPI-2 (p < 0.001) and MPI-3 group (p < 0.001). The results are plotted in Fig. 3.
Boxplot of the self-reported HRQoL as reported on the EQ-Index (a) and visual analogue scale (VAS) (b) for each MPI risk group, showing the median. Whiskers extend 1.5 times the interquartile range from the 25th and 75th percentiles, and outliers are represented by dots. Higher scores on EQ5D Index and visual analogue scale indicate higher self-reported HRQoL. a Patients in low-risk group MPI-1 reported significantly higher HRQoL on the EQ-Index compared to patients in the moderate-risk (MPI-2) and high-risk (MPI-3) groups. b Patients in MPI-1 group reported significantly higher HRQoL on the VAS compared to patients in MPI-2
Partial Spearman correlation analysis revealed that the MPI showed a moderate to strong negative correlation with the VAS as well as with the EQ-Index at admission and both FU visits. As expected, the HRQoL measures correlated highly with each other. The results are presented in Table 2. Linear regression analyses indicated that the MPI was associated with the EQ-Index and VAS at all three time points. At admission, a decimal point increase on the MPI implied a decrease of 0.09 points on the EQ-Index (p < 0.0001). For the VAS, an increase of one decimal unit on the MPI at admission corresponded to a decrease of 3.83 points on the VAS (p = 0001). Detailed results for FU1 and FU2 are shown in Table 3.
Discussion
The main result of the present study is that HRQoL as assessed by the EQ5D was significantly associated with clinical prognosis in older multimorbid patients admitted to the ED. Clinical prognosis, as indicated by the MPI, had a moderate to strong correlation with HRQoL at assessment and up to 6 months later. The results of linear regression analyses support this association at all three time points adjusted for age and sex. Patients with a poor health status as indicated by the MPI group classification tended to report lower general and specific HRQoL indicated by the EQ-Index and VAS than patients with a better MPI score. These results indicate that clinical prognosis assessed by the MPI is related to the patients’ self-perceived HRQoL at admission to the ED and after hospital discharge.
In line with our findings, a recent meta-analysis by Kojima et al. [31] on community-dwelling older people emphasized a negative association of a multidimensional frailty status and multiple HRQoL questionnaires. Furthermore, low self-rated HRQoL measured by the EQ5D at hospital admission has been linked to increased mortality and functional decline after discharge [32]. Consistent with other studies examining the HRQoL after an episode of emergency illness, we observed a significant increment from baseline to follow-up indicated by the EQ-Index and VAS [33, 34].
While the main diagnosis was often registered as the reason for admission to the ED, most patients presented a background of multimorbidity, with a median of four geriatric syndromes and eight different diagnoses. In addition, we found that the number of geriatric syndromes correlated negatively with HRQoL as indicated by the EQ-Index, although the observed association was weak and the correlation with the VAS missed significance level after Bonferroni correction.
Underlying multimorbidity as well as geriatric syndromes and related impact on quality of life might be important determinants of patients’ trajectories and might substantially add to the traditional organ-centred approach [30, 35,36,37]. Following disease-specific care can conflict with patients’ values and preferences and might even lead to harm [37,38,39]. Reasons for this clinical practice are mostly unclear responsibilities and lack of geriatric training [40]. Therefore, to improve prognosis and strengthen therapeutic adherence, a more complex and elaborated approach than one-disease-one-treatment is recommended [41]. Only a structured CGA can enable coordinated, integrated care planning for the treatment and long-term follow-up care of older people [42], more so if accompanied by the assessment of patients’ perspective [43]. Our findings provide further insight into the relationship between HRQoL and clinical prognosis due to multimorbidity as indicated by the MPI score.
There are limitations to our study. The study sample was relatively small, and patients with worse clinical status may have been more likely to reject participation in the study. In addition, we only used data from patients with complete MPI and EQ5D questionnaires. Patients who were unable to complete the assessment likely had worse health or cognitive status. Taken together, this may have introduced selection bias and could be an explanation for the low number of participants in MPI-3 compared to MPI-1 and MPI-2. The low number of high-risk patients may also have impacted statistical power to detect differences between the MPI groups.
Furthermore, while HRQoL was measured at admission and on two follow-up time points, the design of the study did not enable us to collect information on HRQoL before admission to the ED. Therefore, we cannot compare HRQoL before and after the ED visits, which limits the interpretation of the progression of HRQoL over time. Being in a stressful environment such as the ED with an acute medical condition could likely bias HRQoL ratings [33]. However, we found the strongest correlation of the MPI with HRQoL at 3 months after ED visit, where we can assume a decreased influence of the initial ED visit. Looking at the components of both indices, the correlation might be explained by similar targets like mobility, self-care and daily activities. Nevertheless, both questionnaires aim to address a different purpose: whereas the MPI is applied to constitute an objective multidimensional assessment of the patients’ overall clinical status, the EQ5D is intended to evaluate the patients’ self-perceived rating of their health. The relationship between both scales shows that the MPI assessment mirrors the patients’ subjective evaluation of their health status.
Assessing and addressing HRQoL elaborately is rarely feasible in clinical practice due to time and resource constraints, especially in the ED. However, given that our data suggests that HRQoL is related to clinical prognosis, patients would likely benefit from additional assessment of HRQoL-related factors to support a holistic treatment that considers both health and well-being in the management of geriatric care. The MPI’s ability to address HRQoL is limited, but our study shows that the MPI as a multidimensional snapshot of the patient can nevertheless provide insight into the patients self-perceived health status. A trained person could assess the full MPI in 20–30 min. This qualifies this prognostic instrument as a substitute for a CGA-like assessment at an early stage of treatment. Further studies are needed to evaluate the feasibility and effectiveness of the MPI in the clinical setting of an ED. This kind of multidimensional examination might improve personalised treatment of the older multimorbid acutely ill person through tailored intervention. Anticipating geriatric needs and fostering prevention could aid the management of multimorbidity, avoid hospitalisation and institutionalisation, improve self-reliance and ultimately, quality of life.
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
European Commission (2017) Directorate General for Health and Food Safety. State of health in the EU: companion report, Publications Office. https://doi.org/10.2875/684855
Schüling K (2018) Kodierhandbuch Geriatrie (2018). In: Geriatrie B (ed) Schüling Verlag, Münster
Dent E, Hoogendijk EO, Cardona-Morrell M et al (2016) Frailty in emergency departments. Lancet 387:434
Carpenter CR, Shelton E, Fowler S et al (2015) Risk factors and screening instruments to predict adverse outcomes for undifferentiated older emergency department patients: a systematic review and meta-analysis. Acad Emerg Med 22:1–21. https://doi.org/10.1111/acem.12569
Weinrebe W, Schiefer Y, Weckmüller K et al (2019) Does the identification of seniors at risk (ISAR) score effectively select geriatric patients on emergency admission? Aging Clin Exp Res 31:1839–1842
Aminzadeh F, Dalziel WB (2002) Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med 39:238–247
Ellis G, Gardner M, Tsiachristas A et al (2017) Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev 9:CD006211. https://doi.org/10.1002/14651858.CD006211.pub3
Ellis G, Whitehead MA, Robinson D et al (2011) Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ 343:d6553
Gladman JR, Conroy SP, Ranhoff AH et al (2016) New horizons in the implementation and research of comprehensive geriatric assessment: knowing, doing and the ‘know-do’gap. Age Ageing 45:194–200
Polidori MC (2019) Geriatrics’ turning point. Springer, Berlin
Meyer AM, Polidori MC (2019) Including prognosis evaluation in the management of older patients across different healthcare settings: the cologne experience. Geriatr Care 5:8663
Guyatt GH, Feeny DH, Patrick DL (1993) Measuring health-related quality of life. Ann Intern Med 118:622–629
Herdman M, Gudex C, Lloyd A et al (2011) Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 20:1727–1736
Brazier J, Walters S, Nicholl J et al (1996) Using the SF-36 and Euroqol on an elderly population. Qual Life Res 5:195–204
Lutomski JE, Krabbe PF, Bleijenberg N et al (2017) Measurement properties of the EQ-5D across four major geriatric conditions: findings from TOPICS-MDS. Health Qual Life Outcomes 15:45
Pilotto A, Ferrucci L, Franceschi M et al (2008) Development and validation of a multidimensional prognostic index for one-year mortality from comprehensive geriatric assessment in hospitalized older patients. Rejuvenation Res 11:151–161
Warnier R, Van Rossum E, Velthuijsen E et al (2016) Validity, reliability and feasibility of tools to identify frail older patients in inpatient hospital care: a systematic review. J Nutr Health Aging 20:218–230
Pilotto A, Rengo F, Marchionni N, group F-Ss et al (2012) Comparing the prognostic accuracy for all-cause mortality of frailty instruments: a multicentre 1-year follow-up in hospitalized older patients. PLoS ONE 7:e29090
Dent E, Kowal P, Hoogendijk EO (2016) Frailty measurement in research and clinical practice: a review. Europ J Intern Med 31:3–10
Polidori MC (2017) Target and patient-oriented care using the comprehensive geriatric assessment: prognosis estimation for clinical decisions with elderly patients. Z Gerontol Geriatr 50:706–709
Meyer AM, Becker I, Siri G et al (2019) New associations of the Multidimensional Prognostic Index. Z Gerontol Geriatr 52:460–467. https://doi.org/10.1007/s00391-018-01471-6
Ludwig K, von der Schulenburg J-MG, Greiner W (2018) German value set for the EQ-5D-5L. PharmacoEconomics 36:663–674
Katz S, Downs TD, Cash HR et al (1970) Progress in development of the index of ADL. Gerontol 10:20–30
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontol 9:179–186
Linn BS, Linn MW, Gurel L (1968) Cumulative illness rating scale. J Am Geriatr Soc 16:622–626
Bliss M, McLaren R, Exton-Smith A (1966) Mattresses for preventing pressure sores in geriatric patients. Monthly Bull Minist Health Public Health Lab Serv 25:238
Sancarlo D, D’Onofrio G, Franceschi M et al (2011) Validation of a Modified-Multidimensional Prognostic Index (m-MPI) including the Mini Nutritional Assessment Short-Form (MNA-SF) for the prediction of one-year mortality in hospitalized elderly patients. J Nutr Health Aging 15:169–173
Pfeiffer E (1975) A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 23:433–441
Kane RL, Shamliyan T, Talley K et al (2012) The association between geriatric syndromes and survival. J Am Geriatr Soc 60:896–904
Meyer AM, Becker I, Siri G et al (2020) The prognostic significance of geriatric syndromes and resources. Aging Clin Exp Res 32:115–124. https://doi.org/10.1007/s40520-019-01168-9
Kojima G, Iliffe S, Jivraj S et al (2016) Association between frailty and quality of life among community-dwelling older people: a systematic review and meta-analysis. J Epidemiol Community Health 70:716–721
Parlevliet JL, MacNeil-Vroomen J, Buurman BM et al (2016) Health-related quality of life at admission is associated with postdischarge mortality, functional decline, and institutionalization in acutely hospitalized older medical patients. J Am Geriatr Soc 64:761–768
Chin MH, Jin L, Karrison TG et al (1999) Older patients’ health-related quality of life around an episode of emergency illness. Ann Emerg Med 34:595–603
Ali TF, Warkentin LM, Gazala S, Care A, Group ES et al (2015) Self-Reported outcomes in individuals aged 65 and older admitted for treatment to an acute care surgical service: a 6-month prospective cohort study. J Am Geriatr Soc 63:2388–2394
Andreasen J, Gobbens RJ, Eriksen HH et al (2019) Health-related quality of life at hospital discharge as a predictor for 6-month unplanned readmission and all-cause mortality of acutely admitted older medical patients. Qual Life Res 28:3015–3024
Hutchinson AF, Graco M, Rasekaba TM et al (2015) Relationship between health-related quality of life, comorbidities and acute health care utilisation, in adults with chronic conditions. Health Qual Life Outcomes 13:69
Boyd CM, Darer J, Boult C et al (2005) Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA 294:716–724
Fried TR, McGraw S, Agostini JV et al (2008) Views of older persons with multiple morbidities on competing outcomes and clinical decision-making. J Am Geriatr Soc 56:1839–1844
Lorgunpai SJ, Grammas M, Lee DS et al (2014) Potential therapeutic competition in community-living older adults in the US: use of medications that may adversely affect a coexisting condition. PLoS ONE 9:e89447
Williams BC, Malani PN, Wesorick DH (2013) Hospitalists’ guide to the care of older patients. Wiley, Hoboken
Boyd C, Smith CD, Masoudi FA et al (2019) Decision making for older adults with multiple chronic conditions: executive summary for the American Geriatrics Society Guiding Principles on the Care of Older Adults With Multimorbidity. J Am Geriatr Soc 67:665–673
Rubenstein LZ, Josephson KR, Wieland GD et al (1984) Effectiveness of a geriatric evaluation unit. A randomized clinical trial. N Engl J Med 311:1664–1670. https://doi.org/10.1056/NEJM198412273112604
Barry MJ, Edgman-Levitan S (2012) Shared decision making — The pinnacle patient-centered care. N Engl J Med 366:780–781. https://doi.org/10.1056/NEJMp1109283
Acknowledgements
The study design and preliminary results of the study have been presented at the 2018 Conference of the German society of geriatrics in Cologne (oral presentation), the 16th EUGMS Congress in Berlin (2018, poster presentation) as well as the 17th EUGM Congress in Krakow (2019, oral presentation). We wish to thank Lena Sannemann for her assistance with the statistics used in this report and her critical revision.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
MPR, VB and MCP conceived and designed the clinical trial. VB provided resources. MPR. LP performed the experiments. MPR analysed the data. MPR wrote the paper. MRP, AMM and MCP were involved in the conception of the manuscript. AMM, LP, AP, TB, VB and MCP contributed to critical revisions.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Statement of human and animal rights
The study was registered at the German Clinical Trials Register (DRKS00012694) and complies with the ethical rules for human experimentation that are stated in the Declaration of Helsinki (1983). It was approved by the Ethical Committee of the University Hospital of Cologne, Germany.
Informed consent
Written informed consent was obtained from all individual participants or proxy respondent included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rarek, M.P., Meyer, A.M., Pickert, L. et al. The prognostic signature of health-related quality of life in older patients admitted to the emergency department: a 6-month follow-up study. Aging Clin Exp Res 33, 2203–2211 (2021). https://doi.org/10.1007/s40520-020-01732-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01732-8