Abstract
Background
Falls are a leading cause of injury in older women. Stepping thresholds quantify balance-reaction capabilities. It is unclear how such evaluations predict falls in comparison to, or as a complement to, other objective measures of gait, standing postural control, strength, and balance confidence.
Aims
The objective of this study was to determine if stepping thresholds are prospectively related to falls in older women.
Methods
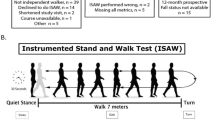
For this prospective cohort study, 125 ambulatory, community-dwelling women, age ≥ 65 years were recruited. Using a treadmill to deliver perturbations to standing participants, we determined anteroposterior single- and multiple-stepping thresholds. Here, thresholds represent the minimum perturbation magnitudes that consistently evoke one step or multiple steps. In addition, gait kinematics, obstacle-crossing kinematics, standing sway measures, unipedal stance time, the functional reach, lower extremity isometric strength, grip strength, balance confidence, and fall history were evaluated. Falls were prospectively recorded for one year.
Results
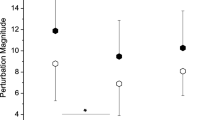
Seventy-four participants (59%) fell at least once. Posterior single-stepping thresholds were the only outcome that predicted future fall status (OR = 1.50, 95% CI 1.01–2.28; AUC = .62). A multivariate approach added postural sway with eyes closed as a second predictive variable, although predictive abilities were not meaningfully improved.
Discussion
These results align with the previous evidence that reactive balance is a prospective indicator of fall risk. Unlike previous studies, strength scaled to body size did not contribute to fall prediction.
Conclusion
Posterior single-stepping thresholds held a significant relationship with future fall status. This relationship was independent of, and superior to that of, other measures of standing balance, gait, strength, and balance confidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Women comprise nearly two-thirds of older adult fallers [1]. Falls account for about 1.9 million nonfatal injuries of older women each year, resulting in an injury rate more than 50% higher than that of men [2]. Given this disparity in the impact of falls on men and women, as well as apparent between-sex differences in how strength [3] and balance [4] are altered with age, it is reasonable to take a sex-specific approach to identify fall-risk factors.
Up to 63% of older adult falls are from an extrinsic perturbation [5,6,7,8]. Therefore, balance-reaction tests are relevant in evaluating fall risk. At-home fallers have been characterized by lower perturbation forces that elicit a posterior step [9]. In the same study, responses to anterior and lateral perturbations did not hold that relationship. Conversely, the inability to limit steps after a lateral waist pull [10, 11] or forward lean release [12] has been associated with future falls. For feet-in-place reactions to an oscillating platform, the resulting lateral sway was larger for future fallers [8]. From these studies, it was clear that some, but not all, balance-reaction tests could play a meaningful role in evaluating fall risk. Between-study variability may underlie inconsistencies in results. Differences include the method, direction, size, and precision of perturbations; instructions pertaining to step constraints; and the participant’s certainty of the fall direction. These factors likely affect the measure’s reliability, precision, and ecological validity. Furthermore, a sex-specific approach to fall prediction had not been considered, despite difference in fall injury rates, incidence, risk factors, and balance-reaction capabilities [2, 13,14,15,16].
We developed a protocol to reliably and precisely quantify anteroposterior single- and multiple-stepping thresholds [17]. Using the same data set as the present study, we determined that these thresholds could only partially be inferred from a combination of age, functional measures, and balance confidence [18]. We did not know, however, if the unique perspective on balance reactions was relevant to fall risk.
The purpose of this study was to determine if stepping thresholds are prospectively related to falls in ambulatory, community-dwelling older women. We hypothesized that such thresholds would be related to falls in the year after assessment. Additionally, we hypothesized that thresholds would persist as independent predictors of falls when combined with the other measures of standing balance, gait, strength, balance confidence, and fall history. This study represented an exploratory aim of the Mayo Clinic Study Assessing Fall Epidemiology and Risk (SAFER), the primary goal of which was to evaluate the relationships between balance/function assessments and the Fracture Risk Assessment Tool (FRAX) [19] score.
Materials and methods
Study participants
We recruited 125 community-dwelling women for this study, targeting approximately 25 women per 5-year age strata from 65 to 85 + years (65–69 years: n = 27, 70–74 years: n = 26, 75–79 years: n = 26, 80–84 years: n = 25, 85 + years: n = 21). This sample size was chosen to provide 90% power for the SAFER primary analysis, correlating fall risk with FRAX scores (results not yet published). All women reported the ability to walk a city block without a gait aid. Participants were, on average, overweight, active, and with a few chronic comorbidities (Table 1). They had no previous diagnosis of dementia and were cognitively intact. This study was approved by the Mayo Clinic Institutional Review Board, and all participants provided written informed consent.
Assessment of stepping thresholds
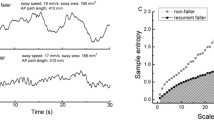
Stepping thresholds were assessed as participants stood on a computer-controlled treadmill (Simbex, Lebanon, NH, USA, Fig. 1, video in Supplementary Material). All participants wore a safety harness (Maine Anti-Gravity Systems, Inc., Portland, ME, USA) attached to an overhead rail, as well as their own pair of well-cushioned shoes. Two progressively challenging series of perturbations were administered [17]. One series was designed to quantify anterior (ASST) and posterior (PSST) single-stepping thresholds (Fig. 1a). A subsequent series evaluated anterior (AMST) and posterior (PMST) multiple-stepping thresholds (Fig. 1b). We have previously described this protocol in detail [17, 18]. Briefly, participants were instructed to “try not to step” in the single-stepping-threshold test and “try to take only one step” in the subsequent multiple-stepping-threshold test. The perturbation direction was randomized, so that, at most, three perturbations in the same direction were consecutively delivered. After participants acknowledged that they were ready, the timing of the perturbation was delayed 3–10 s. Therefore, participants were expecting a perturbation, but could not predict the timing or direction of it. Aside from the failure to respond as instructed, responses were also considered failures if the participant reported assistive support from the harness or the investigator observed unambiguous harness support. The perturbation that represented the threshold of interest elicited four consecutive failed responses. Given this criterion, it was typically the case that participants stepped against instructions early in the assessment, doing so in response to relatively small perturbations. However, participants usually learned to withhold steps within the next three attempts. To best estimate the magnitude of the destabilizing perturbation, thresholds were expressed as the resulting torque at the base of an inverted pendulum (τ =|m · a · l|), where m is body mass, a is the perturbation acceleration, and l is the estimated pendulum height (0.586 height).
a An 82-year-old participant recovers from anterior and posterior disturbances without a step. Here, anterior and posterior refer to the direction of the fall, not the translation of the treadmill belt. Shown are the responses to the largest disturbance recovered without taking a step. b Shown are the same participant’s responses to the largest disturbance recovered with a single step. A video of these tests with a different participant is available as Online Supplementary Material
Other assessments
-
1.
Balance Confidence was recorded using the Activities-specific Balance Confidence (ABC) questionnaire [23].
-
2.
Fall History in the 12 months prior to enrollment was self-reported.
-
3.
Gait Analysis: Participants walked at preferred speeds, with body-segment motion recorded over 3–6 strides (120 Hz, Motion Analysis Corporation, Santa Rosa, CA, USA). Measures included average gait speed, stride time, the percent of stride in double-support, and step width, as calculated using commercial (C-Motion Inc., Rockville, MD, USA) and custom (Mathworks, Natick, MA, USA) software.
-
4.
Obstacle Crossing: Participants walked 2.5 m before crossing a 2.4 cm obstacle. The average peak lateral speed of the whole-body center of mass (COM) during the crossing step [24], including three left and right crossing-steps, was determined from motion recordings.
-
5.
Standing Postural Sway: Participants stood on two force plates (Kistler Instrument Corp., Amherst, NY, USA; 600 Hz) for 30 s. Outcomes included the center of pressure root-mean-square error (RMSE) under eyes-closed [RMSEEC] and eyes-opened [RMSEEO] conditions, as well as the Romberg ratio of the two (RMSEEC/EO) [8].
-
6.
Unipedal Stance: Participants stood on one foot for up to 30 s. The maximum time of six attempts, three on each foot, was recorded [25].
-
7.
Functional Reach: Participants reached as far forward as they could with their dominant hand. The average reach of the last three of five successful trials was determined [26].
-
8.
Strength: Hip, knee, and ankle flexor and extensor isometric strength of the non-kicking limb was measured for three trials each (HUMAC NORM, Computer Sports Medicine, Inc., Stoughton, MA, USA). Grip strength of each hand was tested three times using a dynamometer (Aeverl Medical, Gainesville, GA, USA). The greatest force (hand grip) or torque (lower extremity) among all trials was selected.
Fall tracking
For 1 year, twice-monthly questionnaires were completed by participants [20]. Falls were defined as when the participant lost their balance and landed (1) on the floor, ground, or lower level; (2) on an object (e.g., furniture); or (3) against a wall or railing. We had 97.5% of fall mailers completed, a rate that benefited from careful tracking and follow-ups by phone [20].
Statistical analyses
To evaluate function relative to body size, all measures were scaled to unitless values (Table 2) [18, 27]. Logistic regression evaluated the univariate relationship of each measure with fall status (any vs none). Variables were selected for inclusion in a multivariable logistic regression model using penalized logistic regression analysis after imputing the data tenfold to include participants with missing data [28, 29]. A lasso penalty was chosen using cross-validation to select the penalty that resulted in the smallest misclassification error. The area under the receiver operator curve (AUC) was calculated to summarize the predictive accuracy of the logistic models. Significance was held at α = 0.05 for all tests. Analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA) and R version 3.4.2 (Vienna, Austria; www.R-project.org).
Results
Some participants did not complete all assessments (Table 2). Seven participants were partially limited by study staff as a safety precaution. Reasons for exclusion included acute knee pain, ankle tendon injury history with preferred use of an ankle brace, a history of cardiac events with current use of a pacemaker or loop recorder, or medical shunts or pouches that could be affected by the safety harness. Additional participants (n = 17) did not complete all stepping-threshold assessments. Thirteen participants completed none or only part of the tests due to self-reported nervousness on the treadmill. Four participants chose to end their participation due to back pain or knee soreness. Six participants did not complete all strength tests due to discomfort, self-reported fatigue, or, in one case, user error in saving data.
Over the year after assessment, 74 participants (59%) fell at least once. Fall details are reported in a separate report [20]. Of all measures, only PSSTs significantly discriminated future fallers from non-fallers (OR = 1.50, 95% CI 1.01–2.28, AUC = 0.62, Table 2). A standard-deviation decline in PSST was associated with a 50% increase in the odds of being a faller. In a multivariable model, PSSTs (OR = 1.45, 95% CI 0.98–2.21, p = 0.1) were paired with postural sway with the eyes closed (OR = 1.27, 95% CI 0.85–1.99, p = 0.3), although the predictive ability of this model did not increase (AUC = 0.62). So that results can be compared to other studies, non-normalized values are presented in the appendix. For non-normalized values, PSSTs and grip strength were significant discriminators of future fallers and non-fallers.
Discussion
The purpose of this study was to determine if stepping thresholds were prospectively related to falls in older women. PSSTs, or the disturbance magnitude that consistently elicited a backward step, were predictive of subsequent falls. This measure paired with vision-occluded sway in a multivariable model of fall prediction.
These results partially agreed with previous studies on balance reactions and subsequent falls in older adults. After a waist pull, PSSTs, but not ASSTs were predictive of falls [9]. Contrary to our results, AMSTs after a lean release predicted falls [12]. This discrepancy could be due to differences in study samples. The aforementioned study included both men and women, with women more likely to take multiple steps [12]. We encouraged treating sex as an independent factor, as there appeared to be interactions between sex, age, and fall circumstances [30]. In the lean-release study, 70% of falls were anterior in direction; and 13% were posterior [12]. The lean-release threshold specifically predicted forward falls. In our cohort of women, 44% of falls were anterior in direction and 41% were posterior [20]. PSSTs did not significantly predict posterior fallers (n = 42, OR = 1.27, 95% CI 0.85–1.93, p = 0.2, AUC = 0.60).
Our multivariable model aligned with previous studies. In a study that included both men and women, falls were predicted by a combination of mediolateral standing sway with vision occluded and anteroposterior sway while on an oscillation platform [8]. Therefore, there was a trend that steadiness and balance-reaction measures were independent, yet valid indicators of fall risk. This trend was supported by evidence that the tendency to take multiple anterior steps after a lean release predicted falls when partnered with tests of vision, sensation, strength, reaction time, sway, and dynamic balance [12].
Unlike previous studies [31], strength did not predict falls. A key difference in our study was that we scaled strength to body size. This was a logical approach, as many perturbations outside the laboratory were likely proportional to body size. In other words, larger people move with greater momentum, and their collisions with fixed objects will result in larger perturbing forces. In addition, the impulses necessary to arrest a fall were also proportional to body size. Using non-adjusted values, grip strength was a significant fall predictor (p = 0.04, Appendix). However, a positive correlation between grip strength and body mass (r = 0.26, p = 0.01) suggested that scaling was warranted. Of note, the combination of low grip strength and obesity, as measured by waist circumference, was a strong risk factor of falling [32]. Regardless of scaling, lower extremity strength did not predict falls. In a previous study, adding peak isokinetic hip abductor torque to the tendency to take multiple steps after a lateral fall made fall prediction more specific, albeit less sensitive [10]. Perhaps, isokinetic measures or tests of muscles acting in the frontal plane would have contributed to our fall-prediction model.
The association of posterior stepping thresholds with falls was likely weak (AUC < 0.63) due to the multifactorial nature of falling. Falls were influenced by intrinsic, extrinsic, and behavioral factors [33]. Therefore, a small battery of intrinsic assessments was not likely to sensitively and consistently identify fallers. The observation that a balance-reaction measure persisted, despite confounding influences, was a promising indicator that balance reactions should be part of a comprehensive fall-risk evaluation.
Our observed 59% fall incidence was higher than most previous reports [5,6,7,8], a result we attributed to frequent, twice-monthly questionnaires and persistent follow-up that resulted in 97.5% adherence in returning reports [20]. An alternative approach to the analysis of our study would be to use the number of falls as the dependent variable. With 158 recorded falls, and with 30% of participants falling more than once, this cohort of older women fell at a rate of 1.3 falls per person-year [20]. In this context, vision-occluded sway was the only measure to have a significant relationship with the number of falls (RR = 1.22, 95% CI 1.01–1.47, p = 0.043). Posterior stepping thresholds did not hold such a significant relationship (RR = 1.13, 95% CI 0.90–1.42, p = 0.30). This disparity in results, when considering the number of falls, may be due to the aforementioned intrinsic, extrinsic, and behavioral factors that underly fall risk [33]. Consider that, after a single fall, an individual would likely modify their behavior or extrinsic factors so as to reduce the risk of a subsequent fall. These modifications could include avoiding hazardous areas or activities, removing hazards in their environment, reducing gait speed, or being less physically active [34]. Such modifications would alter the likelihood of experiencing an external perturbation. In turn, fall-recovery skill, as measured by posterior stepping thresholds, would be a less-relevant factor underlying fall risk. Conversely, the sway test may be more sensitive to impaired sensory function, an intrinsic risk factor. In the presence of this substantial risk factor, behavioral and extrinsic-factor modifications, then, may be less effective at limiting a subsequent loss of balance. Therefore, the sway-based measure and the stepping-threshold measures may reflect two distinct influences on the risk of falling, an important consideration when determining an individualized approach to preventing a fall.
We have demonstrated a significant relationship between a measure of performance (i.e., PSSTs) and subsequent falls. From these data alone, however, we do not know the underlying mechanisms that lead to worse stepping thresholds. Standing balance reactions consist of complex, multi-joint actions to prevent a step [35, 36]. Posterior responses share common neural pathways to that of the startle response [37]. Therefore, posterior thresholds could reflect the ability to control the startle response in situations where the perturbation is anticipated, but the timing and direction are not known. Nearly all participants failed in response to perturbations smaller than their final threshold, but learned to recover successfully in the next three attempts. Our assessment, then, is not just a measure of motor performance, but is also an indicator of short-term motor learning. Further biomechanics and motor control studies are needed to elucidate the specific underlying features of the posterior stepping-threshold test that are related to fall risk.
An advantage of stepping thresholds as a fall-risk assessment is that it directly informs fall-recovery skill as an intervention target. Perturbation-based balance training has significantly reduced falls in older adults and individuals with Parkinson’s Disease (RR = 0.54, 95% CI 0.34–0.85) [38]. Perhaps, for those with impaired balance-reaction performance, this approach would prevent behavioral adaptations, such as limiting physical activity, that would have negative health consequences. Additional study is needed to determine if specifically improving PSSTs, a task in which a non-stepping response is encouraged, will subsequently decrease the risk of falls. It could be that such an approach would benefit the robustness of standing or walking when perturbed, limiting reliance on the separate skill of reactive stepping [39].
A limitation of this protocol is the risk of soreness or feasibility. Across all assessments, 4% of participants ended participation due to soreness, and 12% ended participation due to nervousness. These proportions were reduced to 1% and 4% when only accounting for the single-stepping-threshold protocol. We assume that the nervous response was associated with a fear of falling, a factor that is predictive of falls, yet can also result from experiencing a fall [40]. Therefore, the stepping-threshold test may not be applicable to a subset of older adults with substantial fear or very low fall self-efficacy, a group in which cognitive factors may play a more important influence on fall risk than motor factors [41]. Of the five participants who did not register a PSST due to nervousness, two subsequently fell. The psychological risk factors considered in our study only included balance confidence, ignoring other aspects such as depression [42], apathy [43], or chronic pain [44]. A second limitation may be insufficient power to detect significant relationships between our measures and subsequent falls. Numerous measures in this exploratory analysis had promising, non-significant (p < 0.35) relationships with fall status (Table 2). We cannot conclude that these measures have no utility in evaluating fall risk, yet our observed effect sizes may be of use in meta-analyses, or they can inform expectations for more rigorous, powered study.
Conclusions
PSSTs are prospectively related to falls in community-dwelling older women. Given its promising reliability [17], these thresholds may also serve as a relevant pre- and post-test indicator of how rehabilitation alters the risk of falling. Subsequent work is needed to determine if this assessment is indicative of fall risk in other populations, such as older men.
References
Florence CS, Bergen G, Atherly A et al (2018) Medical Costs of Fatal and Nonfatal Falls in Older Adults. J Am Geriatr Soc 66:693–698. https://doi.org/10.1111/jgs.15304
Prevention CfDCaP-NCfI (2019) Web-based Injury Statistics Query and Reporting System (WISQARS). https://www.cdc.gov/injury/wisqars/index.html. Accessed 3 Jan 2019
Lindle RS, Metter EJ, Lynch NA et al (1997) Age and gender comparisons of muscle strength in 654 women and men aged 20–93 yr. J Appl Physiol 83:1581–1587. https://doi.org/10.1152/jappl.1997.83.5.1581
Sullivan EV, Rose J, Rohlfing T et al (2009) Postural sway reduction in aging men and women: relation to brain structure, cognitive status, and stabilizing factors. Neurobiol Aging 30:793–807. https://doi.org/10.1016/j.neurobiolaging.2007.08.021
Berg WP, Alessio HM, Mills EM et al (1997) Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing 26:261–268
Campbell AJ, Borries MJ, Spears GF et al (1990) Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing 19:136–141
Davis JW, Ross PD, Nevitt MC et al (1997) Incidence rates of falls among Japanese men and women living in Hawaii. J Clin Epidem 50:589–594
Maki BE, Holliday PJ, Topper AK (1994) A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J Gerontol 49:M72–84
Sturnieks DL, Menant J, Delbaere K et al (2013) Force-controlled balance perturbations associated with falls in older people: a prospective cohort study. PLoS ONE 8:e70981. https://doi.org/10.1371/journal.pone.0070981.g001
Hilliard MJ, Martinez KM, Janssen I et al (2008) Lateral balance factors predict future falls in community-living older adults. Arch Phys Med Rehabil 89:1708–1713. https://doi.org/10.1016/j.apmr.2008.01.023
Mille ML, Johnson-Hilliard M, Martinez KM et al (2013) One step, two steps, three steps more … Directional vulnerability to falls in community-dwelling older people. J Gerontol A Biol Sci Med Sci 68:1540–1548. https://doi.org/10.1093/gerona/glt062
Carty CP, Cronin NJ, Nicholson D et al (2015) Reactive stepping behaviour in response to forward loss of balance predicts future falls in community-dwelling older adults. Age Ageing 44:109–115. https://doi.org/10.1093/ageing/afu054
Carty CP, Barrett RS, Cronin NJ et al (2012) Lower limb muscle weakness predicts use of a multiple- versus single-step strategy to recover from forward loss of balance in older adults. J Gerontol A Biol Sci Med Sci 67:1246–1252. https://doi.org/10.1093/gerona/gls149
Ek S, Rizzuto D, Fratiglioni L et al (2019) Risk factors for injurious falls in older adults: the role of sex and length of follow-up. J Am Geriatr Soc 67:246–253
Gale CR, Cooper C, Aihie Sayer A (2016) Prevalence and risk factors for falls in older men and women: the English Longitudinal Study of Ageing. Age Ageing 45:789–794. https://doi.org/10.1093/ageing/afw129
Sturnieks DL, Menant J, Vanrenterghem J et al (2012) Sensorimotor and neuropsychological correlates of force perturbations that induce stepping in older adults. Gait Posture 36:356–360. https://doi.org/10.1016/j.gaitpost.2012.03.007
Crenshaw JR, Kaufman KR (2014) The intra-rater reliability and agreement of compensatory stepping thresholds of healthy subjects. Gait Posture 39:810–815. https://doi.org/10.1016/j.gaitpost.2013.11.006
Crenshaw JR, Bernhardt KA, Atkinson EJ et al (2018) The relationships between compensatory stepping thresholds and measures of gait, standing postural control, strength, and balance confidence in older women. Gait Posture. https://doi.org/10.1016/j.gaitpost.2018.06.117
Kanis JA, Johnell O, Oden A et al (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397. https://doi.org/10.1007/s00198-007-0543-5
Crenshaw JR, Bernhardt KA, Achenbach SJ et al (2017) The circumstances, orientations, and impact locations of falls in community-dwelling older women. Arch Gerontol Geriatr 73:240–247. https://doi.org/10.1016/j.archger.2017.07.011
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Ainsworth BE, Haskell WL, Leon AS et al (1993) Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc 25:71–80. https://doi.org/10.1249/00005768-199301000-00011
Powell LE, Myers AM (1995) The Activities-Specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci 50A:M28–34
Chou L, Kaufman KR, Hahn ME et al (2003) Medio-lateral motion of the center of mass during obstacle crossing distinguishes elderly individuals with imbalance. Gait Posture 18:125–133
Hurvitz EA, Richardson JK, Werner RA et al (2000) Unipedal stance testing as an indicator of fall risk among older outpatients. Arch Phys Med Rehabil 81:587–591
Duncan PW, Studenski S, Chandler J et al (1992) Functional reach: predictive validity in a sample of elderly male veterans. J Gerontol 47:M93–98
Hof AL (1996) Scaling gait data to body size. Gait Posture 4:222–223
Friedman J, Hastie T, Tibshirani R (2010) Regularization paths for generalized linear models via coordinate descent. J Statist Soft 33:1–22
van Buuren S, Groothuis-Oudshoorn K (2011) MICE: Multivariate imputation by chained equation in R. J Stat Soft. https://doi.org/10.18637/jss.v045.i03
O'Loughlin JL, Robitaille Y, Boivin J-F et al (1993) Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 137:342–354
Moreland JD, Richardson JA, Goldsmith CH et al (2004) Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc 52:1121–1129. https://doi.org/10.1111/j.1532-5415.2004.52310.x
Gadelha AB, Neri SGR, Vainshelboim B et al (2019) Dynapenic abdominal obesity and the incidence of falls in older women: a prospective study. Aging Clin Exper Res. https://doi.org/10.1007/s40520-019-01318-z
Todd C, Skelton D (2004) What are the main risk factors for falls among older people and what are the most effective interventions to prevent these falls? World Health Organization Regional Office for Europe
Wijlhuizen GJ, de Jong R, Hopman-Rock M (2007) Older persons afraid of falling reduce physical activity to prevent outdoor falls. Prev Med 44:260–264. https://doi.org/10.1016/j.ypmed.2006.11.003
van Roden EAR, Petersen DA, Pigman J et al (2018) The contribution of counter-rotation movements during fall recovery: a validation study. J Biomech 78:102–108. https://doi.org/10.1016/j.jbiomech.2018.07.025
Runge CF, Shupert CL, Horak FB et al (1999) Ankle and hip postural strategies defined by joint torques. Gait Posture 10:161–170. https://doi.org/10.1016/S0966-6362(99)00032-6
Nonnekes J, Scotti A, Oude Nijhuis LB et al (2013) Are postural responses to backward and forward perturbations processed by different neural circuits? Neuroscience 245:109–120. https://doi.org/10.1016/j.neuroscience.2013.04.036
Mansfield A, Wong JS, Bryce J et al (2015) Does perturbation-based balance training prevent falls? Systematic review and meta-analysis of preliminary randomized controlled trials. Phys Ther 95:700–709
Van Hooren B, Meijer K, McCrum C (2018) Attractive gait training: Applying dynamical systems theory to the improvement of locomotor performance across the lifespan. Front Physiol 9:1934. https://doi.org/10.3389/fphys.2018.01934
Friedman SM, Munoz B, West SK et al (2002) Falls and fear of falling: Which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc 50:1329–1335. https://doi.org/10.1046/j.1532-5415.2002.50352.x
Langeard A, Desjardins-Crepeau L, Lemay M et al (2019) Cognitive performances better identify fallers than mobility assessment among older adults with fear of falling. Aging Clin Exp Res. https://doi.org/10.1007/s40520-019-01338-9
Lauretani F, Ticinesi A, Gionti L et al (2019) Short-physical performance battery (SPPB) score is associated with falls in older outpatients. Aging Clin Exper Res 31:1435–1442. https://doi.org/10.1007/s40520-018-1082-y
Henstra MJ, Rhebergen D, Stek ML et al (2019) The association between apathy, decline in physical performance, and falls in older persons. Aging Clin Exper Res 31:1491–1499. https://doi.org/10.1007/s40520-018-1096-5
Asai T, Misu S, Sawa R et al (2015) Multi-chronic musculoskeletal pain is a useful clinical index to predict the risk of falls in older adults with normal motor function. Aging Clin Exper Res 27:711–716. https://doi.org/10.1007/240520-015-0340-5
Acknowledgements
We thank Louise McCready, R.N. for study coordination and Diana Hansen for data collection and processing.
Funding
This work was supported by National Institutes of Health [grant numbers R01AR027065 to SK/SA, T32HD07447 to J. R. Basford, NIH UL1TR000135 to SK]. The NIH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
Jeremy R. Crenshaw, Ph.D.: conceptualization, methodology, formal analysis, investigation, writing—original draft, and visualization. Kathie A. Bernhardt, B.S.: methodology, software, investigation, data curation, writing—review & editing, and project administration. Elizabeth J. Atkinson, M.S.: software, formal analysis, data curation, and writing—review & editing. Sara J. Achenbach, M.S.: software, formal analysis, data curation, and writing—review & editing. Sundeep Khosla, M.D.: conceptualization, resources, writing—review & editing, and funding acquisition. Shreyasee Amin, M.D. M.P.H.: conceptualization, methodology, resources, writing—review & editing, supervision, project administration, and funding acquisition. Kenton R. Kaufman, Ph.D. P.E.: conceptualization, methodology, resources, writing—review & editing, supervision, project administration, and funding acquisition.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
None, this paper is the authors’ own original work, which has not been previously published elsewhere.
Statement of human and animal rights
This study was approved by the Mayo Clinic Institutional Review Board.
Informed consent
All participants provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
An 89-year-old participant undergoes assessments of single- and multiple-stepping thresholds. Electronic supplementary material 1 (MP4 23740 kb)
Appendix 1
Appendix 1
See Table 3.
Rights and permissions
About this article
Cite this article
Crenshaw, J.R., Bernhardt, K.A., Atkinson, E.J. et al. Posterior single-stepping thresholds are prospectively related to falls in older women. Aging Clin Exp Res 32, 2507–2515 (2020). https://doi.org/10.1007/s40520-020-01480-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01480-9