Abstract
Background
Osteoporotic fractures are associated with increased morbidity, mortality, and increased health care use. As the number of older adults increases, identifying those at increased risk for osteoporotic fractures has become of utmost importance to providing them with preventive and therapeutic interventions.
Aims
To determine the prevalence of unknown clinical and densitometric osteoporosis and to investigate the performance of different diagnostic strategies for osteoporosis in elderly patients admitted to rehabilitation.
Method
This is an observational study. Eligible participants were older adults admitted to rehabilitation in an academic hospital in Switzerland over an 11-month period. Patients with previously unknown osteoporosis underwent dual-energy X-ray absorptiometry (DXA), vertebral fracture assessment (VFA), and history review for past fractures.
Results
Complete assessment was available for 252 patients. Previously undiagnosed osteoporosis was identified in 62.3% of these patients, a proportion that was higher among women (71.5%) than men (44.8%). DXA proved most sensitive, followed by VFA and history review. Results differed across gender: DXA remained the most sensitive single test among women, but VFA proved most sensitive in men. The best test to combine with history review was DXA in women (detection increasing from 47.5 to 93.2%) and VFA in men (detection increasing from 35.9 to 84.6%).
Conclusions
Prevalence of previously unknown osteoporosis appears very high in elderly patients admitted to post-acute rehabilitation. The combination of history review of previous fractures with DXA in women and with VFA in men appears the best two-step strategy to improving detection of osteoporosis in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Osteoporosis is a progressive systemic disease of the skeleton characterized by altered bone density and microarchitecture that results in bone fragility and fractures [1]. Worldwide, osteoporosis causes about 9 million fractures annually, corresponding to one osteoporotic fracture occurring every 3 s [2]. About one in two Caucasian women and one in five Caucasian men will undergo an osteoporotic fracture over their lifetime [3,4,5,6,7]. In the United States, the lifetime risk of hip, spine, or forearm fracture at age 50 is estimated at 40% in women and 13% in men [8], with a sharp increase thereafter [9,10,11]. Worldwide, osteoporosis affects approximately one out of five women aged 70 years, two out of five women aged 80, and two out of three women aged 90 [12].
Osteoporotic fractures, particularly hip fractures, are associated with increased morbidity [13], disability [2, 14], and mortality [14], as well as increased health care use [15]. As the number of older adults increases in most countries, identifying those at increased risk for osteoporotic fractures has become of utmost importance to providing them with preventive and therapeutic interventions. Despite its high prevalence and important consequences, osteoporosis remains yet underdetected and undertreated [16, 17], particularly in older men and in long-term care residents [18, 19]. Moreover, frail old adults are often underrepresented in studies about diagnostic and the management strategies adapted to this specific population are, therefore, less well defined [20].
Osteoporosis can be diagnosed using different criteria. Clinical osteoporosis is diagnosed after spontaneous or low energy fractures at hip, thoraco-lumbar vertebras, proximal humerus, and distal radius. Osteoporosis is also diagnosed based on results from measures of bone mineral density by dual-energy X-ray absorptiometry scan (DXA). According to criteria established by the World Health Organization [21], osteoporosis corresponds to a bone mineral density (BMD) with a T score < − 2.5 standard deviation (SD) compared to average values for young healthy women. DXA also permits to classify BMD as normal (T score > − 1.0 SD) or osteopenic (T score between − 1.0 and − 2.5 SD). However, DXA is not always available or has restricted accessibility due to reimbursement limitations [22]. Screening for osteoporosis with DXA is further limited in the oldest population by difficulties in positioning those disabled. Finally, when realized, DXA results can be difficult to interpret because of BMD under- and over-estimation resulting from concomitant osteomalacia or osteoarthritis [23], respectively. On the other hand, DXA can provide views of dorsal and lumbar vertebral bodies, thus allowing to perform vertebral fracture assessment (VFA) to identify fractures [24]. VFA produces less radiation than a plain X-ray of the spine and was shown to have similar accuracy in identifying grade 2 and 3 vertebral fractures [25].
Screening strategies for osteoporosis have been proposed in the long-term care population [22], but, to the best of our knowledge, no similar specific strategy is available in older patients admitted to post-acute rehabilitation. Indeed, the prevalence as well as the rate of undiagnosed osteoporosis in patients admitted to rehabilitation remains unknown.
Thus, the objectives of this study were (a) to determine the prevalence of unknown clinical and densitometric osteoporosis in elderly patients admitted to post-acute rehabilitation; and (b) to investigate the performance of different strategies to diagnose osteoporosis in this specific population. Specifically, we wanted to determine which combination of history review (Hx), DXA, and/or VFA would best perform in these patients.
Methods
Population and setting
This observational study was conducted in the geriatric post-acute rehabilitation unit of an academic hospital in Lausanne, Switzerland. Patients are admitted mainly from general internal medicine, orthopedic surgery, traumatology, and general surgery wards.
Over an 11-month period, all patients aged 65 years or older consecutively admitted were screened for eligibility to participate to the study. Patients were excluded if already diagnosed with osteoporosis (i.e., prior documented DXA, receiving specific osteoporosis treatments such as bisphosphonates, denosumab, teriparatide, selective estrogen receptor modulator, and hormone replacement therapy). In addition, those unable to climb 4 stairs to access the DXA machine or unable to lie down during the examination, those colonized with multiresistant microorganism (i.e., Methicillin-resistant Staphylococcus aureus, Vancomycin-resistant Enterococci, Extended-Spectrum β-Lactamase) were also excluded. Finally, patients judged by their physician as unable to consent to the protocol and those with expected survival shorter than 6 months were also excluded.
Densitometric and VFA analysis
Participants underwent DXA scan and vertebral fracture assessment using a Hologic® Discovery C model (SN80021) installed in a mobile van. The exam was performed and interpreted by a specialist in bone diseases (KMA). Stability and reliability of the DXA scan were regularly assessed. Bone mineral density (BMD) was assessed at lumbar (L1–L4) and hip (total hip and femoral neck) sites. If one of these sites could not be assessed (due to marked osteoarthritis, prosthetic material, or artifacts), the non-dominant radius was examined. Vertebral fractures were graded using Genant’s classification [26], and only those of grade 2 or 3 were considered as VFA has a low sensitivity for detection of grade 1 vertebral fractures [25].
Data collection
A research assistant collected data at admission during a structured assessment within 1 week after admission. Socio-demographic (age, gender, and living situation) and medical (number of falls over the last 6 months, past fractures, sites, and type of fractures, i.e., fragility fractures resulting from low energy trauma) data were collected.
In addition, performance in basic [27] and instrumental [28] activities of daily living (ADL) prior to hospital admission were recorded. Balance and gait were assessed using Tinetti’s Performance Oriented Mobility Assessment (POMA) [29] by a trained physiotherapist, and cognitive and affective statuses were assessed using the Mini-Mental Status Exam (MMSE) [30] and the 15-item Geriatric Depression scale (GDS) [31], respectively.
Definition of osteoporosis
Osteoporosis was defined as any one of: (1) bone mineral density (BMD) ≤ − 2.5 SD at any site at DXA; (2) one or more vertebral fractures (grade 2 or 3 by Genant’s classification) at VFA; (3) history of fragility fracture (i.e., low energy or non-traumatic) at hip, distal radius, proximal humerus, or pelvis sites, or periprosthetic non-traumatic fracture of the hip.
Statistical analysis
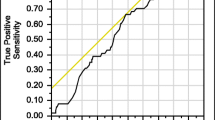
Usual statistics were used to describe the population’s characteristics. Osteoporosis prevalence was determined according to criteria (i.e., history, DXA, and VFA) previously described. Sensitivities for different diagnostic strategies were calculated using the combination of osteoporosis diagnosis by history review, VFA, and DXA as criterion standard.
Results
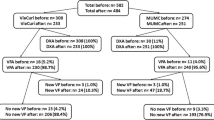
Overall, 599 patients were screened for eligibility (Fig. 1). Among those, 66 (11%) declined participation to the study, and 215 (36%) had one or more exclusion criteria, including 85 (14%) with already diagnosed osteoporosis. Among these patients (N = 85) with previously diagnosed osteoporosis, about two-thirds (N = 54/85, 63.6%) were transferred to rehab after being hospitalized in acute care secondary to a fall, about a third (N = 18/54, 33.3%) of whom suffered a fracture. The remaining patients were transferred after treatment in acute care of other musculoskeletal problems (lumbar canal stenosis, total hip, and knee replacement, etc.) (N = 16/85, 18.8%), and miscellaneous acute problems (N = 15/85, 17.6%) such as respiratory tract infections, congestive heart failure, etc.
From the remaining 318 (53%) patients initially enrolled into the study, 66 were discharged to their home before DXA evaluation could be performed. Thus, a final sample of 252 participants was analyzed (Table 1). Participants had a mean age of 83.0 ± 6.5 years, were predominantly women (65.5%), mostly independent in both basic and instrumental ADLs prior to admission to hospital, but with a large majority (70.1%) reporting at least one fall over the last 6-month period.
Prevalence of unknown osteoporosis
History review for fragility fracture was positive in 70 (27.8%) patients (Table 2). The most frequent fracture site was the distal radius, followed by hip fractures and vertebral fractures.
Radius DXA was not performed systematically but only in selected patients (N = 82) in whom lumbar and hip measures could not be performed or interpreted. Among these patients, 32 (39.0%) had abnormal BMD (T score ≤ − 2.5). Although a majority (22/32 = 69%) of these patients also reported an osteoporotic fracture, only a quarter (8/32 = 25%) had a specific history of radius fracture that was the only reported fracture in three.
VFA revealed a total of 140 grade 2 or 3 (Genant’s classification) vertebral fractures in 77 patients, with a mean of 1.8 fractures per patient and a maximum of 5 fractures in a single patient. Table 3 shows the gender-specific distribution of these vertebral fractures, with a slightly higher prevalence among women than men (1.85 vs 1.73, respectively). The most frequent sites were the 12th thoracic (T12, n = 27, 19.3% of all vertebral fractures), the 1st lumbar (L1, n = 23, 16.4%), and the 8th thoracic (T8, n = 18, 12.9%).
Finally, DXA identified densitometric osteoporosis in 109 (43.3%) patients (Table 2), more than twice more frequently in women (53.9%) than men (23.0%).
Combining all three criteria, previously undiagnosed osteoporosis was identified in 157 of the 252 (62.3%) patients, a proportion that was higher in women (71.5%) than men (44.8%).
When assessing diagnostic performance of each single test among patients (N = 157) with newly diagnosed osteoporosis (Fig. 2a), history review was positive in 44.6% and performed slightly better in women (47.5% vs 35.9% in men). DXA proved most sensitive (69.4% of all unknown osteoporosis detected), followed by VFA (49.0%). However, results differed across gender (Fig. 2): whereas DXA remained the most sensitive single test in women, identifying three quarters (75.4%) of osteoporosis cases, VFA proved most sensitive in men where it identified 59.0% of the cases (vs 51.3% detection rate for DXA). Several hypotheses can be proposed to explain the better performance of VFA in men and the better performance of DXA in women. First, this observation could be related to the fact that for the same T score, the absolute value of the BMD is higher in men than in women. Indeed, a study of a Canadian cohort reported that, for a similar T score, the fracture risk was lower in men than in women [32]. Several prospective studies have also shown that men and women with identical hip absolute BMD value have the same fracture risk.
Second, vertebral fractures are associated with an increased risk for any other osteoporotic fracture. For instance, an unknown vertebral fracture is often found in patients with a hip fracture when systematically assessed as performed in our study. Furthermore, several previous studies reported a higher risk of other osteoporotic fractures in men than in women with a vertebral fracture [33, 34], even though other studies reported the inverse. These discordant findings likely relate to differences in the population studied and future studies should further investigate this interesting observation.
When looking at the best test to combine with history review, adding DXA in women (detection increasing from 47.5 to 93.2%) and VFA in men (detection increasing from 35.9 to 84.6%) proved most effective (Fig. 2b). In comparison, combining DXA and VFA achieved detection rates of 87.3% in women and 87.2% in men.
Discussion
Results from this study show that previously unknown, and therefore untreated, osteoporosis is frequent among older patients admitted to post-acute rehabilitation, amounting up to almost one in two men and three in four women. These results further highlight the potential for secondary fracture prevention to be delivered in the rehabilitation setting as recently proposed in the Global Call to Action on Fragility Fractures [35]. In particular, these results emphasize the need for better-adapted screening and diagnostic strategies in frail old–old patients. In this regard, a unique contribution of this study is to provide detailed information about the performance of each single test, as well as of their combination, in diagnosing osteoporosis in this specific population. Based on the most comprehensive diagnostic criteria that combined results from history review for fragility fractures, DXA and VFA, DXA was the best performing single test in the total population. However, DXA performance differed across gender, with about three quarters of osteoporosis cases diagnosed in women, but only about half of the cases in men. Indeed, VFA performed best as a single test in men according to our results. Thus, DXA alone appears less than ideal as a diagnostic strategy in these older patients admitted to rehabilitation where it missed almost one-third of overall cases.
Another important and pragmatic contribution of this study is to further highlight the importance of history review as a first step in osteoporosis diagnosis. Although history review did not achieve acceptable detection threshold as a single test, combining it with either DXA in women or VFA in men resulted in excellent figures (93.2% and 84.6% detection rate, respectively) that largely exceeded those of each of these tests when used alone. Thus, despite the relatively high proportion of participants with cognitive impairment, history review for fragility fracture should definitely be part of standard care in similar population admitted to post-acute rehabilitation.
The good-to-excellent potential contribution of VFA to osteoporosis diagnosis when combined with history review is another interesting finding. VFA contribution was especially evident in men, where it increased detection by 48.7% (from 35.9 to 84.6%) when combined with history review. But even in women, combining VFA to history review increased detection of osteoporosis cases from 47.5% up to 75.4%, a 27.9% increase. In the present study, vertebral fractures were mostly prevalent in lower thoracic and upper lumbar vertebras, suggesting that fractures should be mainly searched at these sites. Using lateral thoracic X-ray as criterion standard, VFA has excellent sensitivity and specificity (92% and 99.9%, respectively) for the diagnosis of vertebral fractures [25], if excluding grade 1 deformities. In addition, VFA delivers significantly lower radiation doses (reported to be from 0.002 to about 0.05 mSv) compared to lateral thoracic and lumbar spine radiographs (0.6 mSv) [36]. When available VFA should, therefore, be part of osteoporosis screening in similar population.
Despite its limitation in frail older persons, DXA remained the best single test in women and thus in the overall population. Added to history review, it increased detection rate up to 69.8% (33.3% increase) in men and up to 93.2% (45.7% increase) in women. As the prevalence of degenerative disorders increases with age, lumbar spine BMD may be falsely high or reassuring in older people. Increase in lumbar spine BMD ranging from 7 to 16.6% has been in the presence of degenerative disorder [37,38,39,40]. For instance, in the OsteoLaus study, from 9.6 to 34.5% of the vertebrae were excluded from interpretation as proposed by ISCD guidelines, because their BMD was more than one SD different compared to the vertebrae immediately adjacent [23, 41].
Finally, our study also illustrates the potential usefulness of mobile DXA machines installed in a van. Mobile DXA allowed screening patients in a convenient mode in a hospital where DXA is not easily available.
Several limitations of this study needs to be mentioned. First, only about half of all screened patients were enrolled, mostly because of an already known osteoporosis or limited life expectancy. Although some excluded patients might be more likely to suffer from osteoporosis (i.e., patients with limited life expectancy), others (i.e., N = 66 lacking DXA due to early discharge) might inversely have had a lower risk. Thus, overall effect on prevalence was likely small if any. Second, VFA was missing in some patients and could have altered results about this test. Finally, VFA was performed by an experienced physician and results from VFA performed by less experienced professionals might result in lower performance.
This study also has several strengths such as the inclusion of a substantial proportion of men, the inclusion of the simple and pragmatic approach in the diagnostic strategy with history review as a first step.
Conclusions
Prevalence of previously unknown osteoporosis appears very high in these elderly patients admitted to post-acute rehabilitation. The combination of history review of previous fractures with DXA in women and with VFA in men appears the best two-step strategy to improving detection of osteoporosis in this population. Further studies are necessary to validate this approach and to investigate the contribution of integrating additional tools such as the FRAX or the trabecular bone score (TBS) into osteoporosis screening among old–old patients.
References
(1993) Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med 94:646–50
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733. https://doi.org/10.1007/s00198-006-0172-4
Lippuner K, Johansson H, Kanis JA et al. (2009) Remaining lifetime and absolute 10-year probabilities of osteoporotic fracture in Swiss men and women. Osteoporos Int 20:1131–1140. https://doi.org/10.1007/s00198-008-0779-8
Kanis JA, Johnell O, Oden A et al. (2000) Long-term risk of osteoporotic fracture in Malmo. Osteoporos Int 11:669–674
Nguyen ND, Ahlborg HG, Center JR et al. (2007) Residual lifetime risk of fractures in women and men. J Bone Miner Res 22:781–788. https://doi.org/10.1359/jbmr.070315
Melton LJ 3rd, Atkinson EJ, O’Connor MK et al. (1998) Bone density and fracture risk in men. J Bone Miner Res 13:1915–1923. https://doi.org/10.1359/jbmr.1998.13.12.1915
Melton LJ, Chrischilles EA, Cooper C, et al. (1992) Perspective. How many women have osteoporosis. J Bone Miner Res 7:1005–1010. https://doi.org/10.1002/jbmr.5650070902
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16:S3–S7. https://doi.org/10.1007/s00198-004-1702-6
Felsenberg D, Silman AJ, Lunt M et al. (2002) Incidence of vertebral fracture in europe: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res 17:716–724. https://doi.org/10.1359/jbmr.2002.17.4.716
Svedbom A, Ivergard M, Hernlund E et al. (2014) Epidemiology and economic burden of osteoporosis in Switzerland. Arch Osteoporos 9:187. https://doi.org/10.1007/s11657-014-0187-y
Hernlund E, Svedbom A, Ivergard M et al. (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136. https://doi.org/10.1007/s11657-013-0136-1
Kanis J (2007) WHO technical report. University of Sheffield, UK
Oleksik A, Lips P, Dawson A et al. (2000) Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res 15:1384–1392. https://doi.org/10.1359/jbmr.2000.15.7.1384
Trombetti A, Herrmann F, Hoffmeyer P et al. (2002) Survival and potential years of life lost after hip fracture in men and age-matched women. Osteoporos Int 13:731–737. https://doi.org/10.1007/s001980200100
Lippuner K, Grifone S, Schwenkglenks M et al. (2012) Comparative trends in hospitalizations for osteoporotic fractures and other frequent diseases between 2000 and 2008. Osteoporos Int 23:829–839. https://doi.org/10.1007/s00198-011-1660-8
Gillespie CW, Morin PE (2017) Osteoporosis-related health services utilization following first hip fracture among a cohort of privately-insured women in the United States, 2008–2014: an observational study. J Bone Miner Res 32:1052–1061. https://doi.org/10.1002/jbmr.3079
Yusuf AA, Matlon TJ, Grauer A et al. (2016) Utilization of osteoporosis medication after a fragility fracture among elderly Medicare beneficiaries. Arch Osteoporos 11:31. https://doi.org/10.1007/s11657-016-0285-0
Zarowitz BJ, Cheng LI, Allen C et al. (2015) Osteoporosis prevalence and characteristics of treated and untreated nursing home residents with osteoporosis. J Am Med Directors Assoc 16:341–348. https://doi.org/10.1016/j.jamda.2015.01.073
Morris CA, Cabral D, Cheng H et al.(2004) Patterns of bone mineral density testing: current guidelines, testing rates, and interventions. J Gen Intern Med 19:783–790. https://doi.org/10.1111/j.1525-1497.2004.30240.x
Greenspan S, Nace D, Perera S et al. (2012) Lessons learned from an osteoporosis clinical trial in frail long-term care residents. Clin Trials (London, England) 9:247–256. https://doi.org/10.1177/1740774511430516
WHO (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. WHO, Geneva
Greenspan SL, Perera S, Nace D et al.(2012) FRAX or fiction: determining optimal screening strategies for treatment of osteoporosis in residents in long-term care facilities. J Am Geriatr Soc 60:684–690. https://doi.org/10.1111/j.1532-5415.2011.03884.x
Padlina I, Gonzalez-Rodriguez E, Hans D et al. (2017) The lumbar spine age-related degenerative disease influences the BMD not the TBS: the Osteolaus cohort. Osteoporos Int 28:909–915. https://doi.org/10.1007/s00198-016-3829-7
Binkley N, Krueger D, Gangnon R et al. (2005) Lateral vertebral assessment: a valuable technique to detect clinically significant vertebral fractures. Osteoporos Int 16:1513–1518. https://doi.org/10.1007/s00198-005-1891-7
Domiciano DS, Figueiredo CP, Lopes JB et al. (2013) Vertebral fracture assessment by dual X-ray absorptiometry: a valid tool to detect vertebral fractures in community-dwelling older adults in a population-based survey. Arthritis Care Res 65:809–815. https://doi.org/10.1002/acr.21905
Genant HK, Wu CY, van Kuijk C et al.(1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148. https://doi.org/10.1002/jbmr.5650080915
Katz S (1983) Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc 31:721–727
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontol 9:179–186
Tinetti ME, Williams TF, Mayewski R (1986) Fall risk index for elderly patients based on number of chronic disabilities. Am J Med 80:429–434
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Sheikh JI, Yesavage JA (1986) Geriatric depression scale (GDS): recent evidence and development of a shorter version. Clin Gerontol J Aging Ment Health 5:165–173
Leslie WD, Langsetmo L, Zhou W et al. (2014) Choice of lumbar spine bone density reference database for fracture prediction in men and women: a population-based analysis. J Clin Densitom 17:295–300. https://doi.org/10.1016/j.jocd.2013.09.003
Melton LJ III, Atkinson EJ, Cooper C et al. (1999) Vertebral fractures predict subsequent fractures. Osteoporos Int 10:214–221
Hasserius R, Johnell O, Nilsson BE et al. (2003) Hip fracture patients have more vertebral deformities than subjects in population-based studies. Bone 32:180–184
Dreinhofer KE, Mitchell PJ, Begue T et al. (2018) A global call to action to improve the care of people with fragility fractures. Injury 49:1393–1397. https://doi.org/10.1016/j.injury.2018.06.032
Vokes T, Bachman D, Baim S et al. (2006) Vertebral fracture assessment: the 2005 ISCD Official Positions. J Clin Densitom 9:37–46. https://doi.org/10.1016/j.jocd.2006.05.006
Liu G, Peacock M, Eilam O et al. (1997) Effect of osteoarthritis in the lumbar spine and hip on bone mineral density and diagnosis of osteoporosis in elderly men and women. Osteoporos Int 7:564–569
Vogt MT, Rubin DA, San Valentin R et al. (1999) Degenerative lumbar listhesis and bone mineral density in elderly women. The study of osteoporotic fractures. Spine 24:2536–2541
Haugen IK, Slatkowsky-Christensen B, Orstavik R et al. (2007) Bone mineral density in patients with hand osteoarthritis compared to population controls and patients with rheumatoid arthritis. Ann Rheum Dis 66:1594–1598. https://doi.org/10.1136/ard.2006.068940
Ichchou L, Allali F, Rostom S et al. (2010) Relationship between spine osteoarthritis, bone mineral density and bone turn over markers in post menopausal women. BMC Women’s Health 10:25. https://doi.org/10.1186/1472-6874-10-25
Hans D, Downs RW Jr, Duboeuf F et al. (2006) Skeletal sites for osteoporosis diagnosis: the 2005 ISCD Official Positions. J Clin Densitom 9:15–21. https://doi.org/10.1016/j.jocd.2006.05.003
Funding
This study was funded by internal research fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest for this study.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and cantonal research committee (Human Research Ethical Committee of Vaud Canton, Switzerland (Protocol Number 04/10) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Major, K., Monod, S., Bula, C.J. et al. Unknown osteoporosis in older patients admitted to post-acute rehabilitation. Aging Clin Exp Res 32, 1145–1152 (2020). https://doi.org/10.1007/s40520-019-01302-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01302-7