Abstract
Background
Trips account for over half of outdoor falls among community-dwelling older adults.
Aims
To investigate to what extent obstacle-induced trip-perturbation training could reduce fall-risk among older adults and to see whether training effects could be retained short term.
Methods
Forty community-dwelling older adults were exposed to 24 repeated trip-perturbations given in a “blocked-and-mixed” manner during over-ground gait. Another trip was given 30 min post-training. For each trip, recovery strategies and outcomes (fall versus no fall) were analyzed. Within-trial changes to proactive and reactive dynamic center of mass stability, pre-trip toe clearance and trunk angle, trunk angle at recovery completion, and recovery step length were analyzed.
Results
48% of participants fell on their novel trip. The fall rate decreased significantly for subsequent trips, with no falls on the last trip. The decreased fall incidence resulted from improved feedforward and feedback adjustments for controlling center of mass stability and body kinematics. Proactive adaptations included reduced forward center of mass velocity, which lessened forward instability, and larger toe clearance, which increased the likelihood of obstacle avoidance. Reactive adjustments included reduced forward instability and improved trunk control (reduced forward rotation) at recovery step completion. Post-training, training effects were retained in terms of fall incidence, with slight decay in toe clearance and reactive stability.
Conclusions
Older adults demonstrated appropriate locomotor-based proactive and reactive adaptations to repeated obstacle-induced trips with short-term retention similar to young adults, and thus could reduce their fall-risk through such training.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Falls are the leading cause of hospitalization and mortality in older adults aged over 65 years [1]. Specifically, trip was one of the most frequent self-reported causes of outdoor falls (~ 33%) among community-dwelling older adults [2]. In addition, trip accounted for 21% of falls captured by video in a cohort of elderly people residing in long-term care [3]. Trip-induced falls are highly dangerous [4, 5] and the subsequent fear of falling leads to reduced activity and quality of life [6]. Hence, it is essential to develop preventive interventions for reducing trip-related falls among older adults.
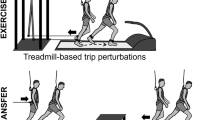
Researchers have successfully reproduced real-life-like, trip-induced large postural disturbances either by changing belt acceleration during treadmill-walking [7,8,9] or obstructing individuals’ swing limb during over-ground walking [10]. In general, an adequate reactive motor response is needed to avoid a fall by reducing excessive forward angular momentum from obstacle impact. It is well established that forward instability after an unexpected trip is caused by a forward shift in center of mass (COM) velocity and displacement with respect to the existing base of support (BOS, the feet which are usually left behind) [11]. Therefore, compensatory stepping reactions establish a new, functional BOS [12], enabling individuals to regain stability. Previously, faster reaction time of the obstructed limb (the time between obstacle-hit and touchdown) [13], effective reduction of excessive forward trunk angle and angular velocity [8, 9], sufficient net extensor torque generation from the support limb (limb contralateral to the tripping limb) during push-off [14], and proper recovery foot placement [15] have all been reported as significant contributors for successful post-trip recovery outcome.
Although reactive responses play a decisive role in reducing post-trip fall-risk, other factors could also identify the likelihood of a trip or predict the outcome of one even before obstacle-hit. A sufficient toe clearance was generally reported to be necessary for avoiding an obstacle, but this can be negatively affected by muscle fatigue [16] or premature approaching trajectory of the swing foot towards an obstacle [17]. Additionally, a faster walking speed before obstacle-hit increases the likelihood of a fall [13], while a more stable initial COM state (COM position and velocity) in relation to the BOS at recovery step completion would lessen forward instability following a trip [11]. However, researchers reported such proactive factors which can be easily modified before exposure to perturbation can reduce, but not completely eliminate fall-risk [11, 18]. Therefore, a strategy which enhances proactive factors to reduce the risk of being tripped and improves reactive responses to increase recovery rates after obstacle-hit would be most ideal to reduce trip-induced falls.
While numerous fall-prevention interventions have shown efficacious results [19], healthy, community-dwelling older adults continue to have an increased occurrence of falls from environmental perturbations [20]. These studies found conventional exercise-based training, such as resistance training [21], might not target key factors for improving recovery from a specific type of fall (i.e., trip) [9]. For example, a study showed older adults who fell did not necessarily have less muscle strength than those who recovered from laboratory-induced trips [22]. Past literature also demonstrated that muscle activity patterns (timing and sequence) selected to recover after a trip are strategy-dependent (i.e., activation of the swing limb biceps femoris facilitates the swing limb to cross over an obstacle, but this would be dangerous in a lowering strategy) [23, 24]. Therefore, the task-specific approach of practicing the actual motor skill of avoiding a fall following balance loss might possess greater specificity to prevent falls during daily living. Owing et al. [25] reported that older adults could rapidly adapt and execute a longer recovery step after experiencing the first treadmill trip trial, while also reducing their forward trunk flexion angle at recovery foot touchdown, which reduced falls on subsequent trials. It is postulated that with each repeated trip exposure the central nervous system (CNS) recalibrates its internal representation of fall-risk thresholds from previously received sensorimotor error signals, subsequently refining or updating motor commands for effectors to alter the whole-body motion state [11]. Such implicit trial–error process ultimately induces adaptive improvements in one’s COM state and limb support control for an enhanced outcome (no fall) when encountering a similar context (i.e., perturbation) [26, 27].
However, a large group of trip-perturbation studies were delivered in standing [8, 9, 25, 28, 29], and recovery from stance perturbations might not generalize to gait-perturbations. Stance trips are initiated from a symmetrical bipedal position while gait-trips are initiated from an asymmetrical bipedal support position that better simulates a community-trip. While there is an increasing number of studies inducing trips during treadmill-walking, such as those using a resistance tether or ankle strap attached to the swing foot to induce a trip [30, 31], kinematics of recovery from a treadmill-induced trip, during stance or gait, could differ from obstacle-induced trips and would subsequently influence adaptive training mechanisms. It has been shown that the recovery step, which is critical for reestablishing the BOS and reducing fall-risk, is longer and faster during recovery from an obstacle-induced trip than from a treadmill-induced trip [32]. Further, treadmill-induced trips do not promote adaptations in toe clearance, which is a critical strategy for recovery after encountering obstacles while walking [11, 17].
To date, relatively few studies have attempted to examine adaptations to obstacle-induced trips during over-ground locomotion among older adults, and most studies involving trip perturbations adopted a pre- and post-design or limited their investigation to the novel trip response [8, 9, 14, 24, 25, 28, 29]. In contrast, a series of experiments have been conducted using over-ground-slip-perturbation training with a combination of perturbation threat (slip intensity) and dosage (slip repetition) [33,34,35] to investigate trial-to-trial adaptations [18]. A “slip-no-slip-reslip” paradigm with 24 slips was provided to older adults and the study reported a 50% reduction in falls during daily living with effects retained for 12 months [36]. But, relatively few studies have reported trial-to-trial adaptations to repeated obstacle-induced trips in older adults, even though examining the adaptive pattern of recovery could provide insights into aging-induced deteriorations in reactive motor adaptation [30, 37].
Recent findings in young adults indicated rapid (within three trials) and significant improvements in reactive stability and trunk control over repeated obstacle-induced trips during over-ground gait [11]. In that study, proactive adaptation was also seen in improved pre-trip stability accompanied by larger toe clearances. Similarly, Bhatt et al. [18] and Okubo et al. [38] found young adults demonstrated improved reactive responses to a trip (i.e., longer compensatory step and improved margin of stability and dynamic stability) even from a paradigm with a mixed-slip-and-trip design.
In light of age-related sensorimotor deteriorations [39, 40], it is unclear, yet essential to determine, to what extent older adults can adapt from repeated over-ground, obstacle-induced trips to ultimately reduce falls. Due to older adults’ declining lower extremity muscle strength [41], delayed muscle reaction time, and altered strategies for recovering from a perturbation [42], it remains to be determined if older adults could attain similar recovery strategies and motor adaptations from obstacle-induced trip-perturbation training as were previously seen in young adults. It is also unknown whether a “mixed-and-blocked” paradigm which extends the simple, consecutive repeated trip paradigm would consolidate adaptation effects and retain training effects to the same degree as was seen for the slip-perturbation training.
Therefore, the primary purpose of the study was to investigate the extent to which an obstacle-induced trip paradigm in older adults could reduce trip-induced falls during over-ground gait. We hypothesized that older adults would show reduced incidences of falls on their last trip compared to their novel trip. We expected reduced fall-risk to stem from improved proactive stability control with a larger toe clearance before obstacle-hit, as well as from improved reactive stability control with reduced forward trunk rotation at recovery step completion. The secondary purpose was to examine retention of training-induced effects on an immediate basis. We hypothesized that, although older adults were expected to have some decay in stability control after a brief retention interval, motor learning from the current training protocol would still be retained for at least 30 min and older adults would have fewer falls on the retention trip than their novel trip with this fall rate not differing significantly from the last trip of the initial training session.
Methods
Participants
Forty healthy, community-dwelling older adults (mean age = 67.9 years) were initially screened to pass a cognition test (> 25 on the c [MMSE]) [43], a calcaneal ultrasound screening (T-score > − 2.0) [44], a mobility test (Timed-Up-Go [TUG] < 13.5 s) [45], and a monofilament foot sensation test (able to detect the Weinstein 5.07 monofilament at all nine locations on both feet) [46]. Exclusion criteria included recently (≤ 6 months) self-reported diagnosed neurological, musculoskeletal, or other systemic disorders. Participants also received other commonly used clinical measurements and questionnaires, including the Berg Balance Scale (BBS), Activities-specific Balance Confidence scale (ABC), a fall history questionnaire, and a 6-min walking test (6MWT). All participants provided written informed consent, and this study was approved by the Institutional Review Board in the University of Illinois at Chicago.
Protocol
The obstacle device consisted of a hinged metal plate 8-cm high, 27-cm wide, and 0.5-cm thick. During regular walking, the plate was locked in a flat position by a pair of electromagnets. During trip trials, the electromagnets were powered off (to unlock the plate) when the vertical ground reaction force (GRF) under the unperturbed (right) limb exceeded 80% of participants’ body weight after right heel strike. The springs returned the plate to its upright position in less than 150 ms to induce a trip. Participants were protected by a safety harness connected through a load cell (Transcell Technology Inc., Buffalo Grove, IL) to a low-friction trolley-and-bean system mounted to the ceiling along the walking path. The harness did not limit participants’ maximum voluntary forward reaching while standing (Fig. 1).
The trip was induced by an obstacle device consisting of a hinged metal plate 8-cm high, 27-cm wide, and 0.5-cm thick. During regular walking, the plate was locked in a flat position by a pair of electromagnets. During the perturbation trials, the springs returned the plate to its upright position to induce a trip by obstructing the left leg. The trip plate was triggered by the ground reaction force detected by force plates beneath the walkway. Participants were protected during all trials by a safety harness connected through a load cell mounted to the ceiling along the walking path
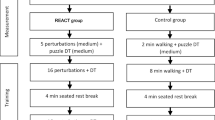
Participants first had 25–35 unperturbed walking trials on the 7-m walkway to become familiar with the laboratory walking environment. They were told “a slip or trip may or may not occur during your walking”. The starting position was adjusted during baseline walking to ensure upcoming trip trials were induced to consistently obstruct participants’ left foot during the mid-to-late swing phase. The unperturbed walking trial (Nat) before the novel trip was analyzed for baseline performance. The subsequent training paradigm adopted a “trip-no-trip-retrip” design following a previously reported “slip-no-slip-reslip” paradigm which induced sufficient adaptive improvements in stability control and yielded long-term training-induced retention [36, 47]. The training consisted of an acquisition session with eight repeated trips (T1–T8), followed by three non-trips (NT1–NT3), another eight trips (T9–T16), an additional three non-trips (NT4–NT6), and a final block of 15 mixed trials. The randomly selected sequence of the mixed-block was consistent for each participant: T17–T18, NT7–NT8, T19, NT9, T20, NT10, T21–T22, NT11–NT12, T23, NT13, and T24. Thirty minutes after training completion, participants received three non-trips followed by a final trip (Retrip) to assess immediate post-training retention (Fig. 2). The three non-trips served as wash-out trials, making the Retrip less predictable.
Schematic of the training protocol. Participants received 25–35 unperturbed walking trials followed by an acquisition session of a block of eight repeated trips (T1–T8), a block of three non-trips (NT1–NT3), another block of eight trips (T9–T16), a second block of three non-trip trials (NT4–NT6), and a final block of mixed trip and unperturbed walking trials. The randomly selected sequence of the mixed-block session was T17–T18, NT7–NT8, T19, NT9, T20, NT10, T21-T22, NT11–NT12, T23, NT13, and T24 for all participants. After 30 min had passed since completion of the initial training, participants took a block of three non-trip trials followed by a trip (Retrip) to test the immediate retention effects of the trip training
Data collection and reduction
An eight-camera motion capture system (Qualysis., Gothenburg, Sweden) recorded data at 120 Hz from 27 reflective markers placed on bilateral upper and lower extremities, the torso, and the trip plate (Fig. 1). Marker data was low-pass filtered at marker-specific cut-off frequencies (range 4.5–9 Hz determined through a residual analysis) using fourth-order Butterworth filters. Force plate and load cell data were collected at 600 Hz and were synchronized with motion data.
Behavior outcome—a fall was determined if the load cell detected more than 30% of the participant’s body weight after trip onset [48] and was verified using motion videos. The recovery strategies were classified as follows: (1) lowering hit, the obstructed foot (left) was quickly lowered to the ground and the contralateral unobstructed foot (right) took a recovery step (Fig. 3a); (2) elevating-hit, the obstructed foot took a recovery step after hitting the obstacle (Fig. 3b); or (3) elevating-cross, subjects crossed over the obstacle without hitting it (Fig. 3c) [23]. The instant of recovery-foot-touchdown was the touchdown of the right or left foot for lowering or elevating/crossing strategies, respectively.
Dynamic gait stability—dynamic stability was defined as the shortest distance between the instantaneous COM state (position and velocity) in the anteroposterior direction, indicating feasible stability limits for forward balance loss [49]. COM position was calculated relative to BOS position normalized by foot length (Relative PCOM), and COM velocity was calculated relative to BOS velocity normalized by \(\sqrt {g*{\text{bh}}}\) (gravitational acceleration [g] and body height [bh]) (Relative VCOM). A greater value indicated more forward instability against forward balance loss. Dynamic stability was measured at two instants indicative of proactive and reactive adaptive performances, respectively: (1) pre-trip: 30 ms before obstacle-hit/cross and (2) post-trip: recovery-foot-touchdown. The instant of obstacle-hit was defined as the time of minimum toe marker acceleration of the obstructed foot (left) in the walking direction [14]. For regular walking trials, the time of obstacle-crossing was defined as the instant when the foremost point of the left foot was immediately above plate location. Events of liftoff and touchdown were identified from the vertical GRF.
Kinematic variables—Toe clearance was measured as the vertical distance from the ground to the left toe at the pre-trip instant [11]. Recovery step length was measured as the heel-to-heel distance between the obstructed foot and the recovery foot for the lowering strategy and the heel-to-heel distance between the foot of the supporting limb (the contralateral stance limb before obstacle-hit) and the obstructed foot for the elevating/obstacle-crossing strategies, normalized by body height (Fig. 3). Proactive and reactive trunk angles were calculated as the angles between the trunk segment (defined by a line connecting the midpoint of the shoulders and the midpoint of the hips) and the vertical line at pre-trip instant and at completion of the first recovery step, respectively. The change in relative VCOM from the instant of the first recovery step touchdown to 100 ms after recovery step completion was also calculated. This duration was selected to examine any immediate recovery response because past studies reported very rapid limb muscle activation served to either support or recover within 100 ms [14, 50].
Statistical analysis
Independent t tests were conducted to detect differences in participants’ baseline demographics (age, height, weight, BBS, ABC, MMSE, TUG, and 6MWT), and a Chi-square test was conducted to examine any differences in gender and history of falls between fallers and non-fallers on the novel trip. The Cochran’s Q test was performed to examine the overall change in fall incidence over trials. The Friedman test was applied to examine the main effects of training on recovery strategies (lowering hit, elevating hit, and obstacle-crossing). Subsequently, the Cochran’s Q test was used to examine the main effects of training on obstacle-crossing and obstacle-hit (combining both hit outcomes). Trials included in the abovementioned analyses were T1–T24 and Retrip. Follow-up comparisons were applied using the McNemar test for binominal variables (fall vs no fall and obstacle-crossing vs obstacle-hit) and the Wilcoxon signed-rank test for the three recovery strategies for these pairs: T1 vs T8, T8 vs T9, T16 vs T17, T1 vs T24, and T24 vs Retrip. One-way repeated ANOVA was performed to analyze the main effects of training (Nat, T1 to T24, and Retrip) on the following variables: pre- and post-trip dynamic stability, pre-trip toe clearance, proactive trunk angle, trunk angle at recovery-foot-touchdown, and recovery step length. Follow-up planned comparisons were conducted via paired-t tests between these pairs: Nat vs T1, Nat vs T24, T1 vs T8, T1 vs T24, T8 vs T9, T9 vs T16, T16 vs T17, T17 vs T24, T24 vs Retrip, and T1 vs Retrip.
Linear regression was performed to examine the relationship between relative PCOM and relative VCOM with pre- and post-trip dynamic stability, as well as the relationship between trunk angle and relative PCOM at pre-trip and recovery foot completion. The relationship between recovery step length and the change in relative VCOM within 100 ms of recovery step completion was also examined using linear regression. All analyses were performed using SPSS (V.24.0, SPSS Inc., IL) with a significance level of p < 0.05.
Results
Fall and behavior outcome
There was a significant difference in gender (p = 0.024), with no other differences in clinical measurements or history of falls, between fallers and non-fallers on the novel trip (Table 1). Fall incidence significantly changed over trials (χ2 (24)=271.335, p < 0.001). Participants had significantly fewer falls in T8 (2.5%) than their novel trip (48%) (p < 0.001). There was no significant difference in fall rates between T8 and T9 or T16 and T17 (all p = 1). Fall rate was significantly lower in T24 (0%) than T1 (p < 0.001) (Fig. 4a). The distribution of recovery strategies differed significantly across trials (χ2 (24) = 79.527, p < 0.001). Follow-up comparisons revealed the recovery strategy differed between T1 and T8 (p = 0.001), T8 and T9 (p = 0.003), T16 and T17 (p = 0.003), and between T1 and T24 (p < 0.001). Further, the rate of obstacle-crossing differed significantly across trials (χ2 (24) = 112.050, p < 0.001). There was a significant difference in the rate of obstacle-crossing between T1 and T8 (p < 0.001), T8 and T9 (p = 0.021), T16 and T17 (p = 0.002), and between T1 and T24 (p < 0.001). During the novel trip, all participants hit the obstacle and attempted to recover using either a lowering (27/40) or elevating (13/40) strategy, and none were able to cross over the obstacle. However, 60% of participants adopted an obstacle-crossing strategy in T24 (Fig. 4b).
Trip recovery outcomes and strategies. Shown are a the percentage of falls for each trip and b the percentage of each strategy used for trip recovery from each trip trial. T represents the trip trials, NT represents the unperturbed walking trials, and Retrip represents the trip trial after the 30-min break
Pre-trip adaptation
Proactive stability was significantly different over trials (main effect: F (25, 900) = 5.299, p < 0.001) (Fig. 5a). Planned comparison revealed participants had comparable proactive stability between Nat and T1 (p = 0.488). Proactive stability was lower in T8 than T1 (p = 0.023) and was lower in T16 than T9 (p = 0.002). Participants were more unstable in T17 than T16 (p = 0.011). There were no further significant differences between pairs (all p > 0.05). By the end of the acquisition session, participants had lower stability (reduced forward instability) in T24 than Nat (p < 0.001) and T1 (p < 0.001) (Fig. 5a).
Pre-trip adaptation in a proactive stability, b toe clearance, and c the relationship between proactive stability and the center of mass (COM) position and velocity relative to the base of support (relative PCOM and relative VCOM, respectively) (proactive stability = 0.015 + 1.097*relative PCOM + 5.269*relative VCOM). Proactive stability was defined as the shortest distance of the instantaneous COM state (position and velocity) from a theoretically predicted threshold for backward or forward loss of balance. Pre-trip, a larger stability value indicated a more unstable initial COM state before obstacle-hit
Pre-trip adaptations were most apparent in increased swing foot toe clearance (main effect: F (25, 825) = 16.337, p < 0.001) (Fig. 5b). There was no significant difference between Nat and T1 (p = 0.077). Toe clearance first increased from T1 to T8 (p < 0.001), lowered from T8 to T9 (p < 0.001), and then further increased from T9 to T16 (p = 0.003). Toe clearance was smaller in T17 than T16 (p < 0.001), but it increased from T17 to T24 (p = 0.003). By the end of training, toe clearance increased by 8.2 cm from T1 to T24 (p < 0.001) and was 7.4 cm higher than in Nat (p < 0.001) (Fig. 5b). There was no significant difference in proactive trunk angle over trials [main effect: F (25, 900) = 3.371, p < 0.730].
Post-trip adaptation
Reactive stability differed significantly across trials [main effect: F (25, 875) = 15.127, p < 0.001] (Fig. 6a). Participants were more unstable in T1 than Nat (p < 0.001). Reactive instability decreased from T1 to T8 (p < 0.001). Participants were more unstable in T9 than T8 (p = 0.003), and then reactive stability further improved from T9 to T16 (p < 0.001). Participants were less stable in T17 than T16 (p < 0.001) but became more stable in T24 than T17 (p = 0.019). By the end of training, reactive instability for T24 significantly decreased from T1 (p < 0.001). In addition, there was no significant difference between T24 and Nat (p = 0.511) (Fig. 6a).
Post-trip adaptation in a reactive stability and b the relationship between reactive stability and the center of mass (COM) position and velocity relative to the base of support (relative PCOM and relative VCOM, respectively) (reactive stability = − 0.561 + 1*relative PCOM + 7.458*relative VCOM). Post-trip, a larger stability value indicated more forward instability and that participants were more likely to fall forward
Reactive trunk angle was also significantly affected by trials [main effect: F (25, 900) = 21.357, p < 0.001)] (Fig. 7a). After the novel trip, participants had a larger forward trunk angle in T1 than Nat (p < 0.001). Forward trunk angle decreased from T1 to T8 (p < 0.001), however, it was larger in T9 than T8 (p = 0.005). Trunk angle further decreased from T9 to T16 (p = 0.001). Forward trunk angle was slightly larger in T17 than T16 (p = 0.024), but there was no significant difference between T17 and T24 following the mixed-block session (p = 0.084). By the end of training, trunk forward rotation was 17.5 degrees smaller than in T1 (p < 0.001), with a slight difference between T24 and Nat (p = 0.042) (Fig. 7a).
Post-trip adaptation in a forward trunk angle at recovery touchdown, b recovery step length normalized to participants’ body height (bh), c the correlation between trunk angle and the center of mass position relative to the base of support (relative PCOM), and d the correlation between recovery step length and the change in COM velocity relative to the base of support (relative VCOM). Changes in relative VCOM were calculated as the differences between relative VCOM at the instant of recovery foot touchdown and the relative VCOM at 100 ms following recovery foot touchdown. Mean values of the recovery step length and the corresponding relative VCOM change for the novel trip and the 24th trip were indicated by triangle and square, respectively
Such proactive and reactive adjustments diminished the need for a long post-trip compensatory step. There was a decreasing trend in recovery step length over trials (main effect: F (25, 875) = 3.946, p < 0.001) (Fig. 7b). Participants demonstrated a longer recovery step in T1 than in Nat (p < 0.001). Recovery step length decreased from T1 to T8 (p < 0.001) with no further change in the following trials. By the end of training, participants had a significantly smaller recovery step length in T24 than in T1 (p < 0.001). The recovery step length in T24 was similar to participants’ step length during natural walking (Nat) (p = 0.308) (Fig. 7b).
Immediate retention of training
There was no significant difference in fall outcomes between Retrip and T24 (p = 1) (Fig. 4a). However, recovery strategies were different between T24 and Retrip (p < 0.001). Fewer participants crossed the obstacle in Retrip (9/40) than T24 (24/40) (p < 0.001) (Fig. 4b). There were also no significant differences in proactive stability, reactive forward trunk rotation or recovery step length between T24 and Retrip (all p > 0.05) (Figs. 5a and 7a, b). Toe clearance was slightly smaller in Retrip than T24 (p = 0.032) (Fig. 5b). Participants also had greater reactive instability (p = 0.001) in Retrip than T24 (Fig. 6a). Nevertheless, toe clearance was 7 cm higher in Retrip than T1 (p < 0.001) (Fig. 5b). Additionally, participants had less reactive instability in Retrip than T1 (p < 0.001) (Fig. 6a) with forward trunk rotation reduced by 15° (p < 0.001) (Fig. 7a).
Mechanism of stability control
A linear regression analysis showed relative PCOM and VCOM, together, explained 100% (r2 = 1) and 94.4% (r2 = 0.944) of pre-trip (Fig. 5c) and post-trip stability (Fig. 6b) changes, respectively. Pre-trip, decreased stability was mainly associated with reduced relative VCOM (r2 = 0.998, p < 0.001) and a posterior shift of relative PCOM (r2 = 0.125, p < 0.001) (Fig. 5c). The relationship was similarly seen post-trip, with decreased stability being associated with reduced relative VCOM (r2 = 0.674, p < 0.001) and a posterior shift of relative PCOM (r2 = 0.422, p < 0.001) (Fig. 6b). Furthermore, a linear regression analysis demonstrated a posterior shift of relative PCOM was associated with reduced forward trunk angle at recovery foot touchdown (r2 = 0.315, p < 0.001) (Fig. 7c). Additionally, linear regression revealed a larger recovery step length was positively correlated with a larger reduction in forward relative VCOM within 100 ms of completion of the first recovery step (r2 = 0.113, p < 0.001) (Fig. 7d).
Discussion
The results supported our first hypothesis that community-dwelling older adults were able to adapt to repeated trip exposures and reduce their incidence of laboratory trip-induced falls in the anterior–posterior direction. Older adults rapidly acquired fall-resisting skills with decreased forward instability after unexpected obstacle-contact. Such motor adaptation involved an interaction between improved proactive and reactive control mechanisms. Our second hypothesis was partially supported as it was evident participants’ fall-rates did not increase after a 30-min retention interval, but they did have a slight deterioration in toe clearance and stability during Retrip.
The trip intensity utilized in our study did successfully induce a fall during older adults’ over-ground locomotion, enabling us to examine acquisition of adaptations to reduce rates of laboratory-induced falls. This differs from previous trip adaptation studies which did not specifically report falls as a behavioral outcome [10, 11, 18, 31, 38]. Older adults in the current study demonstrated a rapid reduction in falls after being exposed to the novel trip. The rate of falls during the second trip (10/40) was about half that of the first trip (19/40), and the rate of falls during the third trip (6/40) was about one-third that of the first trip. Very few participants (< 2) fell during later trials (Fig. 4a). Similarly, Owing et al. [25] reported healthy older adults who fell on the novel trip-induced during treadmill-stance (18/25) successfully recovered in subsequent attempts. Such rapid rates of fall reduction were also seen in slip-perturbation studies in both young and older adults [51, 52], indicating healthy older adults’ retained a similar intact adaptive control across functional activities (i.e., a slip or trip perturbation) as did young adults.
More fallers on the novel trip were women (73.7%) (Table 1). This is consistent with previous findings [53] and provided laboratory-based evidence for generally reported higher rates of falls and fall-related injuries in older women [54]. Besides gender, fallers and non-fallers on the initial trial had comparable clinical measurements and fall histories (Table 1). This suggests common clinical measurements such as the BBS or 6MWT lack the ability to detect reactive responses to perturbations, and hence, lack the ability to discriminate risks for specific types of falls (i.e., a slip or a trip) [55].
Further, findings regarding proactive and reactive adaptations across trials were also in line with previous results in older and young adults. By the end of the acquisition training session, older adults had lower pre-trip instability due to a posterior shift of relative PCOM and a reduced relative VCOM before obstacle-hit (Fig. 5a, c). Pavol et al. [13] reported a faster walking velocity and a forward-leaning COM position prior to obstacle-hit would increase the risk of during-step (recovering using lowering strategy) and after-step (recovering using elevating strategy) falls, respectively, among older adults. In addition, this trend of reduced forward instability before obstacle-hit was similar to that demonstrated in young adults [11, 18]. This suggests an improved feedforward adaptation strategy might have been adopted by the CNS to prepare a more stable initial COM motion state [49, 56].
Increased toe clearance was reported to be an anticipatory behavior to reduce, or even eliminate, subsequent obstacle-contact immediately after a novel trip [11, 18, 38]. Conceivably, a high enough toe clearance may avoid obstacle-hit altogether, however, only 50% of older adults could avoid obstacle-hit during their entire training session (Fig. 4b). However, because the exact dimensions of the obstacle were unknown, there was a chance for destabilization upon obstacle-hit if the preplanned foot trajectory was too low [32]. Pijnappels et al. [57] reported a diminished toe-height after three to five unperturbed trials similar to what was observed in the current study between T8 and T9 and between T16 and T17. Such waned proactive adjustment affected subsequent feedback control such that participants had reduced stability and trunk control in T9 and T17 compared to T8 and T16, respectively. Moreover, raising the limb more than necessary may require additional energy cost [58]. Thus, the CNS could not solely rely on anticipatory control to avoid subsequent forward balance loss, and improvements in reactive control were essential to recover during the following trials.
Taken together, the results suggest participants mainly focused on toe elevation and reduced velocity for proactive trip adaptation, rather than altering COM position or trunk angle prior to obstacle-hit.
Reactively, older adults demonstrated decreased forward instability stemming from a posterior shift of relative PCOM and reduced relative VCOM at recovery foot touchdown (Fig. 6b). Improved COM stability was coupled with reduced forward trunk rotation, contributing to the posterior shift of relative PCOM. Such adaptive reactive control was similarly reported in treadmill-stance trips [9], treadmill-gait trips [59, 60], and over-ground obstacle-induced trips in young adults [11, 18]. Although an insufficient compensatory step length was the key factor for failure to recover from a trip [25, 61], older adults in the current study showed reduced recovery step lengths after exposure to repeated over-ground obstacle-induced trips, which was consistent with young adults [11, 18]. On the novel trip, a larger recovery step was necessary to mitigate the increased relative VCOM caused by obstacle-hit (Fig. 7d). As proactive and reactive stability improved on the 24th trip, relative VCOM at recovery foot touchdown reduced drastically, which diminished the need for a longer recovery step (Fig. 7d), reflecting a shift from feedback to feedforward control. Similarly, improved feedforward adjustment diminished the need to take a backward recovery step after repeated over-ground slips [26]. However, reduced compensatory step lengths across training were rarely reported for repeated treadmill-induced trips. Dijkstra et al. [62] did not find a significant difference in compensatory step length after repeated treadmill-trips. The longer compensatory step indicates adaptive reactive control upon exposure to repeated treadmill-trips [30] in which the CNS predominantly relies on a feedback system. Such a difference might be key for differentiating over-ground-gait obstacle-induced perturbations from treadmill-gait perturbations.
Only recently have training-induced retention effects from a treadmill-induced trip-perturbation training been reported. Studies found improved reactive control could be retained for a month [60], 14 weeks [63], and even 1.5 years [59], with only a minor decay in the margin of stability. However, only margin of stability was examined in those studies and retention of fall outcomes has not been reported. The present study made the first attempt to examine retention for an over-ground trip training paradigm on an immediate basis (30 min post-training) to exclude potential distractors outside the laboratory. In the retest session, we observed a diminished toe clearance (1 cm) compared to T24 (Fig. 5b). This decayed toe clearance might be due to an anticipatory error as proactive adjustments are based on the CNS’s prediction of the upcoming context based on previous experiences [64]. Therefore, the three unperturbed walking trials before Retrip could have served as wash-out trials, eliciting error. Such 1 cm decay led to more obstacle-contact in Retrip (31/40) than in T24 (16/40) (Fig. 4b). Obstacle-hit could have also increased the body’s external forward angular momentum [53], leading to a more unstable COM state and a larger forward trunk angle at recovery touchdown in Retrip than T24 (Figs. 6a and 7a). The partial retention might also be due to individual differences which were reported in an over-ground slip retention study [47]. However, a point-biserial correlation for the current study revealed a positive correlation between obstacle-crossing in Retrip and the total number of successful obstacle-crossings across all 24 trips in the acquisition session (rbp = 0.656, p < 0.001). This means participants who avoided the obstacle during Retrip tended to have a higher ratio of obstacle-avoidance during training. Therefore, further investigation is needed to examine the mechanism underlying individual differences. Nonetheless, the slight decay did not alter older adults’ fall-rate during retest.
Although three to five perturbations were sufficient to induce adaptive improvements in balance loss [51, 65], a “mixed-and-blocked” design, identical to a well-studied over-ground slip training paradigm, was adopted in the current trip-training paradigm. This “overtraining” with extra trials in a blocked and random design was previously confirmed to further enhance over-ground training-induced retention over 12 months [36]. However, different than what was seen in the training effects from previous slip studies during the mixed-block [47, 51], participants did not reach a steady state of toe elevation prior to trips (toe clearance: T24 > T17) or reactive stability control after repeated trips (forward instability: T24 < T17). These findings of partial retention after trip-perturbation training compared to the complete retention after slip-perturbation training designed in the same manner might suggest individual differences acquiring perturbation-induced adaptations, as previously demonstrated [47], and this paradigm might not have provided sufficient stimuli, in terms of either practice dosage (number of repetitions) or intensity dosage (plate height), for adequate motor learning in all participants.
The findings of this study must be interpreted in light of its limitations. Trips were always induced during left foot swing with the trip plate fixed in a certain location, however, in real-life, the trip could happen in various locations to perturb either leg. Therefore, further studies should test whether training effects could be transferred from the left side to the right side, or to a trip presented at a different location. The intensity (height of the trip plate) adopted is only one of many options to produce successful training effects, and we are unsure whether a higher trip plate or mixed obstacle heights would exert better adaptation and retention. Additionally, the current training protocol which only tripped participants walking in the anterior–posterior direction might have limited improvements on their responses to a trip occurs in the medio-lateral direction. In addition, only healthy older adults were included in the current study which most likely does not represent the population of older populations most likely to fall. Nonetheless, there is still a high incidence of environmental falls reported in such a healthy, community-dwelling older adult population.
In conclusion, the rapid adaptive improvements in stability control demonstrated by healthy older adults were similar to that of young adults following repeated obstacle-induced trips, resulting in significant reduction of falls across trials in the laboratory environment. Additionally, such acquired adaptive improvements could be retained on a short-term basis for 30 min to prevent a trip-related fall induced in the same context. Given the positive findings of improved adaptive control from a single session and the potential to induce short-term retention, such perturbation training, added as a supplement to conventional training or combined with other perturbation approaches such as slip or perturbation in the medio-lateral direction, could potentially reduce fall-risk among older adults. Future studies should examine dose–response relationships that would facilitate translation of such intervention for clinical application. Moreover, prospective studies need to establish efficacy of such perturbation training for real-life fall-risk reduction.
References
Bergen G, Stevens MR, Burns ER (2016) Falls and fall injuries among adults aged ≥65 years—United States, 2014. MMWR Morb Mortal Wkly Rep 65:993–998
Li W et al (2006) Outdoor falls among middle-aged and older adults: a neglected public health problem. Am J Public Health 96:1192–1200
Robinovitch SN et al (2013) Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study. Lancet 381:47–54
Rosen T, Mack KA, Noonan RK (2013) Slipping and tripping: fall injuries in adults associated with rugs and carpets. J Inj Violence Res 5:61
Verma SK et al (2016) Falls and fall-related injuries among community-dwelling adults in the United States. PLoS One 11:e0150939
Stenhagen M et al (2014) Accidental falls, health-related quality of life and life satisfaction: a prospective study of the general elderly population. Arch Gerontol Geriatr 58:95–100
Bieryla KA, Madigan ML, Nussbaum MA (2007) Practicing recovery from a simulated trip improves recovery kinematics after an actual trip. Gait Posture 26:208–213
Crenshaw JR et al (2012) The discriminant capabilities of stability measures, trunk kinematics, and step kinematics in classifying successful and failed compensatory stepping responses by young adults. J Biomech 45:129–133
Grabiner MD et al (2012) Task-specific training reduces trip-related fall risk in women. Med Sci Sports Exerc 44:2410–2414
Potocanac Z et al (2014) Fast online corrections of tripping responses. Exp Brain Res 232:3579–3590
Wang TY et al (2012) Adaptive control reduces trip-induced forward gait instability among young adults. J Biomech 45:1169–1175
Pai YC et al (2000) Thresholds for step initiation induced by support-surface translation: a dynamic center-of-mass model provides much better prediction than a static model. J Biomech 33:387–392
Pavol MJ et al (2001) Mechanisms leading to a fall from an induced trip in healthy older adults. J Gerontol A Biol Sci Med Sci 56:M428–M437
Pijnappels M, Bobbert MF, van Dieen JH (2005) How early reactions in the support limb contribute to balance recovery after tripping. J Biomech 38:627–634
Schillings A, Mulder T, Duysens J (2005) Stumbling over obstacles in older adults compared to young adults. J Neurophysiol 94:1158–1168
Barbieri FA et al (2014) Interactions of age and leg muscle fatigue on unobstructed walking and obstacle crossing. Gait Posture 39:985–990
Barrett RS, Mills PM, Begg RK (2010) A systematic review of the effect of ageing and falls history on minimum foot clearance characteristics during level walking. Gait Posture 32:429–435
Bhatt T et al (2013) Adaptation and generalization to opposing perturbations in walking. Neuroscience 246:435–450
Gillespie LD, Robertson MC, Gillespie WJ et al (2012) Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD007146.pub3
Luukinen H et al (2000) Fracture risk associated with a fall according to type of fall among the elderly. Osteoporos Int 11:631–634
Province MA et al (1995) The effects of exercise on falls in elderly patients. A preplanned meta-analysis of the FICSIT Trials. Frailty and Injuries: cooperative studies of intervention techniques. JAMA 273:1341–1347
Pavol MJ et al (2002) Influence of lower extremity strength of healthy older adults on the outcome of an induced trip. J Am Geriatr Soc 50:256–262
Eng JJ, Winter DA, Patla AE (1994) Strategies for recovery from a trip in early and late swing during human walking. Exp Brain Res 102:339–349
Pijnappels M, Bobbert MF, van Dieen JH (2004) Contribution of the support limb in control of angular momentum after tripping. J Biomech 37:1811–1818
Owings TM, Pavol MJ, Grabiner MD (2001) Mechanisms of failed recovery following postural perturbations on a motorized treadmill mimic those associated with an actual forward trip. Clin Biomech 16:813–819
Bhatt T, Wening JD, Pai YC (2006) Adaptive control of gait stability in reducing slip-related backward loss of balance. Exp Brain Res 170:61–73
Wolpert DM, Ghahramani Z, Jordan MI (1995) An Internal Model for Sensorimotor Integration. Science 269:1880–1882
Oludare SO et al (2018) Trip-specific training enhances recovery after large postural disturbances for which there is NO expectation. Gait Posture 61:382–386
Pater ML, Rosenblatt NJ, Grabiner MD (2015) Expectation of an upcoming large postural perturbation influences the recovery stepping response and outcome. Gait Posture 41:335–337
Karamanidis K, et al (2011) Reactive response and adaptive modifications in dynamic stability to changes in lower limb dynamics in the elderly while walking. In: 15th Nordic-Baltic Conference on Biomedical Engineering and Medical Physics (NBC 2011). Springer
Shirota C, Simon AM, Kuiken TA (2014) Trip recovery strategies following perturbations of variable duration. J Biomech 47:2679–2684
Troy KL, Grabiner MD (2005) The presence of an obstacle influences the stepping response during induced trips and surrogate tasks. Exp Brain Res 161:343–350
Bhatt T, Pai YC (2009) Prevention of slip-related backward balance loss: the effect of session intensity and frequency on long-term retention. Arch Phys Med Rehabil 90:34–42
Lee A, Bhatt T, Pai YC (2016) Generalization of treadmill perturbation to overground slip during gait: effect of different perturbation distances on slip recovery. J Biomech 49:149–154
Liu X, Bhatt T, Pai YC (2016) Intensity and generalization of treadmill slip training: high or low, progressive increase or decrease? J Biomech 49:135–140
Pai YC et al (2014) Perturbation training can reduce community-dwelling older adults’ annual fall risk: a randomized controlled trial. J Gerontol A Biol Sci Med Sci 69:1586–1594
McCrum C et al (2016) Locomotor stability and adaptation during perturbed walking across the adult female lifespan. J Biomech 49:1244–1247
Okubo Y et al (2018) Exposure to trips and slips with increasing unpredictability while walking can improve balance recovery responses with minimum predictive gait alterations. PLoS One 13:e0202913
Horak FB, Shupert CL, Mirka A (1989) Components of postural dyscontrol in the elderly: a review. Neurobiol Aging 10:727–738
Stelmach GE et al (1989) Age related decline in postural control mechanisms. Int J Aging Hum Dev 29:205–223
Goodpaster BH et al (2006) The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci 61:1059–1064
Lin S, Woollacott M, Jensen J (2002) Differentiating postural responses following dynamically changing balance threats in young adults, healthy older adults and unstable older adults: electromyography. J Mot Behav 34:37–44
Folstein M, Folstein S, McHugh P (1975) Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Thompson PW et al (1998) Quantitative ultrasound (QUS) of the heel predicts wrist and osteoporosis-related fractures in women age 45–75 years. J Clin Densitom 1:219–225
Podsiadlo D, Richardson S (1991) The timed “Up and Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39:142–148
Kumar S et al (1991) Semmes-Weinstein monofilaments: a simple, effective and inexpensive screening device for identifying diabetic patients at risk of foot ulceration. Diabetes Res Clin Pract 13:63–67
Bhatt T, Wang E, Pai YC (2006) Retention of adaptive control over varying intervals: prevention of slip- induced backward balance loss during gait. J Neurophysiol 95:2913–2922
Yang F, Pai YC (2011) Automatic recognition of falls in gait-slip training: harness load cell based criteria. J Biomech 44:2243–2249
Pai YC, Patton J (1997) Center of mass velocity-position predictions for balance control. J Biomech 30:347–354
Schillings AM et al (2000) Muscular responses and movement strategies during stumbling over obstacles. J Neurophysiol 83:2093–2102
Pai YC et al (2010) Inoculation against falls: rapid adaptation by young and older adults to slips during daily activities. Arch Phys Med Rehabil 91:452–459
Pavol MJ, Runtz EF, Edwards BJ et al (2002) Age influences the outcome of a slipping perturbation during initial but not repeated exposures. J Gerontol A Biol Sci Med Sci 57:M496–M503
Pijnappels M, Bobbert MF, van Dieen JH (2005) Push-off reactions in recovery after tripping discriminate young subjects, older non-fallers and older fallers. Gait Posture 21:388–394
Talbot LA et al (2005) Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC Public Health 5:86
Bhatt T et al (2011) Dynamic gait stability, clinical correlates, and prognosis of falls among community-dwelling older adults. Arch Phys Med Rehabil 92:799–805
Wu M et al (2007) Minimal step length necessary for recovery of forward balance loss with a single step. J Biomech 40:1559–1566
Pijnappels M, Bobbert MF, van Dieen JH (2006) EMG modulation in anticipation of a possible trip during walking in young and older adults. J Electromyogr Kinesiol 16:137–143
Patla AE, Rietdyk S (1993) Visual control of limb trajectory over obstacles during locomotion—effect of obstacle height and width. Gait Posture 1:45–60
Epro G et al (2018) Retention of gait stability improvements over 1.5 years in older adults: effects of perturbation exposure and triceps surae neuromuscular exercise. J Neurophysiol 119:2229–2240
McCrum C et al (2018) Retention, savings and interlimb transfer of reactive gait adaptations in humans following unexpected perturbations. Commun Biol 1:230
Grabiner MD et al (1993) Kinematics of recovery from a stumble. J Gerontol 48:M97–M102
Dijkstra BW et al (2015) Older adults can improve compensatory stepping with repeated postural perturbations. Fron Aging Neurosci 7:201
König M et al (2018) Retention of improvement in gait stability over 14 weeks due to trip-perturbation training is dependent on perturbation dose. J Biomech 84:243–246
Vetter P, Wolpert DM (2000) Context estimation for sensorimotor control. J Neurophysiol 84:1026–1034
Pavol MJ, Runtz EF, Pai YC (2004) Young and older adults exhibit proactive and reactive adaptations to repeated slip exposure. J Gerontol A Biol Sci Med Sci 59:494–502
Acknowledgements
This work was supported by the National Institutes of Health [RO1-AG050672-01A1]. The authors thank Ms. Alison Schenone for helpful edit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interests in the manuscript.
Statement of human and animal rights
This study was approved by the Institutional Review Board in the University of Illinois at Chicago.
Informed consent
All participants provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Y., Wang, S., Bolton, R. et al. Effects of task-specific obstacle-induced trip-perturbation training: proactive and reactive adaptation to reduce fall-risk in community-dwelling older adults. Aging Clin Exp Res 32, 893–905 (2020). https://doi.org/10.1007/s40520-019-01268-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01268-6