Abstract
Purpose
Various factors have been shown to affect the rehabilitation outcome of hip fractured patients. Considering the decrease in muscle mass with aging and its impact on mobility, we hypothesized that a relationship exists between hand grip strength and rehabilitation outcome.
Methods
We retrospectively studied 373 post-hip fracture patients, admitted for rehabilitation. Muscle strength was measured by hand grip dynamometer. Main outcome measures: functional independence measure motor functional independence measure, motor functional independence measure effectiveness and length of stay). A favorable functional gain was defined as a motor Functional Independence Measure effectiveness score > 0.5. The Spearman correlation assessed the associations between hand grip strength and outcome measures. A multiple linear regression model tested whether hand grip strength was an independent predictor of discharge motor Functional Independence Measure scores and length of stay
Results
Significant correlations were found between hand grip strength and functional outcomes. A significant independent association was found between hand grip strength and discharge motor Functional Independence Measure score after adjustment for confounding demographic and clinical variables. High hand grip strength on admission was significantly associated with a greater chance of achieving a favorable functional gain (OR 1.064, 95% CI, 1.01–1.13; p = 0.032). Hand grip strength was not found to be associated with length of stay.
Conclusion
Hand grip strength is independently associated with rehabilitation outcome in post-acute frail hip fractured patients. Initial screening for hand grip strength on admission may help identify patients who require an intensive resistance exercise program.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fracture often occurs in frail older people and is a major concern for the health care systems because it is associated with an up to 36% excess mortality within 1 year. Hip fracture also represents a risk factor for further falls and fractures, functional decline and institutionalization, with < 40% of hip fractured patients regaining their preinjury level of ambulation [1,2,3]. Predicting functional outcomes of hip fractured patients may enable clinicians to select treatment interventions, set rehabilitation goals and coordinate expectations with the patients and caregivers to plan a proper discharge program.
Rehabilitation outcome of hip fractured patients has been shown to be associated with a number of factors, including muscle strength [4,5,6,7,8]. Whereas hand grip strength (HGS) has been acknowledged as a direct measure of hand strength, it has frequently been applied as an overall measure of body strength [7, 9]. HGS is considered to be a reliable and portable strength test that can be administered in different settings [7,8,9,10]. Previous studies have shown that HGS may predict important outcomes such as post-operative complications, morbidity and mortality, increased length of stay (LOS), functional decline and institutionalization amongst middle-aged and older people [10, 11]. A reduced HGS was found to be associated with a poor ability to perform activities of daily living (ADL) and ambulation in hip fractured patients [4,5,6,7,8]. A recent systematic review and meta-analysis found that sarcopenia is a significant predictor of readmission in old inpatients, but is not associated with hospitalization or length of stay in community-dwelling old adults [12]. Nevertheless, to the best of our knowledge, an association with rehabilitation outcome in post-acute frail hip fractured patients has as yet not been studied. The aim of this study was to assess the association between HGS and rehabilitation achievements in post-acute hip fractured patients.
Methods
Participants
This retrospective study was performed in a university-affiliated 300-bed major free-standing post-acute geriatric rehabilitation center, admitting older patients from nearby major acute hospitals. All consecutive hip fractured patients admitted to a 60-bed rehabilitation department from January 2016 to December 2017, were enrolled in the study. Patients who had not completed the rehabilitation program (i.e., were admitted to a general hospital or skilled nursing ward due to worsening of their medical condition, died during the program or unexpectedly ceased rehabilitation) were omitted from the statistical analyses.
Rehabilitation setting
The multidisciplinary team provided medical, nursing, physical, occupational, and social work interventions. Rehabilitation care included: (1) 30–45 min of individual physical therapy (PT) [i.e., improving transferring, walking the length of a room, climbing stairs, equilibrium and joint range of motion (ROM)], 2–3 times a week; (2) 30–40 min of physical therapy in an adapted fitness room, including muscle resistance training of major muscle groups (two sets of 8–12 repetitions), aerobic training on a treadmill with and without partial weight support and stationary bicycles, 2–3 times a week; (3) 30– 40 min of virtual reality training of challenging functional tasks, two times a week and (4) 30–45 min of individual occupational therapy (OT), (i.e., improving of basic ADL, cognitive evaluation and stimulation, safety education, and learning to use assistive devices), three times a week. Weekly meetings were held with the multidisciplinary team as to the continuation of treatment and a progress review.
Measures
Functional, clinical and demographic data of patients admitted to rehabilitation were collected from their medical files. Functional variables included the functional independence measure (FIM) instrument [13], a disability measure administered on admission and at discharge. The FIM comprises 18 parameters, each rated on a scale of 1–7 according to the degree of assistance required to perform a specific activity in 3 domains: ADL (8 parameters), mobility level (5 parameters) and cognitive function (5 parameters). The motor FIM (mFIM) includes 13 parameters of ADL and mobility. The maximal total score for the FIM is 126 and for the mFIM, 91. The patient’s FIM score was assessed at multidisciplinary team meetings. Cognitive function was measured by the Mini Mental State Examination (MMSE) [14] and administered by occupational therapists. The degree of home care was defined as: dependent (24-hour assistance/supervision by staff provided by a health care agency); partially dependent (assistance in basic ADL, usually 10–15 h/week, staff provided by the Israeli Social Security Agency) and independent (no assistance needed).
Clinical variables included comorbidity and albumin level on admission. Vascular burden was defined as ≥ 3 cardiovascular diseases. Demographic variables included: gender, living arrangements (home vs. nursing home), presence of a caregiver and educational level (elementary < 10 years; higher education ≥ 10 years). Data relating to the fracture included: fracture type (extracapsular, intracapsular), fracture side, type of treatment (operation, conservative), days from fracture to surgery and days from operation to rehabilitation. LOS was defined as the number of days patients resided in the rehabilitation center. Discharge destination and level of home care assistance at discharge were also recorded.
Functional gain was determined as an FIM and mFIM score change (discharge score–admission score). The relative functional gain achieved on the mFIM (mFIM effectiveness) score was calculated by the Montebello Rehabilitation Factor Score (MRFS) [15,16,17] which was designed to overcome the floor and ceiling effect problem and used to calculate each patient’s specific potential for improvement: mFIM score change (discharge mFIM score-admission mFIM score) divided by the mFIM maximum score (91) minus the mFIM admission score.
Assessing muscle strength
Isometric HGS was measured on admission, using the Camry® Digital Hand Grip Dynamometer. Results were expressed in kilograms (100-g intervals). Assessment was carried out in a sitting position. The procedure was demonstrated to the patients and one trial prior to measurements was performed to ensure their cooperation. The patients were instructed to keep their shoulder adducted and neutrally rotated, with the elbow flexed at 90° and the wrist in a neutral position and to squeeze the Camry HG with maximal strength. The highest results of two HGS trials with the dominant hand were recorded.
Statistical analysis
Statistical analysis was performed using the SPSS 19 for Windows. Data were expressed as either mean ± SD, medians and/or frequencies, as appropriate. A nonparametric Spearman's correlation assessed the associations between HGS and outcome measures. A favorable functional gain was defined as an mFIM effectiveness > 50% [16]. The significance of differences or associations in clinical, demographic, and comorbidity variables between patients who achieved a favorable functional gain during rehabilitation and those who did not, was assessed by the Mann–Whitney U and the Chi-square tests, respectively.
A multiple linear regression model estimated the association between admission HGS and outcome measures (discharge FIM and mFIM scores, mFIM effectiveness) and between admission HGS and LOS after controlling for sociodemographic characteristics and chronic diseases. A logistic regression analysis assessed the association between HGS and achievement of favorable rehabilitation outcome (mFIM effectiveness > 0.5).
The hospital’s Institutional Review Board (#0198–18-RMC) approved the study.
Results
Population description
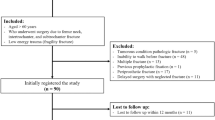
The initial study population consisted of 433 patients admitted from January 2016–December 2017. Sixty patients were excluded from the final analysis: 35 were admitted to an acute hospital due to a worsening of their medical condition, five experienced complications during hospitalization and were transferred to a skilled nursing ward, 10 died during rehabilitation and 10 left before completion their rehabilitation program. Table 1 presents the demographic, clinical and functional characteristics of the two groups (included vs. excluded). The group included in the study, showed a significant lower percentage of individuals with a higher educational level, fewer were living with caregivers, had a significant better metabolic status, presented with a significantly higher functional level upon admission to rehabilitation and exhibited a significantly lower rate of vascular burden compared with the excluded group. No significant differences were noted in HGS between the two patient groups of both sexes. Of the 373 patients who terminated the rehabilitation program, 313 (83.9%) were discharged home; 128 (34.3%) needed partial assistance at home and 245 (65.7%) needed 24-h assistance.
Hand grip strength
Significant correlations were found between HGS and functional outcomes, but not with LOS (Table 2). No correlation was found between time to surgery and HGS (r = 0.015; p = 0.775); whereas, a low yet significant correlation, was found between time from operation to rehabilitation and HGS (r = − 0.151; p = 0.005).
A multiple linear regression analysis showed that HGS was significantly associated with a discharge mFIM score after adjustment for confounding demographic and clinical variables (Table 3).
A logistic regression revealed that the HGS on admission was significantly associated with a lower chance of achieving a favorable functional gain (mFIM effectiveness > 0.5). The higher the HGS, the greater the chances of achieving a favorable functional gain (OR 1.064, 95% CI, 1.01–1.13; p = 0.032) (Table 4).
HGS was not found to be associated with LOS (Table 5).
Discussion
The study results show that HGS is associated with rehabilitation outcomes in post-acute hip fractured patients. Many factors are known to affect functional outcome after hip fracture, the most significant include pre-fracture functional and cognitive level [18,19,20]. These factors were shown to be significant in the current study as well. Nevertheless, HGS was also found to be an independent predictor of functional outcome (as measured by the FIM tool) and for the achievement of favorable functional gain defined as mFIM effectiveness > 0.5) [16]. Previous studies have already demonstrated that HGS can be used as a marker of muscle strength and that it is associated with physical performance in community-dwelling older people. Rantanen et al showed that assessment of HGS in middle-aged individuals was highly predictive of functional limitations 25 years later [21]. Low HGS has been associated with increased mortality, post-operative complications, increased LOS and increased disability amongst middle-aged and older people [10, 11]. Cooper et al in a meta-analysis based on 13 studies, found that higher HGS was associated with lower subsequent mortality [22].
HGS was also found to be a significant factor affecting functional outcome and mobility recovery in hip fractured patients. Beloosesky et al found that measuring HGS a week after a hip fracture operation was highly correlated with motor functioning 6 months later [4]. Di Monaco et al showed that assessment of HGS in hip fractured patients on admission to rehabilitation was associated with the ability to perform ADL at the end of the inpatient rehabilitation and 6 months later [5]. Visser et al. found that loss of muscle strength, but not muscle mass from baseline to 12 months after hip fracture, was associated with a poorer recovery of mobility function [7]. Savino et al. showed that HGS, assessed upon hospital admission before hip surgery, predicted walking recovery 1 year post-surgery [8].
Post-acute patients are usually very old and frail. At the age of 83 years, the average age of the current study population, patients had already lost > 50% of their muscle mass compared with individuals of 30 years old. The loss of muscle mass (sarcopenia), involves a number of underlying mechanisms including intrinsic changes in the muscle and central nervous system (such as a decrease in the proportion in type II fibers, a reduction in mitochondrial and myofibrillar protein synthesis rates, mitochondrial damages, loss of alpha motor units from the spinal cord) and humoral factors (alteration in hormone and cytokine production). Inadequate protein intake and low physical inactivity, common amongst older people, also contribute to the development of sarcopenia [23,24,25]. Several studies have suggested that the decrease in muscle strength is caused by increased fat infiltration, which occurs with ageing and contributes to the decline in muscle quality [26,27,28]. A critical review of available methods for muscle mass estimation, highlighting strengths and weaknesses of each, as well as their proposed field of application was published by Tosato et al [29]. A positive correlation was found between muscle mass and strength [30, 31]. Nevertheless, a decrease in muscle mass was not always found to be associated with a decrease in physical performance, whereas, a decrease in muscle strength was [7, 32, 33]. Similarly, Beaudart et al found that poor quality of life is more related to muscle function than muscle mass [34].
Woods et al. found that hip strength is an important indicator of physical functioning and, therefore, its measurement may be a useful screening tool in detecting patients at risk of functional decline and a requirement for additional care [33]. Hayashida et al. demonstrated that muscle strength is significantly correlated with walking speed in both older men and women [31]. Prevention of decline in muscle strength, according to these authors, is necessary for health promotion in older people. Visser et al. found that lower knee extensor muscle strength is associated with an increased risk of loss of mobility in older men and women [28]. Several studies have examined the issue of exercising in improving muscle strength in the elderly. Host et al. found strong correlations between training intensity, lower extremity strength gains as well as improvements in measures of physical function [35]. They suggested that frail elderly adults post-hip fracture might benefit by extending their rehabilitation in a supervised exercise setting performing at high intensities to optimize gains in strength and physical function. Sylliaas et al. found that 12 weeks of progressive strength training, performed once a week as a follow-up to a more intensive training period, improves strength and endurance and results in better self-reported extended ADL and self-perceived health in post-hip fracture patients [36]. They claim that hip fractured patients comprise a group needing long-term follow-up to achieve the improvements crucial for independent functioning. Lee et al. in a meta-analysis, reported that progressive resistance exercise significantly improved overall physical functions after hip fracture surgery compared with a control group [37]. This was particularly effective in the areas of mobility, ADL, balance, lower limb strength and performance task outcomes.
The uniqueness of our study is the supplemental data regarding post-acute frail hip fractured patients. Our results suggest that HGS should be added to a growing list of factors associated with rehabilitation outcome in post-acute frail hip fractured patients. Further studies, however, are required to assess whether HGS might provide better or additional prognostic value compared to functional assessment by the FIM tool on admission to rehabilitation.
The multidisciplinary team should place a greater emphasis on increasing muscle strength when designing a rehabilitation program [37, 38]. In addition to aerobic training and flexibility exercises, physical therapy should include strength training to all large muscle groups taking place in a fitness room for at least two days per week. The training should be planned according to the American College of Sport Medicine’s (ACSM) guidelines for the elderly [39]. Patients and caregivers should also be encouraged to self-exercise during their free time in post-acute care. Progressive training after discharge is also recommended for those patients who are able to participate in the intervention [18, 35, 36]. A coordination of expectations with patients and caregivers, regarding rehabilitation outcome and the degree of assistance needed after discharge, can be achieved, taking into account the patient’s muscle strength.
Limitations
Our study has several limitations. The study population was comprised of patients hospitalized in one ward in one post-acute geriatric rehabilitation center, a fact that may weaken the generalization of our results. This was a retrospective study with its inherent limitations such as available outcome measures from patients’ files, missing data, etc. which might bias the results. There is no clear definition for favorable rehabilitation outcomes. We used the mFIM effectiveness and a cutoff of 0.5. This parameter, however, is not suitable for all populations and settings, thus comparisons of results might be limited. Finally, albeit, we tried to control for the possible effect of confounding, we cannot totally exclude the possibility of residual confounding associated with drugs and lifestyle habits (smoking, food intake, physical exercise).
Conclusion
HGS is associated with rehabilitation outcome in post-acute frail hip fractured patients. Assessment of HGS may assist the multidisciplinary team in identifying patients who require an intensive resistance exercise program and enable a coordination of expectation with patients and caregivers regarding rehabilitation goals and expected outcome.
References
Haleem S, Lutchman L, Mayahi R et al (2008) Mortality following hip fracture: trends and geographical variations over the last 40 years. Injury 39:1157–1163
National Institute for Clinical Effectiveness: Clinical Guideline 124 - Hip Fracture. https://www.nice.org.uk/guidance/cg124/resources/hip-fracture-management-35109449902789). Accessed 11 Jul 2017
Zuckerman JD (1996) Hip fracture. N Engl J Med 6:1519–1525
Beloosesky Y, Weiss A, Manasian M et al (2010) Handgrip strength of the elderly after hip fracture repair correlates with functional outcome. Disabil Rehabil 32:367–373
Di Monaco M, Castiglioni C, De Toma E et al (2014) Handgrip strength but not appendicular lean mass is an independent predictor of functional outcome in hip-fracture women: a short-term prospective study. Arch Phys Med Rehabil 95:1719–1724
Di Monaco M, Castiglioni C, De Toma E et al (2015) Handgrip strength is an independent predictor of functional outcome in hip-fracture women: a prospective study with 6-month follow-up. Medicine 94:1–6
Visser M, Harris TB, Fox KM et al (2000) Change in muscle mass and muscle strength after a hip fracture: relationship to mobility recovery. J Gerontol A Biol Sci Med Sci 55:M434–440
Savino E, Martini E, Lauretani F et al (2013) Handgrip strength predicts persistent walking recovery after hip fracture surgery. Am J Med 126:1068–1075
Sherrington C, Lord SR (2005) Reliability of simple portable tests of physical performance in older people after hip fracture. Clin Rehabil 19:496–504
Bohannon RW (2001) Dynamometer measurements of hand-grip strength predict multiple outcomes. Percept Mot Skills 93:323–328
Bohannon RW (2008) Hand-grip dynamometry predicts future outcomes in aging adults. J Geriatr Phys Ther 31:3–10
Zhao Y, Zhang Y, Hao Q et al (2019) Sarcopenia and hospital-related outcomes in the old people: a systematic review and meta-analysis. Aging Clin Exp Res 31:5–14
Hamilton BB, Granger CV, Sherwin FS et al (1987) A uniform national data system for medical rehabilitation. In: Fuhrer MJ (ed) Rehabilitation outcomes: analysis and measurement. Brookes Publishing Company, Buffalo, NY, pp 137–147
Folstein MF, Folstein SE, McHuge PR (1975) “Mini-Mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Rolland Y, Pillard F, Lauwers-Cances V et al (2004) Rehabilitation outcome of elderly patients with hip fracture and cognitive impairment. Disabil Rehabil 26:425–431
Heruti RJ, Lusky A, Barell V et al (1999) Cognitive status at admission: does it affect the rehabilitation outcome of elderly patients with hip fracture? Arch Phys Med Rehabil 80:432–436
Koh GC, Chen CH, Petrella R et al (2013) Rehabilitation impact indices and their independent predictors: a systematic review. BMJ Open 3:e003483
Beaupre LA, Binder EF, Cameron ID et al (2013) Maximising functional recovery following hip fracture in frail seniors. Best Pract Res Clin Rheumatol 27:771–788
Mukka S, Knutsson B, Krupic F et al (2017) The influence of cognitive status on outcome and walking ability after hemiarthroplasty for femoral neck fracture: a prospective cohort study. Eur J Orthop Surg Traumatol 27:653–658
McGilton KS, Chu CH, Naglie G et al (2016) Factors influencing outcomes of older adults after undergoing rehabilitation for hip fracture. J Am Geriatr Soc 64:1601–1609
Rantanen T, Guralnik JM, Foley D et al (1999) Midlife hand grip strength as a predictor of old age disability. JAMA 281:558–560
Cooper R, Kuh D, Hardy R et al (2010) Objectively measured physical capability levels and mortality: systematic review and meta-analysis. BMJ 341:c4467
Walrand S, Guillet C, Salles J et al (2011) Physiopathological mechanism of sarcopenia. Clin Geriatr Med 27:365–385
Nilwik R, Snijders T, Leenders M et al (2013) The decline in skeletal muscle mass with aging is mainly attributed to a reduction in type II muscle fiber size. Exp Gerontol 48:492–498
Degens H (2007) Age-related skeletal muscle dysfunction: causes and mechanisms. Musculoskelet Neuronal Interact 7:246–252
Goodpaster BH, Park SW, Harris TB et al (2006) The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci 61:1059–1064
Delmonico MJ, Harris TB, Visser M et al (2009) Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr 90:1579–1585
Visser M, Goodpaster BH, Kritchevsky SB et al (2005) Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol A Biol Sci Med Sci 60:324–333
Tosato M, Marzetti E, Cesari M et al (2017) Measurement of muscle mass in sarcopenia: from imaging to biochemical markers. Aging Clin Exp Res 29:19–27
Chen L, Nelson DR, Zhao Y et al (2013) Relationship between muscle mass and muscle strength, and the impact of comorbidities: a population-based, cross-sectional study of older adults in the United States. BMC Geriatr 13:74
Hayashida I, Tanimoto Y, Takahashi Y et al (2014) Correlation between muscle strength and muscle mass, and their association with walking speed, in community-dwelling elderly Japanese individuals. PLoS One 9:e111810
Kim KE, Jang SN, Lim S (2012) Relationship between muscle mass and physical performance: is it the same in older adults with weak muscle strength? Age Ageing 41:799–803
Woods JL, Iuliano-Burns S, King SJ et al (2011) Poor physical function in elderly women in low-level aged care is related to muscle strength rather than to measures of sarcopenia. Clin Interv Aging 6:67–76
Beaudart C, Locquet M, Reginster JY et al (2018) Quality of life in sarcopenia measured with the SarQoL®: impact of the use of different diagnosis definitions. Aging Clin Exp Res 30:307–313
Host HH, Sinacore DR, Bohnert KL et al (2007) Training-induced strength and functional adaptations after hip fracture. Phys Ther 87:292–303
Sylliaas H, Brovold T, Wyller TB et al (2012) Prolonged strength training in older patients after hip fracture: a randomised controlled trial. Age Ageing 41:206–212
Lee SY, Yoon BH, Beom J et al (2017) Effect of lower-limb progressive resistance exercise after hip fracture surgery: a systematic review and meta-analysis of randomized controlled studies. J Am Med Dir Assoc 18:1096
Fiatarone Singh MA (2014) Exercise, nutrition and managing hip fracture in older persons. Curr Opin Clin Nutr Metab Care 17:12–24
American College of Sports Medicine (2009) Position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc 41:687–708
Acknowledgement
The authors thank Mrs. Phyllis Curchack Kornspan for her editorial services.
Author information
Authors and Affiliations
Contributions
AH initiated the study, helped write the manuscript, was involved in data collection, and review of the literature. CA was involved with data collection and review of the literature. SB assisted in editing the manuscript and review of the literature. RN helped write the manuscript, review of the literature and was involved in data collection.
Corresponding author
Ethics declarations
Conflict of interest
All authors report no conflicts of interest. This work was not supported by any funding sources.
Statement of human and animal rights
This study was approved by the hospital’s Institutional Review Board (human and animals rights) #0198-18-RMC.
Informed consent
For this type of retrospective study informed consent is not necessary.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hershkovitz, A., Yichayaou, B., Ronen, A. et al. The association between hand grip strength and rehabilitation outcome in post-acute hip fractured patients. Aging Clin Exp Res 31, 1509–1516 (2019). https://doi.org/10.1007/s40520-019-01200-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01200-y