Abstract
Background
Although previous studies have described a positive correlation between physical activity and 25-hydroxyvitamin D concentrations (25(OH)D), there have been inconsistent results in regard to the frequency or intensity of physical activity needed to achieve adequate 25(OH)D status.
Aims
To examine the relationship between self-reported leisure-time physical activity and 25(OH)D3 and 25(OHD) concentrations among US adults aged 60 years and older.
Methods
The present analysis was based on data from participants in the National Health and Nutrition Examination Survey 2007–2012. Moderate or vigorous leisure-time physical activity was calculated by min/week or metabolic equivalent task scores-minutes/week and defined according to the 2008 Physical Activity Guidelines for Americans. General linear models adjusted for confounders were created to compare mean 25(OH)D and 25(OH)3 concentrations across physical activity status.
Results
A total of 4764 adults with a mean age of 69.7 years comprised the study sample. Overall, 33.3% men and 23.1% women were defined as physically active and participants’ mean 25(OH)D and 25(OH)D3 concentration was 75.0 and 68.8 nmol/L, respectively. Older adults physically active had 8.1 and 7.1 nmol/L higher 25(OH)D and 25(OH)3 levels than those physically inactive, respectively. Moreover, higher 25(OH)D3 and 25(OH)D concentrations were consistently seen during the summer and autumn months. In contrast, sedentary older adults had on average 25(OH)D levels < 75 nmol/L irrespective of the 6-month study period examined.
Conclusions
Leisure-time physical activity appears to be an effective manner of maintaining adequate vitamin D concentrations later in life. Therefore, promoting physical activity in older adults should be a national public health priority.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The main source of vitamin D is the endogenous production of 25-hydroxyvitamin D3 (25(OH)D3) in the skin from 7-dehydrocholesterol upon exposure to sunlight [1]. In general, older adults are at increased risk of developing vitamin D deficiency as result of inadequate dietary vitamin D intake and decreased outdoor activities [2]. Moreover, aging reduces the concentration of 7-dehydrocholesterol in the epidermis and the total production of previtamin D3 after exposure to solar ultraviolet B radiation [3].
Numerous studies have described that physical activity positively correlates with 25-hydroxyvitamin D (25(OD)D) concentrations [4,5,6,7,8,9,10,11,12]. However, there have been inconsistent results in regard to the frequency or intensity of leisure-time physical activity needed to achieve adequate 25(OH)D status [4, 5, 8, 10,11,12, 19]. Moreover, there is paucity of data about the effect of physical activity on 25(OH)D3 concentrations, particularly among older adults. Previously, Scragg et al. among participants in the National Health and Nutrition Examination Survey (NHANES) during 1988–1994 demonstrated that the mean 25(OH)D concentration difference between those who engaged in outdoor physical activities compared with those physically inactive was similar for subjects aged 20–39 and 60 years and older suggesting that US older adults who participate in daily outdoor physical activity may potentially prevent the age-related decline in vitamin D status [11]. Since that latter study, the 2008 Physical Activity Guidelines for Americans were issued by the Federal government to inform policy makers, physical educators, health providers, and the public on the amount, types, and intensity of physical activity needed to achieve many health benefits for Americans across the life span [13]. In this context, the present study aimed to examine the association between leisure-time physical activity status and 25(OH)D3 and 25(OH)D concentrations in a nationally representative sample of US older adults.
Materials and methods
The NHANES is a biannual cross-sectional study conducted by National Center for Health Statistics of the Centers for Disease Control and Prevention. The purpose of the NHANES is to collect data about the health, nutritional status, and health behaviors of the noninstitutionalized civilian resident population of the United States (US). The NHANES data were obtained using a complex, multistage probability sampling design to select a sample representative of the US civilian noninstitutionalized household population [14]. For this analysis, the NHANES data for subjects aged 60 years and older for the cycles 2007–2012 (n = 6018) were selected. Those participants who were only interviewed (n = 281) and had missing data on physical activity (n = 2), BMI (n = 106), dietary vitamin D intake (n = 286), and 25(OH)D concentrations (n = 577) were excluded, leaving a total sample size of 4764 participants. In general, participants with missing data were more likely to be women, non-hispanic white, had less than high school education, were physically inactive, self-reported fair to poor health.
Demographic characteristics of participants
All participants who completed a household interview record were included in the demographics file. The 6-month time period when the examination was performed (November 1st through April 30th and May 1st through October 31st), age, gender, race/ethnicity (Mexican American, other Hispanic, non-Hispanic white, non-Hispanic black, and other race) education (< high school, high school/GED equivalent, some college or AA degree, college graduate or above), and the ratio of family income to poverty threshold as a measure of socioeconomic status were reported. In the mobile examination center, the body mass index (BMI) was calculated as body weight (kg) divided by height (m2) and subjects were classified as underweight or normal weight (< 25.0 kg/m2), overweight (25.0–29.9 kg/m2), or obese (≥ 30 kg/m2). Participants also reported their smoking status and were classified as current, former, and never smokers. Moreover, self-reported general health condition was grouped as good to excellent or fair to poor.
Leisure-time aerobic physical activity status
The Physical Activity Questionnaire is based on the Global Physical Activity Questionnaire (GPAQ). Participants were considered to perform vigorous LTPA if they responded affirmatively to the question “Do you do any sports, fitness, or recreational activities that cause large increases in breathing or heart rate like running or basketball for at least 10 min continuously?”. Likewise, subjects were considered to engage in moderate recreational activities if they affirmatively responded to the question “Do you do any moderate-intensity sports, fitness, or recreational activities that cause a small increase in breathing or heart rate such as brisk walking, bicycling, swimming, or golf for at least 10 min continuously?”. The reported number of days and time in minutes spent performing vigorous or moderate leisure-time physical activity in the previous week were calculated. Based on the 2008 Physical Activity Guidelines for Americans, respondents who engaged in ≥ 150 min/week of moderate-intensity aerobic activity, ≥ 75 min/week of vigorous-intensity aerobic activity, or an equivalent combination of moderate-intensity and vigorous-intensity physical activity (1 min of vigorous-intensity physical activity is equivalent to 2 min of moderate intensity physical activity) totaling at least 150 min/week were defined as meeting the guidelines [13]. For the present analysis, three levels of physical activity were created: (1) participants who engaged in ≥ 150 min/week of moderate activity, or ≥ 75 min/week of vigorous activity, or ≥ 150 min/week of an equivalent combination were defined as physically active; (2) insufficiently active were considered those who reported some physical activity, but not enough to meet the active definition (> 0 to < 150 min/week); inactive if they reported no physical activity [15]. To quantify the energy expenditure of physical activity, metabolic equivalent task (MET) scores based on the NHANES recommendations for vigorous (8.0 MET) and moderate (4.0 MET) leisure-time physical activity were used to calculate MET-minutes per week (MET-min/week). As previously described, participants were classified as inactive (0 MET-min/week), insufficiently active (< 750 MET-min/week), and sufficiently active (≥ 750 MET-min/week) [16].
Total daily vitamin D intake
The NHANES dietary intake data were used to estimate the types and amounts of foods and beverages consumed during the 24-h period prior to the interview, and to estimate intakes of energy, nutrients, and other food components from those foods and beverages. Since 2007–2008, vitamin D has been added to the list of nutrients. The vitamin D values in this dataset reflect the sum of ergocalciferol and cholecalciferol content of foods reported by survey participants. The 24-h dietary supplement interview was collected following the 24-h dietary recall. All NHANES examinees responding to the dietary recall interview were eligible for the dietary supplement and antacid use questions. Information was obtained on all vitamins, minerals, herbals and other dietary supplements that were consumed during a 24-h time period, including the name and the amount of dietary supplement taken. Since 2007–2008, vitamin D supplements (ergocalciferol and cholecalciferol) were reported to estimate participants’ consumption of vitamin D supplements during the 24-h period. For the present analysis, vitamin D intake from the dietary and supplement component was combined to estimate the total daily dietary intake of vitamin D [17].
25(OH)D and 25(OH)3 concentrations
The CDC standardized liquid chromatography-tandem mass spectrometry (LC–MS/MS) method was used for measurement of 25(OH)D for NHANES 2007–2010, which allows laboratories and surveys to compare 25(OH)D measurements. The CDC decided to develop a LC–MS/MS method traceable to the NIST-reference materials for NHANES, and used this method starting with NHANES 2007–2008 to measure 25(OH)D3, 25(OH)D2, and the C3 epimer of 25(OH)D3. For the CDC LC–MS/MS method, total 25(OH)D (in SI units of nmol/L) was defined as the sum of 25(OH)D3 and 25(OH)D2 and excluded the C3 epimer of 25(OH)D3. However, due to rounding, the sum of 25(OH)D3 and 25(OH)D2 will not necessarily be equal to the 25(OH)D. The CDC recommends using the total 25(OH)D in SI units (nmol/L) measured directly by LC–MS/MS and converting this quantity to conventional units (1 nmol/L = 0.4066 ng/mL), if needed. This method has better analytical specificity and sensitivity compared to immunoassay methods, and fixed analytical goals for imprecision (≤ 10%) and bias (≤ 5%) [18].
Statistical analysis
The descriptive characteristic of the study population was reported as proportions and mean values with their respective standard errors. The Chi-squared and ANOVA tests for categorical and continues variables were used to compare demographic and behavioral characteristics of the participants across physical activity status (inactive, insufficiently active, and sufficiently active), respectively. General linear models were created to examine the associations between physical activity status and mean 25(OH)D and 25(OH)D3 concentrations. The following potential confounders were included in the model: 6-month study period, age, gender, race/ethnicity, education, ratio of family income to poverty threshold, BMI, smoking status, self-reported health, and total daily vitamin D intake. Similarly, the association between physical activity status and vitamin D concentrations was examined according to the 6-month study period, as a surrogate for seasons (November 1st through April 30th and May 1st through October 31st), race/ethnicity, and BMI categories. Statistical analyses were performed using SPSS Complex Sample software, V.17 (SPSS Inc, Chicago, IL, USA) to incorporate constructed weights for the combined survey cycles and obtain unbiased, national estimates representative of the US population [19].
Results
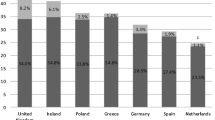
A total of 4764 participants with a mean age of 69.7 (SE 0.1) comprised the study sample, representing an estimated 46 million older adults in the US during the study period. Table 1 shows the demographic characteristics of the participants stratified by physical activity status. Overall, 33.3% men and 23.1% women aged 60 years and older were defined as physically active. Overall, the mean 25(OH)D concentration among older adults was 75.0 (0.93) nmol/L. However, higher 25(OH)D concentrations were found in women 76.9 (1.2) nmol/L than those in men 72.7 (0.98). In general, older non-Hispanic white, college graduate or above, higher socioeconomic status, and a self-reported good to excellent health were characteristics of the participants associated with a higher prevalence of physical activity. In contrast, physical activity status did not differ by the 6-month study period. Likewise, daily vitamin D intake was not significantly associated with physical activity. As shown in Fig. 1, a strong dose–response relationship was seen between minutes of physical activity per week and 25(OH)D3 and 25(OH)D concentrations. For instance, older adults who engaged in 250 min or more of recreational physical activity had 14.2 and 14.0 nmol/L higher mean concentration of 25(OH) and 25(OH)D3 compared with their physically inactive counterparts, respectively. Moreover, even participants who participated between 50 and 99 min per week of physical activity had adequate 25(OH)D concentrations.
As shown in Table 2, 25(OH)D3 concentrations were significantly higher among those physically active than those sedentary according to the 6-month study period. Notably, similar 25(OH)D3 levels were seen irrespective of the reported frequency or intensity of physical activity per week. However, 25(OH)D3 levels differed by study period among older adults physically active. Indeed, participants physically active between May 1st through October 31st had on average 5.4 nmol/L higher 25(OH)D3 concentrations than their counterparts examined between November 1st through April 30th. Similarly, 25(OH)D concentrations were significantly higher among older adults physically active compared with those inactive, irrespective of the 6-month study period. Notably, the highest 25(OH)D concentration was seen among older adults who reported physical activity between May 1st through October 31st. In contrast, sedentary older adults had consistently 25(OH)D concentrations < 75 nmol/L throughout the year.
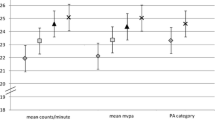
In the fully adjusted model including the 6-month study periods, 25(OH)3 and 25(OH)D concentrations among physically active participants were on average 7.1 and 8.1 nmol/L higher than those physically inactive, respectively. Similarly, older adults defined as physically active according to MET-min/week had increased 25(OH)D3 and 25(OH)D concentrations compared with their physically inactive counterparts. Notably, 25(OH)D3 concentrations among physically active participants accounted for 92% of 25(OH)D levels.
As shown in Fig. 2, higher adjusted mean 25(OH)D3 concentrations were seen among non-Hispanic whites as compared with other racial/ethnic groups. Of interest, non-Hispanic blacks had considerably lower 25(OH)D3 concentrations regardless their physical activity status. Notably, physically inactive non-Hispanic blacks had 25(OH)3 concentrations < 50 nmol/L. As shown in Fig. 3, obese older adults had also lower 25(OH)3 concentrations compared with their normal weight counterparts. This difference was most evident among participants defined as physically active. However, obese older adults were able to synthesize 25(OH)D3 while performing physical activity. For instance, a mean absolute 25(OH)D3 concentration difference of 9.2 nmol/L was seen between obese older adults physically active compared with their physically inactive counterparts.
Discussion
In a nationally representative sample of US older adults, physical activity was significantly associated with higher 25(OHD)3 and 25(OH)D concentrations. This strong relationship persisted irrespective of the frequency or intensity of leisure-time physical activity definition used to meet the 2008 Physical Activity Guidelines for Americans. Moreover, a strong linear dose–response relationship between minutes of physical activity and 25(OH)D3 concentrations was observed during the study period, suggesting that older adults are able to synthesize adequate 25(OH)D3 concentrations as a result of increasing sunlight exposure while participating in outdoor activity. For instance, among older US adults examined during the 6-month period between May 1st through October 31st, 25(OH)D3 concentrations account for 91.7%, 86.8%, and 92.4% of the total 25(OH)D concentrations in those physically inactive, insufficiently, and sufficiently active participants, respectively. Although the present study does not specifically assess participants’ sun exposure, similar 25(OH)D3 concentrations according to physical activity status may be explained by greater sun exposure while performing other recreational outdoor activities, particularly in participants with sedentary lifestyle. However, the present findings are in agreement with published data suggesting that between 80 and 90% of vitamin D is obtained from endogenous synthesis of 25(OH)D3 [20].
Previous studies have concluded that the relationship between physical activity and circulating vitamin D concentrations mostly reflect the effect of sunlight exposure during outdoor physical activity [8, 11, 12]. Of note, a recent cross-sectional study among adults aged 60 years or older from Giessen, Germany (50°35′N) reported that habitual dietary vitamin D and calcium intakes have no independent effects on 25(OH)D3 in elderly subjects without vitamin D deficiency [21]. Although the present survey does not distinguish between participants indoor or outdoor physical activity, the increased 25(OH)D3 concentration seen among older adults physically active compared with those sedentary indicate that sunlight exposure is a major determinant of adequate 25(OH)3 concentrations and 25(OH)D status in older US adults. Of interest, Wanner et al. described that among participants aged 18 years and older in the NHANES 2003–2006, stronger associations between indoor physical activity and 25(OH)D levels even after controlling for potential confounders, which contrast with the present study findings [22]. Possible explanations for these contradictory results may be related to differences in the age distribution of participants, comorbidities, vitamin D intake assessment, and misclassification bias. Previous research has suggested that physical activity may directly affect vitamin D concentrations through changes in hormone levels or changes in body mass index [10]. For instance, Bell et al. reported higher 25(OH)D concentrations in young adult white males who engaged regularly in muscle-building exercise for a year compared with controls [23]. In rat models, exercise also promoted a positive calcium and phosphorus balance and increased the skeletal mass, largely as a result of an increase in 1,25-dihydroxyvitamin D and an enhancement of the intestinal calcium absorption [24].
Notably, physically active older adults who completed a MEC examination from May 1st through October 31st had on average 11.7% higher 25(OH)D3 concentrations than their physically inactive counterparts. Similarly, 12.2% higher 25(OH)3 concentrations were found among physically active subjects examined between November 1st through April 30th. Moreover, 25(OH)3 concentrations were 7.6% higher among physically active participants examined during summer and autumn months than those during winter and spring months. This association remained unchanged even if leisure-time physical activity was defined by MET-min/week. Although the 6-month period examination used in the continuous NHANES does not precisely define seasons, the present findings are consistent with results from previous studies which have demonstrated that season significantly modify the associations between physical activity and 25(OH)D concentrations [4, 8, 10, 11]. For instance, among older adults in Southern Germany (latitude: 48.4°N), objectively measured walking was positively correlated with 25(OH)D levels in all seasons, but not in summer. This unexpected finding was explained by increasing sunlight exposure among participants through other activities such as sitting or lying during summer months [25].
Population-based studies have consistently demonstrated that sunlight exposure, season, latitude, and physical activity are important determinants of adequate 25(OH)D status [9, 26, 27]. For instance, van Dam et al. reported that among adults aged 60–87 years in the Netherlands, more time spent on outdoor physical activity was associated with adequate vitamin D status. In fact, 25(OH)D concentrations increased by 1.8 nmol/L for each hour of outdoor activity [9]. Likewise, among older survivors of the Framingham Heart Study, sunlight exposure variables such as season, residing in sunny states for 3 or more months during the year, and stay outdoors most of the day were major determinant of 25(OH)D concentrations [27]. Reid et al. also demonstrated that sunlight exposure for at least 30 min daily leads to a substantial increase in 25(OH)D levels in elderly subjects [28]. As expected, obese older adults had significantly lower 25(OH)3 concentrations compared with their normal weight counterparts. Of relevance, among obese participants, those defined as physically active were able to synthesize higher 25(OH)D3 concentrations than those physically inactive. This inverse association between low vitamin D status and obesity has been explained by decreased bioavailability of vitamin D as a result of sequestration of vitamin D by the adipose tissue, dilution of vitamin D in the large fat mass of obese people, and reduced sun exposure [29]. Likewise, regardless of their physical activity status, non-Hispanic blacks had significantly lower 25(OH)D3 concentrations than non-Hispanic whites. Notably, the lowest 25(OH)D3 concentrations by race/ethnicity was seen among non-Hispanic blacks with sedentary lifestyle. Scragg et al. previously reported similar racial/ethnic 25(OH)D concentration differences according to the frequency of outdoor activity among participants in the NHANES during 1988–1994 [4]. Since the capacity to synthesize 25(OH)D3 from sun exposure, is inversely related to the degree of skin pigmentation, non-Hispanic blacks, particularly those with sedentary lifestyle should be offered vitamin D supplements [30]. Despite the significant relationship between physical activity and 25(OH)D concentrations found in the present and previous studies, only 33% of men and 23% of women aged 60 years and older met the 2008 Physical Activity Guidelines for Americans, which is consistent with recent national estimates among older adults [31].
The present study has several limitations. First, because of the NHANES survey cross-sectional design, the present results do not infer causation. Second, participants self-reported their physical activity, which may have been subject to recall bias and the individual type of physical activity was not assessed in the NHANES during 2007–2012. Third, subject’s sunlight exposure or use of sunscreen was not evaluated in the present study. Finally, the effect of latitude on participants’ vitamin D concentration was unknown. Despite these limitations, the present findings indicate that leisure-time physical activity was positively and significantly correlated with 25(OH)D3 and 25(OH)D concentrations among older adults in the US.
In conclusion, physical activity appears to be an effective manner of maintaining adequate vitamin D concentrations later in life. However, a small proportion of US older adults participate regularly in recreational physical activity. Therefore, promoting physical activity should be a national public health priority.
References
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281
Mosekilde L (2005) Vitamin D and the elderly. Clin Endocrinol (Oxf) 62:265–281
MacLaughlin J, Holick MF (1985) Aging decreases the capacity of human skin to produce vitamin D3. J Clin Investig 76:1536–1538
Scragg R, Holdaway I, Jackson R et al (1992) Plasma 25-hydroxyvitamin D3 and its relation to physical activity and other heart disease risk factors in the general population. Ann Epidemiol 2:697–703
Jungert A, Neuhäuser-Berthold M (2015) Sex-specific determinants of serum 25-hydroxyvitamin D3 concentrations in an elderly German cohort: a cross-sectional study. Nutr Metab (Lond) 12:2. https://doi.org/10.1186/1743-7075-12-2
Holick MF (2004) Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr 80:1678S–1688S
Brock K, Cant R, Clemson L et al (2007) Effects of diet and exercise on plasma vitamin D (25(OH)D) levels in Vietnamese immigrant elderly in Sydney, Australia. J Steroid Biochem Mol Biol 103:786–792
Kluczynski MA, Lamonte MJ, Mares JA et al (2011) Duration of physical activity and serum 25-hydroxyvitamin D status of postmenopausal women. Ann Epidemiol 21:440–449
Van Dam RM, Snijder MB, Dekker JM et al (2007) Potentially modifiable determinants of vitamin D status in an older population in the Netherlands: the Hoorn Study. Am J Clin Nutr 85:755–761
van den Heuvel EG, van Schoor N, de Jongh RT et al (2013) Cross-sectional study on different characteristics of physical activity as determinants of vitamin D status; inadequate in half of the population. Eur J Clin Nutr 67:360–365
Scragg R, Camargo CA Jr (2008) Frequency of leisure-time physical activity and serum 25-hydroxyvitamin D levels in the US population: results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol 168:577–586
De Rui M, Toffanello ED, Veronese N et al (2014) Vitamin D deficiency and leisure time activities in the elderly: are all pastimes the same? PLoS One 9:e94805. https://doi.org/10.1371/journal
U.S. Department of Health and Human Services (2008) Physical Activity Guidelines for Americans. ODPHP publication no. U0036. 2008:1–61. http://www.health.gov/paguidelines/. Accessed May 2018
https://www.cdc.gov/nchs/data/series/sr01_056.pdf. Accessed May 2018
Zhao G, Li C, Ford ES et al (2014) Leisure-time aerobic physical activity, muscle-strengthening activity and mortality risks among US adults: the NHANES linked mortality study. Br J Sports Med 48:244–249
Yang L, Toriola AT (2017) Leisure-time physical activity and circulating 25-hydroxyvitamin D levels in cancer survivors: a cross-sectional analysis using data from the US National Health and Nutrition Examination Survey. BMJ Open 7:e016064. https://doi.org/10.1136/bmjopen-2017-016064
https://wwwn.cdc.gov/Nchs/Nhanes/2007-2008/DS1IDS_E.htm. Accessed August 2018
https://wwwn.cdc.gov/nchs/nhanes/vitamind/analyticalnote.aspx?h=/Nchs/Nhanes/2007-2008/VID_E.htm&t=VID_E%20Doc. Accessed April 2018
https://www.cdc.gov/nchs/tutorials/NHANES/SurveyDesign/Weighting/intro.htm. Accessed May 2018
Macdonald H, Mavroeidi A, Fraser W et al (2011) Sunlight and dietary contributions to the seasonal vitamin D status of cohorts of healthy postmenopausal women living at northerly latitudes: a major cause for concern? Osteoporos Int 22:2461–2472
Jungert A, Neuhäuser-Berthold M (2013) Dietary vitamin D intake is not associated with 25-hydroxyvitamin D3 or parathyroid hormone in elderly subjects, whereas the calcium-to-phosphate ratio affects parathyroid hormone. Nutr Res 33:661–667
Wanner M, Richard A, Martin B et al (2015) Associations between objective and self-reported physical activity and vitamin D serum levels in the US population. Cancer Causes Control 26:881–891
Bell NH, Godsen RN, Henry DP et al (1988) The effects of muscle-building exercise on vitamin D and mineral metabolism. J Bone Miner Res 3:369–373
Yeh JK, Aloia JF, Yasumura S (1989) Effect of physical activity on calcium and phosphorus metabolism in the rat. Am J Physiol 256:E1–E6
Klenk J, Rapp K, Denkinger M et al (2015) Objectively measured physical activity and vitamin D status in older people from Germany. J Epidemiol Community Health 69:388–392
Palaniswamy S, Hyppönen E, Williams DM et al (2017) Potential determinants of vitamin D in Finnish adults: a cross-sectional study from the Northern Finland birth cohort 1966. BMJ Open 7:e013161
Jacques PF, Felson DT, Tucker KL et al (1997) Plasma 25-hydroxyvitamin D and its determinants in an elderly population sample. Am J Clin Nutr 66:929–936
Reid IR, Gallagher DJ, Bosworth J (1986) Prophylaxis against vitamin D deficiency in the elderly by regular sunlight exposure. Age Ageing 15:35–40
Vitezova A, Muka T, Zillikens MC et al (2017) Vitamin D and body composition in the elderly. Clin Nutr 36:585–592
Clemens TL, Adams JS, Henderson SL et al (1982) Increased skin pigment reduces the capacity of skin to synthesise vitamin D3. Lancet 1:74–76
QuickStats (2016) Percentage of adults aged ≥ 65 years meeting 2008 federal guidelines for leisure-time aerobic and muscle-strengthening activities, by age and type of activity—United States, 2000–2002 and 2013–2015. MMWR Morb Mortal Wkly Rep 65:1019
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author reports no conflict of interest while conducting the present study.
Statement of human and animal rights
The National Center for Health Statistics Research Ethics Review Board approved the study protocol (protocol # 2005-06 and # 2011-17).
Informed consent
During the informed consent process, survey participants were assured that data collected will not be disclosed or released to others without the consent of the individual in accordance with section 308(d) of the Public Health Service Act (42 U.S.C.242m).
Rights and permissions
About this article
Cite this article
Orces, C.H. Association between leisure-time aerobic physical activity and vitamin D concentrations among US older adults: the NHANES 2007–2012. Aging Clin Exp Res 31, 685–693 (2019). https://doi.org/10.1007/s40520-018-1031-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-018-1031-9