Abstract
Background
Knee osteoarthritis (OA) and fear of falling (FoF) are important factors contributing to trunk oscillation during walking. It is of a clinical importance to clarify the association of FoF with trunk oscillation during walking in older adults with knee OA (knee OA adults).
Aim
The purpose of this study was to investigate the association of FoF with trunk oscillation during walking in knee OA adults.
Methods
Forty-one patients who met the criteria participated in the study and were classified into two groups based on their answer to a question on FoF. An accelerometer was attached at the level of the third lumbar vertebra (L3) and the seventh cervical vertebra (C7), and the accelerations at L3 and C7 were measured during a 10-m gait test. Using these data, the acceleration-derived gait indices, such as stride time variability (STV), root mean square (RMS), and autocorrelation at the trunk in the anteroposterior (AP) and mediolateral (ML) directions, were computed.
Results
FoF was associated with a higher STV value and a smaller RMS value in the ML direction at L3.
Discussion
The decreased trunk oscillation in the ML direction in knee OA adults with FoF may reflect a positive, compensatory adaptation for trunk control.
Conclusion
Knee OA adults with FoF decreased trunk oscillation during walking than those without FoF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fear of falling (FoF) is defined as a lack of self-confidence in performing normal activities without falling [1]. FoF is common in older adults, with an estimated prevalence rate of > 20%, and is a major risk factor for falling in older adults [2]. Moreover, it is a clinical factor that contributes to gait changes in older adults. Previous studies have reported that gait changes due to FoF include slower gait speed, shorter stride length, increased step width, and prolonged need for double limb support [2,3,4] as well as lower trunk fluctuations [5,6,7], thereby leading to an increased risk of falling among older adults [8, 9]. Lower trunk oscillation was greater among older adults with FoF than in those without FoF [5,6,7]. Thus, investigating the association of FoF with trunk oscillation during walking is of clinical importance.
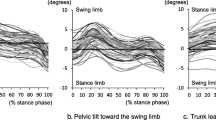
Knee osteoarthritis (OA) is a common orthopedic disease among older adults. Older adults with knee OA (knee OA adults) exhibit typical gait pattern changes, such as slower gait speed, shorter step length, wider step width, and higher stride time variability [10,11,12,13]; trunk motion changes increased lateral trunk sway; and fluctuating trunk oscillation during walking [13, 14]. Importantly, knee OA adults are more prone to develop FoF and falling [15,16,17,18] than normal adults. These reports indicate that some knee OA adults with FoF might experience difficulties during walking because of their efforts to control trunk oscillation. However, the association of FoF with trunk oscillation during walking is poorly understood.
In the present study, we measured the upper and lower trunk oscillation during walking in knee OA adults using accelerometers. We then computed the acceleration-derived gait indices, such as stride time variability (STV), root mean square (RMS), and autocorrelation (AC), and investigated the association of FoF with each acceleration-derived gait index. Our hypothesis was that knee OA adults with FoF have increased trunk oscillation during walking.
Methods
Participants
Forty-six women with knee OA who were scheduled to undergo unilateral total knee arthroplasty at an orthopedic clinic were recruited. These participants were categorized as grade 3 or 4 on the basis of the Kellgren and Lawrence radiographic grading system (K/L grade). The inclusion criteria were as follows: (1) medial OA and (2) no symptoms in the hip, ankle, or contralateral knee joint during walking. The exclusion criteria were as follows: (1) neurological conditions such as Parkinson’s disease or stroke, (2) walking with the use of a cane or other gait-assisting tools, and (3) rheumatoid arthritis. Forty-one women who met the criteria participated in this study and were classified into two groups on the basis of their answer to the following question on FoF: “Are you afraid of falling? Yes/No” [19, 20]. Participants who responded with “Yes” were assigned to the knee OA + FoF group, and those who responded with “No” were assigned to the knee OA group. This format is advantageous in that it is straightforward and helps easily generate prevalence estimates [19, 20]. The ethics committee of the Anshin Hospital approved all procedures performed in this study before testing, and all participants provided a written informed consent in accordance with the Declaration of Helsinki before participating.
Gait measurement
Accelerometer
Triaxial accelerometers (MVP-RF8-HC; Microstone Co., Nagano, Japan) were attached at the level of the third lumbar vertebra (L3) and the seventh cervical vertebra (C7) using a Velcro belt and a surgical tape, respectively (Fig. 1). L3 represents the lower trunk because its location was reported to be approximate to the center of the mass [21], whereas C7 represents the upper trunk because its location was approximately halfway between the head and the trunk [22]. The X and Y axis accelerometers were attached along the anteroposterior (AP) and mediolateral (ML) directions, in the traveling direction, respectively. Prior to the measurement, the accelerometers were calibrated against gravity on a flat floor to correct any potential effect of inclination. All signals were sampled at 200 Hz and synchronously and wirelessly transferred to a personal computer via a Bluetooth personal area network.
Gait measurement
Gait measurements were conducted twice for each participant. All participants were instructed to walk at their preferred speed along a 16-m smooth, horizontal walkway. A 10-m section of the walkway was marked off by two lines positioned 3 m from each end to allow space and time for acceleration and deceleration. The time taken to complete the middle 10-m distance was recorded to the nearest hundredth of a second using a stopwatch.
Signal processing
Signal processing was performed using MATLAB (The Math-Works Co., Release 2008, Cybernet Systems Co., Ltd., Tokyo, Japan). Prior to the analysis, all acceleration data were high- and low-pass filtered with a cutoff frequency of 1 Hz and 20 Hz, respectively. The timing of heel contacts was identified by sharp peaks of acceleration at the lower trunk [23]. Stride time was defined by the time between one heel contact and the next heel contact. Using this method, we obtained the data of stride time in several steps during 10-m walking. Subsequently, STV was calculated by determining the standard deviation (SD) and mean of each patient’s stride time using the following formula: [STV = (SD/mean) × 100%] [24]. A smaller STV value shows better stability during gait [23]. RMS of acceleration signals was calculated at L3 and C7 in the AP and ML directions. An unbiased AC is an estimate value of the regularity of a time series by cross-correlation with itself at a given time shift, independent of the amount of data managed [25]. A perfect replication of the gait cycle signal between neighboring strides will return an AC of 1, whereas no association will give a coefficient of 0. The results of the two trials were averaged to obtain the gait speed, STV, RMS, and AC of stride.
Measurements of physical functions
Knee extensor strength
The maximal isometric strength of knee extensors was measured using a hand-held dynamometer (µTas F1; ANIMA, Chofu, Japan). The details of the measurements are previously described [26]. The peak torque (Nm) was estimated as the product of force and lever-arm length. Two attempts at maximal contraction were performed, and the greater value was recorded and normalized according to the body weight (Nm/kg).
Pain
A numeric rating scale (NRS) is a valid and reliable instrument used in clinical practice because of its good sensitivity [27]. NRS was used to quantify knee pain during the gait measurement. Immediately after the gait measurement, patients were asked to verbally rate the pain on a scale ranging from 0 to 10, with 0 representing no pain and 10 representing the worst pain imaginable.
Statistical analysis
Continuous variables were expressed as mean ± SD, and ordinal variables were expressed as number (%). Normal distributions of all continuous data were confirmed using the Shapiro–Wilk test. Participants’ characteristics and gait parameters were compared between the knee OA + FoF and knee OA groups. Parametric and nonparametric values were compared using the unpaired t test and the Mann–Whitney U test, respectively, and nominal values were compared using the Chi square test. For the gait parameters that showed a significant difference in the bivariate analyses, multiple linear regression analyses were performed to investigate the association of FoF with gait parameters. Age, gait speed, and STV were considered potential confounders. The statistical significance level was set at p < 0.05 for all analyses. All analyses were performed using SPSS for Windows 21.0.0 version (IBM, Tokyo, Japan).
Results
Twenty (49%) participants were classified as the knee OA group and 21 (51%) participants were classified as the knee OA + FoF group. In the demographic data shown in Table 1, no significant differences in participants’ characteristics, physical functions, and pain were observed between the two groups.
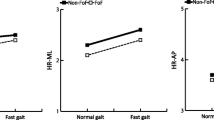
Results for general gait parameters and acceleration-derived gait indices are shown in Table 2. The STV value was significantly higher (p = 0.03) and RMS at L3 in the ML direction was significantly smaller (p = 0.01) in the knee OA + FoF group than in the knee OA group. Results for multilinear regression models are shown in Table 3. STV and RMS at L3 in the ML direction were associated with FoF, independent of age and gait speed in Model 2(STV, standard β = 0.33, p = 0.03; RMS at L3 in the ML direction, standard β = − 0.32, p = 0.02). RMS at L3 in the ML direction was not associated with FoF, independent of age, gait speed, and STV in Model 3(standard β = − 0.26, p = 0.07).
Discussion
FoF is a contributing factor to fluctuate trunk oscillation during walking. Knee OA adults exhibit a typical lateral sway gait disorder, and some of them suffer from FoF. It is of a clinical importance to clarify the association of FoF with trunk oscillation during walking in knee OA adults. In the present study, we investigated the association of FoF with acceleration-derived gait indices, such as STV, RMS, and stride AC at the upper and lower trunks, during walking in knee OA adults. The primary results showed that FoF was significantly associated with a higher STV value and a smaller RMS value at L3 in the ML direction. The strength of our study was that all participants were knee OA adults. To the best of our knowledge, this study was the first to investigate an association of FoF with trunk oscillation during walking in knee OA adults.
Previous studies have reported that older adults with FoF exhibit higher STV value than those without FoF [28]. The present study indicates that FoF was associated with step fluctuations in knee OA adults, supporting the result of the previous research. However, interestingly, lower trunk oscillation in the ML direction was significantly decreased in the knee OA + FoF group than in the knee OA group, which suggests that FoF plays a potential role in decreasing trunk oscillation and does not support the hypothesis that knee OA adults with FoF have increased trunk oscillation during walking. A potential explanation for these results is that knee OA adults exhibit a decline in balance ability and have a higher risk of falling [29, 30]. Donoghue et al. have reported that FoF-associated gait adaptations may be partly attributed to stabilizing strategies [4]. Therefore, the development of FoF may play a compensatory role in trunk control in knee OA-derived decline in balance ability. The decreased trunk oscillation in the ML direction in knee OA adults with FoF may reflect a positive, compensatory adaptation for trunk control. Additionally, based on the results of multi regression analysis, STV affected RMS at L3 in the ML direction, which indicates that an increased STV associated with FoF may lead to decreased RMS at L3 in the ML direction.
Another important finding was that RMS at L3 in the ML direction was significantly decreased in the knee OA + FoF group, whereas RMS at C7 in the ML direction was not significantly decreased between the two groups. These results suggest that upper trunk oscillation in the ML direction was not affected by FoF. It was considered the influence of the trunk motion in the ML direction, which is a typical gait disorder in knee OA adults [13, 14]. In this population, the lateral trunk motion was increased to reduce knee pain when varus moment became larger during walking [28]. Our participants also had severe knee OA classified as K/L grade 3 or 4. Considering that RMS at C7 in the ML direction did not differ between the two groups, the influence of knee pain-derived lateral trunk motion during walking was higher than that of FoF at C7 in the ML direction.
Several limitations have been identified in this study. First, the limitations of our study designs included cross-sectional design, selection bias, and convenience sampling. During convenience sampling, we excluded patients requiring cane or other gait-assessing tools that affect trunk oscillation during walking. Additionally, we did not discuss the causal association between FoF and trunk oscillation during walking. Therefore, future studies should include a larger sample size, a wide range of patients, and a longitudinal design. Second, FoF was assessed using a simple question. Although this assessment tool has been validated [19], other more complex assessment tools would provide more information regarding the degree of FoF or sub-analyses [31]. Further studies should be conducted based on complex questionnaires such as the FES-I or ABC. In addition, FoF was different among cultures and genders. The prevalence of falling in our study was relatively lower than that in previous studies [32, 33]. Therefore, our results may not be generalizable to knee OA adults as a whole group. Finally, other potential confounders such as balance ability and mental status were not measured. Previous studies reported that gait variability such as STV and RMS were correlated with balance ability and mental status [34, 35]. Further studies should be conducted on a wide range of patients to determine whether our results can be generalized and should be based on the guidelines by Zilkstra et al., who have reported on interventions to reduce fear of falling and on the association between activity restriction and fear of falling [36].
Conclusion
This study explored the association of FoF with trunk oscillation during walking in knee OA adults. Our findings suggest that knee OA adults with FoF showed smaller lower trunk oscillation in the ML direction during walking than those without FoF. The results of this study will be helpful in evaluating gait patterns for preventing falls in knee OA adults.
References
Tinetti ME, Richman D, Powell L (1990) Falls efficacy as a measure of fear of falling. J Gerontol 45:239–243
Reelick MF, van Iersel MB, Kessels RP et al (2009) The influence of fear of falling on gait and balance in older people. Age Ageing 38:435–440
Chamberlin ME, Fulwider BD, Sanders SL et al (2005) Does fear of falling influence spatial and temporal gait parameters in elderly persons beyond changes associated with normal aging? J Gerontol A Biol Sci Med Sci 60:1163–1167
Donoghue OA, Cronin H, Savva GM et al (2013) Effects of fear of falling and activity restriction on normal and dual task walking in community dwelling older adults. Gait Posture 38:120–124
Sawa R, Doi T, Misu S et al (2014) The association between fear of falling and gait variability in both leg and trunk movements. Gait Posture 40:123–127
Asai T, Misu S, Sawa R et al (2017) The association between fear of falling and smoothness of lower trunk oscillation in gait varies according to gait speed in community-dwelling older adults. J Neuroeng Rehabil 14:5
Asai T, Misu S, Doi T et al (2014) Effects of dual-tasking on control of trunk movement during gait: respective effect of manual- and cognitive-task. Gait Posture 39:54–59
de Hoon EW, Allum JH, Carpenter MG et al (2003) Quantitative assessment of the stops walking while talking test in the elderly. Arch Phys Med Rehabil 84:838–842
Bautmans I, Jansen B, Van Keymolen B et al (2011) Reliability and clinical correlates of 3D-accelerometry based gait analysis outcomes according to age and fall-risk. Gait Posture 33:366–372
McGibbon CA, Krebs DE (2002) Compensatory gait mechanics in patients with unilateral knee arthritis. J Rheumatol 29:2410–2419
Messier SP, Devita P, Cowan RE et al (2005) Do older adults with knee osteoarthritis place greater loads on the knee during gait? A preliminary study. Arch Phys Med Rehabil 86:703–709
Mundermann A, Dyrby CO, Hurwitz DE et al (2004) Potential strategies to reduce medial compartment loading in patients with knee osteoarthritis of varying severity: reduced walking speed. Arthritis Rheum 50:1172–1178
Mundermann A, Asay JL, Mundermann L et al (2008) Implications of inceased medio-lateral trunk sway for ambulatory mechanics. J Biomech 41:165–170
Hunt MA, Brimingham TB, Bryant D et al (2008) Lateral trunk lean explains variation in dynamic knee joint load in patients with medial compartment knee osteoarthritis. Osteoarthr Cartil 16:591–599
Levinger P, Menz HB, Wee E et al (2011) Physiological risk factors for falls in people with knee osteoarthritis before and early after knee replacement surgery. Knee Surg Sports Traumatol Arthrosc 19:1082–1089
Tsonga T, Michalopoulou M, Kapetanakis S et al (2016) Risk factors for fear of falling in elderly patients with severe knee osteoarthritis before and one year after total knee arthroplasty. J Orthop Surg (Hong Kong) 24:302–306
Stanmore EK, Oldham J, Skelton DA et al (2013) Risk factors for falls in adults with rheumatoid arthritis: a prospective study. Arthritis Care Res (Hoboken) 65:1251–1258
Unver B, Ertekin Ö, Karatosun V (2014) Pain, fear of falling and stair climbing ability in patients with knee osteoarthritis before and after knee replacement: 6 month follow-up study. J Back Musculoskelet Rehabil 27:77–84
Maki BE, Holliday PJ, Topper AK (1991) Fear of falling and postural performance in the elderly. J Gerontol 46:123–131.15
Ayoubi F, Launay CP, Annweiler C et al (2015) Fear of falling and gait variability in older adults: a systematic review and meta-analysis. J Am Med Dir Assoc 16:14–19
Moe-Nissen R (1998) A new method for evaluating motor control in gait under real-life environmental conditions. Part 1: The instrument. Clinical Biomech 13:320–327
Kavanagh JJ, Menz HB (2008) Accelerometry: a technique for quantifying movement patterns during walking. Gait Posture 28:1–15
Zijlstra W (2004) Assessment of spatio-temporal parameters during unconstrained walking. Eur J Appl Physiol 92:39–44
Hausdorff JM, Cudkowicz ME, Firtion R et al (1998) Gait variability and basal ganglia disorders: stride-to-stride variations of gait cycle timing in Parkinson’s disease and Huntington’s disease. Mov Disord 13:428–437
Moe-Nilssen R, Helbostad JL (2004) Estimation of gait cycle characteristics by trunk accelerometry. J Biomech 37:121–126
Mizner RL, Petterson SC, Snyder-Mackler L (2005) Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J Orthop Sports Phys Ther 35:424–436
Williamson A, Hoqqart B (2005) Pain: a review of three commonly used pain rating scales. J Clin Nurs 14:798–804
Van der Esch M, Steultjens MP, Harlaar J et al (2011) Lateral trunk motion and knee pain in osteoarthritis of the knee: a cross-sectional study. BMC Musculoskelet Disord 12:141
Hinman RS, Bennell KL, Metcalf BR et al (2002) Balance impairments in individuals with symptomatic knee osteoarthritis: a comparison with matched controls using clinical tests. Rheumatology 41:1388–1394
Kim HS, Yun DH, Yoo SD et al (2011) Balance control and knee osteoarthritis severity. Ann Rehabil Med 35:701–709
Legters K (2002) Fear of falling. Phys Ther 82:264–272
Stanmore EK, Oldham J, Skelton DA et al (2013) Fall incidence and outcomes of falls in a prospective study of adults with rheumatoid arthritis. Arthritis Care Res (Hoboken) 65:737–744
Tsonga T, Michalopoulou M, Malliou P et al (2015) Analyzing the history of falls in patients with severe knee osteoarthritis. Clin Orthop Surg 7:449–456
Lord SR, Menz HB, Tiedemann A (2003) A physiological profile approach to falls risk assessment and prevention. Phys Ther 83:237–252
Sturnieks DL, Tiedemann A, Chapman K et al (2004) Physiological risk factors for falls in older people with lower limb arthritis. J Rheumatol 31:2272–2279
Zijlstra G, van Haastregt JC, van Eijk JT et al (2005) Evaluating an intervention to reduce fear of falling and associated activity restriction in elderly persons: design of a randomised controlled trial [ISRCTN43792817]. BMC Public Health 5:26
Acknowledgements
We acknowledge all subjects who participated in this study, and this study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
All participants provided a written informed consent in accordance with the Declaration of Helsinki before participating.
Rights and permissions
About this article
Cite this article
Oka, T., Asai, T., Kubo, H. et al. Association of fear of falling with acceleration-derived gait indices in older adults with knee osteoarthritis. Aging Clin Exp Res 31, 645–651 (2019). https://doi.org/10.1007/s40520-018-1022-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-018-1022-x