Abstract
Backgrounds
Imbalance in elderly is a common problem strictly related to fall.
Aims
This study investigates the possibility that a new protocol based on the focal mechanical muscle vibration may improve balance and stability in elderly.
Methods
Pre-post non-randomized clinical trial has been used. Patients referring postural disequilibrium with negative vestibular bed-side examinations have been treated with focal muscle vibration applied to quadriceps muscles and evaluated before and immediately after therapy and after 1 week and after 1 month with postural stabilometric examination and with an inertial measurement units during the time up and go test.
Results
Stabilometric analysis showed statistically significant differences in both the area (p = 0.01) and sway (p < 0.01) of the center of pressure during the close eyes tests. Moreover, the global time of the time up and go test was reduced (p < 0.05) and the rotation velocity was increased (p < 0.01).
Conclusions
The findings confirm the beneficial role of focal muscle vibration in elderly patients improve postural stability and mobility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dizziness and imbalance in older people are a growing public health concern due to the significantly higher risk of accidental falls and consequent injuries [1, 2]. Falls are the leading cause of hospital admission and accidental death in older people. The underlying cause of dizziness in the elderly is complex and multi-factorial [3, 4]. Postural stability is maintained by the integration of somatosensory, visual and vestibular inputs to the central nervous system, followed by outputs to the musculoskeletal system. Dizziness and imbalance can be caused by changes in any of the factors associated to the balance system, be they of sensory, visual, vestibular, neurologic, and muscular origin. All these components deteriorate with age [5]. Teasdale et al. [6] have demonstrated that alteration in any two of the three sensory inputs (visual, vestibular and somatosensory) had a significantly greater effect on older subjects than in younger ones, whereas alteration in a single input did not have a significant effect due to age. These results suggest that decreased inputs from the vestibular, visual and somatosensory systems in older subjects lead to a decreased capacity for compensation by the other inputs to maintain postural stability.
A wealth of literature exists underscoring the importance of proprioceptive feedback in the control of voluntary movements. Mounting evidence suggests that declines in proprioceptive function may represent a fundamental aspect of the aging process. Given the rising proportion of individuals over 65 years of age, these deficits have, therefore, spurred increased interest in the field of motor neuroscience regarding the proprioceptive abilities of older individuals, and the role of proprioceptive feedback in elderly movement [7].
Effective neurorehabilitation strategies to enhance the sensorimotor abilities of elderly individuals is the main objective in a rehabilitation approach.
Recently different studies showed the effectiveness of the repetitive muscle vibration (rMV) protocol, based on a mechanical vibratory stimulation focally applied on voluntary contracted muscles, to improve neuromuscular functionality [8, 9] and to reduce the risk of falling of elderly subjects [10].
From these assumptions, the aim of the present study was to evaluate the proprioceptive role of the focal muscle vibration in the postural control, balance and in functional activities in a group of elderly lamenting postural disequilibrium.
Methods
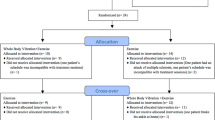
We used a pre-post non-randomized clinical trial; patients were evaluated before treatment (T0), immediately after therapy (T1) after 1 week (T2) and after 1 month (T3) from treatment. The subjects were evaluated with clinical scales and quantitative functional tests based on wearable devices for the evaluation of the movement kinematics and baropodometric systems for the evaluation of kinetics.
Research participants
Between January and October 2016, a homogeneous group of patients older than 65 years followed at the Otolaryngology Department for postural disequilibrium were enrolled in the study. Exclusion criteria were acute vestibular disease, acute orthopedic injuries, the presence of dementia, and drug therapies that could alter movement or spatial perception. At the baseline patients have been evaluated with the Mini Mental State Evaluation (MMSE), Geriatric Depression Scale (GDS) and Activities of Daily Living (ADL) scales (see Table 1). All subjects underwent vestibular bed-side examinations with video-oculographic monitoring, completed with the study of paroxysmal positional nystagmus and caloric stimulation according to Fitzgerald–Hallpike’s criteria to exclude an acute labyrinthine deficit. Bed-side examination consisted the following tests: Romberg, Fukuda, Halmagyi, Head shaking, and Vibration.
Caloric test stimulates the left or right ear with warm and cool air or water causing a fluid density change in the lateral canal. By comparing the response of the left and right ear to warm and cool stimuli one can determine if there is a unilateral weakness.
During the Halmagyi head thrust test (HHTT) the examiner thrusts the head of the patient firmly from left to right at random and from right to left a little later. The instruction to the patient is to fix on a point in the distance behind the examiner. When the healthy subject’s head is turned to the side, the vestibulo-ocular reflex will maintain the target on the fovea and no refixation saccade will be needed. The Halmagyi test is positive for the side that causes the refixation saccade upon thrust.
Vibration testing involves placing a handheld vibrating instrument on the left and right mastoid bone and then observing changes in the presence or intensity of nystagmus. The results may be abnormal in patients with unilateral vestibular hypofunction.
During the head-shake assessment, the examiner shakes the head of the patient quickly back and forth for 30 s with fixation removed, after which the eyes are examined for the presence or absence of nystagmus. Presence of head-shake nystagmus may indicate asymmetric peripheral vestibular function.
The experimental protocol was designed in accordance with the Declaration of Helsinki (1964). All study participants provided informed consent.
Intervention
Intervention protocol was the same used in previous research, to allow for a better comparison among the different studies [9,10,11]. Vibration was simultaneously applied on the quadriceps tendon insertion of the two legs. Vibratory stimulation was applied to the quadriceps by a specific device, consisting of an electromechanical transducer, a mechanical support rigidly fixed to the floor and an electronic control device. A mechanical arm allowed the transducer to be placed on the distal end of the vastus medialis and the common tendon of the rectus and intermedius femoris, at about 2 cm from the medial edge of the patella [10]. Soft tissues were compressed to ensure better transmission of vibrations to the quadriceps muscles. The transducer was applied perpendicular to the muscle, near its distal tendon insertion generating a sinusoidal displacement at 100 Hz, 0.2–0.5 mm peak-to-peak. The vibration frequency was set at 100 Hz. During vibratory stimulation, the participants were supine and contracted their quadriceps. To maintain this contraction, the subjects were asked to keep the cavum popliteus in contact with the bed as indicated by previous studies [10]. The researchers monitored muscle contraction throughout the entire series of applications, by palpation and visual inspection. Mechanical stimulation was applied over 3 consecutive days. Each of these applications lasted 30 min; for every 10 min of vibrations, there was a 1-min interval during which the mechanical application was interrupted and the subject relaxed her quadriceps.
Outcome
Patients were evaluated both functionally and instrumentally.
The main clinical outcomes were evaluated through the Performance-Oriented Mobility Assessment (POMA) scale, originally developed by Tinetti; POMA is a widely reliable and commonly used tool for assessing mobility and the risk of falling of the elderly [12]. It is easily applied in clinical setting and requires less than 15 min to be administered. Several adapted versions of POMA have been published [13]; in this study only the original 28-point version was applied [14]. The total POMA scale (POMA-T) consists of a balance scale (POMA-B) and a gait scale (POMA-G). POMA-B carries the subject through positions and changes in position, reflecting on stability tasks. In POMA-G, several qualitative aspects of the locomotion pattern are examined. Each item is scored on a two- or three-point scale, resulting in a maximum score of 28 on POMA-T and 16 and 12 on POMA-B and POMA-G, respectively [12]. POMA-T has been shown to have high intra- and inter-rater reliability [15] and is a suitable performance measure for evaluating balance among the elderly [16].
The following functional tests were done:
-
Posture The subjects were required to maintain the standing posture on a Pressure Platform (BTS Bioengineering P-WALK) for 30 s with the feet fixed position (30° externally rotated in respect to the anterior axis direction). Participants were instructed to stand upright with their feet together and hands at their side while looking at a visual target located in front of them in the first test and standing in absence of visual input in the second test. The tests, each of 60 s in duration, were alternately recorded for each condition (open OE and close eyes CE). A 1-min resting interval time was considered between each trial. Static balance has been evaluated by the record of center of pressure (CoP) sway with open eyes and closed eyes. The sway area and the sway length has been recorded in both the OE and CE conditions using the SWAY software program (BTS Engineering). Pressure Platform (BTS Bioengineering P-WALK) used is composed of 2304 resistive sensors (10 × 10 mm size) with the dimension of 500/4000 × 480 mm. The acquisition frequency is 100 Hz and the pressure range 30–400 kPa. Moreover, Romberg index as a ratio between closed/open eyes area × 100 was calculated.
-
Timed Up-and-Go (TUG) Test Subjects were requested to sit on a standard office chair. Following a verbal signal, they stood up, walked straight for 3 m at a comfortable and safe speed [17], performed a 180° turn, walked back to the chair and performed a second 180° turn to sit down. Three trials were considered. The Timed Up-and-Go (TUG) Test is widely used in the assessment of functional mobility and dynamic balance and measures the time (in seconds) necessary to stand up from a chair with arm rests, walk 3 m, turn around, walk back to the chair and sit down again [17]. TUG test has been measured and evaluated with an inertial measurement units (IMUs), a new system that have become quite popular for activity logging and healthcare applications [18]. The tool used in this analysis was BTS G-Walk®. It is made up of an IMU, the BTS® G-Sensor. The IMU was built with a triaxial accelerometer 16 bit/axes with multiple sensitivity (± 2, ± 4, ±8, ± 16 g), a triaxial magnetometer 13 bit (± 1200 uT) and a triaxial gyroscope 16 bit/axes with multiple sensitivity (± 250, ± 500, ±1000, ± 2000 °/s). This hardware is capable of acquiring and transmitting data to a PC through a Bluetooth connection. The software used is BTS® G-Studio (Copyright © BTS Bioengineering S.p.A. 2009–2012) which performs data acquisition, elaboration, reporting and storage. For this study, data were collected using a sampling frequency of 100 Hz. BTS G-Studio has numerous built-in analysis protocols. More specifically, it has a specific protocol capable of analyzing the TUG test which automatically computes all the test’s temporal parameters. Prior to data acquisition, the IMU has to be precisely placed in L5 using an elastic belt.
IMUs have been utilized quite extensively for instrumenting the Time Up and Go test. This system was able to measure angular positions, velocities and accelerations in the three axial directions.
The following parameters were selected as more representative for the evaluation of TUG test:
-
Time needed to perform the TUG test (TUG time) [s];
-
Time needed to perform the standing up phase (the time required from sit to stand) [s];
-
Time needed to perform the sitting phase (the time required from stand to sit) [s];
-
The velocity to perform the TUG mid turning (TUG mid turning): [°/s].
Statistical analysis
The statistical analysis of the continuous variables was conducted calculating median and range (min–max), since these variables were not normally distributed. Time trends of these variables were plotted with box plot.
Friedman test for non-parametric values had been used.
The statistical significance was set at p = 0.05. The analysis was carried out using SPSS 19.0.
Results
Thirty patients (8 male and 22 female; 80.9 ± 4.0) have been enrolled and evaluated before and at three different follow-up time after treatment.
Table 2 shows the stabilometric parameters and the Tinetti Test results.
Stabilometric analysis showed statistically significant differences in both the CoP area and CoP sway in close eyes testing while no significant differences have been showed in open eyes evaluation. A significant score reduction of Romberg Index (closed/open eyes reported to area) was found between pre and after treatment with a score reduction.
The median value of the Tinetti score significantly increased after treatment but specially at the follow-up evaluation passing from a class score indicating a “moderate’’ risk of falling (score between 20 and 22) to a class of ‘‘low’’ risk of falling (score between 23 and 27).
Table 3 shows the TUG evaluation results: the global time was significantly reduced after treatment associated to a reduction of the standing up phase while the sitting phase remained unchanged; the rotation velocity during test significantly improved.
In Fig. 1 the box plot diagram for Romberg Index for equivalent area and Tinetti test are shown.
Discussion
From our knowledge for the first time in this study, we have evaluated and treated with focal muscle vibration patients older than 65 years lamenting postural disequilibrium previously studied to exclude vestibular and ear problems; moreover an instrumental evaluation was proposed not only for postural stability but also for clinical testing.
The main finding in this study is that r-MV led to significant improvement of stability both in static and in dynamic trials; this is particularly significant if we consider the TUG test. The TUG test is commonly used to evaluate older people, both in clinical practice and in research settings, with the score of 12 s used as the average time taken by elderly people residing at home [19, 20] and a score under 20 s is considered as not requiring personal assistance for transfers. The cutoff for risk of falls is 14 s [21].
In our sample of autonomous patients we have observed a statistically significant reduction of the total time of the test associated to an amelioration of the standing up phase and in addition an improvement of rotation speed; these parameters suggest that immediately after vibration but even more at distance from the rMV treatment, patients showed an improved stability and motor output. These data confirm the double hypothesis of the capacity of rMV to induce persisting changes in the central nervous system associated to a spontaneous increase of the daily activities, following the increased strength and fatigue resistance [10], which might create new virtuous circles.
Furthermore, the postural stability seems to also improve after the vibratory treatment in accordance to other studies done in pathologic condition [8, 22] We observed a significant improvement of postural control in only the trail with closed eyes; in this condition the visual cues are abolished and the patient maintains his/her balance only by means of the vestibular and proprioceptive inputs. These results may be attributed to the proprioceptive role of muscle vibration in improving postural stability.
The findings presented in this paper confirm the beneficial role of rMV in elderly patients with postural instability. Future studies are recommended using a randomized controlled trial model in a bigger cohort and with longer follow up.
Abbreviations
- rMV:
-
Repetitive muscle vibration
- POMA:
-
Performance-oriented mobility assessment
- CoP:
-
Center of pressure
- TUG:
-
Timed up-and-go
- IMU:
-
Inertial measurement unit
References
Gravamens WC, Ooms ME, Hofstee HM et al (1996) Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol 143:1129–1136
O’Loughlin JL, Boivin JF, Robitaille Y et al (1994) Falls among the elderly: distinguishing indoor and outdoor risk factors in Canada. J Epidemiol Community Health 48:488–489
Lawson J, Fitzgerald J, Birchall J et al (1999) Diagnosis of geriatric patients with severe dizziness. J Am Geriatr Soc 47:12–17
Katsarkas A (1994) Dizziness in aging: a retrospective study of 1194 cases. Otolaryngol Head Neck Surg 110:296–301
Barin K, Dodson EE (2011) Dizziness in the elderly. Otolaryngol Clin North Am 44:437–454
Teasdale N, Stelmach GE, Breunig A (1991) Postural sway characteristics of the elderly under normal and altered visual and support surface conditions. J Gerontol 46:B238–B244
Goble DJ, Coxon JP, Wenderoth N et al (2009) Proprioceptive sensibility in the elderly: degeneration, functional consequences and plastic-adaptive processes. Neurosci Biobehav Rev 33:271–278
Celletti C, Castori M, Galli M et al (2011) Evaluation of balance and improvement of proprioception by repetitive muscle vibration in a 15-year-old girl with joint hypermobility syndrome. Arthritis Care Res (Hoboken) 63:775–779
Caliandro P, Celletti C, Padua L et al (2012) Focal muscle vibration in the treatment of upper limb spasticity: a pilot randomized controlled trial in patients with chronic stroke. Arch Phys Med Rehabil 93:1656–1661
Celletti C, Fattorini L, Camerota F et al (2015) Focal muscle vibration as a possible intervention to prevent falls in elderly women: a pragmatic randomized controlled trial. Aging Clin Exp Res 27:857–863
Filippi GM, Brunetti O, Botti FM et al (2009) Improvement of stance control and muscle performance induced by focal muscle vibration in young-elderly women: a randomized controlled trial. Arch Phys Med Rehabil 90:2019–2025
Faber MJ, Bosscher RJ, van Wieringen PC (2006) Clinimetric properties of the performance-oriented mobility assessment. Phys Ther 86:944–954
Ko¨pke S, Meyer G (2006) The Tinetti test: Babylon in geriatric assessment. Z Gerontol Geriatr 39:288–291
Tinetti ME (1986) Performance oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34:119–126
Cipriany-Dacko L, Innerst D, Johannsen J et al (1997) Interrater reliability of the Tinetti balance scores in novice and experienced physical therapy clinicians. Arch Phys Med Rehabil 78:1160–1164
Lin MR, Hwang HF, Hu MH et al (2004) Psychometric comparisons of the timed up and go, one-leg stand, functional reach, and Tinetti balance measures in community-dwelling older people. J Am Geriatr Soc 52:1343–1348
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic function al mobility for frail elderly persons. J Am Geriatr Soc 39:142–148
Bolink SA, Naisas H, Senden R et al (2016) Validity of an inertial measurement unit to assess pelvic orientation angles during gait, sit–stand transfers and step-up transfers: comparison with an optoelectronic motion capture system. Med Eng Phys 38:225–231
Bohannon RW (2006) Reference values for the timed up and go test: a descriptive meta-analysis. J Geriatr Phys Ther 29:64–68
Idland G, Rydwik E, Smastuen MC (2013) Predictors of mobility in community-dwelling women aged 85 and older. Disabil Rehabil 35:881–887
Shumway-Cook A, Brauer S, Woollacott M (2000) Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys Ther 80:896–903
Pazzaglia C, Camerota F, Germanotta M (2016) Efficacy of focal mechanic vibration treatment on balance in Charcot-Marie-Tooth 1A disease: a pilot study. J Neurol 263:1434–1441
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has a conflict of interest which could alter the primary interest of this study.
Human and animal rights
The experimental protocol was designed in accordance with the Declaration of Helsinki (1964).
Informed consent
All study participants provided informed consent.
Rights and permissions
About this article
Cite this article
Attanasio, G., Camerota, F., Ralli, M. et al. Does focal mechanical stimulation of the lower limb muscles improve postural control and sit to stand movement in elderly?. Aging Clin Exp Res 30, 1161–1166 (2018). https://doi.org/10.1007/s40520-018-0909-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-018-0909-x