Abstract
Background and aims
To examine antimicrobial resistance of commonly isolated pathogens in elderly hospitalized patients.
Methods
Data regarding all clinically significant isolates from blood and urine cultures of patients admitted to a multilevel geriatric hospital during March 2015 to April 2016 were collected. Antimicrobial susceptibility testing was performed according to Clinical and Laboratory Standard Institute guidelines.
Results
Escherichia coli, Proteus mirabilis, and Klebsiella pneumoniae were the most common isolates, with proportions of extended spectrum beta-lactamase positivity of 60, 40, and 61% respectively. Adjusted logistic regression models indicated that resistance of Escherichia coli to ceftriaxone [odds ratio (OR) 2.8, 95% confidence interval (CI) 1.5–5.1], ceftazidime (OR 2.8, 95% CI 1.5–5.1), ciprofloxacin (OR 2.2, 95% CI 1.2–4.0), amoxicillin/clavulanic acid (OR 2.3, 95% CI 1.2–4.3), and trimethoprim/sulfamethoxazole (OR 2.4, 95% CI 1.4–4.3) was significantly higher in skilled nursing wards than in acute geriatric wards. Resistance of Proteus mirabilis to ceftriaxone (OR 3.1, 95% CI 1.5–6.4) and Klebsiella pneumoniae to ciprofloxacin (OR 3.2, 95% CI 1.3–7.9) was significantly higher in skilled nursing wards than in acute wards.
Conclusions and discussion
Antimicrobial resistance was found to be high in a multilevel geriatric hospital, especially in skilled nursing wards. These findings call for rethinking of the empirical antimicrobial therapy and of the efforts for prevention of nosocomial infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infectious diseases have remained one of the important causes of death, disability, and functional decline in older persons; therefore, frequent prescribing of antibiotics is common practice for this population. The large volume of antibiotics prescribed has contributed to the emergence of highly resistant pathogens among geriatric patients, including methicillin-resistant Staphylococcus aureus, extended spectrum beta-lactamase (ESBL)-positive, and other resistant microorganisms [1,2,3].
Immune function is known to decrease with age together with chronic diseases, such as cancer, which affect host resistance. Thus, the combined effects of age-related decline in host resistance and the presence of underlying diseases and disabilities contribute to the greater vulnerability of older persons to infections and their complications [4, 5].
In elderly patients, the clinical presentation of infectious diseases may differ markedly from that in younger individuals. Localizing symptoms may be absent even when a bacteriologic cause (bacteremia or bacteriuria) has been clearly established. Signs and symptoms are often atypical, blunted or nonspecific. They may consist of altered mental status, general deterioration, falls, and anorexia [6]. Bacteriologic investigations in the elderly remain a diagnostic as well as a therapeutic challenge for the clinician. Only a few published studies of bacteremia in the elderly have referred specifically to skilled nursing facilities (SNF) [7,8,9,10,11].
Resistance of ESBL-positive microorganisms to antibiotics is increasingly reported worldwide, particularly the ESBL-producing Escherichia coli [12,13,14]. The World Health Organization has recognized the importance of studying the emergence and determinants of acquired antimicrobial resistance and the need to devise appropriate strategies for its control.
The high frequency in recent years of antimicrobial resistance to ESBL in our geriatric multilevel hospital led to this investigation of the clinical and microbiological characteristics of antimicrobial resistance in all positive isolates.
Methods
Study design
The setting is a university-affiliated 400-bed geriatric hospital with onsite full laboratory capabilities. Patients are admitted from the community, nursing homes and general hospitals into acute, rehabilitation, chronic mechanical ventilation, or skilled nursing wards. Data were collected retrospectively from records of the bacteriology laboratory for the period 1 year—March 2015 to April 2016. Charts of the cases with positive culture of blood and urine on hospital admission were identified and examined for demographic and clinical data: age (included were patient > 65 years), source of infection, type of hospital ward, and antimicrobial sensitivity or resistance of microorganisms. The same data were retrieved from non-infected patient that were hospitalized in the same geriatric wards in this period. The information retrieved from patients’ files was recorded on worksheets and then transferred to a database software program for statistical analysis.
Bacterial isolation and identification
The hospital’s standard practice is to recover specimens from relevant sites, such as blood or urine, on suspicion of infectious disease. For the purpose of this study, a clinically significant isolate was defined as a positive blood or urinary culture in a patient with high suspicion of infectious disease, and/or with oral fever more than 37.8 °C or less than 35.0 °C and/or other systemic symptoms such as unexplained deterioration of functional and mental status. All strains were cultured and identified by the Clinical Microbiology Laboratory. Blood culture was conducted by Bact Alert with selective media (bioMérieux, Marcy l’Etoile, France). Urine cultures were performed using Vitec 2 technology (V2 System Compact 200-a, North Caroline, USA).
Identification and antimicrobial susceptibility tests were performed with ID 32 E and ATB 32 Gram-negative panels in the automated ATB Expression System (bioMérieux, Marcy l’Etoile, France). Antibiotics used for susceptibility testing were: ampicillin, cloxacillin, cefazolin, ceftriaxone, ceftazidime, ertapenem, meropenem, amoxicillin/clavulanic acid, ciprofloxacin, gentamicin, amikacin, trimethoprim/sulfamethoxazole, nitrofurantoin, piperacillin/tazobactam, and vancomycin. The presence of ESBL in-vitro was confirmed with the Clinical and Laboratory Standard Institute (CLSI) double disc method. During the study period, microbiologists promptly advised clinicians about the strain of bacteria isolated and reported results of antimicrobial susceptibility tests.
Statistical analysis
Data are presented in terms of number and percent of findings. Associations between resistance to antibiotics and hospitalization wards were analyzed using logistic regression models adjusted for sex and age. Outcomes of the logistic regression analysis are presented as odds ratio (OR) and 95% confidence interval (CI). Statistical significance was defined according to α = 0.05, two-tailed. Analysis was performed using the SPSS 21 software (IBM Inc).
Results
During the period of the study, 4506 subjects were hospitalized in our geriatric hospital, in 957 (21%) of them, clinically significant isolates were detected and in 407 men (42.5%) and 550 women (57.5%). The mean age of the patients was 82.2 (SD ± 8.1). There were no significant difference on demographic and clinical data between patients with suspicion on infection disease and the same amount of non-suspected of infection disease patients. Isolates were from: 125 blood and 832 urine samples. The patients were hospitalized in acute geriatric (n = 522), skilled nursing (n = 250), rehabilitation (n = 166), and chronic mechanical ventilation (n = 19) wards.
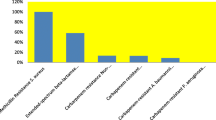
The microorganisms isolated in blood and urine specimens are presented in Table 1. Escherichia coli was the most prevalent isolate (detected in 39.8% of all cases), Proteus mirabilis (20.9%), and Klebsiella pneumoniae (16.0%).
The prevalence of microorganisms according to hospitalization wards is presented in Table 2. Escherichia coli was the most prevalent isolate in acute geriatric wards (detected in 46.2% of the cases). Proteus mirabilis was the most common isolate in skilled nursing wards (29.6%) and mechanical ventilation wards (42.1%).
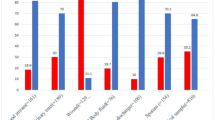
Resistance of microorganisms to antibiotics is presented in Table 3. Resistance of Escherichia coli to ceftriaxone was found in 61% of isolates and to ciprofloxacin in 64%. ESBL-positive Escherichia coli was observed in 60% of cases. Proteus mirabilis was resistant to ceftriaxone in 54% of isolates, to ciprofloxacin in 57%, to trimethoprim/sulfamethoxazole in 62%, and to nitrofurantoin in 84%; 40% of cases were ESBL-positive. Klebsiella pneumoniae was resistant to ceftriaxone in 61% of samples, to ciprofloxacin in 60% and to trimethoprim/sulfamethoxazole in 62%; 61% of isolates were ESBL-positive.
Resistance of microorganisms varied between hospitalization wards (Table 4). Adjusted logistic regression models indicated that resistance of Escherichia coli to ceftriaxone (OR 2.8, 95% CI 1.5−5.1), ceftazidime (OR 2.8, 95% CI 1.5−5.1), ciprofloxacin (OR 2.2, 95% CI 1.2−4.0), amoxicillin /clavulanic acid (OR 2.3, 95% CI 1.2−4.3), and trimethoprim/sulfamethoxazole (OR 2.4, 95% CI 1.4−4.3) was significantly higher in skilled nursing than in acute geriatric wards. Resistance of Proteus mirabilis to ceftriaxone (OR 3.1, 95% CI 1.5−6.4) and Klebsiella pneumoniae to ciprofloxacin (OR 3.2, 95% CI 1.3−7.9) was also significantly higher in skilled nursing than in acute wards.
Discussion
The most important findings of this study are the high prevalence of microorganism resistance to antibiotics and of ESBL-positive microorganisms. An additional interesting observation was the significantly higher rates of the resistance in skilled nursing than in acute geriatric wards.
The finding that Escherichia coli was the most frequent microorganism isolated concurs with other studies [7, 8, 15]. Ho et al. reported high prevalence of ESBL-positive Escherichia coli among elderly patients [16]. In De Vecchi et al. study [15], almost all Enterobacteriaceae isolates were susceptible to trimethoprim/sulfamethoxazole, contrasting with 60% resistance in the current study. Moreover, they reported the detection of ESBLs in 42% of isolates, compared to 60% of Escherichia coli, 40% of Proteus mirabilis, and 61% of Klebsiella pneumoniae in our study. Fluoroquinolones showed a limited activity in both their study and ours [15].
Empirical antimicrobial therapy without microbiological data is a common practice in the long-term care setting such as in SNF. The vast majority of prescribed antibiotics are ordered without direct examination of the resident by the primary care provider [17]. Nitrofurantoin has been suggested recently as an empirical treatment of nosocomial low urinary tract infections involving Escherichia coli and enterococci, comparing favorably with fluoroquinolones and co-trimoxazole [18]. Our results showed 84% Proteus mirabilis resistance to nitrofurantoin and 62% to trimethoprim/sulfamethoxazole.
With the rising number of older peoples, the need for geriatric SNF concomitantly increases. Residents of such facilities are generally very old and frail, often cognitively impaired and physically dependent, as well as highly vulnerable to infections from many origins [19]. Moreover, the setting of the SNF is favorable for regular exposure to microorganisms due to frequent contacts with staff and other residents, who may harbor infection, in a closed environment (limited ventilation, filtration, and removal of recirculated air, which could contain pathogens) [20]. Thus, prevention of nosocomial infection is particularly important [19, 20]. Often, inadequate numbers of highly trained medical personnel make this issue problematic.
Yoshikawa reported that the most common infections encountered in residents of SNFs are pneumonia, urinary tract, and skin/soft tissue infections, which together account for approximately 75% of all nursing facility-acquired infections [21]. Nowadays, the same spectrums of infectious disease are presents in geriatric hospitalization wards. As has been emphasized in other publications, conduction of research on infection monitoring and reducing antibiotic resistance is essential for improving the quality of long-term care facilities [22]. Antibiotic resistance is indeed a major issue confronting healthcare providers and their patients. Changing antibiotic resistance patterns, rising antibiotic costs and the introduction of new antibiotics have made the selection of optimal antibiotic regimens more difficult than in the past. Evidence-based guidelines for the implementation and measurement of antibiotic stewardship interventions in inpatient populations including long-term care were prepared by a multidisciplinary expert panel of the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. These recommendations address the best approaches for antibiotic stewardship programs to influence the optimal use of antibiotics [23, 24].
Limitations of study
The main limitation of the present investigation is its retrospective design. The additional limitation of our study: included were subjects with high suspicion of infectious disease on admission, we can apologize, that cases of intra-hospital infections may be more clinically complicated with higher frequency of resistant microorganisms. Moreover, since the study was conducted at a single medical center, its generalizability to other medical centers is not known.
In conclusion, the high prevalence of microorganism resistance to antibiotics in the multilevel geriatric hospital, especially in skilled nursing wards, calls for rethinking of empirical antimicrobial therapy as well as for additional measures and staff efforts for the successful prevention of nosocomial infection.
References
Augustine S, Bonomo RA (2011) Taking stock of infections and antibiotic resistance in the elderly and long-term care facilities: a survey of existing and upcoming challenges. Eur J Microbiol Immunol 1:190–197
Fagan M, Lindbaek M, Grude N et al (2015) Antibiotic resistance patterns of bacteria causing urinary tract infections in the elderly living in nursing homes versus the elderly living at home: an observational study. BMC Geriatr. doi:10.1186/s12877-015-0097-x
Yoshikawa TT (2002) Antimicrobial resistance and aging: beginning of the end of the antibiotic era? J Am Geriatr Soc 50:S226–S229
Castle SC (2000) Clinical relevance of age-related immune dysfunction. Clin Infect Dis 31:578–585
Staykova S (2013) Urinary tract infections in geriatric patients. Webmed Cent Nephrol 4:WMC003968
Wester AL, Dunlop O, Melby KK et al (2013) Age-related differences in symptoms, diagnosis and prognosis of bacteremia. BMC Infect Dis 13:346
Lubart E, Segal R, Haimov E et al (2011) Bacteremia in a multilevel geriatric hospital. J Am Med Dir Assoc 12:204–207
Lubart E, Kornitsky R, Dan M et al (2014) Bacteremia in a multilevel geriatric hospital, second look 5 years later. Br J Med Med Res 4:1729–1738
Mylotte JM, Tayara A, Goodnough S (2002) Epidemiology of bloodstream infection in nursing home residents: evaluation in a large cohort from multiple homes. Clin Infect Dis 35:1484–1490
Richards CL Jr (2007) Infection control in long-term care facilities. J Am Med Dir Assoc 8:S18–S25
Little MO (2011) Diagnostic challenge of bloodstream infections in long-term care. J Am Med Dir Assoc 12:166–168
Picozzi S, Ricci C, Gaeta M et al (2013) Do we really know the prevalence of multi-drug resistant Escherichia coli in the territorial and nosocomial population? Urol Ann 5:25–29
Briongos-Figuero LS, Gómez-Traveso T, Bachiller-Luque P et al (2012) Epidemiology, risk factors and comorbidity for urinary tract infections caused by extended-spectrum beta-lactamase (ESBL)-producing enterobacteria. Int J Clin Pract 66:891–896
Lu PL, Liu YC, Toh HS et al (2012) Epidemiology and antimicrobial susceptibility profiles of Gram-negative bacteria causing urinary tract infections in the Asia-Pacific region: 2009–2010 results from the Study for Monitoring Antimicrobial Resistance Trends (SMART). Int J Antimicrob Agents 40:S37–S43
De Vecchi E, Sitia S, Romanó CL et al (2013) Aetiology and antibiotic resistance patterns of urinary tract infection in the elderly: a 6-month study. J Med Microbiol 62:859–863
Ho PL, Chau PH, Yan MK et al (2014) High burden of extended-spectrum beta-lactamase - positive Escherichia coli in geriatric patients. J Med Microbiol 63:878–883
Warshaw G, Mehdizadeh S, Applebaum RA (2001) Infections in nursing homes: assessing quality of care. J Gerontol A Biol Sci Med Sci 56:M120–M123
McKinnell JA, Stollenwerk NS, Jung CW et al (2011) Nitrofurantoin compares favorably to recommended agents as empirical treatment of uncomplicated urinary tract infections in a decision and cost analysis. Mayo Clin Proc 86:480–488
Richards CL Jr (2005). Infections in long-term-care facilities: screen or clean? Infect Control Hosp Epidemiol 26:800–801
Yoshikawa TT, Norman DC (1995) Infection control in long-term care. Clin Geriatr Med 11:467–480
Yoshikawa TT, Norman DC (1996) Approach to fever and infection in the nursing home. J Am Geriatr Soc 44:74–82
van Buul LW, van der Steen JT, Veenhuizen RB et al (2012) Antibiotic use and resistance in long term care facilities. J Am Med Dir Assoc 13:568.e1–13
Barlam TF, Cosgrove SE, Abbo LM et al (2016) Executive summary: implementing an Antibiotic Stewardship Program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis 62:1197–2002
Cosgrove SE, Hermsen ED, Rybak MJ (2014)Guidance for the knowledge and skills required for antimicrobial stewardship leaders. Infect Control Hosp Epidemiol 35:1444–1451
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The study did not have specific funding.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the institutional ethical committee.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Goltsman, G., Mizrahi, E.H., Leibovitz, A. et al. Comparative characteristic of antimicrobial resistance in geriatric hospital: a retrospective cohort study. Aging Clin Exp Res 30, 839–843 (2018). https://doi.org/10.1007/s40520-017-0841-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-017-0841-5