Abstract
Background and aims
Executed studies did not clearly identify which index of comorbidity was an independent outcome determinant. The aim of this prospective observational cohort study was to address this issue.
Methods
We analyzed 200 consecutive patients with hip fracture. All patients underwent rehabilitation. At admission comorbidity was assessed through the cumulative severity, severity index, and comorbidity index of the Cumulative Illness Rating Scale. Discharge scores and effectiveness in the Functional Independence Measure motor subscale, and discharge destination were the outcome measures. Multivariate regression analyses were performed to identify determinants of outcome.
Results
Mini Mental State Examination and comorbidity index of the Cumulative Illness Rating Scale were important independent determinants of final (respectively, β = 0.46 and −0.25) and effectiveness (respectively, β = 0.47 and −0.25) in motor Functional Independence Measure scores, while hip strength and Rankin score were determinants of final motor Functional Independence Measure score (respectively, β = 0.21 and −0.20). Comorbidity index of the Cumulative Illness Rating Scale (odds ratio 8.18 for ≥3 versus < 3 comorbidity score; 95% confidence interval, 1.03–64.7) and Geriatric Depression Scale (odds ratio 4.02 for ≥6 versus ≤5 depression scale score; 95% confidence interval, 1.52–10.63) were risk indicators for nursing home.
Conclusions
Among the indices of the Cumulative Illness Rating Scale, comorbidity index is the sole independent determinant of both motor Functional Independence Measure scores and discharge destination in hip fracture patients. This suggests to specifically evaluate this index to identify the patients who may be admitted to a rehabilitation program.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures are one of the most common orthopedic injuries affecting the elderly. They usually occur in patients who are older than 60 years and have pre-existing medical problems or comorbidities. Surgery is the definitive treatment for almost all hip fractures, but evidence indicates that a return to optimal functional levels after surgery is not determined so much by the type of operation as by preoperative comorbidities and postoperative complications [1].
It has long been recognized that comorbidity is a risk factor for increased mortality in the months following hip fracture, longer length of stay in hospital, and poorer quality of life [2, 3]. It is also well established that comorbidity is a risk factor for poor functional outcome in hip fracture. Studies analyzing specific single comorbidities have demonstrated that stroke, depression, and cognitive and neurological impairment have a negative impact on hip fracture rehabilitation [3, 4]. Other studies have analyzed all relevant diseases associated to hip fracture [5, 6] using formal scales of comorbidity such as the Cumulative Illness Rating Scale (CIRS) [5].
However, studies using formal scales of comorbidity so far carried out have discordant findings and have not clearly defined which precise index of comorbidity (e.g., cumulative severity of all comorbidities, average severity of all comorbidities, or the number of moderate-to-severe comorbidities) is the most important outcome determinant.
The aim of this prospective observational cohort study was to verify the relationship between comorbidity and functional outcome in hip fracture patients and identify which index of comorbidity is the most important outcome determinant. This information may offer physicians an additional tool to identify hip fracture patients who may benefit from rehabilitation and, hence, could be admitted to a rehabilitation program.
Methods
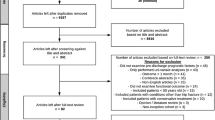
Patients
This prospective cohort study was carried out at the Rehabilitation Center of Lumezzane of the Salvatore Maugeri Foundation (Italy) in hip fracture patients. All consecutive patients with primary diagnosis of hip fracture admitted to our Rehabilitation Unit between January 2010 and February 2014 were considered for inclusion. Patients referred from other departments outside the province of Brescia for concomitant acute events during rehabilitation and patients who died or were transferred back to acute care during the course of rehabilitation were excluded. Patients who did not give informed consent, were not able to walk prior to fracture, were not living at home at the time of the fracture, were aged <65 years, or who had pathological fractures were also excluded.
The Technical Scientific Committee of our Institute approved the study protocol and all patients gave their written informed consent to participate. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Mode of assessment
Clinical evaluation of all patients was performed at admission and at the end of rehabilitation by a qualified team of physiatrists plus geriatrician by means of scales of demonstrated reliability, validity, and sensitivity that have been used in previous studies concerning hip fracture recovery. Patient characteristics (age, gender) and comprehensive clinical data including orthopedic treatment (arthroplasty, osteosynthesis, other), time from fracture to admission for rehabilitation (days), length of stay in hospital (days) (LOS), and discharge destination (home or nursing home) were also recorded.
-
The Cumulative Illness Rating Scale (CIRS) was used to evaluate comorbidity [5]. This instrument measures disease burden in individuals with various chronic diseases. The CIRS provides a comprehensive review of medical problems concerning 14 organ systems, rating each organ system 1–5. The instrument gives a cumulative score of severity of all comorbidities (cumulative severity), average severity of all comorbidities (severity index), and the number of comorbidities of moderate or severe level (comorbidity index). In this study, the CIRS was used without taking into account musculoskeletal problems.
-
The Neuropsychiatric Inventory (NPI) was used to evaluate neuropsychiatric symptoms (delusions, hallucinations, agitation/aggression, depression/dysphoria, anxiety, elation/euphoria, apathy/indifference, disinhibition, irritability/lability, aberrant motor behavior, night-time behavior, and change in appetite/eating) [6]. The NPI total score ranges from 0 to 144 with higher scores indicating more severe psychopathology. The NPI score was obtained within the first 3 days of the patient’s entry in hospital through an interview performed with his/her caregiver.
-
The Functional Independence Measure (FIM) was used to assess the patients’ degree of independence and need of assistance in performing basic activities of daily living (ADLs) [7]. It is an 18-item ordinal scale with 7 levels ranging from 1 (total dependence) to 7 (total independence). The FIM can be subdivided into a 13-item motor subscale and a 5-item cognitive subscale. The motor and cognitive subscale scores range from 13 to 91 (motor-FIM) and from 5 to 35 (cognitive-FIM). The maximum total score is 126. Patients were assessed by a qualified physiatrist.
-
The modified Rankin scale was used to evaluate disability [8]. This is a 6-grade scale, from 0 (independence) to 5 (severe disability).
-
The Mini Mental State Examination (MMSE) was used to evaluate cognitive impairment [9]. The MMSE is scored from 0 to 30, with higher scores indicating better cognitive performance. The MMSE was corrected for age and school education.
-
The 15-item Geriatric Depression Scale (GDS) was used to evaluate baseline depressive symptoms [10]. A GDS score of 6 or higher (range 0–15) was the cut-off used to define significant depressive symptoms.
-
The Muscle Strength Grading Scale (Oxford Scale) [11] was used to assess hip muscle strength. It evaluated the muscle strength with a score ranging from 0 to 5 (where 0 = no movement and 5 = muscle contracts against full resistance). In the current study, the sum of strength of flexor and abductor muscles was considered.
-
A manual goniometer was used to measure the range of motion (ROM) of the hip joint. In the present study, the sum of ROM in flexion (0°–130°) and abduction (0°–45°) was considered.
Rehabilitation program
All patients underwent an average of 330 min/week of motor rehabilitation (6 days/week) and, in the last 2 weeks of their hospital stay, 150 min/week of occupational therapy (5 days/week). The motor rehabilitation program was based on hip ROM, strengthening and conditioning exercises, and bed-to-chair mobility, wheelchair skills, pre-gait (sit-to-stand, standing balance) and gait (parallel bars, walker, crutches) activities, bathroom skills, and ADL training. Rehabilitation commenced the day after admission. Needs, specific goals set, and progress/outcomes achieved were discussed at admission and bi-monthly by the rehabilitation team (composed of physicians, physiotherapists, and an occupational therapist) on a patient-by-patient basis. Patients were discharged only when, after evaluation by the rehabilitation team, it was considered that no further in-hospital improvement with rehabilitation was likely to occur.
Statistical analysis
All statistical analyses were performed with the software application Statistica Version 6 (StatSoft, Tulsa, OK, 2001). The Spearman’s rank correlation coefficient and χ 2 tests (Fisher’s exact or Pearson’s as appropriate) were used to assess the relationship between variables, while stepwise multiple regression analyses (linear and logistic) were performed to identify determinants of outcome measures. All statistically significant variables at the univariate regression analysis were submitted to the multivariate analysis. Age, gender, presence of family caregivers, orthopedic treatment, time interval from onset to admission (OAI), Rankin, MMSE, CIRS (cumulative severity, severity index, comorbidity index), NPI, hip ROM, and muscle strength at admission were independent variables.
For a more immediate comprehension by clinicians, for the logistic regression analysis, the continuous variables were dichotomized on the basis of predetermined clinical or statistical (median) cut-offs. In particular, we used a cut-off point of ≥75 years for age, ≥2 for relatives, longer than 11 days for OAI, >4 severe disability for Rankin, <11 for MMSE (where score <11 indicated severe cognitive impairment), ≥ 6 for GDS (where score ≥6 indicated depression), >2 for CIRS severity (where >2 indicated a mean score of all CIRS comorbidities >2), ≥3 for CIRS comorbidity (where ≥3 indicated presence of 3 or more comorbidities of moderate or severe level), ≥13 for cumulative CIRS severity (where >13 indicated a cumulative score of all CIRS comorbidities), ≥1 for NPI (where a total score ≥1 indicated presence of neuropsychiatric symptoms), >88 for ROM (where score >88 indicated presence of more than 50% of hip ROM in flexion and abduction), and >5 for muscle strength (where score >5 indicated presence of more than 50% of strength of hip flexor and abductor muscles).
Multiple regression analysis was performed after checking of the residual distribution and homoscedasticity.
Final score and effectiveness in motor-FIM and discharge destination were the outcome measures. Effectiveness was defined as the proportion of potential improvement achieved during rehabilitation, calculated by the following formula: [(final score − initial score)/(maximum score − initial score)] × 100 [12].
A p value <0.05 was considered statistically significant with the exception of Spearman’s rank correlation coefficient where p < 0.01 was considered for statistical significance.
Results
During the study period, 218 patients with primary diagnosis of hip fractures were admitted to our Rehabilitation Unit. During in-hospital rehabilitation, 12 patients died or were transferred back to acute care hospitals, and six patients were aged <65 years. As a result, 200 patients were included in the outcome analysis. Out of 200, 174 patients were from Orthopedic Departments, 19 from home, and seven from nursing home, for problems with walking following surgery (e.g., placing weight on the fractured limb).
Table 1 shows the demographic and clinical characteristics of the study population.
In the study population, 101 patients underwent arthroplasty and 91 osteosynthesis.
At admission these patients differed only in cognitive-FIM and time from fracture to admission for rehabilitation: the cognitive-FIM scores were lower in arthroplasty patients (p = 0.016), while the time from fracture to admission for rehabilitation was longer in osteosynthesis patients (p < 0.001) (Table 2).
At discharge arthroplasty patients had the same motor, cognitive, and total-FIM scores and effectiveness in motor-FIM score (p = 0.661, p = 0.143, p = 0.414, p = 0.992, respectively) and LOS (p = 0.118). At discharge 87.1% of arthroplasty patients and 89.0% of osteosynthesis patients returned home (p = 0.688) (Table 2).
Comorbidities
Table 3 lists the comorbidities described by CIRS and their prevalence in the 3 + moderate-to-severe comorbidities patients:hypertension (72.5%) and cardiac (61%) and vascular (55.5%) diseases were the most common diseases.
Relationship between FIM outcome and patients’ demographic/clinical characteristics
Table 4 reports the Spearman’s correlation analysis showing that cumulative severity, severity index, and comorbidity index of CIRS were correlated to FIM final score and effectiveness score. Table 5 shows the results of the multivariate linear regression analysis showing that MMSE and CIRS comorbidity index were independent determinants of final (respectively, β = 0.46 and −0.25) and effectiveness (respectively, β = 0.47 and −0.25) in motor-FIM scores, while hip strength and Rankin score were independent determinants of final motor-FIM score (respectively, β = 0.21 and −0.20).
In the patients’ sample, the number of moderate-to-severe comorbidities on admission ranged from 0 to 11 and was related to FIM outcomes: a higher number of organ systems with moderate-to-severe impairment were associated with lower final score and effectiveness in motor-FIM scores (Table 4).
Relationships between discharge destination and patient demographic/clinical characteristics
At the end of rehabilitation, 87.5% of patients returned to their home. Age, GDS, ROM, Rankin, cumulative severity/severity index, and comorbidity index of CIRS were the variables having associations with discharge destination in the univariate analysis. However, when these variables were included in the backward (stepwise) logistic regression analysis, CIRS comorbidity index and GDS only were the risk determinants for nursing home (Table 6). Patients with a moderate-to-severe impairment on admission in 3 organ systems or more had a risk to go to nursing home eight times higher than that of patients with 1–2 organ systems (Table 6). These findings were confirmed also when continuous variables, instead of dichotomized ones, were entered into the logistic regression model [data not shown: CIRS comorbidity index and GDS only were significantly associated with discharge destination (p = 0.003 and p = 0.019, respectively)].
Discussion
The study found that in hip fracture patients a higher comorbidity is associated to poorer functional outcome [13, 14] and is an independent determinant both of motor-FIM scores and discharge destination.
We assessed comorbidity through the CIRS, that is considered a valid indicator of the health status and longitudinal outcome, and suitable for application in the rehabilitation setting.
CIRS [5] assesses comorbidity through three indices: the cumulative severity, severity index, and comorbidity index. Our study found that among these, only comorbidity index was an independent determinant of final and effectiveness in motor-FIM score.
Other authors have studied this topic [15,16,17] with discordant findings. Patrick et al. [16] showed that total score of CIRS was a predictor of FIM efficiency; Bernardini et al. [15] found that total score of the Severity of Illness Rating Scale was a predictor of functional outcome; while Press et al. [17] reported that the severity index of CIRS-G was a significant predictor of FIM outcomes. We obtained different findings, but the methodology of the present study was different from that of the above studies. Indeed, the cited authors analyzed only one or two of the indices considered, whereas we analyzed all the CIRS indices and found that the comorbidity index was the sole independent determinant of final FIM score.
The CIRS comorbidity index is based on the number of moderate-to-severe comorbidities, which are those with the highest negative impact on rehabilitation. Indeed, these latter may cause impairment of locomotor and cognitive function rendering the rehabilitation very difficult [4, 18]. Otherwise, during the course of rehabilitation, moderate-to-severe comorbidities may be more frequently complicated by adverse clinical events (as chest infection and heart failure) [19] which slow down the rehabilitation program and functional recovery in hip fracture patients [20].
On the contrary, cumulative severity and severity index are based on cumulative score of severity and average severity of all comorbidities considering both the moderate-to-severe and low severity comorbidities, which have in turn a lower impact on rehabilitation. Indeed, these latter are associated to lower neurological and psychiatric impairment and less frequently are complicated by adverse clinical events, so explaining our results.
Findings of rehabilitation in arthroplasty and osteosynthesis patients support the reported explanations. In the study, arthroplasty and osteosynthesis patients had the same number of moderate-to-severe comorbidities and at the end of rehabilitation display the same motor-FIM score and effectiveness in motor-FIM score.
Our study verified also relationships between the number of organ systems, with moderate or greater impairment, and FIM outcomes. Several studies have investigated this topic with conflicting results: Patrick [16] showed that presence of five or more comorbidities, with moderate or severe levels of pathology, was a risk factor for a poorer functional outcome [11], while others found similar results considering two or more than two comorbidities [21, 22]. Analyzing the number of comorbidities as a continuous variable, we found that the risk for a poorer functional outcome was higher when moderate-to-severe comorbidities were more numerous.
In addition, our study showed that all CIRS indices had associations with the discharge destination but, among them, the sole CIRS comorbidity index was a significant independent determinant. In the previous literature, there is no evidence of this finding. Pautex et al. [23] found MMSE score <24 to be a predictor of nursing home admission, while Titler et al. [24] showed younger age, admission from home, and having a spouse to be predictors of discharge to home. Conversely, Becker et al. [25] and Thorngren et al. [26] highlighted that the ability to walk before or after surgery was the most significant factor in predicting the ability to continue to live at home. Finally, Ottenbacher [27] highlighted that independent bowel and/or bladder function were strong predictors of living at home up to 6 months after hospitalization for hip fracture. Our finding adds information with respect to those studies which did not look at comorbidity severity.
In our study, patients having at admission ≥3 organ systems, with moderate-to-severe impairment, had at the end of rehabilitation an eight times higher risk of going in Nursing home than those with ≤2 organ systems.
These data indicate that a high number of organ systems with moderate-to-severe impairment on admission is an unfavorable prognostic factor for home destination at discharge and an independent determinant of destination at discharge. Presence of a high number of moderate-to-severe comorbidities may make it especially difficult for family caregivers to manage hip fracture patients at home and this may be the reason for transferring hip fracture patients to nursing homes at the end of a rehabilitation program.
In the study, MMSE was an independent determinant of final and effectiveness in motor-FIM score. This indicates that MMSE has relationships with FIM outcomes, but not with discharge destination of hip fracture patients who underwent rehabilitation.
This finding is partly in agreement with Ishida [28] and Feng [3] reporting that MMSE is one of most important determinant of functional outcomes.
Lenze at al [29] also pointed out that cognitive impairment is a determinant of functional outcome in hip fracture patients and suggested that this relationship is mediated by rehabilitation participation. He found that cognitively impaired patients have poor outcome because they cannot participate as well in their therapy sessions.
In the study, 101 patients underwent arthroplasty and 91 osteosynthesis. At admission, arthroplasty and osteosynthesis patients differed in cognitive-FIM score and time from fracture to admission for rehabilitation. At the end of rehabilitation these patients had similar cognitive, motor, and total-FIM scores and effectiveness in motor-FIM score, and returned home in the same proportion. Moreover, they obtained the same functional improvement with the same rehabilitation period. These data indicate that arthroplasty and osteosynthesis have a similar impact on rehabilitation of hip fracture patients and a similar influence on functional recovery of these patients [30].
The present study has some limitations. First of all, it was not a population-based study (patients were referred to us by general hospitals) and therefore it does not represent all hip fracture patients. Moreover, CIRS indices were only tested among patients admitted to one specific rehabilitation program and therefore the results may not apply to other programs with different entry criteria or rehabilitation programs. Another important limitation is that we did not include in the regression analysis all the possible determinants. Nevertheless, we have included in the regression analysis those independent variables that in previous studies were shown to be important predictors of outcome in hip fracture patients [17,18,19,20,21,22,23,24,25].
In conclusion, the study shows that, among CIRS indices, comorbidity index is the sole independent determinant both of motor Functional Independence Measure scores and discharge destination in hip fracture patients.
These findings suggest that CIRS comorbidity index should be used together with MMSE, hip strength, and initial disability to identify hip fracture patients who may benefit from rehabilitation and, hence, could be admitted to a rehabilitation program.
A high CIRS comorbidity index score is one of the reasons why to exclude hip fracture patients from rehabilitation program because it indicates a condition of clinical instability (i.e., that may lead to frequent interruptions of the rehabilitation program) and inability to perform daily rehabilitation sessions in full, so limiting the rehabilitation continuity and reducing the rehabilitation effectiveness.
References
Zuckerman JD, Fabian DR, Aharanoff G, Koval KJ, Frankel VH (1993) Enhancing independence in the older hip fracture patient. Geriatrics 48:76–78, 81
Koren-Hakim T, Weiss A, Hershkovitz A et al (2012) The relationship between nutritional status of hip fracture operated elderly patients and their functioning, comorbidity and outcome. Clin Nutr 31:917–921
Feng L, Scherer SC, Tan BY, Chan G, Fong NP, Ng TP (2010) Comorbid cognitive impairment and depression is a significant predictor of poor outcomes in hip fracture rehabilitation. Int Psychogeriatr 22:246–253
Mathew RO, Hsu WH, Young Y (2013) Effect of comorbidity on functional recovery after hip fracture in the elderly. Am J Phys Med Rehabil 92:686–696
Parmelee PA, Thuras PD, Katz IR, Lawton MP (1995) Validation of the Cumulative Illness Rating Scale in a geriatric residential population. J Am Geriatr Soc 43:130–137
Cummings JL (1997) The neuropsychiatric inventory: assessing psychopathology in dementia patients. Neurology 48(5 Suppl 6):S10–S16
Granger CV, Cotter AC, Hamilton BB, Fiedler RC (1993) Functional assessment: a study of persons after stroke. Arch Phys Med Rehabil 74:133–138
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Sheikh JI, Yesavage JA, Brooks JO 3rd, Friedman L, Gratzinger P, Hill RD, Zadeik A, Crook T (1991) Proposed factor structure of the Geriatric Depression Scale. Int Psychogeriatr 3:23–28
Miller DW, Hahn JF (1996) General methods of clinical examination. In: Youmans JR (ed). Neurological surgery, ed 4. W.B. Saunders Philapdelphia, pp 31–32
Shah S, Vanclay F, Cooper B (1990) Efficiency, effectiveness and duration of stroke rehabilitation. Stroke 21:241–246
Kristensen MT (2011) Factors affecting functional prognosis of patients with hip fracture. Eur J Phys Rehabil Med 47:257–264
Di Giorgio L, Sodano L, Touloupakis G, Piciocco P, Attala D, Villani C (2012) Proximal femur fractures in elderly patients: the influence of comorbidity on prognosis in the short, medium and long term. Clin Ter 163:95–99
Bernardini B, Meinecke C, Pagani M et al (1995) Comorbidity and adverse clinical events in the rehabilitation of older adults after hip fracture. J Am Geriatr Soc 43:894–898
Patrick L, Knoefel F, Gaskowski P, Rexroth D (2001) Medical comorbidity and rehabilitation efficiency in geriatric inpatients. J Am Geriatr Soc 49:1471–1477
Press Y, Grinshpun Y, Berzak A, Friger M, Clarfield AM (2007) The effect of co-morbidity on the rehabilitation process in elderly patients after hip fracture. Arch Gerontol Geriatr 45:281–294
Chiu KY, Pun WK, Luk KD, Chow SP (1992) A prospective study on hip fractures in patients with previous cerebrovascular accidents. Injury 23:297–299
Langhorne P, Stott DJ, Robertson L et al (2000) Medical complications after stroke: a multicenter study. Stroke 31:1223–1229
Guerini F, Frisoni GB, Morghen S, Speciale S, Bellelli G, Trabucchi M (2010) Clinical instability as a predictor of negative outcomes among elderly patients admitted to a rehabilitation ward. J Am Med Dir Assoc 11:443–448
Jamal Sepah Y, Umer M, Khan A, Ullah Khan Niazi A (2010) Functional outcome, mortality and in-hospital complications of operative treatment in elderly patients with hip fractures in the developing world. Int Orthop 34:431–435
Shebubakar L, Hutagalung E, Sapardan S, Sutrisna B (2009) Effects of older age and multiple comorbidities on functional outcome after partial hip replacement surgery for hip fractures. Acta Med Indones 41:195–199
Pautex S, Jacques MC, Sant A, Herrmann F, Chevalley T (2005) A short comprehensive assessment to predict outcome of elderly patients after hip fracture. Aging Clin Exp Res 17:116–120
Titler M, Dochterman J, Xie XJ et al (2006) Nursing interventions and other factors associated with discharge disposition in older patients after hip fractures. Nurs Res 55:231–242
Becker C, Gebhard F, Fleischer S et al (2003) Prediction of mortality, mobility and admission to long-term care after hip fractures. Unfallchirurg 106:32–38
Thorngren KG, Ceder L, Svensson K (1993) Predicting results of rehabilitation after hip fracture. A ten-year follow-up study. Clin Orthop Relat Res (287):76–81
Ottenbacher KJ, Linn RT, Smith PM, Illig SB, Mancuso M, Granger CV (2004) Comparison of logistic regression and neural network analysis applied to predicting living setting after hip fracture. Ann Epidemiol 14:551–559
Ishida Y (2004) Mortality and functional outcome of hip fractures in the elderly. Clin Calcium 14:408–417
Lenze EJ, Munin MC, Dew MA et al (2004) Adverse effects of depression and cognitive impairment on rehabilitation participation and recovery from hip fracture. Int J Geriatr Psychiatry 19:472–478
Kos N, Burger H, Vidmar G (2011) Mobility and functional outcomes after femoral neck fracture surgery in elderly patients: a comparison between hemiarthroplasty and internal fixation. Disabil Rehabil 33:2264–2271
Acknowledgements
The authors thank Rosemary Allpress for English revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The research was not supported by Pharmaceutical Companies, but by institutional funding.
Ethical approval
The Technical Scientific Committee of our Institute approved the study protocol. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Informed consent
All patients gave their written informed consent to participate.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gialanella, B., Prometti, P., Monguzzi, V. et al. Determinants of functional outcome in hip fracture: the role of comorbidity. Aging Clin Exp Res 30, 643–650 (2018). https://doi.org/10.1007/s40520-017-0812-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-017-0812-x