Abstract
Background
Life-space assessment incorporates all movements in terms of the distance from home, the frequency of movement and the need of assistance for movement. Executive function (EF) is an important higher order cognitive ability that controls and guides people’s goal-directed actions. We examined the cross-sectional and longitudinal associations between EF and life-space mobility, and investigated if perceived walking difficulties, lower extremity performance, and transportation difficulties explain the association.
Methods
157 community-dwelling persons aged 76–91 years participated in the study at the baseline, and 103 of them in 2-year follow-up study. Based on the distribution on the Trail Making Test participants were categorized into tertiles of EF. Life-space mobility was assessed using the Life-Space Assessment (range 0–120). Perceived walking difficulties and transportation difficulties were self-reported, and lower extremity performance was assessed with the short physical performance battery (SPPB). Adjustments were made for gender, age, number of chronic conditions, and years of education.
Results
Average age of participants at the baseline was 82.6 (SD 4.2) years and 61% were women. Individuals with poor EF had lower life-space mobility compared to those with good EF. SPPB and transportation difficulties explained the association. Over the 2-year follow-up, those with poor EF at the baseline showed steeper decline but the difference did not quite reach statistical significance (p = 0.068).
Conclusions
People with better executive function had higher life-space mobility. This was explained by better lower extremity performance and absence of transportation difficulties. Cognitive decline may hinder access to community amenities, which in turn may further accelerate cognitive decline.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ability to go where and when one wants to go and how one wants to get there is a key component of active aging [1]. Limitations in mobility reduce access to community amenities and threaten possibilities for social contacts [1], and predict further disability [2]. Life-space mobility, an indicator of community mobility, incorporates an individual’s internal physiologic and psychological capability relative to the environmental requirements of the place where the travel takes place [3]. Life-space mobility assessment includes estimates of the distance, the frequency and the need of assistance for moving [4]. Highly coordinated voluntary bodily movements caused by contracting muscles such as walking, as well as cognitively more complex but physically less demanding tasks such as using public transportation or driving a car [5] constitute important building blocks of life-space mobility. The association of life-space mobility with cognitive capacity in old age has been less studied. There are, though, some studies, that show that memory decline assessed with Mini-Mental State Examination correlates with lower life-space mobility [3, 6].
Mobility requires cognitive processing in addition to physiological functioning [7]. Holding information in mind, switching between tasks, inhibiting action and resisting distraction [8] are examples of cognitive processes needed for mobility control [9] and supervised by executive functioning (EF). EF refers to the higher order cognitive abilities, which are required when planning and carrying out complex, goal-oriented behavior [8]. Executive function plays an important role in supervising and managing many different cognitive domains [5]. These cognitive processes and mobility are supported primarily by the same prefrontal areas of the brain, which have been identified as the most vulnerable areas of the brain in the normal aging process [9–12]. The deterioration of the prefrontal area in aging does not only affect cognition but may contribute to motor performance and mobility as well, since the prefrontal areas regulate the speed of information processing, working memory and attention which have a crucial role in capability to complete motor tasks rapidly and efficiently [9, 13, 14]. Walking performance for example utilizes executive function and other complex cognitive processes such as estimation, planning and adjustments [15].
Life-space mobility correlates with lower extremity performance [16] and use of transportation [17], both of which also correlate with EF [18–20]. In this study, we investigated the association between EF and life-space mobility among community-dwelling older people, and assessed if perceived walking difficulties, lower extremity performance, and transportation difficulties, underlie this association.
Materials and methods
Study population
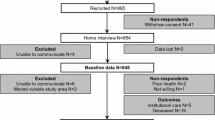
Altogether 169 community-dwelling people aged 76 to 91 years participated in the Hearing, Cognition and Wellbeing Study. Face-to-face interviews and sensory, physical and cognitive functioning measurements were conducted in the participants’ homes. Valid data on executive function (EF) and life-space mobility were available for 157 participants who form the analytic sample of the current cross-sectional study (eight refused and four were unable to perform the TMT test due to poor vision or upper extremity impairment). Of the initial 169 persons, 108 participated in the follow-up study 2 years later (32 were not interested to participate, 19 had deceased, one moved outside study area and nine were not reached). Of them, 103 participants had complete data available, and form the analytic sample of the current follow-up study (four refused and one was unable to perform the TMT test due to poor vision).
The participants of the current study were part of the Life-Space Mobility in Old Age (LISPE) study, described in detail previously [21]. LISPE is a population-based study among community living older people including 848 participants. Using random number tables a subset of 230 individuals was selected for the Hearing, Cognition and Wellbeing sub-study in year 2014 [22]. Those willing to participate and who did not experience severe problems in communicating, underwent the examinations and interviews during spring 2014 (n = 169).
The Hearing, Cognition and Wellbeing substudy sample (n = 169) did not differ from the initial LISPE study sample (n = 848) in terms of sex, age, years of education, number of chronic conditions, lower extremity performance measured with the Short Physical Performance Battery (SPPB), or cognitive functioning measured with Mini-Mental State Examination (MMSE) (all p values >0.127).
The LISPE study and the Hearing, Cognition and Wellbeing sub-study both comply with the principles of good scientific conduct and good clinical practice in all aspects of the Declaration of Helsinki, and were approved by the Ethical Committee of the University of Jyväskylä. All participants gave a written informed consent.
Executive function
EF was measured with the Trail Making Test (TMT). TMT is a paper-and-pencil task providing information on visual search, scanning, processing speed, mental flexibility, and executive function [23]. The TMT consists of two parts. In the TMT-A task participants were required to draw lines sequentially connecting randomly arranged encircled numbers (from 1 to 25) spread over a sheet of paper. In the TMT-B task participants were required to draw lines in numeric and alphabetical order (1-A-2-B-3-C, etc.) connecting randomly arranged encircles containing numbers (from 1 to 13) and letters (from A to L) spread over a sheet. The examiner pointed out errors as they occurred and the subject could continue to complete the task at the expense of additional time. Time to complete each task was measured in seconds [24, 25]. A maximum accepted time to complete each part of the test was 240 s and maximum accepted amount of errors was 4 [24]. Delta-TMT was calculated by subtracting time to perform TMT-A from time to perform TMT-B to control for the effects of motor function, visual scanning and processing speed. Delta-TMT has been used in previous studies to indicate executive functioning [19, 26]. EF was categorized into three approximately equal distribution-based groups as follows. Poor EF included those who did not perform TMT-A or TMT-B tasks within accepted time, or made more than 4 errors, or who failed to complete the task so that Delta-TMT could not have been calculated. Intermediate EF included those whose Delta-TMT was between 95 and 179 s and good EF included those whose Delta-TMT was 94 s or less. The cut-off between intermediate and good EF was defined according to the median value of Delta-TMT among those who completed the tests.
Life-space mobility
Life-space mobility was measured with the 15-item University of Alabama at Birmingham Study of Aging Life-Space Assessment (LSA) [3], which was translated into Finnish [27]. Participants were asked how many times during the past four weeks they had attained each life-space level (bedroom, other rooms, outside home, neighborhood, town, beyond town), and whether they needed help from another person or used assistive device. A composite score (range 0–120) that reflects distance, frequency, and independence of movement was calculated and used as an indicator of life-space mobility. Higher scores indicated higher life-space mobility [5, 21].
Mobility indicators
Lower extremity performance was assessed with the Short Physical Performance Battery (SPPB) [28]. The test battery comprises three tests assessing standing balance, walking speed over a distance of 2.44 m and time taken to complete five chair rises. Each test is rated from 0 to 4 points according to established age- and gender-specific cut-off points [28, 29]. A SPPB sum score was calculated (range 0–12) when at least two of the tests were completed [16]. If one of the tests was missing, the sum score of the two tests was transformed using proportion equation formula to reflect the maximum possible test score, i.e., the sum score was first multiplied by the maximum possible test score (12) and then divided by maximum possible performed test score (8). Higher scores indicate better physical performance.
Perceived difficulties walking 500 meters were self-reported. Participant was asked; “Are you able to walk about 500 m?” with response options “able without difficulty”, “able with minor difficulty”, “able with a great deal of difficulty”, “unable without the help of another person”, and “unable to manage even with help”.
Transportation difficulties were assessed based on perceived difficulties in use of public transportation, and frequency of driving. Participants were asked how they manage to use public transportation with response options; “able without difficulty”, “able with minor difficulty”, “able with a great deal of difficulty”, “unable without the help of another person”, and “unable to manage even with help”. This question was drawn from an 11-item self-report questionnaire for instrumental activities of daily living (IADL) [37]. Driving was assessed by asking “How often do you drive a car?” with response options; “Daily or nearly daily”, “Once or twice a week”, “Once or twice a month”, “Once or twice a year”, “Less than once a year”, “Never, I have never driven a car” and “Never, I have stopped driving a car”. People who did not drive regularly (at least once or twice a month) and had difficulties in using public transportation were categorized as having transportation difficulties while those, who did not have difficulties in using transportation or who drove a car at least once or twice a month were categorized as not having transportation difficulties.
Covariates
Number of self-reported chronic conditions was calculated from a list of 22 physician-diagnosed diseases and an additional open-ended question about any other physician-diagnosed chronic diseases [16, 21]. Participants were asked to report their total number of years of education.
Other variables
Cognitive functioning was measured using Mini Mental State Examination (MMSE) [30].
Statistical analyses
The descriptive measures were computed using means and standard deviations (SD) for continuous variables and percentages for categorical variables. Comparison between the three different EF groups was performed with one-way analysis of variance (ANOVA) for continuous variables and with cross-tabulation followed by Pearson’s Chi-square test for proportions in categorical variables.
The cross-sectional association between EF and life-space mobility was investigated with general linear regression model (GLM). The base model was adjusted for age and gender. To examine if the association between EF and life-space mobility was explained by the covariates, perceived walking difficulties, lower extremity performance and transportation difficulties were included into the model one at a time, and finally all the factors were included in the model simultaneously. Additionally, in the fully adjusted model we included the number of chronic conditions and years of education as covariates. The longitudinal association between EF and life-space mobility was investigated by constructing a general estimation equation (GEE) model [31] by specifying an unstructured outcome covariance matrix. We estimated the main effects of EF on life-space mobility and time interaction effects (group by time) for the 2-year follow-up. Models were adjusted for age and gender. The interaction between gender and EF on life-space mobility was not statistically significant (p > 0.290), thus all analyses were pooled by gender. For all tests two-tailed p values are reported and the level of significance was set at p < 0.05. The analyses were carried out with SPSS IBM version 24.0 (SPSS, Armonk, NY, IBM Corp).
Results
Baseline characteristics of the study participants according to the approximate tertiles of EF are presented in Table 1. The average age of the participants at the baseline was 82.6 years (SD 4.2) and 61% of them were women. Mean MMSE score at the baseline was 26.2 (SD 2.6) and 7.6% of the participants had MMSE < 23. Compared to individuals with good EF those with poor or intermediate EF were less educated, had significantly lower SPPB scores and lower life-space mobility. Eighty-three per cent of participants with good EF had no transportation difficulties while 56% of those with poor EF had no difficulties. Number of chronic conditions or difficulties in walking 500 meters did not differ between EF groups (Table 1).
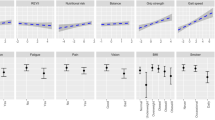
Marginal means and regression coefficients of life-space mobility by EF are shown in Table 2. Persons with poor or intermediate EF had lower life-space mobility compared to those with good EF (p = 0.006: marginal means 53.0, SE 2.7 for poor, 63.5, SE 2.7 for intermediate, and 64.0, SE 2.7 for good EF). Perceived difficulties in walking 500 meters did not attenuate the association between EF and life-space mobility (p = 0.005). Lower extremity performance and transportation difficulties attenuated the associations between EF and life-space mobility and rendered the differences statistically non-significant.
Compared to those who did not participate in the follow-up study (n = 61), those who participated (n = 108) were younger (82.2 years, SD 4.1 vs. 83.6 years, SD 4.3, p = 0.038), their mean SPPB (9.3, SD 2.0, vs. 7.2, SD 3.4, p < 0.001), MMSE (26.3, SD 2.7 vs. 25.4, SD 2.5, p = 0.033), and life-space mobility scores (63.1, SD 19.7 vs. 51.2, SD 20.4, p < 0.001) were higher at the baseline. The attrition was highest among those with poor EF at the baseline (53.7%), followed by those with intermediate (30.0%) or good (18.9%) EF at the baseline. Those with poor EF were five times (OR = 4.99, 95% CI 2.09–11.92), and those with intermediate EF almost two times (OR = 1.84, 95% CI 0.74–4.61) more likely to drop out from the follow-up compared to those with good EF.
Table 3 shows the mean values for life-space mobility at baseline and 2-year follow-up according to EF. Life-space mobility decreased most among those who had poor EF at baseline compared to those with intermediate or good EF, but the difference did not quite reach statistical significance (group by time interaction effect β= −6.198, p = 0.068).
Discussion
Our results showed that people with poor EF had lower life-space mobility than those with intermediate or good EF. The differences were largely explained by their poorer lower extremity performance and higher prevalence of transportation difficulties, both of which also underlie life-space mobility. The results of the 2-year follow-up study suggest that poor EF predicts a steeper decline in life-space mobility among older community-dwelling people; however, the interaction term did not quite reach statistical significance.
This is to our knowledge the first study examining the cross-sectional and longitudinal association between EF and life-space mobility among older community-dwelling individuals. Our findings add novel knowledge to emerging literature relative to association between cognitive functioning and mobility. In relation to EF and mobility, previous studies have examined only one aspect of mobility at a time whereas we were able to use life-space mobility as an outcome, which takes into account all mobility in its’ different forms including both physically active movement and movement using a vehicle. Life-space mobility assessment provides us information about “real life” mobility that may take place closer or further away from home. As a person moves further away from one’s home, the cognitive effort needed for the mobility may increase, e.g., in terms of finding directions, orienting oneself and recognizing the less familiar environmental features when approaching a far-away destination. Consequently, life-space mobility may be sensitive to early cognitive changes that may reduce the willingness to travel to more distant destinations [6, 32].
Motor control relies in prefrontal brain areas, which are most vulnerable to age-related losses [33], and cognitive and motor functions share the same neural network [13], which potentially explain why lower extremity performance and transportation difficulties coexist with cognitive decline. Adequate motor control, reaction speed, attention and working memory are important for lower extremity performance but they also are prerequisites for competent driving, and contribute to cognitive processes where EF is involved. Low EF decreases the likeliness that an individual could independently use public transportation or drive safely due to decreased ability to integrate information and plan a response [18, 34]. It is also possible that restricted life-space mobility due to physical disability or disease, may diminish brain stimulation needed for maintaining cognitive skills and thus have a negative influence to cognitive functioning over time.
One of the strengths of the study was that we analyzed the association between EF and life-space mobility which has not been addressed before. Additionally, using different mobility measures, we were able to investigate which mobility indicators may explain this association. Our study included persons who were community-dwelling and from all social stratum, who did not have severe cognitive decline (Mean MMSE score: 26.2, SD 2.6). We used computer-assisted face-to-face interviews by trained interviewers at participants’ homes allowing cognitive and physical performance tests in a setting familiar to the participants.
There are also some limitations in this study that need to be acknowledged. First of all, the participants with poorer EF, or lower SPPB and MMSE scores and lower life-space mobility were more likely to drop out from the follow-up study than those with higher values. Therefore, the strength of the longitudinal association between EF and life-space mobility may have been underestimated. Second, the attrition reduced the statistical power in the longitudinal analyses. Nevertheless, the results suggest that life-space mobility may show steeper decline over time among those with lower EF. However, this needs to be confirmed in future studies. Third, self-reported walking difficulties as a measurement may under- or over-estimate true participants’ difficulties. However, self-reported walking difficulties is a widely used measure in aging research, and thus, is an established method for assessing perceived mobility difficulties that participants experience in their daily life surroundings [28]. Fourth, we were using a single test to measure executive function instead of multiple tests due to time constraints in the study protocol considering that the participants were very old. Although TMT is a widely used test and simple and easy to perform, further studies should use more detailed test batteries for a more comprehensive evaluation of executive function.
Conclusion
Better EF is associated with higher life-space mobility and poorer lower extremity performance and transportation difficulties explained the association. Poor EF may predict steeper decline in life-space mobility. Our finding lays ground to future studies on the topic.
References
Satariano WA, Guralnik JM, Jackson RJ et al (2012) Mobility and aging: new directions for public health action. Am J Public Health 102:1508–1515
Hirvensalo M, Rantanen T, Heikkinen E (2000) Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. J Am Geriatr Soc 48:493–498
Barnes LL, Wilson RS, Bienias JL et al (2007) Correlates of life space in a volunteer cohort of older adults. Exp Aging Res 33:77–93
Baker PS, Bodner EV, Allman RM (2003) Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc 51:1610–1614
Webber SC, Porter MM, Menec VH (2010) Mobility in older adults: a comprehensive framework. Gerontologist 50:443–450
Crowe M, Andel R, Wadley VG et al (2008) Life-space and cognitive decline in a community-based sample of african american and caucasian older adults. J Gerontol A Biol Sci Med Sci 63:1241–1245
Wood KM, Edwards JD, Clay OJ et al (2005) Sensory and cognitive factors influencing functional ability in older adults. Gerontology 51:131–141
Banich MT (2009) Executive function the search for an integrated account. Curr Dir Psychol Sci 18:89–94
Diamond A (2000) Close interrelation of motor development and cognitive development and of the cerebellum and prefrontal cortex. Child Dev 71:44–56
Kramer AF, Hahn S, Cohen NJ et al (1999) Ageing, fitness and neurocognitive function. Nature 400:418–419
Salthouse TA, Atkinson TM, Berish DE (2003) Executive functioning as a potential mediator of age-related cognitive decline in normal adults. J Exp Psychol: Gen 132:566
Rosso AL, Studenski SA, Chen WG et al (2013) Aging, the central nervous system, and mobility. J Gerontol A Biol Sci Med Sci 68:1379–1386
Rosano C, Studenski SA, Aizenstein HJ et al (2012) Slower gait, slower information processing and smaller prefrontal area in older adults. Age Ageing 41:58–64
Killane I, Donoghue OA, Savva GM et al (2014) Relative association of processing speed, short-term memory and sustained attention with task on gait speed: a study of community-dwelling people 50 years and older. J Gerontol A Biol Sci Med Sci 69:1407–1414
Hausdorff JM, Yogev G, Springer S et al (2005) Walking is more like catching than tapping: gait in the elderly as a complex cognitive task. Exp Brain Res 164:541–548
Portegijs E, Rantakokko M, Mikkola TM et al (2014) Association between physical performance and sense of autonomy in outdoor activities and life-space mobility in community-dwelling older people. J Am Geriatr Soc 62:615–621
Viljanen A, Mikkola TM, Rantakokko M et al (2016) The association between transportation and life-space mobility in community-dwelling older people with or without walking difficulties. J Aging Health 28:1038–1054
Anstey KJ, Wood J, Lord S et al (2005) Cognitive, sensory and physical factors enabling driving safety in older adults. Clin Psychol Rev 25:45–65
Ble A, Volpato S, Zuliani G et al (2005) Executive function correlates with walking speed in older persons: the InCHIANTI study. J Am Geriatr Soc 53:410–415
Vaughan L, Giovanello K (2010) Executive function in daily life: age-related influences of executive processes on instrumental activities of daily living. Psychol Aging 25:343
Rantanen T, Portegijs E, Viljanen A et al (2012) Individual and environmental factors underlying life space of older people—study protocol and design of a cohort study on life-space mobility in old age (LISPE). BMC Public Health 12:1018-2458-12-1018
Polku H, Mikkola TM, Rantakokko M et al (2016) Hearing and quality of life among community-dwelling older adults. J Gerontol B Psychol Sci Soc Sci. doi:10.1093/geronb/gbw045
Reitan R (1993) Wolfson D, ed. The halstead-reitan neutopsychologic test battery: theory and clinical interpretation. Neuropsychology Press, Tucson
Lezak M (ed) (1995) Neuropsychological assessment. 3rd edition ed. Oxford University Press, Oxford
Bowie CR, Harvey PD (2006) Administration and interpretation of the trail making test. Nature protocols 1:2277–2281
Drane DL, Yuspeh RL, Huthwaite JS et al (2002) Demographic characteristics and normative observations for derived-trail making test indices. Neuropsychiatry Neuropsychol Behav Neurol 15:39–43
Portegijs E, Iwarsson S, Rantakokko M et al (2014) Life-space mobility assessment in older people in finland; measurement properties in winter and spring. BMC Res Notes 7:323-0500-7-323
Guralnik JM, Simonsick EM, Ferrucci L et al (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:M85-94
Mänty M (2007) Iäkkäiden henkilöiden kaatumistapaturmat: Opas kaatumisten ja murtumien ehkäisyyn. National Public Health Institute
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Liang K, Zeger SL (1986) Longitudinal data analysis using generalized linear models. Biometrika 73:13–22
James BD, Boyle PA, Buchman AS et al (2011) Life space and risk of alzheimer disease, mild cognitive impairment, and cognitive decline in old age. Am J Geriatric Psychiatry 19:961–969
Seidler RD, Bernard JA, Burutolu TB et al (2010) Motor control and aging: Links to age-related brain structural, functional, and biochemical effects. Neurosci Biobeh Rev 34:721–733
Anstey KJ, Horswill MS, Wood JM et al (2012) The role of cognitive and visual abilities as predictors in the multifactorial model of driving safety. Accid Anal Prev 45:766–774
Acknowledgements
This study was supported by the Academy of Finland: the Future of Living and Housing Program ASU-LIVE; Grant number 255403 to [TR], number 263729 to [AV]; number 285747 to [MR]; numbers 129369, 129907, 135072, 129255 and 126775 to [JGE] and number 257239 to [MBvB]; Finnish Ministry of Education and Culture to [TR], [MR] and [EP]. TP-C was supported by Yrjö Jahnsson Foundation and Juho Vainio Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Ethical approval
The LISPE study and the Hearing, Cognition and Wellbeing sub-study both comply with the principles of good scientific conduct and good clinical practice in all aspects of the Declaration of Helsinki, and were approved by the Ethical Committee of the University of Jyväskylä
Informed consent
Informed consent All participants gave a written informed consent.
Rights and permissions
About this article
Cite this article
Poranen-Clark, T., von Bonsdorff, M.B., Rantakokko, M. et al. Executive function and life-space mobility in old age. Aging Clin Exp Res 30, 145–151 (2018). https://doi.org/10.1007/s40520-017-0762-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-017-0762-3