Abstract
Physical frailty (PF) and sarcopenia are major health issues in geriatric populations, given their high prevalence and association with several adverse outcomes. Nevertheless, the lack of an univocal operational definition for the two conditions has so far hampered their clinical implementation. Existing definitional ambiguities of PF and sarcopenia, together with their complex underlying pathophysiology, also account for the absence of robust biomarkers that can be used for screening, diagnostic and/or prognostication purposes. This review provides an overview of currently available biological markers for PF and sarcopenia, as well as a critical appraisal of strengths and weaknesses of traditional procedures for biomarker development in the field. A novel approach for biomarker identification and validation, based on multivariate methodologies, is also discussed. This strategy relies on the multidimensional modeling of complementary biomarkers to cope with the phenotypical and pathophysiological complexity of PF and sarcopenia. Biomarkers identified through the implementation of multivariate strategies may be used to support the detection of the two conditions, track their progression over time or in response to interventions, and reveal the onset of complications (e.g., mobility disability) at a very early stage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sarcopenia, the age-related decline in skeletal muscle mass and function, is a major health issue in geriatric medicine, given its association with a wide spectrum of negative health outcomes, including disability, loss of independence, institutionalization and mortality [1]. In addition, sarcopenia has been proposed to represent the biological substrate of the physical function impairment that characterizes physical frailty (PF) [2].
Although the theoretical foundations of sarcopenia and PF are widely acknowledged, their clinical implementation is still hampered by the lack of an univocal operational definition [3]. This is also reflected by the absence of robust biomarkers that may be used to support the diagnosis, facilitate the tracking of the conditions over time, and monitor their response to interventions [4].
This review summarizes the current state of knowledge regarding biomarkers for PF and sarcopenia, and presents a possible novel approach for biomarker identification based on multivariate methodology.
Biomarkers for physical frailty and sarcopenia: where are we?
As indicated in the position statement of the International Working Group on Sarcopenia [5], several imaging, functional, and biological parameters may be used as biomarkers for PF and sarcopenia. With respect to imaging markers, magnetic resonance imaging (MRI), computed tomography (CT), and dual energy X-ray absorptiometry (DXA) provide an objective and sufficiently reliable estimation of muscle mass [5]. However, such imaging techniques, especially MRI and CT, are rather expensive and technically difficult and are only available in well-equipped medical centers. Other methods for muscle mass estimation, such as peripheral quantitative CT, electrical impedance myography, ultrasonography, bioelectrical impedance analysis (BIA), neutron activation, creatinine excretion, and anthropometry, are either not sufficiently standardized or inaccurate [5].
Although originally based on the sole estimation of muscle quantity [6], it is now clear that the adequate framing of sarcopenia requires the simultaneous assessment of multiple domains [7]. Indeed, the loss of muscle mass, albeit being associated with strength decline, shows distinct trajectories of changes over time relative to those in muscle function [8]. Furthermore, maintaining or even gaining muscle mass may not protect against strength loss in old age [8]. On the other hand, improvements in muscle strength via behavioral [9] or pharmacological interventions [10] are not necessarily associated with increases in muscle quantity.
Given these considerations, the objective assessment of muscle strength and function is an indispensable requisite for identifying PF and sarcopenia. The most popular tools include the handgrip strength test [11], the short physical performance battery (SPPB) [12], the usual gait speed [13], and the lower extremity muscle power [14]. In particular, the combined assessment of muscle mass and the three domains explored by the SPPB (i.e., balance, walking speed, and strength) allows a practical conceptualization of PF and sarcopenia, easily implementable in research and clinical settings [15].
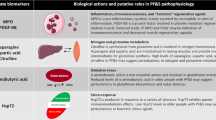
Several muscle-specific cellular processes have been proposed to play a role in the pathogenesis of PF and sarcopenia, including alterations in mitochondrial function, redox imbalance, defects in protein metabolism, acceleration of myonuclear apoptosis, and deregulation of autophagy (reviewed in [16]). The dissection of these and other pathways, besides identifying a vast array of potential biomarkers for muscle atrophy and dysfunction, has also contributed to advancing our understanding of PF and sarcopenia pathophysiology. However, the invasive procedure required to access muscle tissue (biopsy) as well as the complex and expensive analyses necessary to interrogate specific cellular pathways, hampers the clinical applicability of tissular biomarkers [17].
With regard to circulating biomolecules, numerous mediators linked to systemic inflammation, hormonal status, and redox homeostasis have been associated with muscle atrophy and dysfunction [5]. However, they are not specific to muscle and their levels may, therefore, be altered in a variety of conditions unrelated to PF and sarcopenia.
In recent years, novel circulating mediators have been identified that are more closely related to muscle pathophysiology. For instance, plasma concentrations of procollagen type III N-terminal peptide (P3NP), a fragment released during cleavage of procollagen type III to generate collagen III, have been proposed as a marker for muscle remodeling induced by exercise training [18] or pharmacological interventions [19, 20]. However, P3NP seems to be associated with muscle mass in older women only [21], therefore, restricting the use of this molecule as a biomarker for muscle atrophy to the female gender.
The circulating C-terminal agrin fragment (CAF) has recently emerged as a potential marker for skeletal muscle mass and function [18, 22–26]. Agrin is motor neuron-derived proteoglycan implicated in the assembly and stabilization of the neuromuscular junction (NMJ). Agrin is degraded at the NMJ by neurotrypsin to produce a C-terminal 22-kDa fragment (CAF) that is released into the circulation [27]. In laboratory rodents, excess agrin cleavage causes NMJ disruption, muscle fiber denervation, and early development of sarcopenia [28]. Elevated serum CAF levels have been associated with sarcopenia in community-dwelling elderly as well as in older hip-fractured patients [18, 22–26]. On the other hand, the determination of serum CAF levels shows good sensitivity, but low specificity for detecting muscle wasting in patients with chronic heart failure [29]. Finally, serum CAF has recently been proposed as a biomarker for muscle loss after acute stroke [30].
Plasma extracellular heat shock protein 72 (eHsp72) has been proposed as an additional sarcopenia biomarker [31]. In a sample of 665 community-living men and women aged 65–96 years, plasma eHsp72 levels were inversely related to muscle mass, handgrip strength and 5-meter gait speed. The mechanistic link between eHsp72 and sarcopenia is unclear, although it may involve systemic inflammation and neuronal apoptosis [32, 33].
Circulating skeletal muscle-specific troponin T (sTnT) may be used as a marker for sarcomere dysfunction and muscle wasting [34]. TnT, besides being involved in the assembly of thin filaments [35], also functions as the tropomyosin-binding subunit of the troponin complex [36]. Within sarcomeres, sTnT and tropomyosin regulate cross-bridge cycling and, hence, contraction via calcium binding [36]. Under physiologic conditions, only trace amounts of sTnT can be retrieved in the circulation, in relation to muscle tissue turnover. Serum levels of troponins, including sTnT, are increased following skeletal muscle injury as well as in muscular dystrophies and neuromuscular disorders [37]. Notably, in older community-dwellers, 10-week strength training elicited a substantial decrease in serum sTnT levels, paralleled by improvements in physical performance and muscle strength [34]. This observation, albeit preliminary, suggests that circulating sTnT may be used as an index for assessing the effect of physical exercise on muscle function [38].
The intimate relationship among muscle loss, physical function impairment and the aging process has led researchers hypothesize that biomarkers of organismal aging may be able to capture the complexity of PF and sarcopenia [39]. Indeed, an association was reported between sarcopenia and the length of telomeres in peripheral blood mononuclear cells (PBMCs) in geriatric outpatients [39]. The association was independent of gender, lifestyle habits, and comorbidity burden. In contrast, no significant associations were determined between PBMC telomere length and measures of physical performance or the frailty status. Similarly, PBMC telomere length was unrelated to PF in a cohort of community-living elderly aged 85+ years [40].
As an attempt to overcome the limitations of currently available imaging techniques, a novel method for muscle mass quantification has recently been developed, based on creatine (methyl-d3) dilution (D3-creatine) measured by enrichment of urine D3-creatinine [41]. The method is able to accurately quantify whole-body muscle mass in humans [41] and track longitudinal changes in total muscle mass in growing rats [42]. Yet, the D3-creatine dilution method only allows for the quantitative assessment of sarcopenia, with no information on muscle strength or function. Furthermore, the detection of D3-creatine relies on isotope ratio mass spectrometry or liquid chromatography/tandem mass spectrometry technologies, which precludes, at least at present, the large-scale implementation of the methodology.
Multivariate biomarker discovery: moving the field forward
Given the complex phenotypical and pathophysiological features of PF and sarcopenia, it is highly likely that there might not be one single biomarker, whichever class it belongs to, that can adequately frame these conditions. Indeed, it is well possible that distinct pathogenic processes may be responsible for the appearance of a given phenotype (e.g., muscle atrophy and weakness). A single biomarker may, therefore, not be equally valid from person to person. What is more, PF and sarcopenia develop over years and distinct pathogenic processes may predominate depending on the stage and severity of the conditions. This implies that specific biomarkers may be relevant only within limited timeframes. Last but not least, comorbidities and chronic exposure to several medications may interfere with the progression of PF and sarcopenia, by triggering or suppressing specific pathogenic pathways.
These considerations call for a shift of paradigm in the field of PF and sarcopenia biomarkers, prompting the transition from the “one-fits-all” paradigm to the multidimensional modeling of a panel of complementary biomarkers [4]. The adoption of multivariate methodologies may optimally serve to overcome the limitations that afflict presently available biomarkers for PF and sarcopenia.
Depending on the size of the investigated cohort, the knowledge of the subjects and the study design, different strategies may be undertaken, involving an increasing degree of complexity. When the number of participants is too small to formulate reliable predictions and/or the aim of the study is the phenomenological characterization of a condition, an exploratory approach is recommended. In such cases, principal component analysis (PCA) is the method of election [42]. PCA allows for the straightforward representation of the most relevant features of data onto a low-dimensional subspace, and the corresponding interpretation of the observed variation in terms of the variables that mostly contribute to the model.
When data are collected according to a crossover or nested experimental design, the exploratory power of PCA may be coupled with approaches that can be thought of as generalizations of the classical analysis of variance (ANOVA) [43–45]. For instance, depending on the design, the identification of multivariate contributions of the investigated factors and their interactions may be accomplished through ANOVA-simultaneous component analysis (ASCA [44]) or multilevel simultaneous component analysis (MSCA [45]). In these approaches, the data matrix is decomposed according to the underlying design into a series of matrices, each accounting for the contribution of a controlled source of variability (factor or interaction) and then interpretation of the observed effect is accomplished through PCA of individual matrices.
When the characteristics of the study and, in particular, the dimension of the cohort are suitable, biomarker discovery can be carried out through the construction and validation of predictive (classification) models. In this context, one valid tool is the partial least squares discriminant analysis (PLS-DA) [46–48]. PLS-DA couples the reliability and accuracy of prediction with the possibility of a low-dimensional representation of data. This, in turn, allows for an easier and more straightforward interpretation of results.
A PLS-DA approach was recently used to characterize the patterns of inflammatory biomarkers associated with varying levels of physical performance in a sample of older community-dwellers [49]. For the purpose of the study, a panel of 14 circulating inflammatory mediators was measured via a multiplex immunoassay. The PLS-DA analysis revealed that participants with gait speed above the critical threshold of 0.8 m s− 1 showed higher circulating levels of P–selectin, interferon γ and granulocyte macrophage colony-stimulating factor. Higher levels of interleukin 8, myeloperoxidase and tumor necrosis factor α defined the inflammatory profile of older persons walking slower than 0.8 m s− 1. Double cross-validation confirmed the reliability of the PLS-DA model and the obtained results. Using a similar approach, we also identified specific clusters of imaging, functional and biochemical alterations in young and older adults [50].
Multivariate approaches may also be used to model the overall homeostatic condition of a person by monitoring how all measured parameters co-vary when nothing anomalous is occurring [51]. The longitudinal analysis of individual time trajectories could help detect the possible onset of a critical condition (e.g., mobility disability) at an early stage and prompt the timely implementation of specific interventions.
Conclusion
Over the years, several imaging, functional and biological parameters have been proposed as biomarkers for PF and sarcopenia. However, due to complex phenotypical and pathophysiological nature of the conditions, none of available biomarkers provides a comprehensive picture of PF and sarcopenia. Existing limitations may be overcome through the implementation of multidimensional/multivariate methodologies for the simultaneous modeling of complementary biomarkers. Indeed, the longitudinal implementation of such an innovative strategy could allow for the tracking of health status over time, the early detection of deviations in health trajectories, and the monitoring of response to treatments. This knowledge, in turn, would assist in developing more comprehensive and patient-tailored interventions [52, 53].
References
Hirani V, Blyth F, Naganathan V, Le Couteur DG, Seibel MJ, Waite LM, Handelsman DJ, Cumming RG (2015) Sarcopenia is associated with incident disability, institutionalization, and mortality in community-dwelling older men: The Concord Health and Ageing in Men project. J Am Med Dir Assoc 16:607–613. doi:10.1016/j.jamda.2015.02.006
Landi F, Calvani R, Cesari M, Tosato M, Martone AM, Bernabei R, Onder G, Marzetti E (2015) Sarcopenia as the biological substrate of physical frailty. Clin Geriatr Med 31:367–374. doi:10.1016/j.cger.2015.04.005
Cesari M, Landi F, Vellas B, Bernabei R, Marzetti E (2014) Sarcopenia and physical frailty: two sides of the same coin. Front Aging Neurosci 6:192. doi:10.3389/fnagi.2014.00192
Calvani R, Marini F, Cesari M, Tosato M, Anker SD, von Haehling S, Miller RR, Bernabei R, Landi F, Marzetti E; for the SPRINTT consortium (2015) Biomarkers for physical frailty and sarcopenia: State of the science and future developments. J Cachexia Sarcopenia Muscle 6:278–286. doi:10.1002/jcsm.12051
Cesari M, Fielding RA, Pahor M, Goodpaster B, Hellerstein M, van Kan GA, Anker SD, Rutkove S, Vrijbloed JW, Isaac M, Rolland Y, M’rini C, Aubertin-Leheudre M, Cedarbaum JM, Zamboni M, Sieber CC, Laurent D, Evans WJ, Roubenoff R, Morley JE, Vellas B (2012) Biomarkers of sarcopenia in clinical trials-recommendations from the International Working Group on Sarcopenia. J Cachexia Sarcopenia Muscle 3:181–190. doi:10.1007/s13539-012-0078-2
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147:755–763
Marzetti E (2012) Imaging, functional and biological markers for sarcopenia: the pursuit of the golden ratio. J Frailty. Aging 1:97–98
Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, Simonsick EM, Tylavsky FA, Visser M, Newman AB (2006) The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci 61:1059–1064
Reid KF, Callahan DM, Carabello RJ, Phillips EM, Frontera WR, Fielding RA (2008) Lower extremity power training in elderly subjects with mobility limitations: a randomized controlled trial. Aging Clin Exp Res 20:337–343. doi:10.1007/BF03324865
Carter CS, Giovannini S, Seo DO, DuPree J, Morgan D, Chung HY, Lees H, Daniels M, Hubbard GB, Lee S, Ikeno Y, Foster TC, Buford TW, Marzetti E (2011) Differential effects of enalapril and losartan on body composition and indices of muscle quality in aged male Fischer 344 × Brown Norway rats. Age (Dordr) 33:167–183. doi:10.1007/s11357-010-9196-y
Rantanen T, Guralnik JM, Foley D, Masaki K, Leveille S, Curb JD, White L (1999) Midlife hand grip strength as a predictor of old age disability. JAMA 281:558–560. doi:10.1001/jama.281.6.558
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:M85–M94. doi:10.1093/geronj/49.2.M85
Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, Brach J, Chandler J, Cawthon P, Connor EB, Nevitt M, Visser M, Kritchevsky S, Badinelli S, Harris T, Newman AB, Cauley J, Ferrucci L, Guralnik J (2011) Gait speed and survival in older adults. JAMA 305:50–58. doi:10.1001/jama.2010.1923
Bassey EJ, Fiatarone MA, O’Neill EF, Kelly M, Evans WJ, Lipsitz LA (1992) Leg extensor power and functional performance in very old men and women. Clin Sci (Lond) 82:321–327
Marzetti E, Calvani R, Cesari M, Tosato M, Cherubini A, Di Bari M, Pahor M, Savera G, Collamati A, D’Angelo E, Bernabei R, Landi F (2016) Operationalization of the physical frailty & sarcopenia syndrome: rationale and clinical implementation. Transl Med UniSa 13:29–32
Marzetti E, Lees HA, Wohlgemuth SE, Leeuwenburgh C (2009) Sarcopenia of aging: underlying cellular mechanisms and protection by calorie restriction. Biofactors 35:28–35. doi:10.1002/biof.5
Marzetti E, Calvani R, Cesari M, Buford TW, Lorenzi M, Behnke BJ, Leeuwenburgh C (2013) Mitochondrial dysfunction and sarcopenia of aging: from signaling pathways to clinical trials. Int J Biochem Cell Biol 45:2288–2301. doi:10.1016/j.biocel.2013.06.024
Fragala MS, Jajtner AR, Beyer KS, Townsend JR, Emerson NS, Scanlon TC, Oliveira LP, Hoffman JR, Stout JR (2014) Biomarkers of muscle quality: N-terminal propeptide of type III procollagen and C-terminal agrin fragment responses to resistance exercise training in older adults. J Cachexia Sarcopenia Muscle 5:139–148. doi:10.1007/s13539-013-0120-z
Bhasin S, He EJ, Kawakubo M, Schroeder ET, Yarasheski K, Opiteck GJ, Reicin A, Chen F, Lam R, Tsou JA, Castaneda-Sceppa C, Binder EF, Azen SP, Sattler FR (2009) N-terminal propeptide of type III procollagen as a biomarker of anabolic response to recombinant human GH and testosterone. J Clin Endocrinol Metab 94:4224–4233. doi:10.1210/jc.2009-1434
Chen F, Lam R, Shaywitz D, Hendrickson RC, Opiteck GJ, Wishengrad D, Liaw A, Song Q, Stewart AJ, Cummings CE, Beals C, Yarasheski KE, Reicin A, Ruddy M, Hu X, Yates NA, Menetski J, Herman GA (2011) Evaluation of early biomarkers of muscle anabolic response to testosterone. J Cachexia Sarcopenia Muscle 2:45–56. doi:10.1007/s13539-011-0021-y
Berry SD, Ramachandran VS, Cawthon PM, Gona P, McLean RR, Cupples LA, Kiel DP (2013) Procollagen type III N-terminal peptide (P3NP) and lean mass: a cross-sectional study. J Frailty Aging 2:129–134
Hettwer S, Dahinden P, Kucsera S, Farina C, Ahmed S, Fariello R, Drey M, Sieber CC, Vrijbloed JW (2013) Elevated levels of a C-terminal agrin fragment identifies a new subset of sarcopenia patients. Exp Gerontol 48:69–75. doi:10.1016/j.exger.2012.03.002
Drey M, Sieber CC, Bauer JM, Uter W, Dahinden P, Fariello RG, Vrijbloed JW (2013) C-terminal Agrin Fragment as a potential marker for sarcopenia caused by degeneration of the neuromuscular junction. Exp Gerontol 48:76–80. doi:10.1016/j.exger.2012.05.021
Stout JR, Fragala MS, Hoffman JR, Robinson EH, Mccormack WP, Townsend JR, Jatjner AR, Emerson NS, Oliveira LP, Fukuda DH (2015) C-terminal agrin fragment is inversely related to neuromuscular fatigue in older men. Muscle Nerve 51:132–133. doi:10.1002/mus.24443
Marzetti E, Calvani R, Lorenzi M, Marini F, D’Angelo E, Martone AM, Celi M, Tosato M, Bernabei R, Landi F (2014) Serum levels of C-terminal agrin fragment (CAF) are associated with sarcopenia in older hip fractured patients. Exp Gerontol 60C:79–82. doi:10.1016/j.exger.2014.10.003
Landi F, Calvani R, Lorenzi M, Martone AM, Tosato M, Drey M, D’Angelo E, Capoluongo E, Russo A, Bernabei R, Onder G, Marzetti E (2016) Serum levels of C-terminal agrin fragment (CAF) are associated with sarcopenia in older multimorbid community-dwellers: results from the ilSIRENTE study. Exp Gerontol 79:31–36
Stephan A, Mateos JM, Kozlov SV, Cinelli P, Kistler AD, Hettwer S, Rülicke T, Streit P, Kunz B, Sonderegger P (2008) Neurotrypsin cleaves agrin locally at the synapse. FASEB J 22:1861–1873. doi:10.1096/fj.07-100008
Butikofer L, Zurlinden A, Bolliger MF, Kunz B, Sonderegger P (2011) Destabilization of the neuromuscular junction by proteolytic cleavage of agrin results in precocious sarcopenia. FASEB J 25:4378–4393. doi:10.1096/fj.11-191262
Steinbeck L, Ebner N, Valentova M, Bekfani T, Elsner S, Dahinden P, Hettwer S, Scherbakov N, Schefold JC, Sandek A, Springer J, Doehner W, Anker SD, von Haehling S (2015) Detection of muscle wasting in patients with chronic heart failure using C-terminal agrin fragment: Results from the Studies Investigating Co-morbidities Aggravating Heart Failure (SICA-HF). Eur J Heart Fail 17:1283–1293. doi:10.1002/ejhf.400
Scherbakov N, Knops M, Ebner N, Valentova M, Sandek A, Grittner U, Dahinden P, Hettwer S, Schefold JC, von Haehling S, Anker SD, Joebges M, Doehner W (2016) Evaluation of C-terminal Agrin Fragment as a marker of muscle wasting in patients after acute stroke during early rehabilitation. J Cachexia Sarcopenia Muscle 7:60–67. doi:10.1002/jcsm.12068
Ogawa K, Kim HK, Shimizu T, Abe S, Shiga Y, Calderwood SK (2012) Plasma heat shock protein 72 as a biomarker of sarcopenia in elderly people. Cell Stress Chaperones 17:349–359. doi:10.1007/s12192-011-0310-6
Asea A, Kraeft SK, Kurt-Jones EA, Stevenson MA, Chen LB, Finberg RW, Koo GC, Calderwood SK (2000) HSP70 stimulates cytokine production through a CD14-dependant pathway, demonstrating its dual role as a chaperone and cytokine. Nat Med 6:435–442. doi:10.1038/74697
Robinson MB, Tidwell JL, Gould T, Taylor AR, Newbern JM, Graves J, Tytell M, Milligan CE (2005) Extracellular heat shock protein 70: a critical component for motoneuron survival. J Neurosci 25:9735–9745. doi:10.1523/JNEUROSCI
Abreu EL, Cheng AL, Kelly PJ, Chertoff K, Brotto L, Griffith E, Kinder G, Uridge T, Zachow R, Brotto M (2014) Skeletal muscle troponin as a novel biomarker to enhance assessment of the impact of strength training on fall prevention in the older adults. Nurs Res 63:75–82. doi:10.1097/NNR.0000000000000018
Hinkle A, Goranson A, Butters CA, Tobacman LS (1999) Roles for the troponin tail domain in thin filament assembly and regulation. A deletional study of cardiac troponin T. J Biol Chem 274:7157–7164. doi:10.1074/jbc.274.11.7157
Zot AS, Potter JD (1987) Structural aspects of troponin-tropomyosin regulation of skeletal muscle contraction. Annu Rev Biophys. Biophys Chem 16:535–559. doi:10.1146/annurev.bb.16.060187.002535
Huxley AF, Niedergerke R (1954) Structural changes in muscle during contraction: interference microscopy of living muscle fibres. Nature 173:971–973. doi:10.1038/173971a0
Kalinkovich A, Livshits G (2015) Sarcopenia - The search for emerging biomarkers. Ageing Res Rev 22:58–71. doi:10.1016/j.arr.2015.05.001
Marzetti E, Lorenzi M, Antocicco M, Bonassi S, Celi M, Mastropaolo S, Settanni S, Valdiglesias V, Landi F, Bernabei R, Onder G (2014) Shorter telomeres in peripheral blood mononuclear cells from older persons with sarcopenia: results from an exploratory study. Front Aging Neurosci 6:233. doi:10.3389/fnagi.2014.00233
Collerton J, Martin-Ruiz C, Davies K, Hilkens CM, Isaacs J, Kolenda C, Parker C, Dunn M, Catt M, Jagger C, von Zglinicki T, Kirkwood TB (2012) Frailty and the role of inflammation, immunosenescence and cellular ageing in the very old: cross-sectional findings from the Newcastle 85 + Study. Mech Ageing Dev 133:456–466. doi:10.1016/j.mad.2012.05.005
Clark RV, Walker AC, O’Connor-Semmes RL, Leonard MS, Miller RR, Stimpson SA, Turner SM, Ravussin E, Cefalu WT, Hellerstein MK, Evans WJ (2014) Total body skeletal muscle mass: estimation by creatine (methyl-d3) dilution in humans. J Appl Physiol 116(1985):1605–1613. doi:10.1152/japplphysiol.00045.2014
Stimpson SA, Leonard MS, Clifton LG, Poole JC, Turner SM, Shearer TW, Remlinger KS, Clark RV, Hellerstein MK, Evans WJ (2013) Longitudinal changes in total body creatine pool size and skeletal muscle mass using the D-creatine dilution method. J Cachexia Sarcopenia Muscle (Epub ahead of print). doi:10.1007/s13539-013-0110-1
Bro R, Smilde AK (2014) Principal component analysis. Anal Meth 6:2812–2831. doi:10.1039/c3ay41907j
Smilde AK, Jansen JJ, Hoefsloot HC, Lamers RJ, van der Greef J, Timmerman ME (2005) ANOVA-simultaneous component analysis (ASCA): a new tool for analyzing designed metabolomics data. Bioinformatics 21:3043–3048. doi:10.1093/bioinformatics/bti476
Jansen JJ, Hoefsloot HC, van der Greef J, Timmerman ME, Smilde AK (2005) Multilevel component analysis of time-resolved metabolic fingerprinting. Anal Chim Acta 530:173–183. doi:10.1016/j.aca.2004.09.074
Marini F, de Beer D, Joubert E, Walczak B (2015) Analysis of variance of designed chromatographic data sets: The analysis of variance-target projection approach. J Chromatogr A 1405:94–102. doi:10.1016/j.chroma.2015.05.060
Bevilacqua M, Bucci R, Magrì AL, Magrì R, Nescatelli R, Marini F (2013) Classification and class-modeling. In: Marini F (ed) Chemometrics in food chemistry. Elsevier, Oxford, pp 171–233. doi:10.1016/B978-0-444-59528-7.00005-3
Szymanska E, Saccenti E, Smilde AK, Westerhuis JA (2012) Double-check: validation of diagnostic statistics for PLS-DA models in metabolomics studies. Metabolomics 8:3–16. doi:10.1007/s11306-011-0330-3
Marzetti E, Landi F, Marini F, Cesari M, Buford TW, Manini TM, Onder G, Pahor M, Bernabei R, Leeuwenburgh C, Calvani R (2014) Patterns of circulating inflammatory biomarkers in older persons with varying levels of physical performance: a Partial Least Squares-Discriminant Analysis (PLS-DA) approach. Front Med 1:27. doi:10.3389/fmed.2014.00027
Calvani R, Marini F, Cesari M, Manini TM, Buford TW, Pahor M, Leeuwenburgh C, Bernabei R, Landi F, Marzetti E (2016) Systemic inflammation, body composition, and physical performance in old community-dwellers. J Cachexia Sarcopenia Muscle (Epub ahead of print). doi:10.1002/jcsm.12134
Kourti T, MacGregor JF (2014) Process analysis, monitoring and diagnosis, using multivariate projection methods. Chemometr Intell Lab Syst 28:3–21. doi:10.1016/j.saa.2013.02.018
Marzetti E, Sanna T, Calvani R, Bernabei R, Landi F, Cesari M (2016) Brand new medicine for an older society. J Am Med Dir Assoc 17:558–559. doi:10.1016/j.jamda.2016.02.024
Cesari M, Marzetti E, Thiem U, Pérez-Zepeda MU, Abellan Van Kan G, Landi F, Petrovic M, Cherubini A, Bernabei R (2016) The geriatric management of frailty as paradigm of “The end of the disease era”. Eur J Intern Med 31:11–14. doi:10.1016/j.ejim.2016.03.005
Acknowledgments
This work was funded by a grant from the Innovative Medicines Initiative–Joint Undertaking (IMI–JU 115621). The work was also partly supported by the “Centro Studi Achille e Linda Lorenzon” (E.M., R.C.), Fondazione Roma (NCDs Call for Proposals 2013; A.P., E.M., R.C.), and intramural research grants from the Catholic University of the Sacred Heart (D3.2 2013 and D3.2 2015; E.M., F.L., M.T., R.C.).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors of this work, with the exception of Anna Picca and Federico Marini, are partners of the SPRINTT Consortium, which is partly funded by the European Federation of Pharmaceutical Industries and Associations (EFPIA). E.M. served as a consultant for Huron Consulting Group, Genactis, and Novartis. M.C. served as a consultant for and/or received honoraria for scientific presentations from Nestlé. S.A. and S.v.H. received consultant honoraria from Thermo Fisher Scientific, Solartium Dietetics, Professional Dietetics, and Pfizer.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Rights and permissions
About this article
Cite this article
Calvani, R., Marini, F., Cesari, M. et al. Biomarkers for physical frailty and sarcopenia. Aging Clin Exp Res 29, 29–34 (2017). https://doi.org/10.1007/s40520-016-0708-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-016-0708-1