Abstract
Background and aims
High levels of inflammatory markers shortly after an ischemic stroke are associated with a worse prognosis. Whether inflammatory markers predict long-term mortality in stroke-survivors is less clear. We examined whether a persisting inflammatory response (levels of inflammatory markers >1 year after the stroke event) was associated with long-term mortality.
Methods
We recruited participants from the Tromsø Study, Norway, in a nested case–control design. At baseline in 1997, white blood cell count (WBC), serum levels of fibrinogen, interleukin 6 (IL-6) and high sensitive C-reactive protein (hs-CRP) were analysed in 187 stroke-survivors, a median of 7.0 years (range 1–43) after the first-ever ischemic stroke, and in 243 stroke-free subjects. Cox proportional hazard regression model was used to examine whether inflammatory markers predicted all-cause mortality in both groups from 1997 to 2013.
Results
During an average of 16 years follow-up, 117 (62.5 %) stroke-survivors and 107 (44.0 %) stroke-free subjects deceased (p for differences 0.005). In stroke-survivors, fibrinogen and log IL-6 predicted all-cause mortality after adjustment for age, sex, BMI, smoking, Frenchay activity index, comorbidity and use of statins (HRs 1.26; 9 5 % CI 1.05–1.51 and 2.02; 95 % CI 1.12–3.64, respectively). In stroke-free subjects log hs-CRP predicted all-cause mortality after additionally accounting for levels of cholesterol, blood pressure and use of blood pressure lowering drugs (HR 1.95; 95 % CI 1.26–2.99).
Conclusions
Fibrinogen and IL-6 were independent predictors of mortality in long-term stroke-survivors, whereas elevated hs-CRP predicted mortality in stroke-free subjects. Mortality risk prediction in stroke-survivors differed from that of stroke-free subjects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is a leading cause of death worldwide, and stroke-survivors are at increased risk of death compared to stroke-free subjects [1]. Age, comorbidity, severity and location of the cerebral tissue injury, post-stroke infection and other complications are associated with increased mortality [2, 3]. High levels of inflammatory markers shortly after a stroke are associated with increased in-hospital and short-term mortality [4, 5]. Whether the levels of inflammatory markers sampled more than 1 year post-stroke predict long-term mortality among stroke survivors is less clear.
In prospective population based studies, elevated levels of high sensitive C-reactive protein (hs-CRP), and interleukin 6 (IL-6) predict first-ever ischemic stroke in healthy subjects [6, 7]. Increased levels of fibrinogen, IL-6 and hs-CRP are associated with mortality among elderly subjects [6, 8–10]. Stroke related low-grade persistent inflammation is poorly examined, and in particular the inflammatory markers’ ability to predict long-term prognosis [11]. Elevated post-stroke levels of fibrinogen lasting for 1 year was associated with an increased mortality [11], but the long-term prognostic relevance of inflammatory markers is unknown.
Most previous studies have recruited patients and collected blood samples shortly after the stroke, when inflammatory markers are high due to the acute phase reaction [12–14]. Acute stroke patients with increased levels of inflammatory markers at admission or at discharge have poor outcome, in terms of recurrence, complications and mortality, probably reflecting the severity and extent of the acute stroke event [8, 15, 16]. In addition, elevated baseline CRP is associated with an unfavourable long-term functional outcome [17].
In this study, we wanted to examine whether there is a link of a persisting inflammatory response, using baseline samples collected more than 1 year after the stroke event, with the long-term stroke mortality during 16 years follow-up. We hypothesized that long-term stroke-survivors experience persistently elevated levels of the inflammatory markers as white blood cell count (WBC), fibrinogen, IL-6 and hs-CRP, and that biomarkers predict mortality.
Materials and methods
Participants
The Tromsø Study is a population-based prospective study of health issues and chronic diseases consisting of six surveys referred to as Tromsø 1-6, conducted from 1974 to 2008 [18]. At Tromsø 4 in 1994-95, a total of 27,159 women and men over 24 years of age participated (Fig. 1 Flow chart of the study population). Participants in The Tromsø study are independently living individuals. In a nested case-controls design, we recruited participants from the Tromsø 4, and invited them for a re-examination in 1997, which is defined as the baseline of the current study. Of 418 subjects with a self-reported stroke in Tromsø 4, five moved and 51 died during the next 3 years, 362 were invited to re-examination in 1997, and 269 of them attended. A control subject who did not report a history of stroke was randomly selected from the same Tromsø 4 population and matched for each of the 361 stroke-survivors, with age (±2 years) and sex used as matching criteria, and 262 controls were re-examined. A specialist in geriatric medicine validated the medical history of stroke and all information from the hospital medical records, and performed an interview and clinical examination of all participants. The stroke diagnosis was supported by changes on cerebral CT scans, which were assessed by a radiologist, and 221 were verified as stroke-survivors. After excluding subarachnoid haemorrhage (n = 20) and intracerebral haemorrhage (n = 14), 187 ischemic stroke-survivors were included. Of 262 re-examined stroke-free subjects, 243 were verified stroke-free and included. Median 7.0 (range 1–43) years elapsed from first-ever ischemic stroke to inclusion. Further details on the recruitment process, response and attendance rate, stroke definitions and criteria, and the validity of a self-reported stroke have been reported [19]. The stroke-survivors who attended this study had modest functional impairment. None of them was wheelchair dependent, 10 % were unable to raise from a chair without using their arms, 3.6 % had problem with verbal communication, and 1 % were unable to perform finger tapping. None of the participants had a permanent urinary catheter, and none had any clinical signs of acute infection or inflammation at the time of inclusion. The Tromsø Study was approved by the Data Inspectorate of Norway and the Regional Committee of Medical and Health Research Ethics. All participants gave written informed consent.
Variables
At baseline in 1997 data were collected using questionnaires, which included information on previous myocardial infarction and stroke, present diabetes mellitus (yes/no), use of blood-pressure and lipid-lowering drugs (yes/no), acetylsalicylate and current smoking (yes/no). Outdoor physical, social and domestic indoor activities were assessed using the Frenchay Activity Index [20]. This is a marker of the daily life activity, which can be considered as a surrogate marker of disability. Height, weight and blood pressure were measured at baseline. Body mass index (BMI) was calculated as weight divided by the square of height (kg/m2).
The blood samples were drawn at baseline in 1997 and stored at −70 °C until analysis. Fibrinogen was assayed in 1998 with a clothing method in a STA-compact analyzer (Diagnostica Stago, Asnieres, France); the detection limit was 0.6 g/l and the coefficient of variation (CV) was 4.0 %. High sensitive CRP and IL-6 were assayed in 2001. IL-6 was analysed with an ELISA (Quantikine Immunoassay) with detection limit of 0.70 µg/l and CV 4.2 %, from R&D Systems (Abingdon, UK), hs-CRP was assayed by a particle-enhanced immuno-turbidimetric assay from Roche Diagnostics (Mannheim, Germany), with detection limit of 0.175 mg/l and the CV was 4.0 %.
The endpoint data concerning all-cause mortality was collected from electronic hospital medical records and death certificates on all participants during 16 years, from August 1997 until May 1st 2013. In Norway all deaths are reported to health authorities within 2 weeks post mortem and an official document (death certificate) stating cause of death is issued.
Calculation
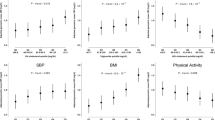
IL-6 and hs-CRP were log transformed to correct for skewed distributions. Analysis of covariance (ANCOVA) was used to test for differences between groups of stroke-survivors and stroke-free subjects after adjustment for age and sex. We used Pearson correlation to analyse the correlation of the cardiovascular risk factors with inflammatory markers. Cox proportional hazard regression model was used to determine whether baseline levels of inflammatory markers predicted all-cause mortality in stroke-survivors and stroke-free subjects. The models were adjusted for age and sex, and additionally adjusted for BMI, smoking, Frenchay activity index, levels of cholesterol, systolic or diastolic blood pressure, a history of myocardial infarction or diabetes (comorbidity), use of statins and blood pressure lowering drugs, whenever these predictors had a p value <0.10 in univariate models of mortality. Due to a high correlation between fibrinogen and hs-CRP (r ≥ 0.66), these variables were not included in the same models. The assumption of proportionality was verified by including log (survival) inflammatory marker as a time dependent interaction term in the Cox proportional hazard regression models and by graphical evaluation of the curves in the log–log (survival) function for the different categories of the inflammatory variables. In subgroup analysis of mortality, we looked at stroke-survivors with and without a history of myocardial infarction, and stroke-free subjects with and without myocardial infarction, because they are at a high cardiovascular risk. We used logistic regression to calculate the area under the receiver operating characteristic curve (AUC) for inflammatory markers in both groups. Analyses were performed using SAS Software package, v9.2 (SAS Institute Inc., Cary, NC, USA) and p values <0.05 were considered significant.
Results
The sex distribution, age and BMI did not differ between stroke-survivors and stroke-free subjects (all p > 0.10, Table 1). Stroke-survivors suffered more comorbidity (myocardial infarction and diabetes), used more medication, had a lower Frenchay activity index score and higher levels of WBC, fibrinogen, log IL-6, and log hs-CRP than stroke-free subjects after adjustment for age and sex (p ranging from <0.001 to 0.03, Table 1). The levels of the inflammatory markers did not differ between patients with stroke ≥7 years ago (n = 98) compared to those who had the stroke <7 years ago (n = 89) (data not shown). Similar calculations were performed for enrolment more than 2, 5 and 10 years, respectively, after the stroke event, and there were no differences in levels of inflammatory markers (data not shown). In stroke-survivors, age, smoking and Frenchay activity index were the main factors that correlated with levels of inflammatory markers, while in stroke-free subjects, age, BMI, smoking, systolic blood pressure and blood pressure lowering drugs were the main factors (data not shown). Levels of cholesterol and use of statins were not correlated with levels of inflammatory markers in any of the groups (data not shown).
During an average of 16 years follow-up, 117 (62.5 %) of the 187 stroke-survivors deceased, and 107 (44.0 %) of 243 the stroke-free subjects deceased (p for differences was 0.005). In stroke-survivors, higher levels of WBC, fibrinogen, log IL-6 and log hs-CRP was associated with increased risk for all-cause mortality after adjustment for age and sex (hazard ratio was ranging from 1.23 to 2.49, all p < 0.05, Table 2). However, only fibrinogen and log IL-6 predicted all-cause mortality after additional adjustment for BMI, smoking, Frenchay activity index, diastolic blood pressure, comorbidity and use of statins (HRs 1.26; 95 % CI 1.05–1.51 and 2.02; 95 % CI 1.12–3.64, respectively, both p < 0.05). AUC for fibrinogen and log IL-6 were 0.65 (95 % CI 0.57–0.73) and 0.63 (95 % CI 0.55–0.72) respectively, both p < 0.01.
In stroke-free subjects log hs-CRP predicted all-cause mortality after adjustment for age and sex (HR 1.63; 95 % CI 1.12–2.36, p = 0.01), and also after additional adjustment for smoking, Frenchay activity index, levels of total cholesterol, systolic blood pressure, comorbidity and use of blood pressure lowering drugs (HR 1.95; 95 % CI 1.26–2.99, p = 0.003). WBC, fibrinogen and log IL-6 were not associated with all-cause mortality in this group. AUC for log hs-CRP was 0.61 (95 % CI 0.54–0.68), p = 0.002.
In subgroup analysis, in those with a history of myocardial infarction, 26 (87 %) of 30 stroke-survivors and 14 (74 %) of 19 stroke-free subjects deceased, and none of the inflammatory markers predicted mortality, except WBC in stroke-free subjects (p = 0.04).
In those without a history of myocardial infarction, 91 (58 %) of 157 stroke-survivors and 93 (42 %) of 224 stroke-free subjects deceased, and the levels of inflammatory markers predicted mortality similarly as reported above, in all stroke-survivors and all stroke-free subjects, respectively (data not shown).
Discussion
We report that long-term ischemic stroke-survivors had higher levels of WBC, fibrinogen, IL-6 and hs-CRP at baseline, and higher all-cause mortality during 16 years follow-up than stroke-free subjects. Moreover, in stroke-survivors, fibrinogen and IL-6 predicted mortality during follow-up, whereas hs-CRP predicted mortality in stroke-free subjects. These findings were independent of traditional cardiovascular risk factors, and remained similar after excluding subjects with a history of myocardial infarction.
To the best of our knowledge, this is the first report on inflammatory markers in a cohort of long-term ischemic stroke-survivors with such a long follow-up. Kwan et al. reported elevated levels of IL-6 at 6 months [5] and Beamer et al. reported elevated levels of fibrinogen 1 year post-stroke [11]. We extend their findings, by reporting that stroke survivors who suffered their stroke more than 2, 5, 7 or 10 years ago, had similar levels of inflammatory markers. These results suggest that an ongoing low-grade inflammation is present in stroke-survivors several years post-stroke.
Measurements of inflammatory markers have been suggested to improve prediction of mortality in middle-aged subjects [8–10], while IL-6 is a better predictor in frail and older subjects [8, 9]. Our data support the observation that IL-6 is a strong predictor of mortality. The association between IL-6 and mortality might reflect age related physiological deterioration and immunosenescence, as aging and frailty is associated with a dysregulated acute phase response promoting enhanced production of proinflammatory cytokines [21, 22].
Interestingly, IL-6, the upstream cytokine of CRP, was an independent mortality predictor among stroke-survivors in contrast to hs-CRP in this study. Stork et al. reported a similar dissociation between IL-6 and CRP on mortality in independently living elderly men [9]. This could be due to variations in the levels of markers by sex- and age, and other traditional risk factors [23].
On the contrary, hs-CRP, and not IL-6, was an independent mortality predictor among the stroke-free subjects in this study. This group was non-significantly younger, had less cardiovascular risk factor burden and less established ischemic heart disease. It is not unlikely that risk factors for a first vascular event might be less predictive for recurrent events due to selection, incident comorbidities, and advanced atherosclerosis [24–26]. These observations are in line with previous reports of a weaker association of CRP with mortality among the oldest, whereas the relation for IL-6 seems to remain by advancing age [8, 10, 27].
Besides carotid revascularization, secondary prevention strategies include antiplatelet therapy, cessation of smoking and control of hyperglycaemia and blood pressure. Statins have anti-inflammatory effects beyond lipid-lowering [28], and may stabilize atherosclerotic plaques [29, 30]. In the SPARCL-study, large doses of atorvastatin reduced the incidence of cardiovascular events and stroke recurrence, when patients were enrolled shortly after the index stroke. No effect on overall mortality was observed [30] and unfortunately no data on inflammatory markers was presented [31]. In our study a small proportion of stroke-survivors used statins, and the levels of inflammatory markers were not influenced by the use of statins.
Our study has several strengths. The cohort was population-based and had long follow-up. All stroke events were verified according to medical records and CT scans. Cause of death was confirmed by reviewing official death certificates and medical records in all cases, with no missing. Inflammatory markers were analysed in blood samples collected more than 1 year after the stroke event, so the levels of the markers were no longer influenced by the stroke-related acute phase reaction. None of the participants suffered clinically manifest infection or inflammation at enrolment, and laboratory analyses were blinded to clinical outcome.
Limitations of the study include that severely ill and disabled stroke-survivors at increased risk of mortality may be underrepresented. Unfortunately, none of the biomarkers studied are specific for cerebral ischemia. Enrolment of subjects at different time points post-stroke may conceal recurrent vascular risks. Consequently, a single measurement of inflammatory markers may mask a potential time-dependency.
Conclusions
Long-term ischemic stroke-survivors had increased mortality, and higher levels of WBC, fibrinogen, IL-6 and hs-CRP at baseline than stroke-free subjects. Fibrinogen and IL-6 were independent predictors of mortality among the stroke-survivors, whereas elevated hs-CRP predicted mortality in stroke-free subjects. Mortality risk prediction in stroke-survivors differed from that of stroke-free subjects.
Abbreviations
- BMI:
-
Body mass index
- WBC:
-
White blood cell count
- IL-6:
-
Interleukin 6
- hs-CRP:
-
High sensitive C-reactive protein
References
Olai L, Omne-Ponten M, Borgquist L et al (2009) Survival, hazard function for a new event, and healthcare utilization among stroke patients over 65 years old. Stroke J Cereb Circ 40:3585–3590. doi:10.1161/STROKEAHA.109.556720
Smith SC Jr, Collins A, Ferrari R et al (2012) Our time: a call to save preventable death from cardiovascular disease (heart disease and stroke). Circulation 126:2769–2775. doi:10.1161/CIR.0b013e318267e99f
Go AS, Mozaffarian D, Roger VL et al (2014) Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation 129:e28–e292. doi:10.1161/01.cir.0000441139.02102.80
Whiteley W, Jackson C, Lewis S et al (2009) Inflammatory markers and poor outcome after stroke: a prospective cohort study and systematic review of interleukin-6. PLoS Med 6:e1000145. doi:10.1371/journal.pmed.1000145
Kwan J, Horsfield G, Bryant T et al (2013) IL-6 is a predictive biomarker for stroke associated infection and future mortality in the elderly after an ischemic stroke. Exp Gerontol 48:960–965. doi:10.1016/j.exger.2013.07.003
Danesh J, Lewington S, Thompson SG et al (2005) Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta-analysis. JAMA 294:1799–1809. doi:10.1001/jama.294.14.1799
Rost NS, Wolf PA, Kase CS et al (2001) Plasma concentration of C-reactive protein and risk of ischemic stroke and transient ischemic attack: the Framingham study. Stroke J Cereb Circ 32:2575–2579
Harris TB, Ferrucci L, Tracy RP et al (1999) Associations of elevated interleukin-6 and C-reactive protein levels with mortality in the elderly. Am J Med 106:506–512
Stork S, Feelders RA, van den Beld AW et al (2006) Prediction of mortality risk in the elderly. Am J Med 119:519–525. doi:10.1016/j.amjmed.2005.10.062
Strandberg TE, Tilvis RS (2000) C-reactive protein, cardiovascular risk factors, and mortality in a prospective study in the elderly. Arterioscler Thromb Vasc Biol 20:1057–1060
Beamer NB, Coull BM, Clark WM et al (1998) Persistent inflammatory response in stroke survivors. Neurology 50:1722–1728
Whiteley W, Chong WL, Sengupta A et al (2009) Blood markers for the prognosis of ischemic stroke: a systematic review. Stroke J Cereb Circ 40:e380–e389. doi:10.1161/STROKEAHA.108.528752
Markaki I, Franzen I, Talani C et al (2013) Long-term survival of ischemic cerebrovascular disease in the acute inflammatory stroke study, a hospital-based cohort described by TOAST and ASCO. Cerebrovasc Dis (Basel, Switzerland) 35:213–219. doi:10.1159/000346094
Whiteley W, Jackson C, Lewis S et al (2011) Association of circulating inflammatory markers with recurrent vascular events after stroke: a prospective cohort study. Stroke J Cereb Circ 42:10–16. doi:10.1161/strokeaha.110.588954
Audebert HJ, Rott MM, Eck T et al (2004) Systemic inflammatory response depends on initial stroke severity but is attenuated by successful thrombolysis. Stroke J Cereb Circ 35:2128–2133. doi:10.1161/01.str.0000137607.61697.77
Winbeck K, Poppert H, Etgen T et al (2002) Prognostic relevance of early serial C-reactive protein measurements after first ischemic stroke. Stroke J Cereb Circ 33:2459–2464
VanGilder RL, Davidov DM, Stinehart KR et al (2014) C-reactive protein and long-term ischemic stroke prognosis. J Clin Neurosci 21:547–553. doi:10.1016/j.jocn.2013.06.015
Jacobsen BK, Eggen AE, Mathiesen EB et al (2011) Cohort profile: the Tromsø Study. Int J Epidemiol. doi:10.1093/ije/dyr049
Engstad T, Bonaa KH, Viitanen M (2000) Validity of self-reported stroke: The Tromso Study. Stroke J Cereb Circ 31:1602–1607
Engstad T, Viitanen M, Arnesen E (2003) Predictors of death among long-term stroke survivors. Stroke J Cereb Circ 34:2876–2880. doi:10.1161/01.str.0000101751.20118.c1
Krabbe KS, Pedersen M, Bruunsgaard H (2004) Inflammatory mediators in the elderly. Exp Gerontol 39:687–699. doi:10.1016/j.exger.2004.01.009
Vasto S, Candore G, Balistreri CR et al (2007) Inflammatory networks in ageing, age-related diseases and longevity. Mech Ageing Dev 128:83–91. doi:10.1016/j.mad.2006.11.015
Silvestri A, Gebara O, Vitale C et al (2003) Increased levels of C-reactive protein after oral hormone replacement therapy may not be related to an increased inflammatory response. Circulation 107:3165–3169. doi:10.1161/01.cir.0000074208.02226.5e
Wolf PA, Clagett GP, Easton JD et al (1999) Preventing ischemic stroke in patients with prior stroke and transient ischemic attack: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke J Cereb Circ 30:1991–1994
Gubitz G, Sandercock P (2000) Prevention of ischaemic stroke. BMJ (Clinical research ed) 321:1455–1459
Egido JA (2005) Benefits of modifying the predictive factors of stroke recurrence. Cerebrovasc Dis (Basel, Switzerland) 20:84–90. doi:10.1159/000089360
Bruunsgaard H, Ladelund S, Pedersen AN et al (2003) Predicting death from tumour necrosis factor-alpha and interleukin-6 in 80-year-old people. Clin Exp Immunol 132:24–31. doi:10.1046/j.1365-2249.2003.02137.x
Stoll G, Bendszus M (2006) Inflammation and atherosclerosis: novel insights into plaque formation and destabilization. Stroke J Cereb Circ 37:1923–1932. doi:10.1161/01.str.0000226901.34927.10
Watanabe K, Sugiyama S, Kugiyama K et al (2005) Stabilization of carotid atheroma assessed by quantitative ultrasound analysis in nonhypercholesterolemic patients with coronary artery disease. J Am Coll Cardiol 46:2022–2030. doi:10.1016/j.jacc.2005.04.070
Amarenco P, Bogousslavsky J, Callahan A 3rd et al (2006) High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 355:549–559. doi:10.1056/NEJMoa061894
Huisa BN, Stemer AB, Zivin JA (2010) Atorvastatin in stroke: a review of SPARCL and subgroup analysis. Vasc Health Risk Manag 6:229–236
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest. On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Regional Committee of Medical and Health Research Ethics.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Frøyshov, H.M., Bjørnerem, Å., Engstad, T. et al. Elevated inflammatory markers predict mortality in long-term ischemic stroke-survivors: a population-based prospective study. Aging Clin Exp Res 29, 379–385 (2017). https://doi.org/10.1007/s40520-016-0575-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-016-0575-9