Abstract
Background and aims
Postoperative delirium (POD) is a common and serious surgical complication among the elderly, especially in those with amnestic mild cognitive impairment (aMCI). Dexmedetomidine (DEX) is neuroprotective for delirium. In this study, we determined the effect of intravenously administered DEX during general anesthesia on POD in elderly aMCI patients undergoing elective hip joint or knee joint or shoulder joint replacement surgery.
Methods
This was a prospective, randomized parallel-group study of aMCI (n = 80) and normal elderly patients (n = 120). Prior to surgery, all subjects underwent neuropsychological assessment and were assigned to one of four groups: the aMCI DEX group (MD group, n = 40), the aMCI normal saline group (MN group, n = 40), the control DEX group (CD group, n = 60), and the control normal saline group (CN group, n = 60). The confusion assessment method was used to screen POD on postoperative days 1, 3, and 7.
Results
We found patients age was positively correlated with POD incidence in the MN group (p < 0.05) but not in the CN group (p < 0.05). DEX treatment significantly decreased POD incidence in both control and aMCI groups relative to their respective placebo groups (all p < 0.05). The fraction of patients whose normal cognitive function was not restored by day 7 after surgery was significantly higher in the MN group than the MD and CN groups (all p < 0.05).
Conclusions
These findings suggested that DEX treatment during surgery significantly reduced POD incidence in both normal and aMCI elderly patients, suggesting that it may be an effective option for the prevention of POD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Delirium is an acute state of confusion characterized by a reduction in the ability to focus, sustain, or shift attention and cognitive changes, including memory loss, disorientation, language disturbance, and perceptual disturbance [1]. Although there is variability in the reported prevalence of delirium in similar settings [2], approximately 20 % of hospitalized patients 65 years and older develop postoperative delirium (POD), accounting for 12.5 million cases each year [3]. POD is a frequent and serious postoperative complication in the elderly, often leading to poor outcomes, including increased mortality, increased length of hospital stay, functional disability, placement in long-term care institutions, and increased hospitalization costs [4, 5]. POD develops within hours to days, and symptoms of POD tend to fluctuate over the course of the day [6]. Although the causes of POD have not yet been identified, several factors, such as advanced age, sex, stroke, use of narcotic analgesics, poor physical condition, alcoholism [7], subjective memory complaints, pre-existing cognitive impairment (Pre-CI) [8], and mild cognitive impairment (MCI), have been linked to increased POD risk.
In a study of nondemented community dwelling elderly admitted to the hospital for acute delirium, 38 % of patients had dementia 2 years later [9]. POD is common in the elderly after surgical repair of hip fractures [10], where 50 % of elderly patients developed POD, and 29 % developed severe delirium [11]. Similarly, in nondemented femoral neck fracture patients, an episode of POD was linked to the development of dementia, higher mortality rate, longer hospitalization, poorer functional recovery [12], and decreased likelihood of returning to previous independent living arrangements [13]. In these studies, cognitive ability prior to the surgery was not established, and MCI patients were usually considered normal. One study found that 20 % of elderly subjects undergoing elective total hip joint replacement surgery exhibited Pre-CI, and of those, 22 % had amnestic MCI (aMCI) [14]. Therefore, it is very important to establish baseline cognitive ability when assessing POD, and cognitive evaluation should be included in the preoperative assessment [15].
MCI refers to mild impairments in cognitive function with intact memory performance, and it may be a transitional stage between normal aging and the development of Alzheimer’s disease (AD) [16]. More specifically, aMCI is a strong risk factor for the progression to AD and dementia, with an annual conversion rate of 10–15 % for both [17, 18]. Consistent with this, there is evidence that subjects with aMCI already exhibit AD pathology [19]. We previously showed that progress of aMCI was accelerated 2 years after surgery and sevoflurane anesthesia, but not after propofol anesthesia. However, in that study we did not determine the relationship between POD and disease progression.
Dexmedetomidine (DEX), a highly selective α2-receptor agonist, provides excellent sedation and analgesia with minimal respiratory depression [20], greater patient satisfaction, and less need for opioids [21, 22]. DEX may be neuroprotective, and its use has been linked to decreased postoperative delirium, stress, and inflammatory responses [23–26], shortened duration of postoperative delirium [27], and increased postoperative cognitive function [25, 26, 28]. In the present study, we evaluated the effect of intravenously administered DEX during general anesthesia on POD in elderly patients with aMCI undergoing elective hip joint or knee joint or shoulder joint replacement surgery.
Materials and methods
Patients
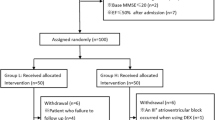
The study protocol was approved by the Institutional Review Board and the Ethics Committee of Beijing Military General Hospital, and written informed consent was obtained from each patient prior to the start of the study. The clinical trial registration number was ChiCTR-ICC-15006276. aMCI (n = 80) and normal elderly (65–80 years old) patients (n = 120, control patients) who underwent a total hip joint or knee joint or shoulder joint replacement surgery with general anesthesia between September 2014 and May 2015, with an American Society of Anesthesiologists physical status II to III were enrolled in the study. A computer-generated random number scheme was used to assign the 200 patients to one of four groups: the aMCI DEX group (MD group, n = 40), the aMCI normal saline group (MN group, n = 40), the control DEX group (CD group, n = 60), and the control normal saline group (CN group, n = 60). Before surgery, all subjects underwent a neuropsychological assessment by a single doctor who was not involved in anesthesia or surgery. The drugs were prepared by one nurse who was not involved in anesthesia or surgery. Both patients and anesthesiologists were blinded to preoperative cognitive function and whether DEX or placebo was administered during surgery. Patients were excluded from the study based on the presence of one of the following conditions: neurological diseases that may affect cognitive function (e.g., subdural hematoma, vascular dementia, frontotemporal dementia, hypothyroidism, alcoholic dementia, vitamin B12 deficiency, and encephalitis), hypoxic pulmonary disease, and perioperative serious cardiopulmonary complications [29].
aMCI was diagnosed clinically with the following criteria: subjective memory complaint (preferably qualified by an informant), an objectively demonstrable memory impairment (e.g., performance 1.5 standard deviations below age-, sex-, and education-matched peers), Clinical Dementia Rating (CDR) score of 0.5, activities of daily living (ADL) score ≤26, a Mini-Mental State Examination (MMSE) score ≤27 (17–27 for illiterates, 20–27 for patients with ≤6 years education, and 24–27 for those with >6 years education), and a Montreal Cognitive Assessment (MoCA) score in the range of 15–24 (indicating no dementia and below the threshold for diagnosis of AD) [29].
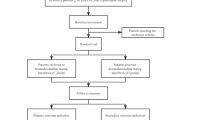
Confusion assessment method (CAM) was used to screen POD. The CAM algorithm consists of four clinical criteria: (1) acute onset and fluctuating course; (2) inattention; (3) disorganized thinking; and (4) altered level of consciousness. For delirium, both the first and the second criteria must be present plus either the third or the fourth criteria or both [30].
Anesthesia procedure
Patients were not medicated prior to surgery. Upon their arrival to the operating room, patients were monitored with invasive blood pressure, an electrocardiogram, a pulse oximeter, and bispectral index (BIS). Anesthetic management was standardized across patients. Midazolam (0.04 mg/kg), etomidate (2 mg/kg), fentanyl (3 µg/kg), and rocuronium (0.6 mg/kg) were used to insert the laryngeal mask (i-gel, Intersurgical Ltd, Wokingham, UK). After induction, patients received a bolus fentanyl infusion (1 μg/kg) and continuous infusion with a syringe pump of propofol (4–6 mg/kg/h) and remifentanil (8–12 µg/kg/h). In the DEX groups, a continuous infusion of DEX at 0.2–0.4 μg/kg/h, without an initial dose, was administered throughout the duration of the surgery. In the control groups, a placebo infusion of normal saline was given. During surgery, the infusion rates of propofol, remifentanil, and DEX were titrated to maintain BIS values between 40 and 50 and changes in mean arterial pressure (MAP) and heart rate (HR) ±20 % of preanesthetic baseline levels. During surgery, patients were given lactated ringer’s solution and hetastarch (5–8 mL/kg) every hour. If hemoglobin levels fell under 80 g/L, concentrated red blood cells were infused. A change in MAP > 20 % below baseline level was corrected with ephedrine. Propofol and remifentanil were discontinued at 5 min, and DEX or placebo was stopped 20 min before the end of surgery. Drugs were not used to reverse the neuromuscular blockade. After restoration of normal breathing and consciousness, the laryngeal mask was removed. A single bolus of fentanyl (0.08 µg/kg) and ondansetron (0.1 mg/kg) was given, and continuous infusion of fentanyl (0.3 µg/kg/h) and ondansetron (12 µg/kg/h) was administered over a 15 min interval for postoperative pain relief. Nonsteroidal anti-inflammatory agent parecoxib was injected intravenously when the visual analogue scale (VAS) was higher than three.
Clinical evaluation
To differentiate aMCI, all the patients prior to surgery were subjected to neuropsychological assessments, including MMSE, MoCA, ADL, and CDR. For postoperative assessment, CAM was used to identify POD on days 1, 3, and 7 after surgery. If patients were normal at 3 days, no follow-up was necessary.
Statistical analysis
Statistical analyses were performed using the SPSS 10.0 software package (SPSS Inc, Chicago, IL). All the data for continuous variables (age, weight, duration of surgery, HR, MAP, SpO2, and MMSE) are shown as mean ± standard deviation. A Pearson \( \chi \) 2 test was used to detect differences in sex, age, diabetes, POD, and POD duration days between groups. When there were less than 40 samples, exact probabilities in a fourfold table were used. Scheffe post hoc test was used to compare differences in POD duration days between groups. To compare the four groups, one-way analysis of variance (ANOVA) was performed with a post hoc least significant difference test. A Spearman’s rank correlation test was used to calculate correlation between age and POD, and the linear trend test was used to analyze bidirectional order grouping data. p < 0.05 was considered statistically significant.
Results
Subjects who did not complete the study, including one patient in the MD group and two patients in the CN group, were sent to the intensive care unit because of delays in recovery. All other patients recovered from anesthesia within 15 min after the end of surgery (Fig. 1).
The levels of HR, MAP, and EtCO2 during surgery were maintained within ±20 % of preoperative levels. As summarized in Table 1, sex, age, age composition, weight, duration of surgery, and education did not differ significantly among the four groups. The number of diabetics in aMCI group was much more than the normal group (44/78 and 39/118, p < 0.01).
As shown in Table 2, the amount of propofol and remifentanil used during anesthesia in the MD group was significantly less than the MN group in two age categories (p < 0.01). Relative to the CN group, the usage of propofol and remifentanil was significantly less than the CD group (p < 0.01).
As shown in Table 3, MMSE scores before surgery were not significantly different between the MD group and the MN group, and between the CD group and CN group. However, MMSE scores were significantly lower in the aMCI groups than the normal groups (all p < 0.01). MoCA and ADL scores were not significantly different among the four groups (all p > 0.05).
Patients were stratified into two age categories (65–75 and ≥75 years) to investigate the correlation between age and POD incidence (Table 4). In the MN group, subject’s age correlated linearly with the incidence of POD (p < 0.05), while not in the CN group. Relative to the CN group, the incidences of POD were significantly higher in 65–75-year-old and ≥75-year-old patients in the MN group (all p < 0.05) and significantly decreased at 65–75-year-old and ≥75-year-old in the CD group (all p < 0.05). Relative to the MN group, both age categories in the MD group exhibited significantly decreased incidence of POD (all p < 0.05). For both age groups, there was no significant difference between the MD and CN groups.
Cognitive function was not restored in some patients by postoperative day 7, including 13 patients (13/25) in the MN group, 2 patients (2/10) in the MD group, and 3 patients (3/18) in the CN group. All POD patients in the CD group recovered to normal cognitive function by postoperative day 7. The ratio of POD patients who did recover by day 7 to total POD patients was significantly greater in the MN group than the MD and CD groups (all p < 0.05), and the ratio of the MN group was not significantly different than the CN group.
These data suggested that age is not a risk factor for POD in normal elderly patients, whereas it is for aMCI patients. DEX administered during surgery significantly reduced the usage of propofol and remifenanil, the incidence of POD in aMCI and normal patients, and the duration of POD days.
Discussion
In the present study, we determined whether administration of DEX improved outcomes in elderly patients with aMCI who underwent elective hip joint or knee joint or shoulder joint replacement surgery under general anesthesia. Older age in aMCI patients was linked with increased POD, whereas POD occurrence did not increase with aging in normal elderly patients. DEX treatment significantly reduced the incidence of POD in both normal and aMCI elderly patients.
Delirium is the most common form of acute brain dysfunction in critically ill patients, and it often goes undetected. We found that the incidence of POD in aMCI patients was higher than in normal elderly patients, suggesting that preoperative cognitive impairment, such as lower MMSE scores and subjective memory complaints, is closely related to the manifestation of POD. To identify patients at risk of developing POD, preoperative assessment by MMSE and direct questions about memory impairment is necessary [15] especially for identification of aMCI patients.
aMCI patients exhibit a broad spectrum of morphological brain changes and pathological characteristics typical of AD like anomalously phosphorylated (p) tau and Aβ fragments in the cerebrospinal fluid (CSF) [31]. aMCI may represent in some individuals a predementia stage of AD, with a population conversion rate to dementia of 10–15 % per year, independent of any effects of anesthesia and surgery [32]. However, there is evidence linking anesthesia and surgery to exacerbation of AD pathologic mechanisms, further augmenting the conversion rate of aMCI to AD [33]. We had found previously that inhaled sevoflurane accelerated the progression of aMCI to progressive MCI after 2 years [29]. Therefore, it is important to neuropsychologically evaluate patients at risk, to identify them prior to surgery and to monitor them closely to prevent POD occurrence. Meanwhile, there was a relationship between aging and POD in aMCI patients but not normal elderly patients, demonstrating that age in aMCI patients is an important predictor of POD incidence.
Previously, DEX treatment significantly reduced the incidence of POD in critically ill patients and those undergoing cardiac surgery with cardiopulmonary bypass [34]. DEX also improved the anesthetic/surgery-induced POCD, attenuated inflammatory response, reduced neuronal apoptosis in hippocampus [35], and decreased the need for benzodiazepines and opioids [36]. Moreover, DEX does not affect the cholinergic system, a major system implicated in cognitive function and the development of delirium. For intensive care unit patients, DEX is a promising agent not only for prevention but also for the treatment of delirium in critically ill patients [37]. Here, administration of DEX during hip joint or knee joint or shoulder joint replacement surgery (anesthesia with propofol and remifentanil) reduced the incidence of POD in aMCI and normal patients at 65–75 years and >75 years old.
Increased body mass index, obesity, impaired glucose tolerance, and type 2 diabetes can significantly increase the incidence of AD and anticipate the age of onset of AD [38]. Absence of insulin in the brain was shown to promote pathological changes and behavioral abnormalities similar to AD and to increase severity of existing AD pathologic lesions [39]. Aβ in AD is toxic to A and B cells in the pancreas, further aggravating existing hormone disorders [40]. aMCI may be an early stage of AD, and we found that the incidence of diabetes in patients with aMCI was significantly higher than normal elderly. Therefore, for those elderly patients with diabetes, especially those with aMCI, preoperative cognitive function should be evaluated and presence of POD monitored.
Management of pain in elderly is an important factor for the development of POD. Avoiding opioids or using very low doses of opioids has been linked with increased risk for delirium. Indeed, cognitively intact patients with undertreated pain were nine times more likely to develop delirium than those patients whose pain was adequately treated, especially in frail older adults [41]. In this study, postoperative pain was alleviated appropriately and in a timely manner, therefore, it was unlikely a factor that affected the conclusions of the study.
POD is not always temporary and can often result in persistent functional and cognitive losses in elderly hospitalized patients [42]. Prolonged duration of POD is an independent risk factor for the development of long-term postoperative cognitive dysfunction (POCD) [37]. In our study, some POD patients did not recover to preoperative cognitive levels by day 7 after surgery (the last day we evaluated patients), and this impairment may be long lasting.
There are a few limitations of our study. First, we did not observe the incidence of POCD after surgery. Second, we did not investigate the relationship between POD and POCD. Third, because of the time restraints of our study, we were unable to investigate the relationship between POD and conversion ratio of dementia. In the future, more long-term studies should be performed to address these important issues.
In conclusion, we found that in aMCI patients, the occurrence of POD was related to aging after total hip joint or knee joint or shoulder joint replacement surgery under general anesthesia. Administration of DEX during surgery was associated with a significant reduction in POD incidence in both normal and aMCI elderly patients.
References
Olofsson B, Lundström M, Borssén B et al (2005) Delirium is associated with poor rehabilitation outcome in elderly patients treated for femoral neck fractures. Scand J Caring Sci 19:119–127
Rooney S, Qadir M, Adamis D et al (2014) Diagnostic and treatment practices of delirium in a general hospital. Aging Clin Exp Res 26:625–633
Inouye SK (2006) Delirium in older persons. N Engl J Med 354:1157–1165
Demeure MJ, Fain MJ (2006) The elderly surgical patient and postoperative delirium. J Am Coll Surg 203:752–757
Mazzola P, Bellelli G, Broggini V et al (2015) Postoperative delirium and pre-fracture disability predict 6-month mortality among the oldest old hip fracture patients. Aging Clin Exp Res 27:53–60
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders (DSM-IV). APA, Washington
Van der Mast RC, van den Broek WW, Fekkes D et al (1999) Incidence of and preoperative predictors for delirium after cardiac surgery. J Psychosom Res 46:479–483
Breteler MM, Claus JJ, Grobbee DE et al (1994) Cardiovascular disease and distribution of cognitive function in elderly people: the Rotterdam Study. BMJ 308:1604–1608
Gustafson Y, Berggren D, Brännström B et al (1988) Acute confusional states in elderly patients treated for femoral neck fracture. J Am Geriatr Soc 36:525–530
Brannstrom B, Gustafson Y, Norberg A et al (1989) Problems of basic nursing care in acutely confused and non-confused hip-fracture patients. Scand J Caring Sci 3:27–34
Marcantonio ER, Flacker JM, Michaels M et al (2000) Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc 48:618–624
Berggren D, Gustafson Y, Eriksson B et al (1987) Postoperative confusion after an-esthesia in elderly patients with femoral neck fractures. Anesth Analg 66:497–504
Rahkonen T, Luukkainen-Markkula R, Paanila S et al (2000) Delirium episode as a sign of undetected dementia among community dwelling elderly subjects: a 2 year follow up study. J Neurol Neurosurg Psychiatry 69:519–521
Evered LA, Silbert BS, Scott DA et al (2011) Preexisting cognitive impairment and mild cognitive impairment in subjects presenting for total hip joint replacement. Anesthesiology 114:1297–1304
Veliz-Reissmüller G, Agüero Torres H, Van der Linden J et al (2007) Pre-operative mild cognitive dysfunction predicts risk for post-operative delirium after elective cardiac surgery. Aging Clin Exp Res 19:172–177
Panza F, D’Introno A, Colacicco AM et al (2005) Current epidemiology of mild cognitive impairment and other predementia syndromes. Am J Geriatr Psychiatry 13:633–644
Forlenza OV, Diniz BS, Gattaz WF (2010) Diagnosis and biomarkers of predementia in Alzheimer’s disease. BMC Med 8:89
Welge-Lüssen A (2009) Ageing, neurodegeneration, and olfactory and gustatory loss. B-ENT 5(suppl 13):129–132
Markesbery WR, Schmitt FA, Kryscio RJ et al (2000) Neuropathologic substrate of mild cognitive impairment. Arch Neurol 63:38–46
Bhana N, Goa KL, McClellan KJ (2000) Dexmedetomidine. Drugs 59:263–268
Candiotti KA, Bergese SD, Bokesch PM et al (2000) Monitored anesthesia care with dexmedetomidine: a prospective, randomized, double-blind, multicenter trial. Anesth Analg 110:47–56
Cooper L, Candiotti K, Gallagher C et al (2011) A randomized, controlled trial on dexmedetomidine for providing adequate sedation and hemodynamic control for awake, diagnostic transesophageal echocardiography. J Cardiothorac Vasc Anesth 25:233–237
Yang S, Lee H (2014) A dose-finding study of preoperative intravenous dexmedetomidine in children’s emergence delirium after epiblepharon surgery. Eur J Ophthalmol 24:417–423
Bekker A, Haile M, Kline R et al (2013) The effect of intraoperative infusion of dexmedetomidine on the quality of recovery after major spinal surgery. J Neurosurg Anesthesiol 25:16–24
Zhang X, Wang J, Qian W et al (2014) Dexmedetomidine inhibits tumor necrosis factor-alpha and interleukin 6 in lipopolysaccharide-stimulated astrocytes by suppression of c-Jun N-terminal kinases. Inflammation 37:942–949
Zhang Y, Xing Z, Xu Y et al (2014) Effects of different doses of dexmedetomidine on cognitive dysfunction in elderly patients early after laparoscopic surgery for colorectal cancer. Nan Fang Yi Ke Da Xue Xue Bao 34:743–746
Shehabi Y, Grant P, Wolfenden H et al (2009) Prevalence of delirium with dexmedetomidine compared with morphine based therapy after cardiac surgery: a randomized controlled trial (dexmedetomidine compared to morphine-DEXCOM study). Anesthesiology 111:1075–1084
Chen J, Yan J, Han X (2013) Dexmedetomidine may benefit cognitive function after laparoscopic cholecystectomy in elderly patients. Exp Ther Med 5:489–494
Liu Y, Pan N, Ma Y et al (2013) Inhaled sevoflurane may promote progression of amnestic mild cognitive impairment: a prospective, randomized parallel-group study. Am J Med Sci 345:355–360
Inouye SK, van Dyck CH, Alessi CA et al (1990) Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 113:941–948
Bickel H, Gradinger R, Kochs E et al (2008) High risk of cognitive and functional decline after postoperative delirium: a three-year prospective study. Dement Geriatr Cogn Disord 26:26–31
Lundstrom M, Edlund A, Bucht G et al (2003) Dementia after delirium in patients with femoral neck fractures. J Am Geriatr Soc 51:1002–1006
Koppel J (2005) Memory impairment, but not cerebrovascular disease, predicts progression of MCI to dementia. Neurology 64:766
Xie Z, Tanzi RE (2006) Alzheimer’s disease and post-operative cognitive dysfunction. Exp Gerontol 41:346–359
Levkoff SE, Evans DA, Liptzin B et al (1992) Delirium: the occurrence and persistence of symptoms among elderly hospitalized patients. Arch Intern Med 152:334–340
Murray AM, Levkoff SE, Wetle TT et al (1993) Acute delirium and functional decline in the hospitalized elderly patient. J Gerontol 48:M181–M186
Morrison RS, Magaziner J, Gilbert M et al (2003) Relationship between pain and opioid analgesics on the development of delirium following hip fracture. J Gerontol A Biol Sci Med Sci 58:76–81
Pasin L, Landoni G, Nardelli P et al (2014) Dexmedetomidine reduces the risk of delirium, agitation and confusion in critically ill patients: a meta-analysis of randomized controlled trials. J Cardiothorac Vasc Anesth 28:1459–1466
Haan MN, Shemanski L, Jagust WJ et al (1999) The role of APOE epsilon 4 in modulating effects of other risk factors for cognitive decline in elderly persons. JAMA 282:40–46
Qian XL, Zhang W, Liu MZ et al (2015) Dexmedetomidine improves early postoperative cognitive dysfunction in aged mice. Eur J Pharmacol 746:206–212
Pasin L, Greco T, Feltracco P (2013) Dexmedetomidine as a sedative agent in critically ill patients: a meta-analysis of randomized controlled trials. PLoS One 8:e82913
Mo Y, Zimmermann AE (2013) Role of dexmedetomidine for the prevention and treatment of delirium in intensive care unit patients. Ann Pharmacother 47:869–876
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Liu, Y., Ma, L., Gao, M. et al. Dexmedetomidine reduces postoperative delirium after joint replacement in elderly patients with mild cognitive impairment. Aging Clin Exp Res 28, 729–736 (2016). https://doi.org/10.1007/s40520-015-0492-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-015-0492-3