Abstract
Background and aims
There is no conclusive evidence that hospital fall prevention programs can reduce the number of falls. We aimed to investigate the effect of a targeted individualized falls prevention program in a geriatric rehabilitation hospital.
Methods
This was a two-stage cluster-controlled trial carried out in five geriatric rehabilitation wards. Participants were 752 patients with mean age 83.2 years. The intervention was a two-phase targeted intervention falls prevention program. The intervention included an assessment of patient’s risk by a risk assessment tool and an individual management that includes medical, behavioral, cognitive and environmental modifications. Patients with moderate risk received additionally orientation guidance, and mobility restriction. Patients determined as high risk were additionally placed under permanent personal supervision. Outcome measures were falls during hospital stay.
Results
In both stages of the trial, intervention and control wards were almost similar at baseline for individual patient characteristics. Overall, 37 falls occurred during the study. No significant difference was found in fall rates during follow-up between intervention and control wards: 1.306 falls per 1000 bed days in the intervention groups and 1.763–1.826 falls per 1000 bed days in the control groups. The adjusted hazard ratio for falls in the intervention groups was 1.36 (95 % confidence interval 0.89–1.77) (P = 0.08) in the first stage and 1.27 (95 % confidence interval 0.92–1.67) (P = 0.12) in the second stage.
Conclusion
These results suggest that in a geriatric rehabilitation hospital a targeted individualized intervention falls prevention program is not effective in reducing falls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Falls are a common incident among elderly inpatients in geriatric rehabilitation hospitals. There is an increasing number of reports in the literature lately, focusing on falls in geriatric rehabilitation wards, especially on risk factors associated with falls in this population [1–5]. In any individual hospital unit, the rate of falls depends on case mix, environment and practice of care. Fall rate in settings providing stroke rehabilitation was found to be 0.76–0.95 falls per patient [1, 2]. Among various forms of geriatric care, 80–90 % of patient’s injuries were caused by falls [3]. The risk of falls is especially high among stroke patients, [6–8] with frequency rates between 25 and 39 % [2, 9, 10]. In our hospital (A 150-bed geriatric rehabilitation facility), frequency rates of falls were 15.6 % in stroke patients, 13.7 % in the orthopedic patients and 13.3 % in the deconditioning patients also [11]. These rates resemble reports from rehabilitation settings that estimated that between 14 and 65 % of the patients fall during the hospitalization [4, 10].
A cornerstone of the most fall prevention programs is prediction of falls by identification of risk factors. Many of the approaches in discriminating fallers from non-fallers and predicting future falls are similarly effective. Therefore, the decision of which instrument to select may rest primarily on factors such as clinician’s practical experience and assessment space availability. Clinical prediction rules are tools designed to predict health outcomes. Risk assessment tools for prediction of falls typically include a number of risk factors from a patient’s history and physical exam that predicts falls [12, 13]. We reported previously [11] in a study that investigated the characteristics and risk factors predictive of falls in patients hospitalized in our hospital, that risk factors for falls differ between different groups of rehabilitation patients, and that the selection of population may affect which combination of risk factors are identified.
We previously investigated the operational characteristics of a geriatric rehabilitation adjusted risk assessment tool, to identify fallers in our hospital [14]. Our current fall risk assessment tool was derived from the results of our previous studies [11, 14] and from published papers on risk factors and risk assessment tools for falls in hospitalized patients [15–19].
Previous studies performed in general hospitals with historical controls and randomized controlled trials in community settings have reduced fall rates using targeted multiple intervention strategies [20–22]. We evaluated the effectiveness of a targeted individualized intervention falls prevention program in reducing the rate of falls in a geriatric rehabilitation hospital. Although the study intervention was directed toward selected patients, we used a cluster design because methodically it was delivered in different wards. It was also important to maximize the ability to control for “contamination” across patients.
Methods
Participants
We carried out a two-stage cluster-controlled trial in our hospital wards. The study took place over a 6-month period at the Fliman Rehabilitation Geriatric Hospital (A 150-bed public geriatric facility affiliated with the Technion-University Medical School and located in Haifa, Israel). All patients over 65 years of age admitted consecutively to the five geriatric rehabilitation wards having a total of 150 beds were assessed. Wards participated in the study were general geriatric rehabilitation wards with very similar mix of patients as can be seen in Tables 1 and 2. Two to three wards were included in each cluster. Patients restricted to bed were excluded.
We obtained approval for the study from our local institutional, and from the Ministry of Health Helsinki committee. Written informed consent was obtained from participants and/or legally authorized representatives only in the active arm before starting the intervention. In the first stage of the study, each ward was studied for 3 months. Three geriatric rehabilitation wards were included in the intervention program and all other wards continued with the usual standards of care. In the second stage of the study, the three wards that performed according to usual standards of care in the first stage started also with the intervention program.
Sample size was determined by estimating Intra-cluster correlation coefficient. Observed ICC was close to the one used in sample size calculations. Clusters size did not vary during the study. Randomization was carried on with a partial stepped wedge design in a way that all clusters eventually were included in the investigation to allow clusters to be enrolled gradually over time. The hospital was the natural unit of inference and standard methods of sample size estimation were applied to the cluster level. Recruitment was done by individuals independent of the trial. We recruited similar size clusters, with stuff of similar experience in the same hospital.
Ward and participant selection
We collected information on fall rates, lengths of stay, and patients’ ages from all the rehabilitation wards. We collected also baseline information on health, drugs, and physical function from the medical records of all patients in intervention and control wards, for descriptive purposes only. Delirium was assessed by the confusion assessment method (CAM). Diagnosis of dementia and depression was based on a standardized clinical approach using diagnostic and statistical manual of mental disorders. The researchers had no direct contact with patients but were not able to be kept blind to whether patients were in intervention or control wards.
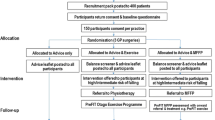
Interventions
The intervention package (a targeted multiple intervention falls prevention program) was delivered by the ward staff, after a comprehensive and detailed training program. In the wards participating, the intervention package was implemented as a part of the usual routine work of the ward. The control wards had no trial interventions.
Participants in the control groups continued to receive usual care which consists of any activities undertaken by the participants recommended or administered by their treating team and did not receive any of the interventions from the falls prevention program. Senior nursing staff in control wards was aware of the study because the researchers were collecting study data.
The targeted multiple intervention falls prevention program
The targeted intervention falls prevention program was composed of two parts:
-
1.
Assessment of every patient’s specific risk by our risk assessment tool. The researchers obtained a risk assessment tool score, for all patients admitted for rehabilitation, once a week. The risk assessment tool was administered once a week because of the dynamic functional characteristics of the patient during the rehabilitation that actually determined the type of intervention. According to this tool, patients were classified as having a high, moderate, mild or minimal risk.
-
2.
Each week and a day after each admission, after obtaining the risk assessment tool score, patients classified as having mild, moderate or high risk were included in an individualized fall prevention program. Each patient with mild risk was assessed and managed individually according to the program. The assessment includes medical interventions, environmental modifications, toilets and shower-room adjustment, mobility care, bed and wheelchair adjustment, behavioral and cognitive treatment and patient and family guidance. Each patient with moderate risk was assessed similarly and received additionally regular orientation guidance, and was assessed for the need of a safety mobility restriction. The safety mobility restriction was assurance that mobility (transfers, walking, toilets usage, etc.) was done only under supervision and/or assistance of a professional stuff member. Each patient determined as high risk received the treatment package as those with moderate risk and were additionally placed in a visible location in the ward, a permanent personal supervision and hip protectors were considered and an urgent multidisciplinary discussion regarding the patient’s individual approach took place.
Outcomes
The primary outcome was falls of patients in study wards during the study period. A fall was defined as unintentionally coming to rest on the ground or other lower level not as a result of a major acute internal medical or external event. Information on falls was collected by the researchers from incident reports filed in patients’ medical records, from notes in medical records themselves, and by asking a senior nurse each day about any falls on the ward in the past 24 h.
Statistical analysis
Comparisons of outcome measures between groups were performed using Chi square tests, Fisher exact test or Mann–Whitney tests, as appropriate. A comparison of the number of falls, number of fallers and fall rate per 1000 bed days between groups was performed using a multivariate Poisson regression model. In multivariate analyses, age category (60–74 vs. ≥75), sex, cognitive impairment, stroke, Parkinson’s disease, diabetes mellitus, visual impairment and history of falls were regarded as possible covariates for the multivariate analysis. These variables have been hypothesized on theoretical grounds or have been shown in previous research to be confounders of the relationship between fall prevention intervention and falls. All P values were two-sided to detect a significance level of P < 0.05. Analysis was conducted on an individual level. Adjusting for clustering and analyses was performed using SAS software version 9.2 (SAS Institute. Inc., Cary, NC, USA).
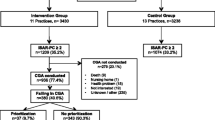
Results
On the first stage of the study, we approached 552 patients, of whom 44 (8.0 %) were excluded (20 in the Intervention group and 24 in the Control group). 200 patients were in the Intervention group and 308 patients in the Control group. On the second stage of the study, we approached 610 patients, of whom 58 (9.5 %) were excluded (22 in the Intervention period and 36 in the Pre-intervention period). 244 patients were in the Intervention period and 308 patients in the Pre-intervention period. Coefficient of variation of cluster size was 0.61. Figure 1 shows a flowchart of the first and second phase’s enrollment and follow-up of participants in the falls prevention program intervention. No participants withdrew from the trial during the study period, and there were no adverse events attributable to the intervention.
Baseline characteristics of participants in each group were similar in the two stages of the study (Tables 1, 2) besides slightly higher age of pre-intervention participants in the second phase and longer stay in the control group patients in the first phase. There were also a higher percentage of females in the control group in the first phase and in the intervention period in the second phase and more patients with delirium in the intervention period in the second phase. In total, 37 falls occurred during the study period, but as 8 falls of the pre-intervention period are counted twice, 22 falls occurred during the first phase and 23 during the second phase. In the first phase, the average fall rates in the intervention group were slightly higher than in the control group, but this difference was not statistically significant: 1.306 falls per 1000 bed days and 1.826 per 1000 bed days, respectively (Table 3). In the second phase, the average fall rates in the intervention period and the pre-intervention period were not significantly different: 1.306 falls per 1000 bed days and 1.763 per 1000 bed days, respectively (Table 4).
The crude results of the proportional hazards analysis were not significant (Tables 3, 4) for the first phase (P = 0.11) and the second phase (P = 0.15). In the first phase, the HR of the intervention to control group was 1.47 [95 % confidence interval (CI) 0.79–1.97]. The HR did not change significantly −1.36 (95 % CI 0.87–1.77) after adjustment for age, sex, cognitive impairment, stroke, Parkinson’s disease, diabetes mellitus, visual impairment and history of falls. In the second phase, the HR of the intervention to pre-intervention period group was 1.42 [95 % confidence interval (CI) 0.91–1.88]. This HR did not change significantly −1.27 (95 % CI 0.92–1.67) after adjustment for age, sex, cognitive impairment stroke, Parkinson’s disease, diabetes mellitus, visual impairment and history of falls.
During the intervention, patients participating in the program were examined for their fall risks according to our risk assessment tool. Most patients in the two phases of the intervention were found to have a high fall risk (moderate–high). In the first phase, 61.5 % of the patients were classified as moderate risk and 30.5 % as high risk. In the second phase, 63.9 % of the patients were classified as moderate risk and 26.6 % as high risk. Examining falls according to risk, we found in the first phase that in the intervention group all falls occurred in the highest fall risk patients, 10 (71.4 %) in moderate risk patients and 4 (28.6 %) in the high risk patients. Also in the second phase intervention group, most falls occurred in the highest fall risk patients, 9 (60 %) in moderate risk patients and 4 (25.6 %) in the high risk patients.
To examine the operational usefulness of our current clinical prediction tool, we tried to validate it in the intervention groups. The tool had sufficiently high sensitivity (87–100 %) applying to moderate and high risk patients together, but insufficiently low specificity. All fallers in the first phase and 87 % of fallers in the second phase were graded as moderate–high risk (Tables 3, 4).
Discussion
This study found that a targeted individualized falls prevention intervention program had no effect on fall rates in elderly care wards in our geriatric rehabilitation hospital. The lack of effect was evident in both phases of the study despite the planned interventions being successfully implemented and used appropriately.
In reviewing recent literature on the subject, we found several systematic reviews addressing prevention of falls during hospitalizations. A recent systematic review of 69 studies reported about in-hospital falls intervention groups and concurrent (controlled trials) or historic comparators (before–after studies) [23]. The pooled post intervention incidence rate ratio (IRR) was 0.77. Meta-regressions showed no systematic association between implementation intensity, intervention complexity, comparator information, or adherence levels and IRR.
Another recent systematic review by Cochrane Database of Systematic Reviews of 10 studies reported about the effectiveness of interventions aimed at preventing falls in people after stroke [24]. They included randomized controlled trials of interventions where the primary or secondary aim was to prevent falls in people after stroke. The review concluded that there is currently insufficient evidence that exercises tested prevent falls or decrease the number of people falling after being discharged from rehabilitation following their stroke. Another recent systematic review by Cochrane Database of Systematic Reviews of 60 trials reported about the effectiveness of interventions designed to reduce falls by older people in care facilities and hospitals [25]. This review concluded that exercise in subacute hospital settings appears effective but its effectiveness in care facilities remains uncertain due to conflicting results, possibly associated with differences in interventions and levels of dependency. They found evidence that multifactorial interventions reduce falls in hospitals but the evidence for risk of falling was inconclusive.
These lately published systematic reviews emphasize that there is no conclusive evidence that hospital fall prevention programs can reduce the number of falls or fallers. These results are compatible with our study that suggests that the current approaches to falls prevention in elderly rehabilitation care wards are ineffective. These observations must be taken carefully in light of some known difficulties in performing conventional clinical trials’ research in the setting of geriatric hospitals. First because falls are not always reliably recorded and are subject to considerable recording bias; second because of the Hawthorne effect that biases the results toward the null because of the potential for standard care group participants to reduce their falls risk independently as a result of being observed; the third problem is that there are inevitably underlying variation and secular trends in fall rates and other factors such as unit case-mix, staffing, layout, etc. These could all have influenced the falls rate so it is hard to attribute the apparent change to the intervention provided without much more rigorous control. We tried to address these potential recording biases by collecting information concerning falls from all sources: staff, patients and families. We tried to overcome the Hawthorne Effect in our study by improving the communication between the participants considering how participants’ experience may influence them.
Another possible factor that may have contributed to the intervention’s observed lack of effect is that our falls risk assessment tool did not accurately predict patients’ risk of falling. Most falls prevention interventions have employed approaches which focus on identifying falls risk factors as a key factor in the process. Certainly, the use of such tools might help focus the mind and raise awareness. Nonetheless, there are serious problems associated with using them [26].
These observations emphasize the fact that the most older people in our wards have some functional impairment and are prone to falls, immobility or confusion in the face of even sometimes quite minor medical illnesses.
Moreover, they tend to have an accumulation of disabilities and are treated with multiple medications which can contribute to falls. Although falls may occasionally have one simple explanation, they are generally the result of synergistic interactions between frailties, long-term medical illness, acute medical illness, medications, the person’s own behavior and environmental hazards. It is also crucial to recognize that, in the rehabilitation hospital setting, we are trying to encourage people to regain independence and mobilize them prior to discharge. In such setting, falls will happen and are almost inevitable if unwelcome part of encouraging older people to rehabilitate following transient disability associated with illness.
Strengths of our study include its appropriate sample size, which resulted in fairly narrow confidence intervals ruling out the possibility that we might have missed a large intervention effects. The randomization of wards seems to have been successful in eliminating major systematic differences between patients in intervention and control wards. Although we did not accomplish a pair wise matching of wards by previous fall rate, the overall previous fall rates in intervention and control wards were similar.
Generalizability of our results is problematic. There is a growing body of evidence that there are considerable difficulties of developing falls predictive tools and fall prevention programs based on such tools, owing to the wide range of factors associated with falls, the varying profiles relating to environmental status and the problems with validating fall events. Our results may be with reasonable caution generalizable to other similar settings. However, generalizing our findings to other settings may be problematic.
This study has a number of other limitations. First, data were not collected blind to intervention status. It is possible that in intervention wards the study raised awareness of falls and resulted in more diligent reporting than in control wards. Second, some falls prevention activities were already occurring in control (and intervention) wards before the start of our study. These activities continued during the study period, making it more difficult to show any effect of our interventions. Third, random error in measuring falls could also contribute to a null result; to minimize this, a criterion standard of falls calendars was used. Fourth, as a cluster-randomized trial, our trial was more vulnerable to lack of comparability between study arms than individual randomization. To minimize this in our intervention, clusters were randomized, and all consenting persons enrolled.
In summary, this study does not support the use of current approaches to falls prevention in geriatric rehabilitation wards. This may not be surprising given that the established risk factors for falls in such wards are all difficult to modify: hyperactive delirium, gait instability, use of sedative or hypnotic drugs, and urinary incontinence. Prevention of falls in geriatric rehabilitation wards may require innovative approaches, including improved methods for assessment and management of cognitive impairment, use of low beds and hip protectors to prevent injury, redesign of hospital wards so that patients at high risk of falling are readily observable at all times by busy nursing staff, hour supervision of patients at highest risk of falling, and a whole system approach to ward-based falls prevention led by ward staff themselves that will result in changes of work practice. Future research involving economic evaluation of wards based services should focus on point-of-care multidisciplinary services that can address directly the medical, physical, and environmental aspects of falls.
References
Nyberg L, Gustafson Y, Patient falls in stroke rehabilitation (1995) A challenge to rehabilitation strategies. Stroke 26:838–842
Teasell R, McRae M, Foley N, Bhardwaj A (2002) The incidence and consequences of falls in stroke patients during inpatient rehabilitation: factors associated with high risk. Arch Phys Med Rehabil 83:329–333
Uden G (1985) Inpatients accidents in hospitals. J Am Geriatr Soc 33:833–841
Ross MK, Egan E, Zaman M, Aziz B, Dewald T, Mohammed S (2012) Falls in the inpatient rehabilitation facility. Phys Med Rehabil Clin N Am 23(2):305–314
Vieira ER, Freund-Heritage R, da Costa BR (2011) Risk factors for geriatric patient falls in rehabilitation hospital settings: a systematic review. Clin Rehabil 25(9):788–799
DeVincenzo DK, Watkins S (1987) Accidental falls in a rehabilitation setting. Rehabil Nurs 12:248–252
Mayo NE, Korner-Bitensky N, Becker R, Georges P (1989) Predicting falls among patients in a rehabilitation hospital. Am J Phys Med Rehabil 68:139–146
Vlahov D, Myers AH, Al-Ibrahim MS (1990) Epidemiology of falls among patients in rehabilitation hospital. Arch Phys Med Rehabil 7:8–12
Dromerick A, Reding M (1994) Medical and neurological complications during inpatient stroke rehabilitation. Stroke 25:358–361
Rochat S, Monod S, Seematter-Bagnoud L, Lenoble-Hoskovec C, Büla CJ (2013) Fallers in postacute rehabilitation have worse functional recovery and increased health services use. J Am Med Dir Assoc 14(11):832–836
Aizen E, Shugaev I, Lenger R (2007) Risk factors and characteristics of falls during inpatient rehabilitation of elderly patients. Arch Gerontol Geriatr 44:1–12
Nyström A, Hellström K (2013) Fall risk 6 weeks from onset of stroke and the ability of the prediction of falls in rehabilitation settings tool and motor function to predict falls. Clin Rehabil 27(5):473–479
Morrison G, Lee HL, Kuys SS, Clarke J, Bew P, Haines TP (2011) Changes in falls risk factors for geriatric diagnostic groups across inpatient, outpatient and domiciliary rehabilitation settings. Disabil Rehabil 33(11):900–907
Aizen E, Zlotver E (2013) Prediction of falls in rehabilitation and acute care geriatric setting. J Clin Gerontol Geriatr 4(2):57–61
Oliver D, Daly F, Martin FC, McMurdo ME (2004) Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age Ageing 33(2):122–130
Vassallo M, Vignaraja R, Sharm JC, Briggs R, Allen SC (2004) Predictors for falls among hospital inpatients with impaired mobility. J R Soc Med 97(6):266–269
Sze KH, Wong E, Leung HY, Woo J (2001) Falls among chinese stroke patients during rehabilitation. Arch Phys Med Rehabil 82:1219–1225
Chu LW, Pei CK, Chiu A, Liu K, Chu MM, Wong S, Wong A (1999) Risk factors for falls in hospitalized older medical patients. J Gerontol A Biol Sci Med Sci 54(1):M38–M43
Gluck T, Wientjes HJ, Rai GS (1996) An evaluation of risk factors for in-patient falls in acute and rehabilitation elderly care wards. Gerontology 42(2):104–107
Oliver D, Hopper A, Seed P (2000) Do hospital fall prevention programs work? A systematic review. J Am Geriatr Soc 48:1679–1689
Gillespie L, Gillespie W, Robertson M, Lamb S, Cumming R, Rowe B (2003) Interventions for preventing falls in elderly people. Cochrane Database Syst Rev 4:CD000340
Vieira ER, Berean C, Paches D, Caveny P, Yuen D, Ballash L, Freund-Heritage R (2013) Reducing falls among geriatric rehabilitation patients: a controlled clinical trial. Clin Rehabil 27(4):325–335
Hempel S, Newberry S, Wang Z, Booth M, Shanman R, Johnsen B, Shier V, Saliba D, Spector WD, Ganz DA (2013) Hospital fall prevention: a systematic review of implementation, components, adherence, and effectiveness. J Am Geriatr Soc 61(4):483–494
Verheyden GS, Weerdesteyn V, Pickering RM, Kunkel D, Lennon S, Geurts AC, Ashburn A (2013) Interventions for preventing falls in people after stroke. Cochrane Database Syst Rev 31(5):CD008728
Cameron ID, Gillespie LD, Robertson MC, Murray GR, Hill KD, Cumming RG, Kerse N (2012) Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev 12:CD005465
Oliver D (2006) Assessing the risk of falls in hospital. Time for a rethink? Can J Nurs Res 38:89–94
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aizen, E., Lutsyk, G., Wainer, L. et al. Effectiveness of individualized fall prevention program in geriatric rehabilitation hospital setting: a cluster randomized trial. Aging Clin Exp Res 27, 681–688 (2015). https://doi.org/10.1007/s40520-015-0330-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-015-0330-7