Abstract
Purpose
The regulation of food intake and body weight involves two interacting systems: (a) The homeostatic system (including biological regulators of hunger and satiety) and (b) the non-homeostatic system, (involving concepts of food reinforcement and food addiction). Studies have established a strong genetic component in eating behavior and obesity. The TaqI A1 polymorphism (rs1800497) has previously been associated with eating behavior, diminished dopamine D2 receptor (DRD2) density, higher body mass, and food reinforcement, but relations to food addiction remain unclear.
Aim
To evaluate the association between the polymorphism rs1800497 with eating behavior, food reinforcement and food addiction in Chilean adults.
Methods
This cross-sectional study recruited a convenience sample of 97 obese, 25 overweight and 99 normal-weight adults (18–35 years). Anthropometric measurements were performed by standard procedures. Eating behavior was assessed using the: Yale Food Addiction Scale (YFAS), the Three Factor Eating Behavior Questionnaire and the Food Reinforcement Value Questionnaire (FRVQ). The DRD2 genotype (rs1800497) was determined by taqman assays.
Results
Twenty-two percentage of the participants met the criteria for food addiction. Food addiction was higher in women than men (26% vs 10.7%) and in obese compared to non-obese (40% vs 6%). There was no relationship between food addiction and DRD2 genotype. However when stratified by sex and nutritional status, obese female carriers of the A1 allele reported greater scores on emotional eating and snack food reinforcement compared to non-carriers.
Conclusions
The DRD2 polymorphism is associated with some hedonic aspects of eating behavior, namely food reinforcement and emotional eating but not food addiction, and this association may be moderated by sex and obesity status, with obese women who are carriers of this genetic variant at higher risk.
Level of evidence
Level V: evidence obtained from a cross-sectional descriptive study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Globally, obesity is a major public health problem in most affluent countries [1, 2]. In Chile, the last National Health Survey shows that 74% of adults and 40% of adolescents are living with overweight or obesity [3]. Understanding the cause of obesity has been a main topic and advances in neuroscience suggest that addiction to specific foods may partially explain the rising rates of obesity [4]. In this sense, highly palatable foods can impact the reward circuitry in a similar way as addictive drugs, resulting in the development of food addiction [5, 6]. “Food addiction” is a behavioral addiction that is characterized by compulsive consumption of palatable foods, and is related to activation of the brain reward system in animals and humans [6, 7]. Like other addictions, the criteria for diagnosing food addiction involves a clinically significant physical and/or psychological dependence on high sugar, high fat, and highly palatable foods, as well as symptoms of withdrawal upon cessation [8]. The construct “food addiction” was first presented by Randolph in 1956, around a period when addictive-like consumption of wheat, corn, potatoes, chocolate, coffee, milk and eggs were reported [9]. Studies have shown evidence that food addiction and drug addiction may be similar in craving, disinhibition and tolerance [10].
Related to food addiction is the concept of food reinforcement, or how hard an organism is willing to work to obtain palatable food. Research shows there are individual differences whereby persons with obesity show a greater prevalence of food addiction and who find food more reinforcing than those without obesity [5]. There is growing attention in defining the functions played by the food reward system in regulating food intake, as well as the possible connections that may exist between this system and the development of food addiction in humans. In this sense, dopamine (DA) is the predominant catecholamine neurotransmitter that modulates the reward circuit and has been implicated in the regulation of food reinforcement, eating and obesity [11]. Studies propose that altered dopamine signaling capacity increases risk of obesity [12], but the findings concerning the direction of signaling (i.e., hypodopaminergic vs hyperdopaminergic states) have been mixed, highlighting the complexity of these relationships and the need for further investigation [13, 14].
The dopamine D2 receptor gene (DRD2) moderates the reward circuitry and is located on chromosome 11 (q22-23). The DRD2 encodes a G protein coupled receptor located in dopaminergic post-synaptic neurons involved in pathways related to reinforcement and gratification [15]. The most common genetic variant of the DRD2 gene is the rs1800497 SNP, also known as the Taql A1 Allele, with the T allele (A1/A2) representing the risk allele. This polymorphism has been linked with habitual use of alcohol, cocaine, nicotine, obesity and eating behavior [16,17,18]. However, few studies have examined the association between this dopamine polymorphism, food reinforcement, food addiction, and eating behavior in adult samples, or explored if these gene-environment associations differ by sex or weight status. Accordingly, the aims of this study were to examine the association between TaqI A1 polymorphism (rs1800497) in the dopamine 2 receptor gene with eating behavior, food reinforcement, food addiction, and obesity in a sample of Chilean adult males and females. We hypothesized that carriers of the TaqI A1 (A1/A2) would exhibit unhealthier eating behavior (higher emotional and uncontrolled eating), higher food reinforcement, higher prevalence of food addiction and greater adiposity compared to non-carriers (A2/A2).
Materials and methods
We conducted this study, which used a cross-sectional design, from January 2016 to March 2017. The convenience sample consisted of 221 adults (74% female; 18–54 years old), 43.8% with obesity, 11.3% overweight, and 44.8% normal weight. Participants were excluded from participating if they were participating in a weight loss program, underweight, not between 18 and 55 years of age, if they were taking medications that influence body weight or metabolism, had diabetes, weight-related hepatic or renal disease, or who had missing phenotypic data. Participants were recruited from diverse sources in the community, including via posters in university campuses, community and recreational centres, as well as online advertising at the Universidad San Sebastian website (http://www.uss.cl). All participants signed informed consent and were tested in the laboratory at San Sebastian University. This study was approved by the Research Scientific Ethics Committee of San Sebastían University at the institution of the principal investigator and lead author. This protocol was conducted in accordance with the research ethics guidelines established in the Declaration of Helsinki.
Anthropometry
Body weight, height, and waist circumference were measured in light clothing, without shoes, using a Seca 700 weight scale with a stadiometer included (100 g and 0.5 cm sensitivity, respectively) [19]. Body mass index (BMI) was quantified by weight in kilograms divided by height in meters squared. Weight status was determined using BMI cut-offs based on criteria defined by the world health organization. Participants were classified as normal-weight, overweight or obese if their BMI values were ≤ 24.9 kg/m2, ≥ 25.0–29.9 kg/m2, or ≥ 30.0 kg/m2, respectively [20]. Waist circumference was measured using a tape (Seca 201) placed between the lowest border of rib cage and the higher border of iliac crest, at the end of normal expiration. Hip circumference was measured at the widest part of the hip at the level of the greater trochanter. All measurements were in centimeters (cm) to the nearest decimal [21].
Body composition was assessed after an overnight fast at 9 AM using foot-to-foot bioelectrical impedance according to the manufacturer’s guidelines with a Tanita TBF-300MA (Tanita Corporation, Tokyo, Japan).
Eating behavior
Three validated questionnaires were used to assess eating behavior: (1) three Factor Eating Behaviour Questionnaire: this 18-item instrument evaluates three components of eating behavior; cognitive restraint (CR), emotional eating (EE), and uncontrolled eating (UE). Participants rate their degree of agreement on each item using a 4-point likert scale. Standardized scores for each subscale were calculated as the average results of summing individual raw scores divided by the number of items in each subscale [22]. In the current study, all subscales showed moderate-to-strong internal consistency, with Cronbach-alpha values ranging from 0.60 to 0.88 [23].
Food Reinforcement Value Questionnaire (FRVQ)
The FRVQ is a 12-item questionnaire that assesses the relative reinforcing value of food in relation to an alternative reinforcer. In this task, we assessed participants’ motivation to work towards obtaining either their most preferred palatable snack food or their highest rated healthy alternative (fruits/vegetables). Work was defined as button presses in this paradigm, with greater button presses reflecting greater relative reinforcing value of food. A fixed ratio schedule was employed on the first item, meaning participants were required to press the button on a joystick 20 times to gain access to either snack food or their the fruit/vegetable of their choice. For the remaining items, the reinforcement schedule increased by 20 button presses for access to preferred snack food to a maximum of 240 presses on item 12, whereas the reinforcement schedule to gain access to preferred fruits/vegetables remained fixed at 20 button presses for all 12 items. The highest number of button presses for snack food choices represented the relative reinforcing value of snack food and was expressed us % food choice. This questionnaire has been validated against the gold-standard computerized program in adults [24], and shown to predict weight gain over time, indicating good predictive validity [25].
24-h diet recall
Total energy intake, macronutrient consumption, fiber, saturated, monounsaturated and polyunsaturated fatty acid (PUFA), total n-6 PUFA, total n-3 PUFA were evaluated on each participant using 24-h diet recalls on randomly selected days by a staff nutritionist. Twenty-four-hour recalls assess energy intake by considering detailed food descriptions, including brand names, ingredients, methods of food preparation, and portion sizes [26]. The 24-h recalls for each patient were analyzed using Food Processor w/PS 10.15.
Yale Food Addiction Scale (YFAS)
This 25-item questionnaire assesses symptoms of dependence on highly palatable food (i.e., high fat and/or high-carbohydrate), and has been adapted from the substance dependence criteria as defined by the DSM-IV criteria. Consistent with this criteria, the YFAS requires the concomitant presence of clinically elevated levels of distress for a diagnosis of food addiction. In addition, symptoms of food addiction were also be measured continuously, with greater scores reflecting greater proneness to food addiction. This tool has been well validated recently in a population of Chilean adults by Obregon and colleagues [27], after the initial development and validation by Gearhardt et al. [28].
Collection of biologic samples
Blood samples were collected after an overnight fast by a registered nurse using a standard vacuum system protocol, in tubes with EDTA-K3 as an anticoagulant for molecular analysis. For molecular analysis, blood was collected into a 4-mL EDTA-coated tube. Plasma was separated from the buffy coat and red blood cells after centrifugation of the EDTA-coated tube at 3300 rpm for 10 min at room temperature. The DNA from each blood sample was extracted with the QIAGEN QIAamp DNA blood mini kit #51104 according to the manufacturer’s instructions [29].
Genetic analysis of ANKK1 gene (DRD2)
The TaqI A1 single nucleotide polymorphism (SNP; rs1800497; Accession Number: NP_848605.1) is located downstream from the DRD2 gene in the ANKK1 region gene [30]. The genotype of the common variant TaqI A1 rs1800497 (C > T) [T or A1; risk alleles] were determined with a predesigned Taqman assay ID C___7486676_10 (Applied Biosystems) that allows for genotype discrimination using the real-time thermocycler ABI-Stepone.
Statistical methods
Descriptive statistics were used to characterize the sample. Genotype and allele frequencies were estimated and Hardy–Weinberg equilibrium was evaluated based on a goodness-of-fit χ2-test. Group differences and associations between variables of interest were evaluated using non-parametric statistics (Mann–Whitney test and Kruskal–Wallis tests), including sex-specific analyses.
Results
Anthropometric and metabolic measures
Anthropometric and metabolic measurements are listed in Table 1. We recruited 221 adults in the whole sample (44% normal weight; 11.9% overweight; 43% obese). As expected, females had higher levels of total body fat in relation to males (34.8 ± 9.4%; 23.7 ± 9.7%). We found higher systolic and diastolic blood pressure in males in relation to females (p < 0.05). No sex differences were found in total cholesterol and glucose (Table 1).
Eating behavior
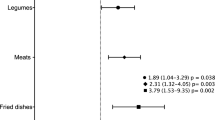
In relation to eating behavior scores, we found that females reported higher scores of the Emotional Eating scale compared to males (p < 0.01). Additionally, women showed higher relative reinforcing value of snack food compared to men (female: 20.9 ± 24.5%; male 14.1 ± 18.8%, p = 0.05) and lower total intake of energy, protein, carbohydrates, fiber, lipids, MUFA, cholesterol, and calcium (Table 2).
When data were analyzed by weight status, compared to normal-weight adults, obese adults showed higher scores of emotional eating and uncontrolled eating scales, as well as higher intake of lipids compared to overweight (p < 0.05) Table 3.
Association between TaqI A1 and food addiction
The genotype and allele frequencies for the genetic variant of the rs1800497 was estimated. The genotype distribution was A2/A2 (CC) = 56.4%; A1/A2 (CT) = 33.6%; A1/A1 (TT) = 9.9%. The genotype distribution of the study sample did not deviate significantly from the Hardy–Weinberg equilibrium (p value = 0.06) (Supplementary Table 1). Allele frequencies were estimated as 73.2% for the C allele and 26.7% for the T allele. When the whole sample was analyzed, no significant differences were found by genotype adjusted by sex, for anthropometric variables.
Twenty-two percent of the participants met the criteria for food addiction. Women had higher prevalence than men (26% and 10.7%, respectively; p = 0.01). There was a higher prevalence in obese individuals (p < 0.01; Supplementary Table 2). There was an association between the UE score and food addiction (r = 0.4; p < 0.0001). In addition, a 1-unit increase in the UE scale was associated with a 19% additional risk of diagnosis for food addiction (OR 1.19, p value = 0.004).
There was no association between the DRD2 genotype and diagnosis of food addiction (p = ns). In the analysis of data by carrier/non-carrier condition, there was no association between food addiction and carrying the risk allele (p = ns).
Genetics and eating behavior
As shown in Table 4, carriers of the risk allele (A1/A2) reported significantly greater relative reinforcing value of snack food compared to non-carrriers (A1/A1) when collapsed across sex and weight status. However, carriers of the A1/A1 showed significantly lower energy intake in relation to carriers of the A1A2 and A2A2 alleles (1418.0 ± 296.0 vs 1643.4 ± 435.1 and 1637.1 ± 375.4, respectively).
Tables 5 and 6 show analyses stratified by sex and weight status for eating behavior scores calculated from the TFEQ, RVFQ, and 24HR energy intake by carrier status of the alternative allele. In the sex-specific analysis, we observed that obese female A1 carriers, showed higher scores compared to non-carriers on the Emotional Eating subscale and on snack food reinforcement Questionnaire (p < 0.05). In addition, they exhibit significantly lower protein and w3 fatty acids intake. Normal weight male A2 carriers showed lower cholesterol intake and obese carriers showed higher protein intake in relation to non-carriers (p < 0.05).
Discussion
Monozygotic (MZ) and dizygotic (DZ) twins studies have recognized a strong genetic influence in obesity and anthropometric measurements [31], rate of consumption [32], macronutrient preference [33], eating attitudes [34], frequency of eating, and many eating behavior traits such as satiety response, responsiveness and enjoyment of food [35]. Knowing the strong genetic contribution in eating behavior, combined with research in adults showing that dopamine signaling is associated with increased food reinforcement, energy intake and obesity [36], we evaluated the influence of the TaqI A1 polymorphism on eating behavior, food reinforcement and food addiction in Chilean adults to fill an important research gap. In relation to genetic variants in the dopamine pathway, there is a lack of studies that have focused on the effects of TaqI A1 genetic variant (ANKK1/DRD2) on food addiction and the current study provides the first evidence in a South America population.
Our study did not find an association between TaqI A1 risk allele and food addiction, either in the overall sample, or when stratified by sex and weight status. Although no other study has examined this allele in relation to food addiction, Yeh et al. found differences in food cravings of carbohydrates and fast food assessed with the Food Craving Inventory between the A1 and A2 carriers among female Asian college students. They also showed there was a difference between carriers and non-carriers of these alleles on a measure of appetite drive to consume highly palatable foods from Power of Food questionnaire [37]. Given food addiction is prevalent in obese samples and believed to contribute to overconsumption of food and subsequent weight gain, future research with larger samples is needed to better understand the relationship between dopamine signaling and food addiction.
Our study documents some important gene-enviroment relationships as they relate to eating behavior. When the complete sample was analyzed, carriers of the risk allele (A1/A2) reported greater snack food reinforcement and lower energy intake than non-carriers. Moreover, when we stratified by carrier status and sex, in females we observed that A1 carriers with obesity had higher scores on Emotional Eating and snack food reinforcement. The emotional eating traits captures the failure to control food intake in a context of experiencing negative emotions and snack food reinforcement is a quantitative measure reflecting how hard someone is motivated to work to gain access to snack food in relation to a healthier food alternative [38]. These results are consistent with some findings from studies performed in American adults. Specifically, Epstein et al. [36] showed that food reinforcement was greater in obese than in non-obese individuals, and these differences were especially prominent in obese carriers of the TaqI A1 allele. Additionally, those participants with high levels of food reinforcement that were carriers of the risk allele (A1/A1-A1/A2) had higher energy intake in an ad-libitum feeding situation. Additionally, Felsted et al. combined genetic and neuroimaging techniques in adults [39]. Using magnetic resonance imaging, they evaluated neural responses after intake of a palatable milkshake in carriers and non-carriers of the TaqI A1 allele. They observed an interaction between genotype and stimuli in the midbrain, thalamus, and OFC, where TaqI A1 carriers showed a diminished neural response to a milkshake compared to a tasteless solution, consistent with the dopamine reward deficiency syndrome. Relatedly, given the evidence that alcohol and sucrose stimulate the same reward pathway (dopaminergic system), Jablonski et al. examined the influence of the TaqI A1 allele on the preference of increasing sucrose concentration in men with alcohol dependence. They found an association between the presence of the risk allele of the TaqI A1 and sucrose preference. More specifically, the A1/A2 risk allele was found more frequently in sweet likers compared to sweet dislikers [40]. Furthermore, Stice et al. showed that a lower caudate response predicted body fat gain in adolescents carrying TaqI A1 allele (less dopamine signaling) [41]. All these results show that TaqI A1 carriers may have a blunted response to reward and therefore may show a compensatory stronger drive to ingest palatable foods. This is consistent with the known relation between reduced DRD2 receptor density and TaqI A1 carriers, and with a study that found reduced brain volume in the sustancia nigra, which contain dopamine cell bodies, in carriers of the TaqI A1 allele [42]. It has been established that obese individuals have a reduced number of dopamine receptors in the stratium region compared to normal weight subjects, and that higher food intake could be a way to balance the hypodopaminergic state, thus promoting obesity development [41, 43]. In contrast, recent findings show that elevated reward activation in response to food cues predicted future body fat gain in adolescent carriers of the A2/A2 allele and lower reward activation predicted body fat gain for those with A1/A1 allele, establishing that too much or too little dopamine signaling and reward region responsivity may increase risk for overeating and obesity [44].
This study has many strengths and limitations that warrant mention. It is possible that some of our null findings regarding the relationship between TaqI A1 dopamine alleles and food addiction and eating behavior were due to limited sample size, most notably considering the smaller than expected number of adults with the diagnosis. In addition, this lack of association could be explained by the fact that there is some evidence indicating that individual polymorphic loci normally contribute only a small proportion of phenotypic variance and that their independent effects typically do not reach statistical significance. A quantitative genetic approach comprised of multiple DA SNP to form a a multilocus genetic risk profile may be more predictive of eating behavior and obesity. Also, it is possible that the effects of dopamine genes may not be fully expressed on certain eating behavior traits such us food addiction, thus future research is needed. In our study the results of the 24-h dietary recall were not consistent with the participants' BMI status, but these findings could be due to the well-documented recall bias due to the reliance on respondents’ memory of energy intake. We tried to minimize this bias using a well-trained dietitian to conduct the food recall interviews over randomly selected days as suggested to obtain valid measures of free-living energy intake, but this bias cannot be eliminated.
Also the sample obtained was based on convenience so results cannot be generalized to all Chilean adults.
These methodological limitations are balanced by several strengths, including the current study representing the first to examine the relationship between dopamine genes and food addiction in Chilean population. Additionally, we used four tools (TFEQ, FRVQ, YAFS and 24HR) which assessed a broad scope of eating behavior traits, all of which have been shown to possess strong validity and reliability [24, 27, 45].
In conclusion, although we did not find associations with food addiction by dopamine genotype in the whole sample, when data were stratified by sex and weight status, our results show that the TaqI A1 allele may play an important role on some eating behavior traits such emotional overeating, food reinforcement, and energy intake, and that women with obesity who are carriers may be at greater risk. These findings could be applied in the understanding of how TaqI A1 genetic variant interact with food addiction and nutritional status in adults. These results could help the clinical community in the understanding of a possible predisposition to food addiction and obesity.
Future research using both cross-sectional and prospective designs are needed to replicate and extend these findings to determine if these relationships are maintained or become stronger over time to better identify adults at highest risk of obesity, information that will inform obesity prevention strategies.
What is already known on this subject?
The rs1800497 variant has been associated with eating behavior, lower DRD2 density, higher weight, food reinforcement, but the relation to food addiction remain unclear.
What this study adds?
Our study does not support a relation between rs1800497 and food addiction, but support that female A—carriers show higher scores of emotional eating and snack food reinforcement.
Abbreviations
- DA:
-
Dopamine
- DRD2:
-
Dopamine 2 receptor
- BMI:
-
Body mass index
- TFEQ:
-
Three Factor Eating Questionnaire
- FRVQ:
-
Food Reinforcement Value Questionnaire
- YFAS:
-
Yale Food Addiction Scale
- SNP:
-
Single nucleotide polymorphisms
- ANKK1:
-
Ankyrin repeat domain containing 1 gene
- OFC:
-
Orbitofrontal cortex
References
Karnik S, Kanekar A (2012) Childhood obesity: a global public health crisis. Int J Prev Med 3(1):1–7
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC et al (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 30–384(9945):766–781. https://doi.org/10.1016/S0140-6736(14)60460-8
http://www.minsal.cl/wp-content/uploads/2017/11/ENS-2016-17_PRIMEROS-RESULTADOS.pdf
Pursey KM, Stanwell P, Gearhardt AN, Collins CE, Burrows TL (2014) The prevalence of food addiction as assessed by the Yale Food Addiction Scale: a systematic review. Nutrients 6(10):4552–4590. https://doi.org/10.3390/nu6104552
Leigh SJ, Morris MJ (2018) The role of reward circuitry and food addiction in the obesity epidemic: an update. Biol Psychol 131:31–42. https://doi.org/10.1016/j.biopsycho.2016.12.013
Hebebrand J, Albayrak Ö, Adan R, Antel J, Dieguez C, de Jong J, Leng G, Menzies J, Mercer JG, Murphy M, van der Plasse G, Dickson SL (2014) “Eating addiction”, rather than “food addiction”, better captures addictive-like eating behavior. Neurosci Biobehav Rev 47:295–306. https://doi.org/10.1016/j.neubiorev.2014.08.016
Olsen CM (2011) Natural rewards, neuroplasticity, and non-drug addictions. Neuropharmacology 61(7):1109–1122. https://doi.org/10.1016/j.neuropharm.2011.03.010
Brownell KD, Gold MS (2012) Food and addiction: a comprehensive handbook. Oxford University Press, Oxford
Tg R (1956) The descriptive features of food addiction; addictive eating and drinking. Q J Stud Alcohol 17(2):198–224
Fortuna JL (2012) The obesity epidemic and food addiction: clinical similarities to drug dependence. J Psychoact Drugs 44(1):56–63
Avena NM, Rada P, Hoebel BG (2009) Sugar and fat bingeing have notable differences in addictive-like behavior. J Nutr 139(3):623–628
Volkow ND, Wang GJ, Baler RD (2011) Reward, dopamine and the control of food intake: implications for obesity. Trends Cogn Sci 15(1):37–46
Cameron JD, Chaput JP, Sjödin AM, Goldfield GS (2017) Brain on fire: incentive salience, hedonic hot spots, dopamine, obesity, and other hunger games. Annu Rev Nutr 37:183–205
Kessler RM, Zald DH, Ansari MS, Li R, Cowan RL (2014) Changes in dopamine release and dopamine D2/3 receptor levels with the development of mild obesity. Synapse 68(7):317–320
Blum K, Sheridan PJ, Wood RC, Braverman ER, Chen TJH, Cull JG et al (1996) The D2 dopamine receptor gene as a determinant of reward deficiency syndrome. J R Soc Med 89:396–400
Munafò MR, Matheson IJ, Flint J (2007) Association of the DRD2 gene Taq1A polymorphism and alcoholism: a metaanalysis of case-control studies and evidence of publication bias. Mol Psychiatry 12:454–546
Noble EP, Blum K, Khalsa ME, Ritchie T, Montgomery A, Wood RC et al (1993) Allelic association of the D2 dopamine receptor gene with cocaine dependence. Drug Alcohol Depend 33(3):271–285
Connor JP, Young RM, Lawford BR, Saunders JB, Ritchie TL, Noble EP (2007) Heavy nicotine and alcohol use in alcohol dependence is associated with D2 dopamine receptor (DRD2) polymorphism. Addict Behav 32(2):310–319
Gordon C, Chumlea C, Roche A (1991) Stature, recumbent length, and weight. In: Lohman T, Roche Martorell R (eds) Anthropometric standardization reference manual. Human Kinetics Books, Champaign, Ill, USA, pp 3–8
Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults (1998). https://www.nhlbi.nih.gov/files/docs/guidelines/ob_gdlns.pdf
Lemieux S, Prud’homme D, Bouchard C, Tremblay A, Despres J (1996) A single threshold value of waist girth identifies normal-weight and overweight subjects with excess visceral adipose tissue. Am J Clin Nutr 64:685–693
Tholin S, Rasmussen F, Tynelius P, Karlsson J (2005) Genetic and environmental influences on eating behavior: the Swedish Young Male Twins Study. Am J Clin Nutr 81(3):564–569
Tavakol M, Dennick R (2011) Making sense of Cronbach’s alpha. Int J Med Educ 2:53–55. https://doi.org/10.5116/ijme.4dfb.8dfd
Goldfield GS, Epstein LH, Davidson M, Saad F (2005) Validation of a questionnaire measure of the relative reinforcing value of food. Eat Behav 6(3):283–292
Hill C, Saxton J, Webber L, Blundell J, Wardle J (2009) The relative reinforcing value of food predicts weight gain in a longitudinal study of 7–10-y-old children. Am J Clin Nutr 90(2):276–281
Vereecken CA, Covents M, Sichert-Hellert W, Alvira JM, Le Donne C, De Henauw S et al (2008) Development and evaluation of a self-administered computerized 24-h dietary recall method for adolescents in Europe. Int J Obes 32(5):S26-34
Obregón A, Fuentes J, Pettinelli P (2005) Association between food addiction and nutritional status in Chilean college students. Rev Med Chile 143(5):589–597. https://doi.org/10.4067/S0034-98872015000500006
Gearhardt AN, Corbin WR, Brownell KD (2009) Preliminary validation of the Yale Food Addiction Scale. Appetite 52(2):430–436. https://doi.org/10.1016/j.appet.2008.12.003
Qiagen . QIAamp® DNA Investigator Handbook; Hilden, Germany, Qiagen 2010
Neville MJ, Johnstone EC, Walton RT (2004) Identification and characterization of ANKK1: a novel kinase gene closely linked to DRD2 on chromosome band 11q23.1. Hum Mutat 23(6):540
Llewellyn C, Wardle J (2015) Behavioral susceptibility to obesity: gene–environment interplay in the development of weight. Physiol Behav 1(152):494–501
Rankinen T, Bouchard C (2006) Genetics of food intake and eating behavior phenotypes in humans. Annu Rev Nutr 26:413–434
Smith AD, Fildes A, Cooke L, Herle M, Shakeshaft N, Plomin R, Llewellyn C (2016) Genetic and environmental influences on food preferences in adolescence. Am J Clin Nutr 104(2):446–453. https://doi.org/10.3945/ajcn.116.133983
Obregón AM, Valladares M, Goldfield G (2017) Association of the dopamine D2 receptor rs1800497 polymorphism and eating behavior in Chilean children. Nutrition 35:139–145. https://doi.org/10.1016/j.nut.2016.11.005 (Epub 2016 Dec 7)
Obregón AM, Oyarce K, Santos JL, Valladares M, Goldfield G (2017) Association of the melanocortin 4 receptor gene rs17782313 polymorphism with rewarding value of food and eating behavior in Chilean children. J Physiol Biochem 73(1):29–35. https://doi.org/10.1007/s13105-016-0521-5 (Epub 2016 Oct 11)
Epstein LH, Temple JL, Neaderhiser BJ, Salis RJ, Erbe RW, Leddy JJ (2007) Food reinforcement, the dopamine D2 receptor genotype, and energy intake in obese and nonobese humans. Behav Neurosci 121(5):877–886
Yeh J, Trang A, Henning SM, Wilhalme H, Carpenter C, Heber D, Li Z (2016) Food cravings, food addiction, and a dopamine-resistant (DRD2 A1) receptor polymorphism in Asian American college students. Asia Pac J Clin Nutr 25(2):424–429. https://doi.org/10.6133/apjcn.102015.05
Kong KL, Feda DM, Eiden RD, Epstein LH (2015) Origins of food reinforcement in infants. Am J Clin Nutr 101(3):515–522. https://doi.org/10.3945/ajcn.114.093237
Felsted J, Ren X, Chouinard Decorte F, Small D (2010) Genetically determined differences in brain response to a primary food reward. J Neurosci 30(7):2428–243.41
Jabłoński M, Jasiewicz A, Kucharska-Mazur J, Samochowiec J, Bienkowski P, Mierzejewski P et al (2013) The effect of selected polymorphisms of the dopamine receptor gene DRD2 and the ANKK-1 on the preference of concentrations of sucrose solutions in men with alcohol dependence. Psychiatr Danub 25(4):371–378
Stice E, Spoor S, Bohon C, Small DM (2008) Relation between obesity and blunted striatal response to food is moderated by TaqIA A1 allele. Science 322(5900):449–452
Cerasa A, Gioia MC, Tarantino P, Labate A, Arabia G, Annesi G et al (2009) The DRD2 TaqIA polymorphism associated with changed midbrain volumes in healthy individuals. Genes Brain Behav 8(4):459–463
Comings D, Blum K (2000) Reward deficiency syndrome: genetic aspects of behavioral disorders. Prog Brain Res 126:325–341
Stice E, Burger KS, Yokum S (2015) Reward region responsivity predicts future weight gain and moderating effects of the TaqIA allele. J Neurosci 35(28):10316–10324. https://doi.org/10.1523/JNEUROSCI.3607-14.2015
Vega JA, Salazar G, Hodgson MI, Cataldo LR, Valladares M, Obregón AM, Santos JL (2016) Melanocortin-4 receptor gene variation is associated with eating behavior in Chilean adults. Ann Nutr Metab 68(1):35–41. https://doi.org/10.1159/000439092
Acknowledgements
The authors acknowledge the help of the entire team of the San Sebastían University, Chile.
Funding
This study was supported by the National Fund of Scientific and Technological Development (Fondo Nacional de Desarrollo Científico y Tecnológico—FONDECYT Grants 11130200), CONICYT and San Sebastián University Grants (Research Grant 2015-0007I).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Research Scientific Ethics Committee of San Sebastían University.
Informed consent
Written consent was obtained from each participant.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Obregón, A.M., Oyarce, K., García-Robles, M.A. et al. Association of the dopamine D2 receptor rs1800497 polymorphism with food addiction, food reinforcement, and eating behavior in Chilean adults. Eat Weight Disord 27, 215–224 (2022). https://doi.org/10.1007/s40519-021-01136-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-021-01136-1