Abstract
Purpose
Sleep duration has emerged as a crucial factor affecting body weight and feeding behaviour. The aim of our study was to explore the relationship among sleep duration, body composition, dietary intake, and quality of life (QoL) in obese subjects.
Methods
Body composition was assessed by DXA. “Sensewear Armband” was used to evaluate sleep duration. SF-36 questionnaire was used to evaluate quality of life (QoL). A 3-day dietary record was administered. Subjects were divided into 2 groups: sleep duration > and ≤300 min/day.
Results
137 subjects (105 women and 32 men), age: 49.8 ± 12.4 years, BMI: 38.6 ± 6.7 kg/m2, were enrolled. Sleep duration was ≤300 min in 30.6 % of subjects. Absolute and relative fat mass (FM) (40.5 ± 9 vs. 36.5 ± 9.1 kg; 40.2 ± 4.7 vs. 36.9 ± 5.6 %), and truncal fat mass (19.2 ± 6.1 vs. 16.6 ± 5 kg; 38.6 ± 5.3 vs. 35.2 ± 5.5 %) were higher in subjects sleeping ≤300 min when compared to their counterparts (all p < 0.05), whereas just a tendency towards a higher BMI was observed (p = 0.077). Even though energy intake was not different between groups, subjects sleeping ≤300 min reported a higher carbohydrate consumption per day (51.8 ± 5.1 vs. 48.4 ± 9.2 %, p = 0.038). SF-36 total score was lower in subjects sleeping ≤300 min (34.2 ± 17.8 vs. 41.4 ± 12.9, p = 0.025). Sleep duration was negatively associated with FM (r = −0.25, p = 0.01) and SF-36 total score (r = −0.31, p < 0.001). The inverse association between sleep duration and SF-36 total score was confirmed by the regression analysis after adjustment for BMI and fat mass (R = 0.43, R 2 = 0.19, p = 0.012).
Conclusion
Reduced sleep duration negatively influences body composition, macronutrient intake, and QoL in obese subjects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last years, accumulating evidence focused on sleep and its association with health status [1, 2]. Sleep duration has emerged as a crucial factor affecting body weight and feeding behaviour [3, 4]. From a number of epidemiological studies, reduced sleep appears to be linked to obesity [4, 5], even though a causal relationship has not been described yet. Moreover, sleep curtailment resulted to be associated with changes in hormones regulating appetite (e.g. ghrelin and leptin) [6]. In prior studies also food intake was affected by sleep deficiency, but results were conflicting in terms of choice of foods and excess of macronutrients [7]. In many studies, food intake was evaluated in a scarcely physiological environment, performing sleep manipulation (partial sleep restriction) in a laboratory setting [7–9]. Furthermore, the use of the self-reported duration of sleep represents another important limitation in terms of quality of the data. On the other hand, the results from the literature are not conclusive because of differences in the study design as well as in the study population (gender, age class or ethnicity differences) [8, 9].
A relationship was found between insufficient sleep and metabolic disorders, such as insulin resistance and type 2 diabetes [10]. Obesity is associated per se to reduced quality of life [11]. Araghi et al. found that poor sleep quality was independently inversely related to quality of life in subjects with extreme obesity [12]. The aim of our study was to explore the relationship among sleep duration, body composition, dietary intake, and quality of life (QoL) in obese subjects.
Methods
Study participants were recruited among subjects referring to the CASCO High Specialization Center for the Care of Obesity at the Department of Experimental Medicine, Sapienza University of Rome, Italy, from January 2014 to June 2015.
The following inclusion criteria were considered: age >18 and <65 years, body mass index (BMI) ≥30 kg/m2, ethnicity: Caucasian Italian subjects.
As exclusion criteria, we considered: any malignant disease during the last 5 years, any inflammatory or autoimmune disease, corticosteroids for systemic use, any medication potentially affecting body weight or body composition, syndromic obesity, participation in a reducing-weight programme in the last 3 months, renal failure, heart failure, any type of diabetes, history of viral or autoimmune liver disease or any other chronic liver disease, excessive alcohol intake (>140 g/week for men and 70 g/week for women), night-shift work, any central nervous system medication.
The study protocol was approved by the Ethical Committee of the “Sapienza” University of Rome and written informed consent was obtained from all participants.
All subjects underwent a complete physical examination. Body weight, height, waist circumference were measured following standardized procedures [13]. The same tools were used in all subjects: a SECA scale 86 (200 kg, to an accuracy of 0.1 kg, certified and homologated as class III), a flexible metallic tape (200 cm, to an accuracy of 0.1 cm), a telescopic stadiometer (200 cm; to an accuracy of 0.1 cm). Body mass index (BMI) was calculated as body weight (kg) divided by height squared (m2). Obesity was defined as BMI ≥30 kg/m2. Fat mass and fat-free mass were assessed by dual-energy X-ray absorptiometry (DXA) (Hologic 4500 RDR), with coefficient of variation of <1.5 % for fat mass and fat-free mass [14].
All participants wore a multisensory body monitor, the SenseWear Pro 2 Armband (BodyMedia, Inc., Pittsburgh, PA, USA) on the triceps muscle of their right arm, at the midpoint between the acromion and olecranon processes [15]. Using algorithms developed by the manufacturer, sleep duration was obtained.
A 3-day dietary record was completed by all participants, following the instructions provided by a trained dietician. Dietary data from the food records were entered into a food analysis software to calculate the total daily intake of energy, fat, protein, and carbohydrate, according with the Italian Food Composition tables [16].
The Short-Form-36 (SF-36) questionnaire was used to evaluate the health-related quality of life [17]. The SF-36 measure is a 36-item self-completed questionnaire exploring 8 dimensions of health: physical functioning, role limitation due to physical problems, role limitation due to emotional problems, social functioning, mental health, energy/vitality, bodily pain and general health perceptions. The 36 items are grouped into two summary measures, the physical composite score (PCS) and the mental composite score (MCS). The scores of the scales range between 0 and 100, with higher scores reflecting greater health-related quality of life, while PCS and MCS are norm-based scores with a mean of 50 and a standard deviation of 10.
Short sleep duration was defined as less or equal than 300 min/day (or “short sleepers”). Study subjects were divided into two groups on the basis of sleep duration: > or ≤300 min/day.
Statistical analysis
After verification of the normal distribution of the variables, the Student’s t test was performed for the comparison of means. Linear regression analysis was performed to verify the association among continuous variables. Differences were considered to be statistically significant for p < 0.05. Statistical analysis was performed using SPSS 10.0 statistical software (SPSS Inc. Wacker Drive, Chicago, IL, USA).
Results
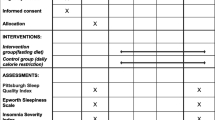
137 subjects (105 women and 32 men), mean age: 49.8 ± 12.4 years, mean BMI: 38.6 ± 6.7 kg/m2, were enrolled. Sleep duration was ≤300 min in 30.6 % of subjects. In Table 1, data concerning anthropometric characteristics, dietary intake, and health-related quality of life, are summarized. Absolute and relative fat mass (40.5 ± 9 vs. 36.5 ± 9.1 kg; 40.2 ± 4.7 vs. 36.9 ± 5.6 %), and truncal fat mass (19.2 ± 6.1 vs. 16.6 ± 5 kg; 38.6 ± 5.3 vs. 35.2 ± 5.5 %) were higher in subjects sleeping ≤300 min when compared to their counterparts (all p < 0.05), whereas just a tendency towards a higher BMI was observed (p = 0.077). Even though energy intake was not different between groups, subjects sleeping ≤300 min reported a higher carbohydrate consumption per day (51.8 ± 5.1 vs. 48.4 ± 9.2 %, p = 0.038). SF-36 total score was lower in subjects sleeping ≤300 min (34.2 ± 17.8 vs. 41.4 ± 12.9, p = 0.025). The PCS was significantly lower (p = 0.045), whereas the MCS was not significantly different, in subjects with short sleep duration than subjects sleeping more than 300 min/day.
Sleep duration was negatively associated with fat mass (r = −0.25, p = 0.01) and SF-36 total score (r = −0.31, p = <0.001). The inverse association between sleep duration and SF-36 total score was confirmed by the regression analysis after adjustment for BMI and fat mass (R = 0.43, R 2 = 0.19, p = 0.012).
Discussion
Even though mounting evidence has shown the association linking sleep duration and obesity, in the majority of the extant studies the BMI and/or waist circumference were used as indicators of adiposity [5]. In addition, different measures of sleep duration were used, especially self-reported data or objectively measured data [5, 8, 10].
In the present study, using an actigraphic measure for sleep duration and measuring body composition by DXA, we found that in subjects sleeping equal or less than 5 h absolute and relative fat mass, and truncal fat mass were significantly increased, despite BMI was not significantly different between the two study groups.
Our results regarding total and visceral adiposity are in agreement with findings from the Québec Family Study [18], in which middle-aged, overweight and obese subjects with a self-reported sleep duration ranging from 5 to 6 h exhibited a greater BMI, body fat percentage, and a higher sum of the trunk skinfolds than their counterparts with a 7- to 8-h sleep time.
Similarly, Patel et al. found that in men and women aged 65 years or older, BMI was higher in those sleeping less than 5 h, as registered by wrist actigraphy [19]. Short sleepers had a higher waist circumference; in women body fat percentage and truncal body fat were also greater than those sleeping 7–8 h. Also in a young population of overweight individuals, BMI or body fat percentage were significantly augmented in case of an objectively measured sleep duration lower than 6 h [20].
Our observations are different from results in the above-mentioned studies with respect to BMI. In fact, in our study, in short sleepers absolute and relative fat mass, as well as central adiposity, were increased when compared to individuals sleeping more than 300 min, whereas difference lacked in terms of BMI. In a meta-analysis by Iftikhar et al., the odds ratio of having metabolic syndrome was 1.5 higher for a sleep duration lower than 5 h [21]. Our findings seem to parallel these results, as visceral adiposity is a stronger predictor of metabolic syndrome than BMI.
Nagai et al. found no significant association between reduced self-reported sleep duration and BMI in an adult Japanese population [22]; beyond the difference potentially linked to ethnicity, this may be actually due to the fact that a more precise evaluation of adiposity was not adopted, other than BMI.
In our study, even though energy intake was not significantly different, subjects sleeping less or equal than 5 h/night reported a higher carbohydrate consumption. Our data seem to be in agreement with findings by Nedeltcheva et al., in which overweight participants underwent bedtime restriction under controlled laboratory conditions: calorie consumption controlled for body weight was not significantly different after 5.5-h bedtime compared to 8.5-h bedtime; on the other hand, in the same study, energy intake from snack, and a subsequent greater carbohydrate intake were significantly higher after bedtime restriction [23].
In a recent meta-analysis including 9 European cohorts, the association between sleep duration and macronutrient intake emerged only in the age- and gender-adjusted analysis: in particular, self-reported sleep duration was significantly inversely associated with carbohydrate intake [24]. In line with this findings, Korean women sleeping less than 7 h per day reported an increased carbohydrate consumption, whereas Korean male short sleepers consumed higher amounts of fat [25].
Conversely, Patterson et al. showed that energy intake was increased in a mixed-ethnicity study population [26], as well as other authors found that the decreased sleep duration led to higher fat consumption [7]. Thus, with respect to energy and macronutrient ingestion, existing data are conflicting and further research is needed, using more stringent methodological choices.
In our study population, short sleepers exhibited a poorer health-related quality of life, as measured by SF-36 questionnaire, when compared to normal sleepers. On one hand, it is well known from a wealth of study that quality of life is affected by obesity [11, 27], as well as obstructive sleep apnoea syndrome, exacerbated by excess truncal fat, is responsible for both sleep disturbances and impaired quality of life in obese subjects [28]. On the other hand, studies investigating the effects of sleep on quality of life independently of other medical conditions are scarce [1]. In our analysis, the negative association between sleep duration and the SF-36 total score was maintained when adjusting for BMI and fat mass, suggesting that the inverse relationship between sleep duration and quality of life is not mediated by the presence of obesity. Our results are in agreement with the study by Nagai et al., in which self-related health was perceived as “not good” in a higher percentage of normal-weight Japanese subjects when considering sleep duration less or equal than 5 h per day [22]. Similar to findings in adults, Paiva et al. observed that in Portuguese adolescents with sleep deprivation, the health-related quality of life was significantly reduced, as well as health complaints were higher, affecting both pain complaints and emotional complaints [29]. In our study, just physical health-related quality of life was affected by sleep restriction, whereas no difference emerged in terms of mental health in short sleepers.
Some limitations to our study need to be considered. We did not prove a causative role of short sleep duration in the development of changes in body composition and dietary intake in subjects with obesity, and other potential determinants of this association need to be further investigated. Secondarily, dietary assessment based on dietary records may be biased by underreporting of energy and nutrient intake in obese individuals [30]. In addition, gender-related differences have to be investigated.
To conclude, the adiposity phenotype was influenced by short sleep duration, with a greater truncal fat mass in subjects sleeping less or equal than 5 h, even in absence of significant difference in terms of BMI. Short sleepers seemed to consume more carbohydrate, even though calorie consumption was not affected by sleep duration. Finally, in obese subjects a decreased sleep duration negatively influenced the health-related quality of life independently of total adiposity and body mass.
Sleep appears to play a pivotal role in adiposity distribution and dietary choices, influencing the global health status. Further research is needed to better characterize what are the metabolic mechanisms involved in the relationship between sleep and energy balance.
References
Frange C, de Queiroz SS, da Silva Prado JM, Tufik S, de Mello MT (2014) The impact of sleep duration on self-rated health. Sleep Sci 7:107–113. doi:10.1016/j.slsci.2014.09.006
Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH (2015) The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Med Rev 22:23–36. doi:10.1016/j.smrv.2014.10.001
Leger D, Bayon V, de Sanctis A (2015) The role of sleep in the regulation of body weight. Mol Cell Endocrinol. doi:10.1016/j.mce.2015.06.030
Chaput JP (2014) Sleep patterns, diet quality and energy balance. Physiol Behav 134:86–91. doi:10.1016/j.physbeh.2013.09.006
Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, Miller MA (2008) Meta-analysis of short sleep duration and obesity in children and adults. Sleep 31:619–626
Kim TW, Jeong JH, Hong SC (2015) The impact of sleep and circadian disturbance on hormones and metabolism. Int J Endocrinol 2015:591729. doi:10.1155/2015/591729
St-Onge MP (2013) The role of sleep duration in the regulation of energy balance: effects on energy intakes and expenditure. J Clin Sleep Med 9:73–80. doi:10.5664/jcsm.2348
Patel SR, Hu FB (2008) Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 16:643–653. doi:10.1038/oby.2007.118
Chen X, Beydoun MA, Wang Y (2008) Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity (Silver Spring) 16:265–274. doi:10.1038/oby.2007.118
Nedeltcheva AV, Scheer FA (2014) Metabolic effects of sleep disruption, links to obesity and diabetes. Curr Opin Endocrinol Diabetes Obes 21:293–298. doi:10.1097/MED.0000000000000082
Poggiogalle E, Di Lazzaro L, Pinto A, Migliaccio S, Lenzi A, Donini LM (2014) Health-related quality of life and quality of sexual life in obese subjects. Int J Endocrinol. 2014:847871. doi:10.1155/2014/847871
Araghi MH, Jagielski A, Neira I, Brown A, Higgs S, Thomas GN, Taheri S (2013) The complex associations among sleep quality, anxiety-depression, and quality of life in patients with extreme obesity. Sleep 36:1859–1865. doi:10.5665/sleep.3216
Lohman TJ, Roache AF, Martorell R (2002) 2002 Anthropometric standardization reference manual. Med Sci Sports Exerc 24:952
Heymsfield SB, Smith R, Aulet M, Bensen B, Lichtman S, Wang J et al (1990) Appendicular skeletal muscle mass: measurement by dual-photon absorptiometry. Am J Clin Nutr 52:214–218
Malavolti M, Pietrobelli A, Dugoni M, Poli M, Romagnoli E, De Cristofaro P, Battistini NC (2007) A new device for measuring resting energy expenditure (REE) in healthy subjects. Nutr Metab Cardiovasc Dis. 17:338–343
http://nut.entecra.it/646/tabelle_di_composizione_degli_alimenti.html
McHorney CA, Ware JE Jr, Raczek AE (1993) The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 31:247–263
Chaput JP, Després JP, Bouchard C, Tremblay A (2007) Short sleep duration is associated with reduced leptin levels and increased adiposity: Results from the Quebec family study. Obesity (Silver Spring). 15:253–261. doi:10.1111/j.1758-8111.2011.00027.x
Patel SR, Blackwell T, Redline S, Ancoli-Israel S, Cauley JA, Hillier TA, Lewis CE, Orwoll ES, Stefanick ML, Taylor BC, Yaffe K, Stone KL, Osteoporotic Fractures in Men Research Group, Study of Osteoporotic Fractures Research Group (2008) The association between sleep duration and obesity in older adults. Int J Obes (Lond) 32:1825–1834. doi:10.1038/ijo.2008.198
Wirth MD, Hébert JR, Hand GA, Youngstedt SD, Hurley TG, Shook RP, Paluch AE, Sui X, James SL, Blair SN (2015) Association between actigraphic sleep metrics and body composition. Ann Epidemiol 25:773–778. doi:10.1038/ijo.2008.198
Iftikhar IH, Donley MA, Mindel J, Pleister A, Soriano S, Magalang UJ (2015) Sleep duration and metabolic syndrome. An updated dose-risk metaanalysis. Ann Am Thorac Soc. 12:1364–1372. doi:10.1513/AnnalsATS.201504-190OC
Nagai M, Tomata Y, Watanabe T, Kakizaki M, Tsuji I (2013) Association between sleep duration, weight gain, and obesity for long period. Sleep Med 14:206–210. doi:10.1016/j.sleep.2012.09.024
Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, Penev PD (2009) Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr 89:126–133. doi:10.3945/ajcn.2008.26574
Dashti HS, Follis JL, Smith CE, Tanaka T, Cade BE, Gottlieb DJ et al (2015) Habitual sleep duration is associated with BMI and macronutrient intake and may be modified by CLOCK genetic. Am J Clin Nutr 101:135–143. doi:10.3945/ajcn.114.095026
Doo M, Kim Y (2015) Association between sleep duration and obesity is modified by dietary macronutrients intake in Korean. Obes Res Clin Pract. doi:10.1016/j.orcp.2015.08.010
Patterson RE, Emond JA, Natarajan L, Wesseling-Perry K, Kolonel LN, Jardack P, Ancoli-Israel S, Arab L (2014) Short sleep duration is associated with higher energy intake and expenditure among African-American and non-Hispanic white adults. J Nutr 144:461–466. doi:10.3945/jn.113.186890
Fontaine KR, Barofsky I (2001) Obesity and health-related quality of life. Obes Rev 2:173–182
Isidoro SI, Salvaggio A, Lo Bue A, Romano S, Marrone O, Insalaco G (2015) Effect of obstructive sleep apnea diagnosis on health related quality of life. Health Qual Life Outcomes. 13:68. doi:10.1186/s12955-015-0253-1
Paiva T, Gaspar T, Matos MG (2015) Sleep deprivation in adolescents: correlations with health complaints and health-related quality of life. Sleep Med 16:521–527. doi:10.1016/j.sleep.2014.10.010
Heitmann BL, Lissner L (1995) Dietary underreporting by obese individuals-is it specific or non-specific? BMJ 311:986–989
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
The study protocol was approved by the Ethical Committee of the ‘‘Sapienza’’ University of Rome
Informed consent
Written informed consent was obtained from all participants.
Rights and permissions
About this article
Cite this article
Poggiogalle, E., Lubrano, C., Gnessi, L. et al. Reduced sleep duration affects body composition, dietary intake and quality of life in obese subjects. Eat Weight Disord 21, 501–505 (2016). https://doi.org/10.1007/s40519-016-0254-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-016-0254-z