Abstract
Background and aims
Anorexia nervosa is an eating disorder characterized by food restriction, irrational fear of gaining weight and consequent weight loss. High mortality rates have been reported, mostly due to suicide and malnutrition. Good outcomes largely vary between 18 and 42 %. We aimed to assess outcome and prognostic factors of a large group of patients with anorexia nervosa. Moreover we aimed to identify clusters of prognostic factors related to specific outcomes.
Methods
We retrospectively reviewed data of 100 patients diagnosed with anorexia nervosa previously hospitalized in a tertiary level structure. Then we performed follow-up structured telephone interviews.
Results
We identified four dead patients, while 34 % were clinically recovered. In univariate analysis, short duration of inpatient treatment (p = 0.003), short duration of disorder (p = 0.001), early age at first inpatient treatment (p = 0.025) and preserved insight (p = 0.029) were significantly associated with clinical recovery at follow-up. In multiple logistic regression analysis, duration of first inpatient treatment, duration of disorder and preserved insight maintained their association with outcome. Moreover multiple correspondence analysis and cluster analysis allowed to identify different typologies of patients with specific features. Notably, group 1 was characterized by two or more inpatient treatments, BMI ≤ 14, absence of insight, history of long-term inpatient treatments, first inpatient treatment ≥30 days. While group 4 was characterized by preserved insight, BMI ≥ 16, first inpatient treatment ≤14 days, no more than one inpatient treatment, no psychotropic drugs intake, duration of illness ≤4 years.
Conclusions
We confirmed the association between short duration of inpatient treatment, short duration of disorder, early age at first inpatient treatment, preserved insight and clinical recovery. We also differentiated patients with anorexia nervosa in well-defined outcome groups according to specific clusters of prognostic factors. Our study might help clinicians to evaluate prognosis of patients with anorexia nervosa.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anorexia nervosa (AN) is an eating disorder occurring during adolescence, mostly among women [1]. High mortality rates have been reported [1–3]. Moreover, a statistically significant increase in mortality was documented in long-term follow-up studies [4]. One of the largest meta-analyses found the standardized mortality ratio (SMR) for AN, quantifying the increase or decrease in mortality with respect to the general population, was 5.86 [2]. SMR for unnatural causes of death during the first year after the first inpatient treatment was 19.3 and remained significantly high 20 years later [1]. Half of deaths were due to suicide, while other causes included alcohol abuse or medical consequences of marasmic malnutrition [5]. Short-term evaluations showed good outcomes ranging from 18 [6] to 42 % [7]. The 4-year or 5-year clinical recovery rate was higher and it was influenced by the duration of follow-up [8–11]. Nevertheless, several long-term studies by Fichter et al. [N = 103, follow-up = 12 years, mean body mass index (BMI) = 14.3 ± 1.6 years, mean age at onset = 18.5 ± 6.4 years] and Wentz et al. [N = 51, follow-up = 18 years, mean BMI = 22.4 ± 4.5 years, mean age at onset = 14 years] showed longer follow-up was not always associated with better outcome [12, 13]. Systematic meta-analysis showed, among surviving patients, less than one-half recovered on average, whereas one-third improved, and 20 % remained chronically ill [9].
Definitions of recovery in literature
Categories of recovery are important to researchers as they often serve as clinical endpoints for intervention [14]. Nevertheless, definition of recovery from AN still can vary, including only physical or also psychological and psychosocial aspects [14]. This can partly explain differences between recovery rates in different studies [14]. A single remission can be defined according to criteria set by Pike, criteria set by Kordy et al., the DSM-IV criteria [weight ≥ 85 % IBW, psychological symptoms within normal weight (EDE within 2SD of normal), absence of amenorrhea], different weight thresholds (85, 90 or 95 % ideal body weight), psychological symptoms measured by the Eating Disorder Examination Interview, and a combination of criteria (Morgan–Russell scale modified by Jeammet [15, 16]) [17]. The Morgan–Russell scale modified by Jeammet is currently one of the best-validated instruments in AN outcome research [13, 15, 16]. It explores three main areas of functioning: clinical (presence/absence of amenorrhea, binging/purging or restrictive behaviors, presence/absence of insight, relationship with food), working (employed/unemployed), social (presence/absence of sentimental and/or friend relationships, satisfaction in familial relationships). Patients are categorized as good (BMI ≥ 18.5 kg/m2 and regular menstruations), intermediate (BMI ≥ 18.5 kg/m2 or regular menstruations) or poor (BMI ≤ 18.5 kg/m2 and irregular or absent menstruations). Continuation of remission for a significantly longer period of time (from 8 consecutive weeks [18] to 1 year [19, 20]) defines recovery [14].
Possible causes of variation in outcome rates
Changes in diagnostic criteria between the 3rd and 4th edition of DSM [21, 22], including the absence of menstruation as a diagnostic criterion, and the 5th edition of DSM [23] could partly explain differences in outcome results. Nevertheless, Delle Grave et al. assessed that the criterion “amenorrhea” was of no clinical utility in the diagnosis and treatment of AN [24]. Indeed the majority of differences among patients with AN who did and did not meet the amenorrhea criterion appeared largely to reflect nutritional status [25]. Overall, the two groups had few psychological differences [25]. Furthermore, diagnostic crossover also leads to problems in clearly comparing outcomes within and between studies. Indeed, more than half of the patients cross over between the restricting and binge eating/purging AN subtypes over time, while one-third is crossing over to bulimia nervosa and are likely to relapse into AN [26]. Moreover, despite of a good outcome related to the eating disorders, patients frequently still display psychopathological changes (e.g. anxiety, depressive disorders, personality disorders, addiction) [27, 28].
Main prognostic factors in anorexia nervosa
Notably, weight and/or food preoccupation, body image disturbances and psychosexual problems remain a major concern and contribute to a risk of relapse [28, 29]. Indeed about one-third of patients with anorexia nervosa display post-remission relapse [29]. During the last years several follow-up studies tried to point out main prognostic factors [1, 2, 9–11, 19, 20, 29]. However, two large meta-analyses found that low BMI and older age at presentation, alcohol misuse [2], vomiting, bulimia, purgative abuse and chronicity of illness [9] were negative prognostic factors. Affective disorders and narcissistic, avoidant, borderline and obsessive personality disorders were also associated with poor outcome [9, 11]. Instead younger age at onset [2, 9] and longer duration of follow-up [9] and longer hospital stay at first inpatient treatment [2] were positive prognostic factors. Nevertheless, a recent population-based study failed to replicate prognostic factors previously identified, finding an association between premorbid depressive symptoms and poor outcome [19]. Moreover, Zerwas et al. found vomiting, impulsivity, and trait anxiety significantly predicted recovery [20]. However, others symptoms can affect quality of life of patients with anorexia nervosa, thus influencing the outcome [30]. Indeed, low self-reported vitality, high scores in eating control and a poor reported health status have also recently been associated with poor health-related quality of life in AN [30].
Despite the efforts made, prognostic factors in anorexia nervosa are still debated. Above all, clinical implications are often ambiguous. Isolated prognostic factors should be reconsidered in a larger perspective to find links between them. Indeed prognostic factors have never been aggregated to outline specific sub-groups of patients with anorexia nervosa. Thus, our study aimed: (1) to assess prognostic factors in our study population (2) to identify clusters of prognostic factors associated with different outcomes.
Methods
Study group and design
We retrospectively reviewed historical data of all patients diagnosed with AN at first inpatient treatment in the Eating Disorder Unit of the Department of Psychiatry of “Federico II” University of Naples between January 1990 and December 2012. The study was approved by the local Ethical Committee. Two points in time concerning evaluation were considered: (1) first inpatient treatment (2) follow-up telephone interview. Diagnosis of AN was made in consecutive unselected patients attending the Eating Disorder Unit of hospitalization, according to diagnostic criteria of the 3rd edition (from 1990 to 1994) and 4th edition (after 1994) of the Diagnostic and Statistical Manual of Mental Disorders (DSM) [21, 22]. During the inpatient treatment we obtained data concerning age at first inpatient treatment, age at onset, BMI, subtype of AN (restrictive or binging/purging), duration of inpatient treatment, presence of positive familiar history for psychiatric disorders, insight, psychotropic drugs intake. Inpatient treatment included case management, medical evaluation and management, nutrition counseling, and individual, family and group therapy. On January 2013 all eligible patients performed a follow-up telephone interview. The telephone interview was conducted by trained psychiatrists and included the 10 items of the Morgan–Russell scale modified by Jeammet [15, 16], exploring clinical, working and social domains. Each item was proposed with close questions and received a score from 1 to 4 (1 = satisfying; 2 = rather satisfying; 3 = unsatisfying; 4 = very satisfying). These data were then dichotomized (present/absent), as already described by other authors [18]. By means of telephone interviews we also retrospectively assessed number of inpatient treatments, duration of illness, duration of long-term inpatient treatment in private centers. Mortality data were confirmed by death certificates and by word of mouth by their relatives (parents or partners when married). All provided data were compared with those obtained during the inpatient treatment and were used to define the outcome.
Study design parameters
(1) “Onset of disorder” was defined as the beginning of weight loss. (2) We defined “follow-up period” as the period between first inpatient treatment and follow-up telephone interview. (3) The presence of “familial conflicts” was defined according to the evaluation of trained psychiatrists. (4) “Long-term inpatient treatment” was defined as more than 2 weeks of hospital stay.
Outcome parameters
(5) “Insight” was defined as self-awareness and self-understanding of attitudes, feelings, behavior, and disturbing symptoms. (6) We defined “duration of illness” the period between onset of disorder and clinical recovery or the period between onset of disorder and persistence of it at the moment of second evaluation. (7) “Clinical recovery” was defined as restoration of weight (BMI ≥ 18.5 kg/m2), menstruations, and the absence of binging and purging for at least 1 year prior to assessment [17].
Exclusion criteria
Exclusion criteria were intelligence quotient <85 and denied informed consent.
Measures
Overall outcome was based on the three measures of the Morgan–Russell scale modified by Jeammet [15, 16]. Individuals with overeating or vomiting (weekly or more) were assigned to the poor outcome group even if they had normal weight and menstrual cycles (Persistence of disorder) [31]. When a patient was dead due to AN, the outcome was considered as poor. However, to facilitate the analysis, the outcome was further dichotomized into “clinically recovered” and “not clinically recovered”. To make this division, the categories “intermediate” and “poor” were merged into the category “not clinically recovered”. Other authors have already successfully used this procedure [32].
Insight was assessed with The Patient’s Experience of Hospitalization (PEH) Scale [33]. This scale is a self-report instrument composed of 18 items. Participants were asked to rate the extent to which they agreed with each statement using a four-point Likert scale ranging from 0 (i.e., “do not agree at all”) to 3 (i.e., “agree completely”). This scale reflects predominant views about the hospitalization (need, aims) and the eating disorder (if and how the patient is worried about his condition). The internal consistency of the scale was 0.868 and the test–retest reliability was 0.81.
Statistical analyses
Univariate analysis and multiple logistic regression analysis
Due to the retrospective nature of our study, a univariate analysis was firstly used to identify those factors with a significant prognostic role in the outcome of anorexia. Independent t test or Mann–Whitney U test was used for quantitative variables, whereas Chi square test was used for categorical variables. Those factors that emerged as statistically significant in this step (p value less than 0.05) were then introduced as explanatory variables in a multiple logistic regression analysis, adjusted for the duration of follow-up, to assess their independent role as predictors of the outcome. In the logistic model, the dependent variable was the clinical outcome (dichotomized into “clinically recovered” and “not clinically recovered”); the whole set of explanatory variables is reported in Table 2. Results of the multiple logistic analysis are presented as adjusted Odds Ratio with 95 % confidence interval (95 % CI).
Multiple correspondence analyses and cluster analyses
The multidimensional approach of the second part of the analysis was aimed to identify groups of patients with homogeneous characteristics. At this aim, following the methodological approach of the French school of Analyse de Données [34], we categorized the original variables (based on that cut-point giving the maximum association between the dichotomized variable and the outcome). Then a new set of variables, obtained as linear combination of the original set of predictors, has been realized using the multiple correspondence analysis. These new factors, which represent a parsimonious description of the information held in the original variables, were used to carry out a hierarchical cluster analysis (HCA) using the Euclidean distance and Ward’s aggregation method. The number of factors used in the Cluster analysis was chosen based on the Cattell criterion [35]. HCA produced a nested sequence of partitions through an iterative aggregation process which starts by considering all subjects as unique clusters and proceeds by grouping at each step those subjects (clusters) with the minimum distance between them. In the final step, all the subjects are merged in a single cluster. For all the variables included in the analysis, the obtained clusters were then characterized pointing out those modalities for which the proportion inside the group (e.g. the ratio of the number of patients belonging to the cluster with preserved insight, to the cardinality of the cluster) was significantly different from that of the whole sample (e.g. the ratio of the number of patients with preserved insight in the overall study population, to the cardinality of the whole sample). Actually, as each cluster is a subsample of the original dataset (which is a sample itself), the probability values obtained in this comparison do not represent p values in the traditional meaning but they were only used to arrange in decreasing order those factors that are over (or under) expressed inside each cluster with respect to the overall sample and thus are retained to describe that class [36]. Statistical Analyses were conducted using SPSS (Statistical Package for Social Sciences), version 21.0 (SPSS Inc, Chicago, IL) and SPAD (Système Portable pour l’Analyse des Données), version 5.5.
Results
Demographic and clinical characteristics of the study population
Eligible patients
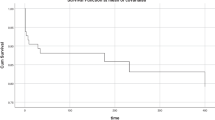
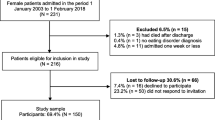
Our database identified 162 eligible female patients with anorexia nervosa. Phone contact was impossible for 60 patients (37 %), due to residence or telephone changes. In 2 cases (1.2 %) patients refused to participate. Median follow-up time was 5.5 years (25th and 75th percentile: 4 years and 11 years). Age at first inpatient treatment, age at onset, BMI at first discharge, duration of inpatient treatment, number of inpatient treatments, duration of illness, duration of long-term inpatient treatment in private centers, number of patients with positive familiar history for psychiatric disorders, number of patients with historical assumption of psychotropic drugs, number of patients with restrictive or binging/purging subtypes and number of patients with preserved insight were not statistically different between groups of included and non-included patients (data not shown).
Participants
In all, 100 patients have been considered for further analyses. All included patients completed the interview and provided all data. 16 % of patients showed an abnormal premorbid BMI (BMI ≤ 18.5 kg/m2), 27 % displayed positive familiar history for psychiatric disorders, 5 % for AN. 46 % of patients were treated with psychotropic drugs. Their former treatment included: serotonergic antidepressants (25 %), tricyclic antidepressants (3 %), benzodiazepines (26 %), first generation antipsychotics (5 %), and second generation antipsychotics (15 %).
Dead patients
We identified four dead patients with anorexia nervosa (4 %). Their characteristics are displayed in Table 1. Three patients displayed binging/purging AN (BP-AN) and were dead due to electrolytic disequilibrium, one patient displayed restrictive AN (R-AN) and was dead due to severe malnutrition. Their last mean BMI was 14.18 ± 2.99 while BMI at first inpatient treatment was 12.8 ± 2.7; median age at onset was 14 years old, median age at first admission was 20 years, insight was absent in 3 out of 4 dead patients. All dead patients displayed conflicting relationships with their parents and 3 out of 4 dead patients with anorexia nervosa were administered psychotropic drugs (antipsychotics, benzodiazepines, antidepressants). No dead patient showed previous suicide attempts or auto-aggressive behaviors.
Univariable and multivariable association with outcome
At follow-up 34 % (R-AN:48.5 %, BP-AN:51.5 %, mean BMI:14.9 ± 2.3) were clinically recovered while 66 % were not clinically recovered (35 % intermediate outcome, 31 % poor outcome) (R-AN:50 %, BP-AN:50 %, mean BMI:14.1 ± 2.1). Their median (25th; 75th percentile) duration of follow-up was, respectively, 10.5 (6; 13.25) years and 5 (3; 8) years (p < 0.001, Mann–Whitney U test). In univariate analysis, these groups did not display significantly different age at onset (p = 0.991, Mann–Whitney U test) or BMI at first inpatient treatment (p = 0.082, Student T test) (Table 1). A younger age at first inpatient treatment was positively associated with a clinical recovery (p = 0.025, Mann–Whitney U test). Clinically recovered patients also showed a shorter duration of illness (p = 0.001, Mann–Whitney U test) and a shorter duration of first inpatient treatment (p = 0.003, Mann–Whitney U test) when compared to not clinically recovered patients. Also a preserved (present or partial) insight was associated with a better clinical outcome with respect to an absent insight (p = 0.042, Chi-square test) (Table 1). The outcome was not associated with presence of familiar mental disorders, psychotropic drug intake, previous suicide attempts, familiar conflicts. Subtype BP-AN was not associated with poor outcome (p = 0.886, Chi square test).
In multiple logistic regression model, after adjusting for the duration of follow-up, duration of first inpatient treatment, duration of illness and preserved insight remained independent predictors of the outcome, while the association with age at first inpatient treatment disappeared (Table 2).
Cluster analysis
Multiple correspondence analysis and cluster analysis revealed the presence of four groups of patients. Group 1, which comprised 26 % of the overall study population, included 84 % of the whole poor outcome group. It was mainly characterized by patients with two or more inpatient treatments (64 % in the cluster vs 21 % in the overall sample), BMI ≤ 14 (76 vs 38 %), absent or partial insight (89 vs 69 %), history of long-term inpatient treatments (32 vs. 9 %), first inpatient treatment ≥30 days (44 vs. 23 %). Group 2 (41 %) did not display specific features when compared with the overall sample. Group 3 (10 %) displayed history of suicide attempts (90.0 vs 9 %) and use of psychotropic drugs (100 vs. 46 %) but no characterization in terms of outcome emerged. Group 4 (23 %) was characterized by a good outcome (64 vs 36 %) preserved insight (82 vs. 31 %), BMI ≥ 16 (73 vs. 30 %), first inpatient treatment ≤14 days (77 vs 35 %), no more than one inpatient treatment (91 vs. 57 %), no psychotropic drugs intake (86 vs 54 %), duration of illness no longer than 4 years (46 vs. 18 %) (Table 3).
Discussion
Clinical recovery
This post-discharge study aimed to investigate outcome and prognostic factors of a group of inpatients with anorexia nervosa on a tertiary level structure. It is currently impossible to predict with certainty which individuals eventually recover from AN completely [37]. Despite considerable efforts to identify clear prognostic factors, predictors of recovery from AN remain controversial and not consistently replicated across the studies [19, 20]. Knowledge of the course and outcome of AN is needed for evaluation of different treatment methods, and for development of future treatment studies [38]. In our study, similarly to other studies with a comparable follow-up time [3, 39], at 5.5 ± 0.7 years follow-up, less than one-half of patients were clinically recovered. Other authors assessed clinical recovery is more frequent among patients with anorexia nervosa of a primary care-based cohort. Nevertheless, we performed a tertiary level study and our method considered both clinical, mental and social functioning, thus we can hypothesize that we used stricter criteria for clinical recovery. Indeed the Morgan–Russell assessment schedule [16] covers weight, food intake, menstruation, and mental state as well as psychosexual and psychosocial functioning. When the latter were considered, a lower recovery rate was assessed [28].
Association between age at onset and clinical recovery
We found no association between age at onset and clinical recovery. Previous studies have failed to assess this association [9, 30]. A recent study [40] assessed that 76 % of patients with childhood-onset eating disorders achieve clinical recovery at 1-year follow-up. Our study was set in a tertiary structure, mainly addressed to adolescents and adults. Indeed our cohort included relatively few patients with early onset AN (median age at onset, 25th and 75th percentile: 16, 14, 20 years). We can argue that our study did not sufficiently consider early onset patients with anorexia nervosa (<13 years, [40]), more probably treated in child neuropsychiatric structures, thus failing proving an association between early age at onset and clinical recovery.
Association between low BMI at first inpatient treatment and poor outcome
Moreover, our study found no association between low BMI at first inpatient treatment and poor outcome. Pinter et al. assessed that patients with a low BMI at admission have a significantly greater chance to develop a lower BMI value at follow-up than those with a higher BMI [41]. However, we did not consider possible diagnostic crossovers between AN and other eating disorders. Indeed patients with anorexia nervosa (with abnormal BMI) are more likely to relapse into bulimia nervosa (with normal BMI) rather than vice versa [26]. We can hypothesize that some chronic patients with anorexia nervosa with abnormal BMI experienced diagnostic changes that we did not assess, thus influencing the possible association between low BMI at first inpatient treatment and poor outcome.
Association between younger age and short duration at first inpatient treatment and outcome
We also found an association between younger age at first inpatient treatment and outcome. However, we considered that the duration of follow-up could be a confounding factor. Indeed the duration of follow-up was rather variable in our study (median: 5.5, 25th and 75th percentile: 4 and 11 years). Thus, we performed a multiple logistic regression analysis adjusted for the duration of follow-up that revealed no association between younger age at first inpatient treatment and outcome. Our study confirmed that a short duration of first inpatient treatment and a short duration of illness were associated with better outcome. One large meta-analysis [3] did already assess this association. Nevertheless, a recent study was unable to replicate this result [19]. The presence of different groups of patients with different outcomes could possibly explain this heterogeneity.
Identification of groups of patients with different outcome
At this aim, we identified four discrete groups of patients, characterized by different clusters of prognostic factors. Notably, we recognized two groups with contrasting outcomes.
Group 1 (poor outcome group)
Group 1 (26 % of our population) showed that the absence of insight was frequently associated with a chronic evolution. Indeed this type of patients presented poorer outcome (84 % of the whole poor outcome group) and more frequent and longer duration of inpatient treatments. Interestingly, other studies also assessed that about one-fourth of patients with anorexia nervosa showed impaired insight [42]. Our study better defined these potentially chronic patients. They should probably be supported with more intense and frequent medical and psychiatric assistance.
Group 4 (good outcome group)
Group 4 mostly included insight preserved patients with anorexia nervosa. These patients also displayed better outcome (64 % of the whole good outcome group) less frequent and shorter inpatient treatments and they did not use psychotropic drugs. These results confirmed the presence of a good outcome group of patients with anorexia nervosa. One can hypothesize that early and short inpatient treatment could contribute to a good outcome. However, a possible confounding association between BMI at admission and duration of first inpatient treatment cannot be excluded. Future studies, with a prospective design, should better define the factors influencing the outcome of this group. Moreover, our study assessed that poor outcome was more clearly associated with specific factors (84 % in Group 1) than good outcome (only 64 % in Group 4). We can argue that good outcome patients were more heterogeneously distributed among the groups. Good outcome patients often display a wide range of post-recovery residual symptoms, psychopathological disorders and psychosocial dysfunctions [27, 28]. This may account for the inability to find an association with a specific cluster of prognostic factors.
Group 3 (history of suicide attempts and drugs intake)
Group 3 (10 % of our population) included patients with history of suicide attempts and psychotropic drugs intake. These two factors had already been associated [43] and predicted a future suicide attempt [3]. About 30 % of patients with anorexia nervosa have a history of suicide attempts [3]. Interestingly, our study assessed that previous suicide attempts and psychotropic drugs intake were not associated with poor outcome. Moreover, in our study, at follow-up, 3 out of 4 dead patients (4 %) used psychotropic drugs. Nevertheless, none of them was dead due to suicide nor had previously attempted suicide. We can hypothesize that these two factors were linked to other confounding variables, such as comorbidities. Indeed the greater use of psychotropic drugs in Group 3 could suggest psychiatric comorbidities in these patients, thus death and suicidality associated to mental illness other than AN should be excluded in this group. Indeed recent studies have highlighted the role of depressive symptoms [19] and trait anxiety [20] in the outcome of AN. Therefore, psychiatric comorbidities should be seriously considered when a history of suicide attempts and psychotropic drugs intake is present.
Finally this study assessed that only half of the patients can be included in the two clusters associated with outcome (Group 1 and 4). However, our study considered a limited number of prognostic factors. Novel prognostic factors have recently been described [19, 20]. They should be considered in future studies to outline specific features of the patients that we included in our residual group (Group 2).
Subtypes of AN and outcome
We also found that subtype BP-AN was not associated with poor outcome. Only a few studies compared outcomes for R-AN and BP-AN [3]. However, at 4-year follow-up, full recovery was achieved in 17 % of patients with BP-AN and in 8 % of patients with R-AN [44]. At 8-years follow-up, no significant differences in recovery rates between R-AN and BP-AN were observed [26]. Nevertheless, a large meta-analysis concluded that vomiting and purgative abuse implied an unfavorable prognosis [9]. However, isolated symptoms of vomiting and purgative abuse are not necessarily linked to BP-AN. Thus, future studies should consider well-defined BP-AN and not only isolated symptoms.
Limitations of the study
Our study has several limitations. First, telephone interviews did not imply a personal contact to the former patients. Therefore, data concerning weight, height and presence of eating disorder symptoms have to be carefully considered. However, our interviews were strictly structured and all data were compared with those of the latest clinical visit. Second, we did not assess diagnostic crossover between AN and bulimia nervosa or eating disorder not otherwise specified. Previous studies assessed that one-third of patients with anorexia nervosa crossed over to bulimia nervosa [26]. Nevertheless, these patients were likely to relapse into AN, having this diagnosis stable across the years [26]. Third, follow-up time is variable in our study (median: 5.5, 25th and 75th percentile: 4 and 11 years). Nevertheless, all statistic analyses were adjusted for follow-up time and multiple logistic regression analyses assured that each factor was an independent predictor of outcome.
Summary
Despite these limitations, our study confirmed the association between short duration of inpatient treatment, short duration of disorder, early age at first inpatient treatment, preserved insight and clinical recovery. Notably this study also aggregated prognostic factors of patients with anorexia nervosa to outline discrete prognostic groups.
Conclusions
This approach has practical implications. Indeed the specific clusters of prognostic factors we defined might help clinicians in early orienting their practice. Once recognized a cluster of prognostic factors in a certain patient, clinicians will have additional informations about his outcome. Future studies should better characterize these outcome groups both with larger samples and with prospective design to find specific therapeutic implications.
References
Papadopoulos FC, Ekbom A, Brandt L, Ekselius L (2009) Excess mortality, causes of death and prognostic factors in anorexia nervosa. Br J Psychiatry 194:10–17. doi:10.1192/bjp.bp.108.054742
Arcelus J, Mitchell AJ, Wales J, Nielsen S (2011) Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry 68:724–731. doi:10.1001/archgenpsychiatry.2011.74
Berkman ND, Lohr KN, Bulik CM (2007) Outcomes of eating disorders: a systematic review of the literature. Int J Eat Disord 40:293–309. http://www.ncbi.nlm.nih.gov/pubmed/17370291
Nielsen S, Moller-Madsen S, Isager T, Jorgensen J, Pagsberg K, Theander S (1998) Standardized mortality in eating disorders–a quantitative summary of previously published and new evidence. J Psychosom Res 44:413–34. http://www.ncbi.nlm.nih.gov/pubmed/9587884
Signorini A, De Filippo E, Panico S, De Caprio C, Pasanisi F, Contaldo F (2007) Long-term mortality in anorexia nervosa: a report after an 8-year follow-up and a review of the most recent literature. Eur J Clin Nutr 61:119–22. http://www.ncbi.nlm.nih.gov/pubmed/16885933
Brewerton TD, Costin C (2011) Treatment results of anorexia nervosa and bulimia nervosa in a residential treatment program. Eat Disord 19:117–131. doi:10.1080/10640266.2011.551629
Brewerton TD, Costin C (2011) Long-term outcome of residential treatment for anorexia nervosa and bulimia nervosa. Eat Disord 19:132–144. doi:10.1080/10640266.2011.551632
Lee S, Chan YY, Hsu LK (2003) The intermediate-term outcome of Chinese patients with anorexia nervosa in Hong Kong. Am J Psychiatry 160:967–72. http://www.ncbi.nlm.nih.gov/pubmed/12727702
Steinhausen HC (2002) The outcome of anorexia nervosa in the 20th century. Am J Psychiatry 159:1284–1293. http://www.ncbi.nlm.nih.gov/pubmed/12153817
Mustelin L, Raevuori A, Bulik CM, Rissanen A, Hoek HW, Kaprio J, Keski-Rahkonen A (2015) Long-term outcome in anorexia nervosa in the community. Int J Eat Disord. doi:10.1002/eat.22415
Smink FR, van Hoeken D, Hoek HW (2013) Epidemiology, course, and outcome of eating disorders. Curr Opin Psychiatry. 26:543–548. doi:10.1097/YCO.0b013e328365a24f
Fichter MM, Quadflieg N, Hedlund S (2006) Twelve-year course and outcome predictors of anorexia nervosa. Int J Eat Disord 39:87–100. http://www.ncbi.nlm.nih.gov/pubmed/16231345
Wentz E, Gillberg IC, Anckarsater H, Gillberg C, Rastam M (2009) Adolescent-onset anorexia nervosa: 18-year outcome. Br J Psychiatry 194:168–174. doi:10.1192/bjp.bp.107.048686
Couturier J, Lock J (2006) What is recovery in adolescent anorexia nervosa? Int J Eat Disord 39:550–5. http://www.ncbi.nlm.nih.gov/pubmed/16791851
Jeammet P, Brechon G, Payan C, Gorge A, Fermanian J (1991) The outcome of anorexia nervosa: a prospective study of 129 patients evaluated at least 4 years after their first admission. Psychiatr Enfant 34:381–442. http://www.ncbi.nlm.nih.gov/pubmed/1798811
Morgan HG, Russell GF (1975) Value of family background and clinical features as predictors of long-term outcome in anorexia nervosa: four-year follow-up study of 41 patients. Psychol Med 5:355–71. http://www.ncbi.nlm.nih.gov/pubmed/1197538
Couturier J, Lock J (2006) What is remission in adolescent anorexia nervosa? A review of various conceptualizations and quantitative analysis. Int J Eat Disord 39:175–83. http://www.ncbi.nlm.nih.gov/pubmed/16485268
Strober M, Freeman R, Morrell W (1997) The long-term course of severe anorexia nervosa in adolescents: survival analysis of recovery, relapse, and outcome predictors over 10–15 years in a prospective study. Int J Eat Disord 22:339–60. http://www.ncbi.nlm.nih.gov/pubmed/9356884
Keski-Rahkonen A, Raevuori A, Bulik CM, Hoek HW, Rissanen A, Kaprio J (2014) Factors associated with recovery from anorexia nervosa: a population-based study. Int J Eat Disord 47:117–123. doi:10.1002/eat.22168
Zerwas S, Lund BC, Von Holle A, Thornton LM, Berrettini WH, Brandt H, Crawford S, Fichter MM, Halmi KA, Johnson C, Kaplan AS, La Via M, Mitchell J, Rotondo A, Strober M, Woodside DB, Kaye WH, Bulik CM (2013) Factors associated with recovery from anorexia nervosa. J Psychiatr Res 47:972–979. doi:10.1016/j.jpsychires.2013.02.011
American Psychiatric Association (1994) Diagnostic and statistical manual for mental disorders. 4th edn. Washington, DC
American Psychiatric Association (1980) Diagnostic and statistical manual for mental disorders, 3rd edn. Washington, DC
American Psychiatric Association (2013) Diagnostic and statistical manual for mental disorders, 5th edn. Washington, DC
Dalle Grave R, Calugi S, Marchesini G (2008) Is amenorrhea a clinically useful criterion for the diagnosis of anorexia nervosa? Behav Res Ther 46:1290–1294. doi:10.1016/j.brat.2008.08.007
Attia E, Roberto CA (2009) Should amenorrhea be a diagnostic criterion for anorexia nervosa? Int J Eat Disord 42:581–589. doi:10.1002/eat.20720
Eddy KT, Dorer DJ, Franko DL, Tahilani K, Thompson-Brenner H, Herzog DB (2008) Diagnostic crossover in anorexia nervosa and bulimia nervosa: implications for DSM-V. Am J Psychiatry 165:245–250. doi:10.1176/appi.ajp.2007.07060951
Espindola CR, Blay SL (2013) Long term remission of anorexia nervosa: factors involved in the outcome of female patients. PLoS One 8:e56275. doi:10.1371/journal.pone.0056275
Wentz E, Gillberg C, Gillberg IC, Rastam M (2001) Ten-year follow-up of adolescent-onset anorexia nervosa: psychiatric disorders and overall functioning scales. J Child Psychol Psychiatry 42:613–22. http://www.ncbi.nlm.nih.gov/pubmed/11464966
Keel PK, Dorer DJ, Franko DL, Jackson SC, Herzog DB (2005) Postremission predictors of relapse in women with eating disorders. Am J Psychiatry 162:2263–2268. http://www.ncbi.nlm.nih.gov/pubmed/16330589
Pohjolainen V, Ryynänen OP, Räsänen P, Roine RP, Koponen S, Karlsson H (2014) Bayesian prediction of treatment outcome in anorexia nervosa: a preliminary study. Nord J Psychiatry 7:1–6. doi:10.1002/eat.20676
Ratnasuriya RH, Eisler I, Szmukler GI, Russell GF (1991) Anorexia nervosa: outcome and prognostic factors after 20 years. Br J Psychiatry 158:495–502. http://www.ncbi.nlm.nih.gov/pubmed/2054565
van Son GE, van Hoeken D, van Furth EF, Donker GA, Hoek HW (2010) Course and outcome of eating disorders in a primary care-based cohort. Int J Eat Disord 43:130–8. http://www.ncbi.nlm.nih.gov/pubmed/25286982
Carsky M, Selzer MA, Terkelsen K, Hurt SW. The PEH. A questionnaire to assess acknowledgment of psychiatric illness. J Nerv Ment Dis 180:458–64. http://www.ncbi.nlm.nih.gov/pubmed/1624928
Lebart M (1997) Piron. Statistique exploratoire multidimensionelle, 2nd edn, 1997, Dunod, Paris
Cattell RB (1966) The scree test for the number of factors. Multivar Behav Res 1:245–276
Morineau A (1984) Note sur la caractérisation statistique d’une classe et les valeurs tests. Bulletin Technique Centre Statistique Informatique Appliquées 2:20–27
Bachner-Melman R, Zohar AH, Ebstein RP (2006) An examination of cognitive versus behavioral components of recovery from anorexia nervosa. J Nerv Ment Dis 194:697–703. http://www.ncbi.nlm.nih.gov/pubmed/16971822
Herzog DB, Sacks NR, Keller MB, Lavori PW, von Ranson KB, Gray HM (1993) Patterns and predictors of recovery in anorexia nervosa and bulimia nervosa. J Am Acad Child Adolesc Psychiatry 32:835–842. http://www.ncbi.nlm.nih.gov/pubmed/8340307
Gillberg IC, Rastam M, Gillberg C (1994) Anorexia nervosa outcome: six-year controlled longitudinal study of 51 cases including a population cohort. J Am Acad Child Adolesc Psychiatry 33:729–39. http://www.ncbi.nlm.nih.gov/pubmed/8056736
Nicholls DE, Lynn R, Viner RM (2011) Childhood eating disorders: British national surveillance study. Br J Psychiatry 198:295–301. doi:10.1192/bjp.bp.110.081356
Pinter O, Probst M, Vandereycken W, Pieters G, Goris M (2004) The predictive value of body mass index for the weight evolution in anorexia nervosa. Eat Weight Disord 9:232–235. http://www.ncbi.nlm.nih.gov/pubmed/15656020
Konstantakopoulos G, Tchanturia K, Surguladze SA, David AS (2011) Insight in eating disorders: clinical and cognitive correlates. Psychol Med 41:1951–1961. doi:10.1017/S0033291710002539
Franko DL, Keel PK, Dorer DJ, Blais MA, Delinsky SS, Eddy KT, Charat V, Renn R, Herzog DB (2004) What predicts suicide attempts in women with eating disorders? Psychol Med 34:843–53. http://www.ncbi.nlm.nih.gov/pubmed/15500305
Herzog DB, Nussbaum KM, Marmor AK (1996) Comorbidity and outcome in eating disorders. Psychiatr Clin North Am 19:843–59. http://www.ncbi.nlm.nih.gov/pubmed/9045226
Acknowledgments
We wish to thank Dr. Pasquale Striano for his precious collaboration and Prof. Salvatore Striano for his important teaching.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have nothing to disclose. On behalf of all authors, the corresponding author states that there is no conflict of interest: the authors have no financial or personal relationships with a third party whose interests could be positively or negatively influenced by the article’s content.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Errichiello, L., Iodice, D., Bruzzese, D. et al. Prognostic factors and outcome in anorexia nervosa: a follow-up study. Eat Weight Disord 21, 73–82 (2016). https://doi.org/10.1007/s40519-015-0211-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-015-0211-2