Abstract
Purpose of Review
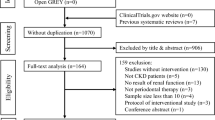
Many clinical studies have reported an association between periodontal disease and chronic kidney disease (CKD). This review aims to update the underlying mechanism and the findings of clinical studies.
Recent Findings
Basic research supports that inflammation might mediate the association between CKD and periodontal disease. Clinical evidence suggests that periodontal treatment improves renal function. Poor oral health has also been reported as a predictor of mortality in patients undergoing hemodialysis.
Summary
Although clinical data have demonstrated a significant association between inflammation in the periodontal tissue and CKD, well-designed studies are needed for a consensus to be widely adopted. Malnutrition and systemic chronic inflammation are often interrelated in patients undergoing hemodialysis. Periodontal disease may contribute to chronic inflammation, and it is possible that a low number of teeth may be involved in impaired nutritional intake in patients undergoing hemodialysis. A novel perspective on malnutrition might be needed to manage oral health in patients with CKD, especially those undergoing dialysis, in addition to conventional factors such as bacterial infection and inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontal disease is characterized by chronic inflammation caused by oral biofilms. Periodontal pathogens in the gingiva may be transferred throughout the systemic blood circulation, leading to elevation of inflammatory cytokines by bacterial lipopolysaccharides (LPS) [1, 2••]. Consequently, increased serum interleukin 17 (IL-17) [3], IL-1 tumor necrosis factor (TNF)-α, and activated nuclear factor kappa beta (NF-κB) [3, 4, 5, 6] cause inflammatory immune response. Oxidative stress has been suggested as a mechanism of enhanced inflammation. Periodontal disease has been reported to increase oxidative stress markers, 8-hydroxy-2′-deoxyguanosine, and isoprostanes in saliva and periodontal tissues [7, 8]. Moreover, periodontal disease also increases systemic oxidative stress by decreasing total antioxidant capacity levels and increasing malondialdehyde (MDA) and nitric oxide levels in the peripheral blood [9].
Conversely, various medical conditions also increase systemic oxidative stress. Hyperlipidemia, induced by obesity, metabolic syndrome, and hyperglycemia in diabetes mellitus, is a major cause of increased oxidative stress. Diabetes mellitus is a chronic hyperglycemic condition caused by insulin deficiency or resistance. This hyperglycemic state directly injures vascular endothelial cells owing to oxidative stress, resulting in complications associated with macro- and micro-blood vessels [10]. The suggested mechanisms include increased superoxide levels due to mitochondrial dysfunction [11] and activation of nicotinamide adenine dinucleotide phosphate oxidase in endothelial cells [12]. In addition, under diabetic conditions, oxidative stress scavenging capacity is reduced due to the denaturation of antioxidant enzymes such as superoxide dismutase and glutathione peroxidase. Periodontal tissues are also subjected to this systemic oxidative stress [13], resulting in delayed wound healing [14, 15], tissue regeneration in periodontal tissues [16], and impaired implant osseointegration [17], Much evidence has been accumulated for this bidirectional association between periodontal tissues and medical conditions, especially in diabetes mellitus [18]. Inflammation in periodontal tissue is associated with glycemic control independent of plaque control [19].
The inflammatory response to periodontal disease has been correlated with insulin resistance [20, 21], suggesting that severe periodontal disease may influence the development and progression of cardiovascular disease or nephropathy in diabetic patients [22, 23]. Recently, an association between periodontal disease and renal disease has been suggested. Diabetic nephropathy is one of the most common complications of diabetes, and it is possible that periodontal disease affects renal function. Furthermore, it has been speculated that periodontal disease may affect renal function independently of diabetes [23–25].
Chronic kidney disease (CKD) is defined as any renal impairment or a glomerular filtration rate (GFR) of less than 60 mL/min/1.73 m2 for more than 3 months [26]. Progression of CKD leads to renal failure, which requires alternative renal therapies, such as renal transplantation or dialysis therapy. Patients undergoing dialysis for end-stage renal disease (ESRD) have a very high crude mortality rate of more than 20% [27]. Cardiovascular problems and infections are the most common causes of death in dialysis patients. Recently, nutritional status was shown to play a significant role in the prognosis of these patients [28, 29].
In this article, we review the relationship between periodontal disease and CKD, focusing on data from basic and clinical studies, including new perspectives, such as inflammation and nutritional intake, in addition to the conventional viewpoint of bacterial infection.
Association Between Periodontitis and Chronic Kidney Disease
In Vitro and In Vivo Studies
Periodontal disease may affect renal function through the following pathways: bacteria and their bacterial components may affect the kidneys and increase the concentration of circulating cytokines [30, 31].
In in vitro studies using vascular endothelial cells derived from mouse kidneys, stimulation with LPS of Porphyromonas gingivalis (P. gingivalis), even at low concentrations, increased the expression of serum amyloid a3 protein (Saa3) and toll-like receptor adaptor molecule 1 (TICAM1), which indicates chronic inflammation and may increase the risk of kidney disease [32].
In in vivo studies on the association between periodontal disease and CKD, two experimental designs, intravascular injection of LPS from periodontal pathogenic bacteria and ligation of molars, have been conducted to expose periodontal inflammation in the kidney. In an experiment involving intravascular injection with LPS of P. gingivalis, Harada et al. showed histological changes in the kidney and increased expression of Saa3 and TICAM1 following the 30-day LPS injection. These results indicate that LPS from periodontal pathogenic bacteria causes chronic inflammation in the kidney [32]. Furthermore, Sawa et al. demonstrated that LPS injection increased the accumulation of type I collagen in glomerular and urinary proteins and upregulated the expression of IL-6, TNF-α, and transforming growth factor (TGF)-β in the renal cortex of the glomeruli of streptozotocin-induced diabetic mice. This finding suggests that the circulating LPS of P. gingivalis causes the progression of diabetic nephropathy [33].
In the molar-ligation model, Fellipe et al. reported that acute periodontitis induced by ligature placement was associated with histological changes in the renal corpuscles; however, renal function evaluated by blood biomarkers (albumin, creatinine, glucose, and urea) was unaffected. In addition, a significant decrease in glutathione and an increase in MDA concentration in the kidney suggest that periodontal disease elevates renal oxidative stress [34].
Based on these studies, it is understood that periodontal disease affects the cellular function of the kidney, resulting in a decreased filtration rate due to glomerular fibrosis and cell damage.
Clinical Studies
Recent findings have suggested a pathological association between periodontal disease and renal dysfunction, with many clinical studies conducted in patients with periodontal disease and CKD [24, 35, 36]. A large cross-sectional study reported that periodontal disease was a potential risk factor for the development of CKD based on the assessment of estimated GFR (eGFR) [35]. A retrospective cohort study of 75-year olds showed that a higher periodontal inflammatory surface area (PISA) score was associated with an increased risk of decline in renal function (odds ratio 2.24, 95% confidence interval [CI], 1.05–4.79) [24]. Recently, a systematic review reported substantial evidence on the association between periodontitis and CKD; however, there are limited studies on the directional association [37]. Currently, the details of the mechanisms underlying this association are controversial. Periodontal disease may impair vascular endothelial function and induce atherosclerosis and hypertension, resulting in renal dysfunction. Indirect interactions between CKD and periodontitis have also been presumed to occur due to diabetes and atherosclerosis associated with periodontitis.
Intervention studies have reported improvements in CKD disease status with periodontal therapy. In a cohort study of pre-dialysis patients with CKD, non-surgical periodontal treatment significantly reduced eGFR at 6 months after treatment [38]. In addition, endogenous inhibitors of nitric oxide synthase, asymmetric dimethylarginine (ADMA), were also significantly decreased [38]. This study highlights the comprehensive association between CKD, endothelial dysfunction, and periodontitis. A recent systematic review of 18 studies also showed that periodontal therapy improved the disease state of CKD [39••]. The findings of this review included significant improvements in serum C-reactive protein (CRP) levels [40]. as well as a significant reduction in inflammatory cytokines. Several studies have reported improvements in IL-6 levels. These findings suggest that periodontal treatment improves CKD marker levels by reducing systemic inflammation. Recent systematic reviews of intervention studies are summarized in Table 1, with two GFR analyses showing significant improvements [37] and one showing no statistically significant differences [41••]. In addition, one systematic review and meta-analysis reported a significant reduction in high-sensitivity CRP [42••].
There is much evidence that periodontal inflammation affects renal function (Fig. 1). However, more high-quality evidence is needed for consensus [43].
Biologically plausible mechanisms linking periodontitis and chronic kidney disease. Periodontal pathogens in the dental plaque invade gingival connective tissue, causing an inflammatory response. This inflammatory response produces various cytokines that are released into the bloodstream and have the potential to reach the kidneys. Fragments of periodontal pathogens, such as P. gingivalis and lipopolysaccharides (LPS), released into the bloodstream may also reach the kidneys. In addition, chronic systemic inflammation and oxidative stress due to periodontitis may affect renal function. This is an original figure prepared for this article
Clinical Studies of Oral Health in Patients Undergoing Hemodialysis
Patients undergoing hemodialysis are known to have a high incidence of oral diseases, including periodontal disease, because they are likely to have xerostomia [44] due to atrophy of salivary gland tissue, decreased body water content, and medications, as well as poor access to dental care [45]. A meta-analysis by Ruospo et al. reported a periodontal disease morbidity rate of 56.8% (95% CI 39.3–72.8) in ESRD patients who required dialysis treatment [46]. Furthermore, it has been reported that among patients undergoing hemodialysis, those with severe periodontitis had significantly higher levels of serum inflammatory markers [47], and that periodontal treatment significantly lowered the inflammatory markers [48]. These studies suggest that periodontitis may add to the inflammatory burden in patients undergoing hemodialysis who are often in a chronic inflammatory state.
We conducted a cohort study of patients undergoing hemodialysis and reported an association between oral and systemic conditions. Oral examinations, including salivary tests, were performed on 121 patients with ESRD undergoing hemodialysis and linked to their systemic condition data to explore the association between periodontal disease and systemic inflammation. The results showed that the number of P. gingivalis in saliva was positively and significantly associated with the levels of serum TNF receptors (TNFRs; TNFR1 and TNFR2) (TNFR1, coefficient 0.76, 95% CI 0.14–1.37, p = 0.02; TNFR2, coefficient 0.95, 95% CI 0.09–1.80, p = 0.03) even after adjusting for confounding factors such as age, sex, and diabetes [49•]. TNF1 and TNFR2 are markers of chronic inflammation and are known prognostic markers of mortality in patients undergoing hemodialysis [50]. Our study suggests that periodontal pathogenic bacteria may be involved in chronic inflammation in patients undergoing hemodialysis. Furthermore, a 3-year prospective cohort study in the same population showed that poor oral hygiene and dental caries predicted a high mortality rate in hemodialysis [51•]. We followed 266 patients undergoing hemodialysis for 3 years and showed that those with a debris index-simplified (DI-S) in the top tertile at baseline, namely those with poor oral hygiene, had a higher mortality rate with a hazard ratio of 3.04 (95% CI 1.50–6.17, p = 0.002) at 3 years than those in the middle and lowest tertiles of DI-S after adjustment for confounding factors. Similarly, a higher number of decayed teeth at baseline were associated with significantly higher mortality at 3 years (hazard ratio 1.21, 95% CI 1.06–1.37, p = 0.003). Further studies are required to determine the mechanism by which oral hygiene status affects mortality in patients undergoing hemodialysis. Previous epidemiological studies have shown that patients undergoing hemodialysis are more likely to suffer from xerostomia [52] and have poorer access to dental care [45], resulting in poor oral health compared to the healthy population [53]. As our study showed, poor oral health in patients undergoing hemodialysis may be related to their systemic condition and even to their life prognosis. Therefore, dental professionals are required to elucidate the details of these mechanisms and to take concrete actions to improve the oral health care environment for patients undergoing hemodialysis.
Relationship Between Malnutrition and Oral Diseases in Patients Undergoing Hemodialysis
Patients undergoing hemodialysis are known to have a high crude mortality rate of > 20% per year [27]. Cardiovascular disease (CVD) is the leading direct cause of death; however, nutritional status is known to play a significant role in life expectancy. Unlike simple undernutrition, such as starvation with low nutritional intake, malnutrition in patients undergoing hemodialysis is characterized by inflammation. Malnutrient patients undergoing hemodialysis are prone to chronic inflammation and atherosclerotic complications due to increased catabolism caused by inflammatory cytokines, such as IL-6, 8, 1b, 18, and TNF-α. This condition is called malnutrition inflammation atherosclerosis (MIA) syndrome [54], which is known to be prone to CVD and death. In the general population, overnutrition is a risk for CVD development, while in patients undergoing hemodialysis, malnutrition, such as low BMI and low cholesterol levels, is a risk for CVD development and mortality, known as “reverse epidemiology” [55, 56].
Various factors such as aging, smoking, decreased energy and protein intake, inflammatory cytokines, uremic substances, fluid overload, decreased muscle mass and physical function, dialysis-related factors, and complications (such as CVD, diabetes, and depression) are associated with nutritional disorders in patients undergoing hemodialysis. Patients undergoing hemodialysis experience gastrointestinal symptoms, such as decreased appetite, flatulence, early satiety, nausea, and gastroesophageal reflux due to decreased gastrointestinal motility [57, 58]. Inflammatory cytokines such as IL-6 and TNF-α are also associated with a decreased appetite, and chronic inflammation leads to decreased albumin production. Dialysis-related factors, such as general malaise, loss of amino acids to the dialysate solution, and uremia due to lack of dialysis, also have an impact on nutrient metabolism.
Chronic inflammation is often the cause of nutritional disorders in patients undergoing hemodialysis. Chronic inflammation is often caused by amyloidosis or atherosclerotic lesions, which renders the causative disease difficult to treat. In contrast, inflammation caused by periodontal disease is one of the candidates of a treatable inflammatory factor. Thus, we hypothesized that oral diseases, including periodontitis, may affect the mortality of patients undergoing hemodialysis via MIA syndrome (Fig. 2). MIA syndrome and periodontitis share common risk factors such as diabetes, smoking, and aging. Moreover, periodontitis increases systematic inflammatory responses due to the spread of inflammatory cytokines through the bloodstream and bacteremia caused by periodontal pathogenic bacteria [59, 60]. Our previous study showed that patients undergoing hemodialysis with high P. gingivalis levels in saliva have significantly higher serum TNFRs, which are markers of chronic inflammation [49•]. Previous studies have also shown elevated inflammatory markers in patients undergoing hemodialysis with periodontitis compared to those without periodontitis [47, 61, 62]. Therefore, periodontitis may be an inflammatory burden in patients undergoing hemodialysis who are in a state of chronic mild inflammation. Periodontal disease is the leading cause of tooth loss in adults, while a low number of teeth increase the risk of malnutrition [63, 64]. In particular, dialysis patients with type 2 diabetes tend to experience a vicious cycle. Our recent cross-sectional study demonstrated that type 2 diabetes was significantly associated with periodontitis and the number of missing teeth in patients undergoing hemodialysis [65]. Based on these considerations, we hypothesized that poor oral health in patients undergoing hemodialysis is closely related to both inflammation and nutrient intake and may contribute to MIA syndrome. Further research will be conducted to verify this hypothesis.
A hypothesis between oral condition and malnutrition inflammation atherosclerosis (MIA) syndrome. It is commonly believed that various factors such as diabetes, smoking, and aging are involved in MIA syndrome in end-stage renal disease patients. Periodontitis might be associated with atherosclerosis via an increase in inflammation, and tooth loss was associated with malnutrition. This is an original figure prepared for this article
Summary and Conclusion
Many clinical investigations have demonstrated an association between periodontal disease and CKD. These studies suggest that inflammation may mediate the association between CKD and periodontal disease. Interestingly, clinical evidence has demonstrated that periodontal treatment can improve renal function. However, large-scale and/or well-designed studies are needed for a consensus to be widely accepted. Chronic systemic inflammation is often the cause of nutritional impairment in patients undergoing dialysis. Periodontal disease may cause chronic inflammation, and it is also possible that a low number of teeth in dialysis patients may be involved. A novel perspective of nutritional intake might be needed to manage oral health in patients with CKD, especially those undergoing dialysis, and conventional factors, such as bacterial infection and inflammation.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hajishengallis G. Periodontitis: from microbial immune subversion to systemic inflammation. Nat Rev Immunol. 2015;15(1):30–44. https://doi.org/10.1038/nri3785.
•• Machado V, Botelho J, Escalda C, Hussain SB, Luthra S, Mascarenhas P, et al. Serum C-reactive protein and periodontitis: a systematic review and meta-analysis. Front Immunol. 2021;12:706432. https://doi.org/10.3389/fimmu.2021.706432. This systematic review and meta-analysis showed that periodontitis is associated with systemic inflammation and that periodontal treatment reduces serum CRP levels through a reduction in the first week and a progressive reduction up to 6 months.
Xiao E, Mattos M, Vieira GHA, Chen S, Corrêa JD, Wu Y, et al. Diabetes enhances IL-17 expression and alters the oral microbiome to increase its pathogenicity. Cell Host Microbe. 2017;22(1):120-8.e4. https://doi.org/10.1016/j.chom.2017.06.014.
Wu YY, Xiao E, Graves DT. Diabetes mellitus related bone metabolism and periodontal disease. Int J Oral Sci. 2015;7(2):63–72. https://doi.org/10.1038/ijos.2015.2.
Abusleme L, Moutsopoulos NM. IL-17: overview and role in oral immunity and microbiome. Oral Dis. 2017;23(7):854–65. https://doi.org/10.1111/odi.12598.
Nishimura F, Iwamoto Y, Mineshiba J, Shimizu A, Soga Y, Murayama Y. Periodontal disease and diabetes mellitus: the role of tumor necrosis factor-alpha in a 2-way relationship. J Periodontol. 2003;74(1):97–102. https://doi.org/10.1902/jop.2003.74.1.97.
Sawamoto Y, Sugano N, Tanaka H, Ito K. Detection of periodontopathic bacteria and an oxidative stress marker in saliva from periodontitis patients. Oral Microbiol Immunol. 2005;20(4):216–20. https://doi.org/10.1111/j.1399-302X.2005.00215.x.
Wolfram RM, Budinsky AC, Eder A, Presenhuber C, Nell A, Sperr W, et al. Salivary isoprostanes indicate increased oxidation injury in periodontitis with additional tobacco abuse. BioFactors. 2006;28(1):21–31. https://doi.org/10.1002/biof.5520280103.
Liu Z, Liu Y, Song Y, Zhang X, Wang S, Wang Z. Systemic oxidative stress biomarkers in chronic periodontitis: a meta-analysis. Dis Markers. 2014;2014: 931083. https://doi.org/10.1155/2014/931083.
King GL. The role of inflammatory cytokines in diabetes and its complications. J Periodontol. 2008;79(8 Suppl):1527–34. https://doi.org/10.1902/jop.2008.080246.
Bullon P, Newman HN, Battino M. Obesity, diabetes mellitus, atherosclerosis and chronic periodontitis: a shared pathology via oxidative stress and mitochondrial dysfunction? Periodontol 2000. 2014;64(1):139–53. https://doi.org/10.1111/j.1600-0757.2012.00455.x.
Mizutani K, Park K, Mima A, Katagiri S, King GL. Obesity-associated gingival vascular inflammation and insulin resistance. J Dent Res. 2014;93(6):596–601. https://doi.org/10.1177/0022034514532102.
Mizutani K, Buranasin P, Mikami R, Takeda K, Kido D, Watanabe K, et al. Effects of antioxidant in adjunct with periodontal therapy in patients with type 2 diabetes: a systematic review and meta-analysis. Antioxidants (Basel). 2021;10(8). doi: https://doi.org/10.3390/antiox10081304.
Kido D, Mizutani K, Takeda K, Mikami R, Matsuura T, Iwasaki K, et al. Impact of diabetes on gingival wound healing via oxidative stress. PLoS ONE. 2017;12(12): e0189601. https://doi.org/10.1371/journal.pone.0189601.
Buranasin P, Mizutani K, Iwasaki K, Pawaputanon Na Mahasarakham C, Kido D, Takeda K, et al. High glucose-induced oxidative stress impairs proliferation and migration of human gingival fibroblasts. PLoS One. 2018;13(8):e0201855. https://doi.org/10.1371/journal.pone.0201855.
Takeda K, Mizutani K, Matsuura T, Kido D, Mikami R, Noda M, et al. Periodontal regenerative effect of enamel matrix derivative in diabetes. PLoS ONE. 2018;13(11): e0207201. https://doi.org/10.1371/journal.pone.0207201.
Saito N, Mikami R, Mizutani K, Takeda K, Kominato H, Kido D, et al. Impaired dental implant osseointegration in rat with streptozotocin-induced diabetes. J Periodontal Res. 2022. https://doi.org/10.1111/jre.12972.
Sanz M, Ceriello A, Buysschaert M, Chapple I, Demmer RT, Graziani F, et al. Scientific evidence on the links between periodontal diseases and diabetes: consensus report and guidelines of the joint workshop on periodontal diseases and diabetes by the International Diabetes Federation and the European Federation of Periodontology. J Clin Periodontol. 2018;45(2):138–49. https://doi.org/10.1111/jcpe.12808.
Takeda K, Mizutani K, Minami I, Kido D, Mikami R, Konuma K, et al. Association of periodontal pocket area with type 2 diabetes and obesity: a cross-sectional study. BMJ Open Diabetes Res Care. 2021;9(1). https://doi.org/10.1136/bmjdrc-2021-002139.
Demmer RT, Squillaro A, Papapanou PN, Rosenbaum M, Friedewald WT, Jacobs DR Jr, et al. Periodontal infection, systemic inflammation, and insulin resistance: results from the continuous National Health and Nutrition Examination Survey (NHANES) 1999–2004. Diabetes Care. 2012;35(11):2235–42. https://doi.org/10.2337/dc12-0072.
Colombo NH, Shirakashi DJ, Chiba FY, Coutinho MS, Ervolino E, Garbin CA, et al. Periodontal disease decreases insulin sensitivity and insulin signaling. J Periodontol. 2012;83(7):864–70. https://doi.org/10.1902/jop.2011.110349.
Saremi A, Nelson RG, Tulloch-Reid M, Hanson RL, Sievers ML, Taylor GW, et al. Periodontal disease and mortality in type 2 diabetes. Diabetes Care. 2005;28(1):27–32.
Shultis WA, Weil EJ, Looker HC, Curtis JM, Shlossman M, Genco RJ, et al. Effect of periodontitis on overt nephropathy and end-stage renal disease in type 2 diabetes. Diabetes Care. 2007;30(2):306–11. https://doi.org/10.2337/dc06-1184.
Iwasaki M, Taylor GW, Nesse W, Vissink A, Yoshihara A, Miyazaki H. Periodontal disease and decreased kidney function in Japanese elderly. Am J Kidney Dis. 2012;59(2):202–9. https://doi.org/10.1053/j.ajkd.2011.08.027.
Grubbs V, Vittinghoff E, Beck JD, Kshirsagar AV, Wang W, Griswold ME, et al. Association between periodontal disease and kidney function decline in African Americans: the Jackson Heart Study. J Periodontol. 2015;86(10):1126–32. https://doi.org/10.1902/jop.2015.150195.
National KF. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1-266.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–305. https://doi.org/10.1056/NEJMoa041031.
Araújo IC, Kamimura MA, Draibe SA, Canziani ME, Manfredi SR, Avesani CM, et al. Nutritional parameters and mortality in incident hemodialysis patients. J Ren Nutr. 2006;16(1):27–35. https://doi.org/10.1053/j.jrn.2005.10.003.
Herselman M, Moosa MR, Kotze TJ, Kritzinger M, Wuister S, Mostert D. Protein-energy malnutrition as a risk factor for increased morbidity in long-term hemodialysis patients. J Ren Nutr. 2000;10(1):7–15. https://doi.org/10.1016/s1051-2276(00)90017-7.
Niedzielska I, Chudek J, Kowol I, Slabiak-Blaz N, Kolonko A, Kuczera P, et al. The odontogenic-related microinflammation in patients with chronic kidney disease. Ren Fail. 2014;36(6):883–8. https://doi.org/10.3109/0886022X.2014.894764.
Brotto RS, Vendramini RC, Brunetti IL, Marcantonio RA, Ramos AP, Pepato MT. Lack of correlation between periodontitis and renal dysfunction in systemically healthy patients. Eur J Dent. 2011;5(1):8–18.
Harada F, Uehara O, Morikawa T, Hiraki D, Onishi A, Toraya S, et al. Effect of systemic administration of lipopolysaccharides derived from Porphyromonas gingivalis on gene expression in mice kidney. Med Mol Morphol. 2018;51(3):156–65. https://doi.org/10.1007/s00795-018-0181-3.
Sawa Y, Takata S, Hatakeyama Y, Ishikawa H, Tsuruga E. Expression of toll-like receptor 2 in glomerular endothelial cells and promotion of diabetic nephropathy by Porphyromonas gingivalis lipopolysaccharide. PLoS ONE. 2014;9(5): e97165. https://doi.org/10.1371/journal.pone.0097165.
França LFC, Vasconcelos ACCG, da Silva FRP, Alves EHP, Carvalho JS, Lenardo DD, et al. Periodontitis changes renal structures by oxidative stress and lipid peroxidation. J Clin Periodontol. 2017;44(6):568–76. https://doi.org/10.1111/jcpe.12729.
Fisher MA, Taylor GW, Shelton BJ, Jamerson KA, Rahman M, Ojo AO, et al. Periodontal disease and other nontraditional risk factors for CKD. Am J Kidney Dis. 2008;51(1):45–52. https://doi.org/10.1053/j.ajkd.2007.09.018.
Sharma P, Dietrich T, Sidhu A, Vithlani V, Rahman M, Stringer S, et al. The periodontal health component of the Renal Impairment In Secondary Care (RIISC) cohort study: a description of the rationale, methodology and initial baseline results. J Clin Periodontol. 2014;41(7):653–61. https://doi.org/10.1111/jcpe.12263.
Zhao D, Khawaja AT, Jin L, Li KY, Tonetti M, Pelekos G. The directional and non-directional associations of periodontitis with chronic kidney disease: a systematic review and meta-analysis of observational studies. J Periodontal Res. 2018;53(5):682–704. https://doi.org/10.1111/jre.12565.
Almeida S, Figueredo CM, Lemos C, Bregman R, Fischer RG. Periodontal treatment in patients with chronic kidney disease: a pilot study. J Periodontal Res. 2017;52(2):262–7. https://doi.org/10.1111/jre.12390.
•• Delbove T, Gueyffier F, Juillard L, Kalbacher E, Maucort-Boulch D, Nony P, et al. Effect of periodontal treatment on the glomerular filtration rate, reduction of inflammatory markers and mortality in patients with chronic kidney disease: a systematic review. PLoS One. 2021;16(1):e0245619. https://doi.org/10.1371/journal.pone.0245619. This systematic review showed that periodontal treatment improves CKD parameters, especially by reducing systemic inflammation and the risk of mortality.
Fang F, Wu B, Qu Q, Gao J, Yan W, Huang X, et al. The clinical response and systemic effects of non-surgical periodontal therapy in end-stage renal disease patients: a 6-month randomized controlled clinical trial. J Clin Periodontol. 2015;42(6):537–46. https://doi.org/10.1111/jcpe.12411.
•• da Silva TA, Abreu LG, Esteves Lima RP. A meta-analysis on the effect of periodontal treatment on the glomerular filtration rate of chronic kidney disease individuals: a systematic review and meta-analysis was conducted to assess the impact of the periodontal treatment on the glomerular filtration rate of individuals with chronic kidney disease. Spec Care Dentist. 2021;41(6):670–8. https://doi.org/10.1111/scd.12625.This systematic review shows that periodontal treatment significantly improves the GFR in patients with CKD.
•• Yue H, Xu X, Liu Q, Li X, Xiao Y, Hu B. Effects of non-surgical periodontal therapy on systemic inflammation and metabolic markers in patients undergoing haemodialysis and/or peritoneal dialysis: a systematic review and meta-analysis. BMC Oral Health. 2020;20(1):18. https://doi.org/10.1186/s12903-020-1004-1.This systematic review reported that non-surgical periodontal therapy can reduce serum hs-CRP levels but did not significantly change IL-6, Alb, TNF-α, and lipid metabolism markers in patients undergoing hemodialysis and/or peritoneal dialysis.
Chambrone L, Foz AM, Guglielmetti MR, Pannuti CM, Artese HP, Feres M, et al. Periodontitis and chronic kidney disease: a systematic review of the association of diseases and the effect of periodontal treatment on estimated glomerular filtration rate. J Clin Periodontol. 2013;40(5):443–56. https://doi.org/10.1111/jcpe.12067.
Nanditha Kumar M, Raghavendra Swamy KN, Thippeswamy HM, Kamath G, Devananda D. Prevalence of xerostomia in patients on haemodialysis: a systematic review and meta-analysis. Gerodontology. 2021;38(3):235–41. https://doi.org/10.1111/ger.12526.
Yoshioka M, Shirayama Y, Imoto I, Hinode D, Yanagisawa S, Takeuchi Y. Current status of collaborative relationships between dialysis facilities and dental facilities in Japan: results of a nationwide survey. BMC Nephrol. 2015;16:17. https://doi.org/10.1186/s12882-015-0001-0.
Ruospo M, Palmer SC, Craig JC, Gentile G, Johnson DW, Ford PJ, et al. Prevalence and severity of oral disease in adults with chronic kidney disease: a systematic review of observational studies. Nephrol Dial Transplant. 2014;29(2):364–75. https://doi.org/10.1093/ndt/gft401.
Chen LP, Chiang CK, Chan CP, Hung KY, Huang CS. Does periodontitis reflect inflammation and malnutrition status in hemodialysis patients? Am J Kidney Dis. 2006;47(5):815–22. https://doi.org/10.1053/j.ajkd.2006.01.018.
Siribamrungwong M, Puangpanngam K. Treatment of periodontal diseases reduces chronic systemic inflammation in maintenance hemodialysis patients. Ren Fail. 2012;34(2):171–5. https://doi.org/10.3109/0886022x.2011.643351.
• Mikami R, Mizutani K, Gohda T, Gotoh H, Matsuyama Y, Aoyama N, et al. Association between circulating tumor necrosis factor receptors and oral bacterium in patients receiving hemodialysis: a cross-sectional study. Clin Exp Nephrol. 2021;25(1):58–65. https://doi.org/10.1007/s10157-020-01952-2. This cross-sectional study demonstrated that the number of P. gingivalis in saliva was significantly associated with serum tumor necrosis factor receptor levels, which have been reported as a mortality predictor in patients undergoing hemodialysis.
Gohda T, Maruyama S, Kamei N, Yamaguchi S, Shibata T, Murakoshi M, et al. Circulating TNF receptors 1 and 2 predict mortality in patients with end-stage renal disease undergoing dialysis. Sci Rep. 2017;7:43520. https://doi.org/10.1038/srep43520.
• Mizutani K, Mikami R, Gohda T, Gotoh H, Aoyama N, Matsuura T, et al. Poor oral hygiene and dental caries predict high mortality rate in hemodialysis: a 3-year cohort study. Sci Rep. 2020;10(1):21872. https://doi.org/10.1038/s41598-020-78724-1. This prospective cohort study suggests that accumulated dental plaque and untreated decay, but not periodontal disease, are independently associated with all-cause mortality in patients undergoing hemodialysis.
Bossola M. Xerostomia in patients on chronic hemodialysis: an update. Semin Dial. 2019;32(5):467–74. https://doi.org/10.1111/sdi.12821.
Palmer SC, Ruospo M, Wong G, Craig JC, Petruzzi M, De Benedittis M, et al. Dental health and mortality in people with end-stage kidney disease treated with hemodialysis: a multinational cohort study. Am J Kidney Dis. 2015;66(4):666–76. https://doi.org/10.1053/j.ajkd.2015.04.051.
Stenvinkel P. Malnutrition and chronic inflammation as risk factors for cardiovascular disease in chronic renal failure. Blood Purif. 2001;19(2):143–51. https://doi.org/10.1159/000046932.
Liu Y, Coresh J, Eustace JA, Longenecker JC, Jaar B, Fink NE, et al. Association between cholesterol level and mortality in dialysis patients: role of inflammation and malnutrition. JAMA. 2004;291(4):451–9. https://doi.org/10.1001/jama.291.4.451.
Kopple JD, Zhu X, Lew NL, Lowrie EG. Body weight-for-height relationships predict mortality in maintenance hemodialysis patients. Kidney Int. 1999;56(3):1136–48. https://doi.org/10.1046/j.1523-1755.1999.00615.x.
Stompór T, Hubalewska-Hola A, Staszczak A, Sulowicz W, Huszno B, Szybinski Z. Association between gastric emptying rate and nutritional status in patients treated with continuous ambulatory peritoneal dialysis. Perit Dial Int. 2002;22(4):500–5.
Strid H, Simrén M, Stotzer PO, Abrahamsson H, Björnsson ES. Delay in gastric emptying in patients with chronic renal failure. Scand J Gastroenterol. 2004;39(6):516–20. https://doi.org/10.1080/00365520410004505.
Ioannidou E, Malekzadeh T, Dongari-Bagtzoglou A. Effect of periodontal treatment on serum C-reactive protein levels: a systematic review and meta-analysis. J Periodontol. 2006;77(10):1635–42. https://doi.org/10.1902/jop.2006.050443.
Demmer RT, Trinquart L, Zuk A, Fu BC, Blomkvist J, Michalowicz BS, et al. The influence of anti-infective periodontal treatment on C-reactive protein: a systematic review and meta-analysis of randomized controlled trials. PLoS ONE. 2013;8(10): e77441. https://doi.org/10.1371/journal.pone.0077441.
Franek E, Blaschyk R, Kolonko A, Mazur-Psonka L, Łangowska-Adamczyk H, Kokot F, et al. Chronic periodontitis in hemodialysis patients with chronic kidney disease is associated with elevated serum C-reactive protein concentration and greater intima-media thickness of the carotid artery. J Nephrol. 2006;19(3):346–51.
Cholewa M, Madziarska K, Radwan-Oczko M. The association between periodontal conditions, inflammation, nutritional status and calcium-phosphate metabolism disorders in hemodialysis patients. J Appl Oral Sci. 2018;26: e20170495. https://doi.org/10.1590/1678-7757-2017-0495.
De Marchi RJ, Hugo FN, Hilgert JB, Padilha DM. Association between oral health status and nutritional status in south Brazilian independent-living older people. Nutrition. 2008;24(6):546–53. https://doi.org/10.1016/j.nut.2008.01.054.
Samnieng P, Ueno M, Shinada K, Zaitsu T, Wright FA, Kawaguchi Y. Oral health status and chewing ability is related to mini-nutritional assessment results in an older adult population in Thailand. J Nutr Gerontol Geriatr. 2011;30(3):291–304. https://doi.org/10.1080/21551197.2011.591271.
Mikami R, Mizutani K, Matsuyama Y, Gohda T, Aoyama N, Matsuura T, Kido D, Takeda K, Saito N, Fujiwara T, Izumi Y, Iwata T. Association of type 2 diabetes with periodontitis and tooth loss in patients undergoing hemodialysis. PLoS One. 2022;17(5):e0267494. https://doi.org/10.1371/journal.pone.0267494.
Funding
This work was supported by a Grant-in-Aid for Research from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (grant number: 19K10125 for KM and 20K18497 for RM).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oral Disease and Nutrition
Rights and permissions
About this article
Cite this article
Mizutani, K., Mikami, R., Saito, N. et al. Periodontal Disease and Chronic Kidney Disease: the Impact of Oral Health on Inflammation and Nutrition in Patients Undergoing Hemodialysis. Curr Oral Health Rep 9, 81–88 (2022). https://doi.org/10.1007/s40496-022-00313-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40496-022-00313-0