Abstract
Purpose
The shoulder pain is one of the main causes that lead the patient to medical evaluation. Today, the ultrasound (US) represents an essential tool in the orthopaedical, rheumatological and rehabilitative setting to address the musculoskeletal causes of pain. Amongst the commonest causes of shoulder complains lay the frequent subacromial chronic bursitis (SACB). In this condition, the thickening of the bursal walls and subsequent fusion of the two synovial sheets leads to the reciprocal loss of bursal walls gliding under the subacromial space and consequently pain. This condition represents a common cause of shoulder pain and may be easily addressed by musculoskeletal sonographers. The purpose of this paper will be to describe the US appearance of SACB and to evaluate the efficacy of US-guided hydrodilation in its treatment.
Methods
We included patients with painful shoulder attending our outpatient clinic for shoulder complains with the diagnosis of SACB with a bursal wall > 1.5 mm. A group was treated via US-guided hydrodilation, while the control group was treated via a classical blind approach using triamcinolone acetonide. Both groups underwent the same rehabilitation program following the injections. The shoulder functionality was assessed via qDASH questionnaire at baseline, days 3, 7, 14, 30, 60, and 90. A p <0.05 was considered significant.
Results
Both groups displayed a significant reduction of pain; nevertheless, in the group treated with US-hydrodilation, there was no need for re-treatment.
Conclusions
The US-guided hydrodilation for SACB should be the preferred technique to detach bursal walls and improve patient symptoms, since it requires fewer invasive maneuvers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The shoulder pain is one of the main causes that lead the patient to medical evaluation. A careful anamnesis and physical examination often help the physician to suspect the causes of pain, in particular impingement tests may be exploited in clinical practice to suspect a precise shoulder pathology. However, despite clinical evaluation allows to suspect the cause of pain, today the ultrasound (US) represent an essential tool in the orthopaedical, rheumatological and rehabilitative setting to study osteo-articular, tendon and muscular structures [1]. In fact, US represent a rapid, low cost and safe examination that allows to fully examine gleno-humeral joint and to investigate the major cause of pain at this level. The most common causes of painful shoulder are represented by pathology of the rotator cuff tendons (lesions, crystal deposition disease, enthesitis), glenohumeral osteoarthritis, osteonecrosis of the humeral head, alterations of the long head of biceps tendon (instability from lesion of the pulley, tendinosis, tenosynovitis), degenerative and traumatic alterations of the acromion-clavicular joint, arthrosynovitis, adhesive capsulitis and, above all, subacromial chronic bursitis (SACB). This latter condition represent a common cause of shoulder pain and it is sonographically characterized by the thickening of the bursal walls and subsequent fusion of the two synovial sheets which lead to the reciprocal loss of bursal walls gliding under the subacromial space and consequently pain. The SACB represent often the result of an untreated chronic subacromial-deltoid impingement or the unfavourable evolution of a calcific tendinopathy with bursal involvement, and these conditions may lead to a severe reduction of quality of life of the affected patients. The altered gliding of subacromial deltoid bursal walls in the subacromial region, with subsequent bursal chronic inflammation and thickening, generates painful arm abduction and flexion. Moreover, this condition may be associated with rest pain also present during night-time and clinically it may act as a mimicker of adhesive capsulitis. In this prospective study we will briefly describe the sonoanatomy of this type of SACB that we will define as fibro-adhesive chronic bursitis and evaluate the efficacy of the US-guided percutaneous hydrodilation of the bursal sheets in such clinical scenario.
Anatomy of the subacromial deltoidal space and fibro-adhesive bursitis pathophysiology
The gleno-humeral joint represents the most complex articulation of the human body. The shoulder joint can be divided into 4 components: scapulo-humeral, acromion-clavicular, sterno-clavicular, and scapulo-thoracic. The rotator cuff, which serves as humeral-head stabilizer and its centerer in the glenoid cavity, is composed by four tendons: supraspinatus, subscapularis, infraspinatus, and teres minor. The subacromial space is a cavity partially covered by the inferior surface of acromion and acromion-clavicular joint, while its anterior part is completed by the coraco-acromial ligament and represent the tunnel where the supraspinatus tendon glides during arm abduction [2]. Between the inferior bony surface of the acromion, the coraco-acromial ligament and the upper part of the supraspinatus tendon lies the subacromial bursa that is the biggest of human body [3]; it is placed between the tendons of the rotator cuff, the deltoid and the coraco-acromial arc. The subacromial-subdeltoid bursa (SASDB) represent a synovial sac with walls made by connective tissue covered by a membrane which contains synovial fluid and serves as a friction reducing system. In fact, the function of the SASDB is to act as a cushion between the cuff tendons and the surrounding structures; in particular, it promotes the sliding of the supraspinatus tendon within the subacromial space and reduces the friction of the tendon against the coraco-acromial bone roof during arm abduction.
The term ‘impingement’ was coined for the first time by Neer [4] and refers to the impaired sliding of the supraspinatus tendon below the coraco-acromial vault and it is a consequence of morphological and structural alterations of the coraco-acromial arch and altered biomechanics of the shoulder. The increase in pressure at this level can cause inflammation of the SASDB with consequent bursal wall thickening, pain, as well as cause tendinosis and superficial tendon lesions thus affecting the supraspinatus and infraspinatus.
US-appearance of fibro-adhesive subacromial bursitis
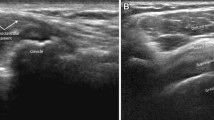
The chronic fibro-adhesive type of SASDB displays usually US features easy to recognize (Fig. 1):
-
Overall bursal thickness measured from the superficial limit of the upper wall to the deep limit of the lower wall > 1.5 mm;
-
The SACB generally displays various degrees of increased echogenicity, however it sometimes may also appear hypoechoic: in this case, the content of the bursa, made up of minimal fibrinous exudate, is generally hypoechoic, non-homogeneous and partly organized into connective septae;
-
Not frequently a wavy aspect of SACB may be present, sometimes appearing with a rosary crown pattern (Fig. 2);
-
When the bursal thickness causes impingement, the "step sign" may be present (Fig. 3): i.e. the imprint and depression of the coraco-acromial ligament on the thickened SASDB in the axial US section of the ligament [5].
Material and methods
We enrolled patients referred to our centre for painful shoulder and a various degree of range of motion reduction that displayed a bursal thickening higher than 1.5 mm. Indeed, the exclusion criteria were the presence of subacromial essudative anechoic fluid bursitis, severe symptomatic gleno-humeral ostheoarthritis, rotatory cuff tendon tear and adhesive capsulitis [6, 7]. We included patients fulfilling the US criteria refractory to conservative therapies with physical treatments. Our rehabilitative protocol consisted of 2 phases for both groups of patients. The first phase (phase 1) in the US-guided approach consisted of stinging and detaching the two stuck sheets of the synovial bursa, washing SASDB: with the patient laying supinated on a medical bed and the forearm held in a palm-up position put under the glutei we individuated via US the two layers of the bursal wall between the deltoid muscle and supraspinatus, then we carefully disinfected patient’s skin with an iodopovidone-chlorhexidine solution and covered the linear multifrequency probe 6–18 MHz with a dedicated sterile hood; subsequently, we used a 18 G needle to inject the SASDB and washed it with 0,9% saline solution until the bursal walls and fibrous septae were completely broken and separated by the injection pressure (during this process the tip of the needle was also used for this purpose, Fig. 4). When the septae were completely broken and the bursa adequately distended, we injected 2 mL of medium molecular weight hyaluronic acid and 40 mg of triamcinolone acetonide to complete the procedure. In the control group, phase 1 consisted of a classical blind anterior SASDB injection with 40 mg of triamcinolone acetonide in the rotator interval of the painful shoulder. Phase 2 for all subjects consisted in a rehabilitative protocol of 3 weeks with 3 sessions per week:
- 1st week: laser therapy + subacromial ultrasound and shoulder rotation exercises;
- 2nd week: strengthening exercises of the humeral head depressors and shoulder retropulsors;
- 3rd week: strengthening of the rotator cuff muscles and postural correction of the cervical-dorsal spine.
In both groups we administered the quick DASH (q-DASH) questionnaire at baseline, after 3,7,14 days, then every month until 3 months of follow up were reached.
The US exploited machinery was an Esaote MyLab Twice®.
Statistical analysis
Descriptive statistics was used to define anthropometric variables and qDASH means at baseline and at each follow up. The normality assumption was evaluated with Saphiro and Wilk test. The ANOVA-Friedman multiple comparison test was exploited to compare the qDASH means between every observation period. The test U of Mann was used to compare the qDASH means between each follow up between the two groups of patients in order to highlight any difference in efficacy between the two techniques. Statistical analysis was carried out with GraphPad Prism® software version 9.4.1. A p < 0.05 was considered significant.
Results
We enrolled 60 subjects: 30 were treated under US-guidance and 30 were treated blindly. Mean age was 41.4 ± 11.14 years, male to female ratio was 18:12 for both groups. In both groups we displayed a significant reduction of qDASH after 1 week from the treatment (p < 0.0001) that persisted significantly lower than baseline values at each follow up (p < 0.0001; Fig. 5). In Table 1 are reported the mean values of qDASH questionnaire at baseline and each subsequent follow-up, Table 2 displays the percentage reduction of qDASH in cases and controls compared to baseline. In the blindly treated group several patients needed a retreatment for symptoms’ persistence: at T-14 25 patients (83.3%), at T-30 14 patients (46.6%) and at T-60 7 patients (23.3%). In the US-guided treatment any patient required a re-treatment (Table 3). Any significant adverse event was recorded in both groups.
Discussion
Fibro-adhesive bursitis represents a common chronic inflammatory condition of SASDB which may be easy to diagnose even by low experienced musculoskeletal sonographers. Indeed, it never appears with an anechoic fluid film associated with synovial hypertrophy or power doppler signal in the bursa and it is characterized by the full thickening of the bursal walls with the fibrinous consolidation of it content. Although some authors in the literature report a maximum normal value of 0.8 mm [8], in our work we considered a safe pathological thickening a value of at least > 1.5 mm with a various degree of bursal echogenicity. In the most chronic forms SACB may also display modifications of its profile, showing a wavy aspect up to a clear ‘rosary crown’ appearance and being frankly hyperechogenic (Fig. 2). The presence of an impingement may be documented at the subacromial deltoidal level with the coraco-acromial ligament determining a “step sign” on the bursa in transverse scan [5]. Adhesive capsulitis clinically may mimic fibro-adhesive chronic bursitis, but frozen shoulder shows significant reduction of both active and passive shoulder motion and it is characterized by the painful limitation in external as well as internal rotation, while in fibro-adhesive bursitis the passive movements are never so limited. Moreover, in frozen shoulder a bursal wall thickness usually lays between normal limits. However both pathologies may be clinically similar and US is of utmost importance to correctly perform a differential diagnosis [6, 7].
In the present study we evaluated the efficacy and safety of percutaneous US-guided hydrodilation of fibro-adhesive bursitis in a group of patients attending our outpatient clinic for painful shoulder followed by a rehabilitation program. In both groups was documented a significant improvement of symptoms after the treatment, however in the group treated with the percutaneous US-guided approach a higher and more rapid reduction of symptoms was achieved; moreover, in this group there was not any need for retreatment. Conversely, in the group of patients treated via blind approach was often required a retreatment, thus testifying, as already documented by other authors [9, 10], that US-guided procedures act superiorly than those blindly conducted. In this context, performing less invasive manoeuvres mean that patients must attend fewer visits with the physicians and, more importantly, that the lower number of injections may reduce the risk of complications, such as infections. Moreover, the higher rate of retreatment in the blind technique group testify that it is impossible to obtain the same results as via US-guidance that allows to fully detach the thickened bursal walls thus obtaining a better clinical result. The need for a rehabilitation plan for the painful shoulder represent an important adjunct in the clinical management of such conditions and it represent the basis to succeed while dealing with these patients. Nevertheless, from our point of view, treating such conditions with the sole physiotherapy and physical therapy may have led to a longer rehabilitative program and rehabilitation, thus leading to a higher economic burden for the patient and to a slower quality of life restoration.
Study limitations
This paper has some limitations since there was a lack of randomization, moreover this is the first paper that describes the condition of fibro-adhesive bursitis which has been individuated by the experience of the authors as musculoskeletal sonographers. It is possible that fibro-adhesive bursitis also occurs in patients with a thickness less than 1.5 mm, however, in this study we focused on patients with symptomatic bursal thickening that was certainly pathological.
Conclusions
The US-guided percutaneous SACB hydrodilation represent a safe and valid tool in the every-day scenario for patients with symptoms and US-findings suggestive of fibro-adhesive bursitis (walls thicker than 1.5 mm) and it should be preferred over blind corticosteroid injections since it requires fewer invasive manoeuvres.
References
Chang KV, Wu WT, Hsu PC, Lew HL, Özcakar L (2020) Clinical tests of the shoulder: accuracy and extension using dynamic ultrasound. Am J Phys Med Rehabil. https://doi.org/10.1097/PHM.0000000000001311
Precerutti M, Garioni E, Madonia L, Draghi F (2010) US anatomy of the shoulder: pictorial essay. J Ultrasound 13:179–187. https://doi.org/10.1016/j.jus.2010.10.005
Ivanoski S, Nikodinovska VV (2019) Sonographic assessment of the anatomy and common pathologies of clinically important bursae. J Ultrason 19:212–221. https://doi.org/10.15557/JoU.2019.0032
Csi NEER (1972) Anterior acromioplasty for the chronic impingement syndrome in the shoulder a preliminary report. J Bone Jt Surg 54:41–50
Stella SM, Trentanni C, Ciampi B et Al. Ecografia Patologica Muscoloscheletrica, Testo e Atlante. In: Galletti S (ed) Piccin Editore Padova, 2018, p. 438–9
Stella SM, Gualtierotti R, Ciampi B, Trentanni C, Sconfienza LM, Del Chiaro A, Pacini P, Miccoli M, Galletti S (2021) Ultrasound features of adhesive capsulitis. Rheumatol Ther. https://doi.org/10.1007/s40744-021-00413-w
Al Khayyat SG, Falsetti P, Conticini E, Frediani B, Galletti S, Stella SM (2023) Adhesive capsulitis and ultrasound diagnosis, an inseparable pair: a novel review. J Ultrasound 26:369–384. https://doi.org/10.1007/s40477-022-00725-9
Holsbeeck M, Van JI (2016) Musculoskeletal ultrasound. Third edit.
D’Alessandro R, Falsetti P, Conticini E, Al Khayyat SG, Bardelli M, Baldi C et al (2021) Difference in pain and accuracy of two hyaluronic acid injection techniques for symptomatic knee osteoarthritis in overweight patients. Reumatologia 59:23–6. https://doi.org/10.5114/reum.2021.103646
Schneeweiss W, Puggioni A, David F (2012) Comparison of ultrasound-guided vs. “blind” techniques for intra-synovial injections of the shoulder area in horses: Scapulohumeral joint, bicipital and infraspinatus bursae. Equine Vet J 44:674–678
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
The present study was conducted in accordance to the Declaration of Helsinki and it’s late amendments, moreover it was approved by our local ethical committee (“Rhelabus” protocol number 22271).
Informed consent and Consent to publish
Informed consent and consent to publish were obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Al Khayyat, S.G., Stella, S.M., Trentanni, C. et al. Ultrasound definition of subacromial chronic “fibro-adhesive” bursitis and its treatment via ultrasound guided hydrodilation: a prospective pilot study. J Ultrasound 27, 599–604 (2024). https://doi.org/10.1007/s40477-024-00894-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-024-00894-9