Abstract
Aims
To identify and highlight pertinent US features that could serve as imaging biomarkers to describe different patient phenotypes, within Great Trochanteric Pain Syndrome (GTPS) clinical diagnosis.
Materials and methods
Using ultrasound we evaluated eighty-eight clinically diagnosed patients with GTPS, for tendon matrix changes and calcium deposits in the gluteus medius (superoposterior and lateral aspects) and in the gluteus minimus. Peritrochanteric examination included fascia lata, trochanteric bursa, cortical irregularities and the presence of enthesophytes. The association of pathological changes with pain and functionality was evaluated using multivariate regression models.
Results
Out of the 88 patients, 86 examinations (97.7%) detected gluteus medius tendinopathy, and 54 patients (61.4%) had gluteus minimus tendinopathy in addition. Calcium deposits were present in 97.7% of patients, associated with tenderness (p = 0.009), and most often located in the gluteus medius rather than in the gluteus minimus (p = 0.014); calcifications were associated with tendon thickness (p = 0.042), hypoechogenicity (p = 0.005) and the presence of partial tears (p = 0.030). Bursa swelling occurred in 36 patients (40.9%); multivariate regression models predicted less pain in patients with bursa distension (p = 0.008) and dysfunction in patients with gluteal muscle atrophy (p = 0.001) and loss of fibrillar pattern in the gluteus medius (p = 0.002).
Conclusion
GTPS involves both degenerative calcifying gluteal tendinopathy and alterations in the peritrochanteric space associated with physical function and pain. The severity of GTPS can be assessed using ultrasound imaging biomarkers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Greater trochanteric pain syndrome (GTPS), formerly known as trochanteritis, is a term that embraces pain generated by traumatic and/or degenerative lesions involving tendons, bursae, trochanteric osseous structure and other anomalies of the peritrochanteric space [1,2,3,4,5,6,7,8,9]. The primary causes of symptoms in patients with GTPS are tendinopathy of the gluteus medius (GMED) and/or minimus tendon (GMIN) [10, 11]. Gluteal tendinopathy is the most prevalent of all lower limb tendinopathies with an incidence of 1.8–5.6 per 1000 annually, affecting 10–25% of the population [12,13,14,15]. The prevalence of gluteal tendinopathy increases with age and typically affects women in their fourth to sixth decades of life [16]. The dysfunction and quality of life of people with gluteal tendinopathy has been shown to be similar to people with end-stage hip osteoarthritis (OA) [17].
The clinical diagnosis of GTPS is based on history, pain on palpation, and findings from provocative physical examination maneuvers. Magnetic resonance imaging (MRI) is the gold standard for confirmation of diagnosis and MRI studies have shown changes in GMED and GMIN insertions at the greater trochanter (GT), muscle fatty atrophy and bursa distension [8, 18]. To better understand GTPS progression and severity, a MRI scoring system (Melbourne Hip MRI score) with five categories has been proposed recently [19]. Similarly, to guide endoscopic management, Lall et al. have proposed an endoscopic grading system with six categories of severity [20]. Likewise, an intraoperative GTPS classification system was useful for driving a stage-adjusted surgical technique and rehabilitation protocol [21, 22].
Models of severity of stage tendinopathy based on US imaging have been proposed for Achilles and patellar tendons [4], but not for gluteal tendons. The diagnostic capabilities of modern US equipment have improved for deep regions, such as the gluteal tendons, and are thus effective for detection and description of gluteal tendinopathy and peritrochanteric pathology in the earlier stages. Ultrasound was effective in the diagnosis of GTPS with a sensitivity of 79% for gluteal tendon tears and 61% for bursa pathology [23]. Although MRI is considered by some authors as the gold standard in GTPS diagnosis, MRI evidence of bursal fluid is commonly present in asymptomatic hips, with detection rates as high as 65–88% [24, 25]. Thus, our study was not meant to assess ultrasound specificity in GTPS diagnosis, but to describe ultrasound findings associated with the clinical diagnosis of GTPS.
We aimed to determine the sonographic pathoanatomy of the gluteal medius and minimus tendons, named here as tendinopathy. We examined changes in echogenicity (hypoechogenicity, heterogeneous echogenicity and loss of fibrillar pattern), changes in thickness, calcifications and partial tendon tears [26, 27]. To explain other structural pathologies associated to the clinical diagnosis of GTPS, we also examined the peritrochanteric space, including the fascial structures next to these tendons: fascia lata (FL)/proximal iliotibial band, trochanteric bursae, subcutaneous fat tissue. We assessed muscle atrophy qualitatively by comparing the gluteal muscles with the quadriceps muscles. In addition, the presence of cortical irregularities and enthesophytes on the greater trochanter facets were recorded. Finally, we investigated their potential association with pain and functional impairment in a clinically diagnosed GTPS population. The essence is to identify and highlight pertinent US features that could serve as imaging biomarkers to identify different patient phenotypes, within GTPS clinical diagnosis.
Methods
Patient selection
The study was performed in the ultrasonography unit of the Radio-diagnostic Services in a tertiary hospital. Orthopedic surgeons specialized in hip pathology performed the clinical GTPS diagnosis, based on flexion/abduction/external rotation and palpation (direct compression) of the soft tissues overlying the greater trochanter. We examined patients complaining from lateral hip pain for pain on resisted abduction and resisted internal rotation of the thigh, abductor strength through extension of the hip and knee and internal rotation at the hip. All patients were positive to the following pain provocation tests: “jump sign” after direct palpation of the greater trochanter [18] and the “single leg stance” test (pain within 30 s of standing on one leg) [18]. All the patients had standardized anterior–posterior x-ray in supine centered on the pelvis. Eventually, we performed MRI to rule out severe hip OA or lumbar pathology. Inclusion/Exclusion criteria are shown in Table S1 (Supplementary Material).
We assessed one hundred nine patients for eligibility between January 2020 and January 2022. Fifteen did not meet the inclusion criteria. The reasons were severe hip OA (n = 4), hip prosthesis (n = 1), massive tendon rupture (n = 2), lumbar pathology (n = 3), BMI > 35 (n = 2) and nine declined to participate. Eighty-eight patients were recruited and informed consent was obtained from the patients before the commencement of the study. The Local Ethics Committee (2,019,028) approved the study, which was performed in accordance with the ethical standards in the 1964 declaration of Helsinki.
We used Hip Outcome Score (HOS) self-reported questionnaire as a tool for measuring functional disability. To assess patient-reported pain, we used the pain visual analogue scale (VAS-P, 0–10 Likert scale), which is a unidimensional measure for pain intensity. Scores were recorded by making a handwritten mark on a 10-cm line that represents a continuum between “no pain” and “worst pain”.
Ultrasound examination
A senior radiologist with more than 15 years’ experience in musculoskeletal interventional ultrasonography performed all US assessments using a LOGIQ E10 ultrasound system (GE Healthcare, CHI, IL, USA), equipped with a high frequency linear array probe (6–15 MHz). Further retrospective evaluation of images was performed for inter-observer reliability using the GE Healthcare’s Pictures Archiving and Communication System (CHI, IL, USA). A second radiologist with 12 years of musculoskeletal ultrasound experience, blind to the other observer’s findings assessed retrospectively the ultrasound images.
Evaluation of gluteal tendon pathology
Patient was positioned over the non-affected side in lateral decubitus with both knees extended. First, we identified the osseous facets. The transducer is positioned over the superior facet in short axis and we move the transducer over the tendon insertion obtaining an optimal long axis view of the posterior band of the GMED (posterior coronal oblique orientation). We move the transducer over the lateral facet in short axis and then rotate it to see the long axis of the lateral band of the GMED (anterior coronal oblique orientation). Finally, we move the transducer over the bared area towards the anterior facet in short axis and rotate the transducer slightly anterior to see the long axis of the GMIN. Sonographically the anterior and posterior bands of the GMED tendon can be differentiated by their morphologic characteristics [28]. GMED has a bipennated structure, including a robust/strong posterior band, which inserts onto the superoposterior facet of the greater trochanter (GT) and the thinner anterior band, which inserts onto the lateral facet. The superoposterior and lateral aspects of the GMED were evaluated independently for changes in echotexture, categorized as hypoechogenic, heterogeneous echogenicity, (i.e. not homogeneous echogenicity and loss of fibrillar pattern), and partial tears (defined as focal anechoic areas with interruption of fibrillar pattern). Changes in morphology (thick > 5 mm, thin < 3.5 mm, normal) (3.5–5 mm) were recorded as well as calcium deposits within the tendons or tendon surface. Although we have not included a control group, we have chosen these values based on our experience. The same features were evaluated for GMIN.
Evaluation of peritrochanteric pathology
The proximal iliotibial band (ITB) is depicted during the examination of the greater trochanter with the patient in the same position as described above. The ITB origin is identified first with the probe in the long-axis and then short-axis images are obtained. The ITB origin and the origin of the FL are typically described together because these structures are directly adjacent to and difficult to distinguish from each other. In pathological cases, nodular thickness with or without decrease of its echogenicity can be observed.
Bony alterations were rated dichotomously and included the presence of enthesophytes, i.e. osseous exostosis in facetary insertions and cortical irregularities along the greater trochanter. The latter were categorized as mild, i.e. a single cortical irregularity and severe, more than one cortical irregularities. We identified the trochanteric bursa merely, which is associated to GTPS according to most authors [26]. Distensions of the greater trochanteric bursa, defined as an anechoic fluid collection within the bursa, were recorded [26].
During the assessment of GMED and GMIN tendons, the presence of muscle atrophy (fat infiltration of the muscle with increase in its echogenicity compared to the quadriceps muscle) was also considered dichotomously (yes/no).
Statistical analyses
For the descriptive analyses, means and standard deviations were used for the continuous variables, and absolute (count) and relative frequencies (percentage) for the categorical variables. χ2 (Chi-square) tests were used to compare the data sets of US pathologies. Pearson’s tests were used to assess the association between continuous variables. Inter-radiologist reliability for the ultrasound structural pathologies was calculated using Cohen’s kappa coefficient, after retrospective evaluation of all the ultrasound images, which were taken following a standardized protocol. To analyze the relationship between the possible predictor variables (including sociodemographic and clinical factors, and structural pathology assessed by ultrasound) and the level of pain (VAS score) and functionality (HOS score), multivariate analyses were performed using multiple linear regressions. In doing so, we obtain a linear relationship between independent variables (clinical and ultrasound characteristics) each of them pondered by a regression coefficient and the dependent variable, i.e. self-reported pain (VAS-P) or function (HOS) scores. The best models were chosen following a stepwise backward strategy using likelihood ratio tests (with a significance criteria of p < 0.05). All analyses were performed with SPSS v28.
Results
The sonographic pathoanatomy of GTPS was assessed in 88 patients (90.9% were female) that had been clinically diagnosed by specialized hip orthopedists. Clinical and demographic characteristics of the cohort are summarized in Table 1.
Two patients showed normal gluteal ultrasound anatomy; the latter is illustrated in Fig. 1; in these patients ultrasound examination revealed a nodular hypoechoic fascial thickening [1], showing tenderness when applying pressure with the probe.
Long axis view of normal ultrasound anatomy of gluteus medius and minimus tendons. Tendons are isoechogenic with gluteus muscles and shows a normal and well organized parallel fibrillar pattern. a Long axis ultrasound image shows the insertion of lateral portion of gluteus medius on the lateral facet of the greater trochanter (arrow). b Long axis ultrasound image displays the insertion of superoposterior portion of gluteus medius on superoposterior facet of the greater trochanter (arrow). c Long axis ultrasound image displays insertion of gluteus minimus at anterior facet of the greater trochanter (arrow). LF lateral facet, SPF superoposterior facet, AF anterior facet
Insertional pathoanatomy of the gluteus medius and minimus
Main ultrasound findings, associated with clinical GTPS, were echotexture alterations in the lateral insertion of the GMED; this feature was evident in 86 patients (97.7% of our cohort). Concomitantly, 74 patients (84.1%) had pathological alterations at the superoposterior insertion.
The number and frequency of pathological echotexture findings, according to the detailed anatomy are summarized in Table 2. Tendinopathy at the lateral insertion of GMED plus GMIN tendinopathy were present in 54 patients (61.4%) with a substantial inter-observer agreement (Supplementary Material, Table S2).
When comparing the frequency of pathological changes by anatomical area, the superoposterior branch of the GMED presented more physiological echotexture than the lateral insertion (χ2(2) = 14.63; p = 0.001), with fewer inhomogeneous abnormalities (χ2(2) = 9.71; p = 0.008), and interstitial tears (χ2(2) = 21.17; p < 0.001).
Representative sonographic images of specific alterations found in echotexture, including hypoechoic/inhomogeneous abnormalities, the loss of fibrillary pattern and partial tears are shown in Fig. 2.
Echogenic alterations of gluteus medius at lateral facet of the greater trochanter. a Long axis ultrasound image demonstrates hypoecogenicity and focal thinning on lateral insertion, marked with crosses. b Long axis ultrasound image reveals heterogeneous echogenicity on insertion at the greater trochanter (of note the increase of echogenicity on bursal surface and the hypoechogenicity on bone surface) (arrow). c Long axis ultrasound image reveals loss of fibillar pattern at the insertion on the greater trochanter (arrow). d Long axis (left) and short axis (right) ultrasound images demonstrate a focal anechoic gap consistent with partial tendon tear (the gap is measured with crosses in the three dimensions)
Calcium deposits were present in 86 patients (97.7%), located in either the superoposterior (38) or lateral branches (46) of the GMED and/or GMIN (16) (Fig. 3). Of note, the presence of calcifications at GMIN was less frequent than at GMED (χ2(2) = 8.56; p = 0.014). At GMED there were significant associations of calcium deposits with other pathological alterations, such as tendon thickness, (χ2(2) = 6.62; p = 0.037) or partial tears (χ2(1) = 7.72; p = 0.005). In GMIN, calcifications were associated with hypoechogenicity (χ2(1) = 7.94; p = 0.005), the presence of partial tears (χ2(1) = 4.69; p = 0.030) and tendon thickness (χ2(2) = 6.33; p = 0.042). Figure 3 depicts representative ultrasound images of calcium deposits.
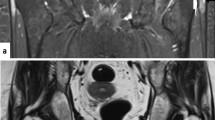
Representative ultrasound images of gluteal calcific tendinopathy. a Long-axis sonographic image demonstrates an echogenic foci, with cloud appearance and without posterior shadowing, measured between crosses at the transition of superoposterior and lateral insertions at the greater trochanter. b Long-axis ultrasound image reveals an echogenic arciform calcium deposit (measured between crosses) without posterior shadowing at the lateral insertion of the gluteus medius
Pathology in the peritrochanteric space
Table 3 shows the findings in the peritrochanteric spaceFocal nodules were present in 51 patients (58%) in which the inter-observer agreement was almost perfect (Supplementary Material Table S3). Mean nodular thickness was 4.498 ± 1.039 mm. Of note, in two patients fascia lata thickening was the only ultrasound abnormal finding (Fig. 4). Trochanteric bursa distension was evident in 36 patients, representing a frequency of 40.9% of GTPS patients (Fig. 5).
Long axis ultrasound image demonstrates trochanteric bursa distension under fascia lata and over lateral insertion of gluteus medius (arrows). Of note, ultrasound image also demonstrates gluteus medius tendinopathy on the lateral insertion and severe cortical irregularities on lateral facet of the greater trochanter
Prevalent anomalies in the peritrochanteric space are cortical irregularities present in 77 patients (87.5%) (Fig. 5); the inter-radiologist agreements were substantial (Table S3). Enthesophytes (Fig. 6a) were present in 30 patients and showed a positive correlation with muscular atrophy (χ2(1) = 4.63, p = 0.032).
Cortical irregularities. a Long-axis sonographic image shows an osseous peak (exostosis) in the transition of lateral and anterior facets of greater trochanter, arrow. b Long-axis sonographic image reveals one irregularity on cortical surface of lateral facet (arrow). c Long-axis sonographic image shows several irregularities on cortical surface of lateral facet (arrows). LF lateral facet
Relationships between pain (VAS-P) and physical function (HOS) with US pathologies associated with GTPS
GTPS limits performance of common functional tasks. HOS (Activity of Daily Living Scale) is a self-reported questionnaire from 0 to 100 with 0 being the worst level of common functional tasks. Pain intensity is measured as a handwritten mark on a 10-cm line that represents a continuum between “no pain” and “worst pain”. There was a negative correlation between baseline clinical scores, HOS and VAS-P, r = − 0.523, p < 0.001.
Our results show that those patients with the lack of parallel-aligned fibers in the lateral branch of the gluteus medius reported worse functionality (Hip Outcome Score, HOS). We found this relationship in the lateral but not in the superoposterior branch.
In order to identify potential sources of pain, all imaging biomarkers and their relationship with self-reported pain (VAS-P) were analyzed using multivariate regression algorithms. Table 4a presents the final model of self-reported pain and its relationship with US biomarkers (all variables with low/non-significant contribution to the model were eliminated). Merely, the presence of distension in the trochanteric bursa predicted less pain intensity. The other structural pathologies did not show any significant relationship with self-reported pain. According to this model, the presence or not of a distended bursa explains 6.9% of the variability found in pain intensity; pain decreased by 1.01 points when the trochanteric bursa was distended. As shown in Table 4a, the association is described by the following equation: Pain = 7.46–1.01*(1 = bursa distension is present or 0 = bursa distension is not present).
We also performed a multivariate regression analysis to explore potential relationships between US pathologies underlying GTPS and impaired function (performance of common functional tasks as assessed by HOS). We found that gluteus muscle atrophy and the loss of normal fibrillar pattern in the lateral branch of the GMED contributed to impaired physical function, p = 0.001 and p = 0.002 respectively. As shown in Table 4b, the HOS score decreased by 13.71 and 12.12 points in the presence of muscle atrophy and lateral loss of the normal fibrillar pattern. However, in those patients with loss of the normal fibrillar pattern in superoposterior branch physical function increased by 10.69 points, p = 0.007.
The significant relationship between these pathologic changes and function is predicted by the following equation, Y = 62.74 – 13.71 X1 − 12.12 X2 + 10.69 X3.
Y, physical function (HOS); X1, muscle atrophy; X2, loss of fibrillar pattern in the lateral branch of GMED; X3, loss of fibrillar pattern in the superoposterior branch of GMED.
Discussion
The quality of ultrasound machines and probes is rapidly improving, and can help identify imaging biomarkers describing different patient phenotypes (or disease stages) according to specific pathological findings. In addition, careful ultrasound examination can help to identify targets for percutaneous treatment of GTPS patients. Here we report some ultrasound findings that have not been described with MR imaging. Broadly, MRI has established five grades of progressive gluteal tendon degeneration [19, 20], specifically Grade 1 bursitis (with minimal tendon changes); increased tendon signal on T1-weighted images as the predominant sign in Grade 2 tendinopathy and Grade 3 involving partial-thickness tears. The severe stages included Grades 4–5 characterized by full-thickness tear with mechanical failure, which were excluded in this study. Other studies have confirmed these MRI severity grades, during intraoperative examinations [11, 21]. By so doing, they have recommended tailored surgical management and rehabilitation procedures.
Recently, Hilligsoe M et al. [26] have reviewed systematically US findings in GTPS and their prevalence. Thirteen studies were included. Four of these studies compared US with MRI, one retrospectively and three in prospective consecutive patients. Three of these studies found good agreement between both imaging modalities. Three other studies compared US with surgical findings in patients with GTPS and found good sensitivity and positive predictive value when detecting full thickness tears.
This present study adds new information to Grade 1–3 tendinopathy; it was undertaken in patients who failed conservative treatments and were candidates to percutaneous interventions. Chiefly, ultrasound examinations revealed the presence of calcium deposits (in 97% of patients) associated with hypoechoic areas and with the loss of fibrillar pattern. The presence of calcifications in GTPS has been described previously [29, 30]. These deposits had varied shapes; some of them are intratendinous with hiperechogenic arciform shape and others show nodular echogenicities. In addition, we also found calcium deposits in the tendon surface. According to Rosinsky et al. pertrochanteric calcifications are common radiographic findings in patients with GTPS [31]. In the surgical setting, the presence of intratendinous calcifications associated with tendon tears were reported in 10.5% of patients in a surgically treated cohort [31]. In eight out of 13 studies reviewed by Hilligsoe [26], calcifications were mentioned as a finding during ultrasound examinations, but the frequency of occurrence was not mentioned.
Just as reported in a recent study, we also found that tendinopathic changes are associated with a range of abnormalities in the peritrochanteric space that could be a source of pain, mainly trochanteric bursitis [20]. Ultrasound scans revealed trochanteric bursa distension only in 40.9% of patients and it was always associated with gluteal tendinopathy. Notably, in our study, multivariable statistics revealed that bursa distension was associated with pain. Interestingly, bursa distension implicated less pain. There are three bursae around the great trochanter and the trochanteric bursa is the largest of the three and associated with GTPS [31]. The bursa distension/swelling visualized by US corresponds to the swelling of the greater trochanteric bursa [32]. We think that bursal fluid can have a damping role, attenuating friction on movement, therefore reducing pain. In clear contradiction with these data, endoscopic bursectomy has been recommended in the operative management of low grade GTPS [21]. Additional research is mandatory to clarify these disparities regarding bursa pathology.
Matthews et al. systematically reviewed tendinopathy studies, which classified tendon matrix changes by means of ultrasound [4]. They recommended the inclusion of three parameters: tendon thickness, echogenicity and vascularity. Gluteal tendinopathy is better characterized by changes in echotexture, loss of fibrillar pattern, calcifications, enthesopathy and tendon tears [30, 32].
The ultrasound examination of gluteal tendinopathy in our study adds complexity to the current state of the art as we sought to discriminate tendon matrix changes in the lateral and superoposterior branches of the gluteus medius as well as in the gluteus minimus. Prior to the commencement of this study, we printed 3D models of the target anatomy (based on segmented MRI) in order to understand the complexity and overlapping anatomy of the gluteus medius and gluteus minimus attachments to bone and, eventually we established an ultrasound assessment protocol and template for systematic data collection.
Our data reveal that those patients with the lack of parallel-aligned fibers in the lateral branch of the gluteus medius reported worse functionality (Hip Outcome Score, HOS). The fibrillar disorganization could be attributed to the change from type I collagen to type III collagen due to a detriment of mechanical properties [33]. Interestingly, we found this relationship in the lateral but not in the superoposterior branch. The reason could be a biomechanical one. In fact, posterior fibers have an almost parallel alignment with the neck of the femur [2], thus, primarily function to stabilize or compress the hip joint. In addition to its stabilizing function, the superoposterior branch also assists in external rotation of the hip [34]. The gluteus maximus however is the strongest external rotator muscle of the hip, therefore degeneration of the posterior portion of the gluteus medius tendon would not largely impact external rotation strength of the hip, hence the results of the HOS seen. On the other hand, the anterior and middle fibers of the gluteus medius initiate hip abduction, which is then taken over by the tensor fascia lata. Accordingly, from a biomechanical point of view, the lateral branch of the gluteus medius and the gluteus minimus are the main contributors to physical function of hip abduction [35]. In accordance with other studies, patients with muscle atrophy reported worse functionality (lower HOS) [36, 37].
We found nodular thickening of fascia lata over the greater trochanter in 58% of patients. Notably, two patients clinically diagnosed as GTPS presented focal thickness at this point, as the sole abnormality originating trochanteric pain [38].
Based on ultrasound examinations, enthesophytes were present in 34% of patients. In more severe GTPS patients assessed intraoperatively, the presence of distally or proximally oriented enthesophytes, was associated with abductor tendon tears [3, 31].
This study has limitations. Although inter-radiologist agreement in gluteal tendinopathy items was substantial or almost perfect, we have not examined participants with normal gluteal tendons in this study. However, previous studies have concluded that MR and ultrasound imaging might be adequate to differentiate pathological versus normal gluteus medius tendons. Likewise, we have to clarify if these findings can guide personalized interventions in the peritrochanteric space. We cannot modify bony irregularities; however, we can manage consequent biomechanical abnormalities with physiotherapy while the nodular focal thickness of the tensor fascia lata, and/or the trochanteric bursa could be targeted with percutaneous interventions. Diagnostic variability from one radiologist to another is a major issue with ultrasound, especially when dealing with deep structures in overweight patients. The challenge is to reach an agreement concerning the features that support ultrasound structural diagnoses for gluteus medius and minimus tendinopathy. Although agreement between radiologists was strong, future studies are mandatory to confirm and optimize the scanning technique and diagnosis guidelines we have proposed. To enhance the quality of assessments, artificial intelligence and machine learning approaches could be adapted to this problem. Using ultrasound images and artificial intelligence based approaches, in supraspinatus tendon pathology, the diagnostic sensitivity and specificity for partial and full thickness tears has improved significantly [6].
Going forward, we need to determine if the response to a given therapeutic intervention is influenced by the different categories of pathology, considering both gluteal tendinopathy and pathology in the peritrochanteric space.
Conclusions
GTPS involves several ultrasound findings not only in gluteal tendons but also in adjacent fascial structures. Predominant findings were hypoechogenicity, loss of fibrillar pattern and tendon/peritendon calcifications in gluteus medius and minimus, above all in the lateral insertion of the gluteus medius. Predominant pathological findings in the peritrochanteric space were cortical irregularities and nodular thickness of fascia lata at the greater trochanter. Both degenerative calcifying gluteal tendinopathy and alterations in the peritrochanteric space associated with physical function or pain. Our results revealed that those patients with the lack of parallel-aligned fibers found in the lateral branch of gluteus medius reported worse functionality (HOS) as well as those with fatty infiltration in the gluteal muscles. The association of trochanteric bursa with pain needs further research, as it is relevant for treatment options.
Data availability
The data that support the findings of this study are available from the corresponding author, AI, upon reasonable request.
References
Long SS, Surrey DE, Nazarian LN (2013) Sonography of greater trochanteric pain syndrome and the rarity of primary bursitis. AJR Am J Roentgenol 201(5):1083–1086
Mallac C (2022) In Anatomy, diagnose & treat, hip injuries, improve, musculoskeletal injuries, power development. https://www.sportsinjurybulletin.com/the-gluteus-medius/#easy-footnote-2-6785. Accessed 26 Apr 2022
Mao LJ, Crudup JB, Quirk CR, Patrie JT, Nacey NC (2020) Impact of fluoroscopic injection location on immediate and delayed pain relief in patients with greater trochanteric pain syndrome. Skeletal Radiol 49(10):1547–1554
Matthews W, Ellis R, Furness J, Hing W (2018) Classification of tendon matrix change using ultrasound imaging: a systematic review and meta-analysis. Ultrasound Med Biol 44(10):2059–2080
McEvoy JR, Lee KS, Blankenbaker DG, del Rio AM, Keene JS (2013) Ultrasound-guided corticosteroid injections for treatment of greater trochanteric pain syndrome: greater trochanter bursa versus subgluteus medius bursa. AJR Am J Roentgenol 201(2):313–317
Pankhania M (2020) Artificial intelligence in musculoskeletal radiology: past, present and future. Indian J Musculoskelet Radiol 2(2):89–96
Park SM, Baek JH, Ko YB, Lee HJ, Park KJ, Ha YC (2014) Management of acute calcific tendinitis around the hip joint. Am J Sports Med 42(11):2659–2665
Pfirrmann CW, Notzli HP, Dora C, Hodler J, Zanetti M (2005) Abductor tendons and muscles assessed at MR imaging after total hip arthroplasty in asymptomatic and symptomatic patients. Radiology 235(3):969–976
Redmond JM, Chen AW, Domb BG (2016) Greater trochanteric pain syndrome. J Am Acad Orthop Surg 24(4):231–240
Tsutsumi M, Nimura A, Akita K (2019) The gluteus medius tendon and its insertion sites: an anatomical study with possible implications for gluteus medius tears. J Bone Joint Surg Am 101(2):177–184
Ladurner A, Fitzpatrick J, O’Donnell JM (2021) Treatment of gluteal tendinopathy: a systematic review and stage-adjusted treatment recommendation. Orthop J Sports Med 9(7):23259671211016850
Albers IS, Zwerver J, Diercks RL, Dekker JH, Van den Akker-Scheek I (2016) Incidence and prevalence of lower extremity tendinopathy in a Dutch general practice population: a cross sectional study. BMC Musculoskelet Disord 17(1):16. https://doi.org/10.1186/s12891-016-0885-2
Barratt PA, Brookes N, Newson A (2017) Conservative treatments for greater trochanteric pain syndrome: a systematic review. Br J Sports Med 51(2):97–104
Heaver C, Pinches M, Kuiper JH et al (2021) Greater trochanteric pain syndrome: focused shockwave therapy versus an ultrasound guided injection: a randomised control trial. Hip Int 33(3):490–499
Torres A, Fernández-Fairen M, Sueiro-Fernández J (2018) Greater trochanteric pain syndrome and gluteus medius and minimus tendinosis: nonsurgical treatment. Pain Manag 8(1):45–55
Jorgensen JE, Fearon AM, Mølgaard CM, Kristinsson J, Andreasen J (2020) Translation, validation and test-retest reliability of the VISA-G patient-reported outcome tool into Danish (VISA-G.DK). PeerJ 8:e8724
Ebert JR, Retheesh T, Mutreja R, Janes GC (2016) The clinical, functional and biomechanical presentation of patients with symptomatic hip abductor tendon tears. Int J Sports Phys Ther 11(5):725
Speers CJ, Bhogal GS (2017) Greater trochanteric pain syndrome: a review of diagnosis and management in general practice. Br J Gen Pract 67(663):479–480
Ganderton C, Semciw A, Cook J, Pizzari T (2017) Demystifying the clinical diagnosis of greater trochanteric pain syndrome in women. J Womens Health (Larchmt) 26(6):633–643
Lall AC, Schwarzman GR, Battaglia BA, Chen SL, Maldonado DR, Domb BG (2019) Greater trochanteric pain syndrome: an intraoperative endoscopic classification system with pearls to surgical techniques and rehabilitation protocols. Arthrosc Tech 8:e889–e903
Tso CKN, O’Sullivan R, Khan H, Fitzpatrick J (2021) Reliability of a novel scoring system for mri assessment of severity in gluteal tendinopathy: the melbourne hip MRI score. Orthop J Sports Med 9(4):2325967121998389
Annin S, Lall AC, Meghpara MB et al (2021) Intraoperative classification system yields favorable outcomes for patients treated surgically for greater trochanteric pain syndrome. Arthroscopy 37(7):2123–2136
Fearon AM, Scarvell JM, Cook JL, Smith PN (2010) Does ultrasound correlate with surgical or histologic findings in greater trochanteric pain syndrome? A pilot study. Clin Orthop Relat Res 468(7):1838–1844
Woodley SJ, Nicholson HD, Livingstone V, Doyle TC, Meikle GR, Macintosh JE, Mercer SR (2008) Lateral hip pain: findings from magnetic resonance imaging and clinical examination. J Orthop Sports Phys Ther 38(6):313–328
Blankenbaker DG, Ullrick SR, Davis KW, De Smet AA, Haaland B, Fine JP (2008) Correlation of MRI findings with clinical findings of trochanteric pain syndrome. Skeletal Radiol 37(10):903–909
Hilligsøe M, Rathleff MS, Olesen JL (2020) Ultrasound definitions and findings in greater trochanteric pain syndrome: a systematic review. Ultrasound Med Biol 46(7):1584–1598
Draghi F, Cocco G, Lomoro P, Bortolotto C, Schiavone C (2020) Non-rotator cuff calcific tendinopathy: ultrasonographic diagnosis and treatment. J Ultrasound 23(3):301–315
Hoffman DF, Smith J (2017) Sonoanatomy and pathology of the posterior band of the gluteus medius tendon. J Ultrasound Med 36(2):389–399
Vereecke E, Mermuys K, Casselman J (2015) A case of bilateral acute calcific tendinitis of the gluteus medius, treated by ultrasound-guided needle lavage and corticosteroid injection. J Belg Soc Radiol 99(2):16–19
Bianchi S, Becciolini M (2019) Ultrasound appearance of the migration of tendon calcifications. J Ultrasound Med 38(9):2493–2506
Ivanoski S, Nikodinovska VV (2019) Sonographic assessment of the anatomy and common pathologies of clinically important bursae. J Ultrason 19(78):212–221
Rosinsky PJ, Yelton MJ, Ankem HK et al (2021) Pertrochanteric calcifications in patients with greater trochanteric pain syndrome: description, prevalence, and correlation with intraoperatively diagnosed hip abductor tendon injuries. Am J Sports Med 49(7):1759–1768
Labrosse JM, Cardinal E, Leduc BE et al (2010) Effectiveness of ultrasound-guided corticosteroid injection for the treatment of gluteus medius tendinopathy. AJR Am J Roentgenol 194(1):202–206
Ruta S, Quiroz C, Marin J et al (2015) Ultrasound evaluation of the greater trochanter pain syndrome: bursitis or tendinopathy? J Clin Rheumatol 21(2):99–101
Leiphart RJ, Pham H, Harvey T et al (2021) Coordinate roles for collagen VI and biglycan in regulating tendon collagen fibril structure and function. Matrix Biol Plus 13:100099
Looney AM, Bodendorfer BM, Donaldson ST, Browning RB, Chahla JA, Nho SJ (2022) Influence of fatty infiltration on hip abductor repair outcomes: a systematic review and meta-analysis. Am J Sports Med 50(9):2568–2580
Cowan RM, Semciw AI, Pizzari T et al (2020) Muscle size and quality of the gluteal muscles and tensor fasciae latae in women with greater trochanteric pain syndrome. Clin Anat 33(7):1082–1090
Long S, Leahy H, Bush C, Surrey D, Nazarian L (2020) Anterolateral hip pain: Sonographic evaluation of the proximal iliotibial band and tensor fascia lata. J Clin Ultrasound 48(4):193–197
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: LA, JIM, NM and IA. Patient recruitment, clinical diagnoses and demographic and clinical data acquisition: NM and MR-P. Methodology, scanning technique, radiologists’ consensus of US template to standardize data acquisition: LA, GI, JIM, and JM. Tridimensional MRI, segmentation and 3D printing model for gluteal tendons anatomy: GI. Scores and images assessment: AA. US diagnoses, image acquisition and intraobserver reliability: LA and GI. Electronic data collection logbook, data curing and statistical analyses: PB. Writing original draft: IA, AA, LA and NM. Writing, review and editing: LA, PB and IA.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the local Ethics Committee of Euskadi (2019028).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the ultrasound images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Atilano, L., Martin, N., Iglesias, G. et al. Sonographic pathoanatomy of greater trochanteric pain syndrome. J Ultrasound 27, 501–510 (2024). https://doi.org/10.1007/s40477-023-00836-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-023-00836-x