Abstract
Background
For solid pancreatic masses, ultrasound endoscopic fine-needle biopsy is suggested as the front-line investigation for tissue achievement, notwithstanding the optimal performance of transabdominal ultrasound (TUS)-guided biopsy.
Purpose
To reassess the efficacy and effectiveness of TUS-guided sampling and to determine the factors predictive of accurate histology.
Methods
In total, 142 patients with an indication for a TUS-guided biopsy of a pancreatic mass were analyzed. A single pass of an 18-gauge Biomol needle was carried out by the Menghini technique. The accuracy, sensitivity, and specificity of the procedure in terms of correctly diagnosing an inflammatory or neoplastic lesion were determined. The patients’ characteristics, the size and location of the mass, and the sonographers’ experience in performing TUS were recorded.
Results
The sampling was unsuccessful in 24 cases, owing to the deep localization of lesions (57%), bloating (33%), or low patient compliance (10%). The accuracy, sensitivity, and specificity of the 118 successful biopsies were 81%, 79%, and 100%, respectively. A biopsy core was obtained in 90 of the 118 patients (76%) in whom the procedure was attempted. In the multivariate analysis, lesion size (≤ 20 mm vs. > 20 mm) (OR = 5.3 [1.7–17.0]) and operator experience (OR = 4.4 [1.6–12.1]) predicted the acquisition of adequate samples. With an expert sonographer, the accuracy, sensitivity, and specificity were 87%, 85%, and 100%, respectively. Two adverse events were registered: mild abdominal pain and a hypotensive crisis.
Conclusions
The present investigation highlights the optimal performance of a TUS-guided biopsy of a pancreatic mass. Because of its simplicity and safety, the procedure needs to be included among the recommended investigative options
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
For primary or metastatic, benign or malignant lesions arising from the exocrine or endocrine pancreas, tissue collection from a pancreatic mass is deemed necessary for establishing a definitive pathological diagnosis. Endoscopic ultrasound-guided fine-needle aspiration or biopsy (EUS-FNA or EUS-FNB) from target lesions is the current investigative approach endorsed by national and international authorities [1, 2]. For a pathological diagnosis of pancreatic ductal adenocarcinoma (PDAC), the procedure has been granted a sensitivity of 64% to 95%, a specificity of 75% to 100%, and a diagnostic accuracy of 78% to 95% [3]. EUS is a technically demanding and expensive procedure [1], which has hampered its widespread use in many institutions. The diagnostic accuracy of EUS-FNA, however, strongly depends on the rapid on-site evaluation (ROSE) of the retrieved specimen by an experienced cytologist [4]. Nevertheless, ROSE is unavailable in many centers owing to costs, physicians’ availability, and expertise. Finally, EUS-FNA is capable of retrieving only small amounts of tissue, which allows a cytological, but not a histological, examination [5].
In recent years, new data on transabdominal ultrasound (TUS)-guided biopsy of pancreatic neoplasms have been produced: After pooling data from 13 surveys, a diagnostic accuracy ranging from 91 to 100% has been registered [6]. Owing to the wide availability, safety, and lower cost of a TUS-guided pancreatic puncture, this option should be considered in the guidelines issued on this topic [2], which still suggest EUS-FNA as the only initial option to adopt. Nevertheless, a single randomized clinical trial on 84 patients that compared sampling with EUS versus computed tomography or TUS reported a higher, although not significant, diagnostic accuracy of the former approach [7]. Five other studies reported that these approaches were equally accurate [8,9,10,11,12]. Because of the growing need to characterize neoplasms (i.e., epithelial, neuroendocrine or stromal cell tumors, and lymphomas) by immunostaining and/or molecular profiling to tailor appropriate clinical and oncological counseling, obtaining a tissue core represents the new standard requirement [5, 13]. Also, histological samples with preserved tissue architecture and morphology are easier to interpret for general pathologists than cytological smears [14].
Finally, most of the previous studies on this topic are methodologically biased as they assess only the efficacy of EUS- or TUS-guided tissue acquisition but not its effectiveness. Indeed, data on sensitivity and specificity are commonly provided in pathological diagnoses when a bioptic attempt is technically successful (efficacy); however, these data are not reported when a clinically indicated biopsy cannot be performed for limitations inherent to the two procedures: that is, interference of bowel gas for TUS and altered upper gastrointestinal tract anatomy for EUS (effectiveness).
The primary aim of this study was to reassess the efficacy and effectiveness of pancreatic tissue sampling by TUS in patients with a pancreatic mass. In addition, the attempts to retrieve a pancreatic tissue core will also be evaluated, and predictors of inadequate pancreatic sampling will be searched for.
Patients and methods
Methods
Study design
This prospective, single-arm, single-center study was approved by the Ethics Committee of IRCCS Casa Sollievo della Sofferenza and received no financial support from any companies.
Patient selection
Consecutive patients with an indication for TUS-guided tissue acquisition of a solid pancreatic lesion were prospectively enrolled. Inclusion criteria were age ≥ 18 years, virgin target lesions, eligibility for surgical resection or locally advanced/metastatic disease, and signed informed consent by the patient. In addition to pregnant women, patients with an expected survival time of < 2 months, abnormal coagulation parameters, or a cystic component of the mass under evaluation were excluded. When a pancreatic neoplasm that was initially detected at a computed tomography or magnetic resonance scan could not be visualized at the time of TUS-guided biopsy planning, the patient was not excluded from the study but was retained in the computation of the effectiveness of the procedure.
US procedure and tissue acquisition
Three sonographers with a life-time performance of > 2000 US abdominal examinations were involved in this study. Each of them had personally performed > 300 fine-needle punctures of abdominal organs (specifically of the liver); however, their personal experience with TUS-guided sampling of the pancreas was variable. In particular, one of them had previously punctured > 100 pancreatic neoplasms and was considered an experienced dedicated operator, while the other two were beginners with < 10 pancreatic biopsies carried out before the study was initiated.
To localize the target lesion accurately, US was performed using the Toshiba Xario 660. In a few cases, also a contrast-enhanced examination with i.v. SonoVue (Bracco International B.V.) injection was used. Characteristics of the lesion, such as its size and location, were registered before sampling. When an optimal insertion track could not be visualized, reasons for the failure were recorded. For the interventional procedure, a tandem-needle technique with a probe with lateral support was used, and the insertion point was the left upper quadrant, left of the midline. A modified Menghini, 18-gauge, Biomol needle was employed for all samplings, with a single pass for each target lesion.
Adverse events
After the TUS biopsy, patients returned to the hospital ward and were checked for the development of complications for the following 24 h. Adverse events were defined according to the classification of Eloubeidi et al. [15].
Pathological evaluation
The retrieved material was fixed in 10% buffered formalin and embedded in paraffin; 3-µm tissue sections were cut and stained with hematoxylin and eosin for morphological evaluation. The pathologists defined a “tissue core” as being all samples with architecturally intact histology and measuring at least 550 µm in the major axis, corresponding approximately to the diameter of a high-power microscopic field. Microfragments (< 550 µm), but not a tissue core, were considered sufficient for histological interpretation [16].
Outcome measures
The primary end point was the evaluation of the efficacy of TUS-guided sampling for a definite pathology diagnosis of the mass lesion. In addition, the ability of the method to retrieve a tissue core was also taken into account. The secondary outcome was the evaluation of the effectiveness of TUS-guided biopsy. Final diagnoses were made based on positive pathological results of the TUS-assisted samples; for patients with a negative and/or inadequate TUS sampling, the final diagnosis was made based on congruent imaging and the follow-up after 24 months.
Statistics
The histological diagnosis of target lesions and follow-up data were used to calculate the sensitivity, specificity, and positive and negative predictive values both for the total population of patients for whom the sampling was indicated (the effectiveness population) and for the subset of patients in whom the biopsy was eventually performed (the efficacy population). Finally, patients’ demographics, features of target lesions, and the operator’s experience were entered in a multivariate analysis to identify factors that are more frequently associated with a definite diagnosis. Statistical analyses were carried out with SPSS software version 13.0 for Windows (SPSS Inc, Chicago, IL), and variables with a p-value < 0.05 were considered significant. Continuous variables are presented as mean and standard deviation. Categorical data were compared using Pearson’s chi-square test or Fisher’s exact test.
Results
A total of 142 patients with a mass-forming pancreatic lesion were prospectively enrolled. Pancreatic lesions were previously diagnosed by using computed tomography and/or magnetic resonance, and all patients were naïve to a previous bioptic attempt. At the initial clinical and instrumental workup, a suspicion of pancreatic malignancies, whether a cancer or a neuroendocrine tumor, was the main indication for biopsy, with inflammatory masses suspected in a minority of cases. The main demographic and clinical characteristics of the patients are shown in Table 1, both for the total population of patients for whom the TUS-guided biopsy was clinically indicated (the effectiveness population) and for the subset of patients in whom the sampling was eventually performed (the efficacy population). Of the latter group of patients, 55 were female, and 63 were male. After subgrouping the patients by age, 47% were older than 70 years, 45% were between 50 and 70 years, and 8% were younger than 50 years. The average BMI was 24, with a range from 15 to 41. The pancreatic mass was located in the head (64% of cases), the uncinate process (15%), the body (15%), and the tail (8%). As to mass size, 85% of the lesions were large (> 20 mm in diameter), and 15% were small (≤ 20 mm in diameter). The average size of the histological samples was 0.75 ± 0.66 cm, most of them (58%) between 0.6 and 1.5 cm; of the remaining lesions, 32 had a size > 1.5 cm, and 8 a size < 0.5 cm.
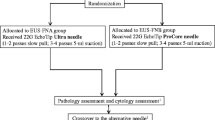
Of the 142 patients, the TUS-guided sampling was technically unsuccessful in 24 cases (16.9%), for the following reasons: deep location within the abdomen (14 cases), bloating (8 cases), and low patient compliance (2 cases). The disposition of the remaining 118 patients in whom the TUS-guided tissue acquisition was successful is shown in Fig. 1. A final diagnosis (whether neoplastic or inflammatory) was achieved with histology in 95 cases (80.5%): 84 patients had a neoplastic lesion (78 pancreatic adenocarcinoma, 4 neuroendocrine tumors, and 2 metastases), and 11 patients had mass-forming chronic pancreatitis. Histology was either negative or inadequate in the remaining 23 patients and, according to the study protocol, the procedure was not repeated. The final diagnosis of these 23 patients (22 PADC and 1 metastasis) could be established by clinical course and follow-up imaging. Diagnostic accuracy, sensitivity, and specificity among the 118 patients were 81%, 79%, and 100%, respectively. The TUS-guided sampling of the pancreatic mass provided a biopsy core, defined as a sampled specimen > 0.5 cm, in 90 of the 118 patients (76%).
Univariate associations with a successful diagnostic procedure are summarized in Table 2. The sonographer’s expertise (p = 0.004) and lesion size (p = 0.008) were significantly associated with a diagnostic sampling. The previous features retained their predictive power in the multivariate analysis: the odds ratio (OR) = 4.4 (1.6–12.1) for operator’s experience, and OR = 5.3 (1.7–17.0) for lesion size. When the biopsy was attempted by an expert sonographer, the accuracy, sensitivity, and specificity were 87%, 85%, and 100%, respectively, when lesions were counted independently of their size.
The procedure was well tolerated by most patients. The incidence of minor complications was 1.6% (2/118): a case of mild abdominal pain requiring analgesics and a case of hypotensive crisis. There were no deaths or major complications. No seeding was documented either in patients who received surgery or in those with inoperable lesions at a follow-up observation after at least 24 months.
Discussion
When a pancreatic lesion is detected at the initial imaging, it remains relevant to achieve a definite diagnosis, whether an adenocarcinoma or rare mass-forming neoplasms, by a direct puncture of the target lesion. The historical precaution of not sampling the pancreas because of the hypothetical fear of inducing acute pancreatitis did not stand the test of time, as the procedure has been proved efficacious and safe [17].
Sampling of pancreatic tissue can be performed via either EUS or TUS. Historically, the initial approach was TUS, but innovations in technical instrumentation have indicated EUS as the preferred investigative tool [18]. An explanation may lie in the closer proximity of the suction needle to the pancreas via EUS, which should theoretically guarantee safer and more precise sampling of target lesions. A thorough review of the literature reveals a diagnostic accuracy of over 90% for both the EUS and the TUS approach, as well as a similar safety profile [3, 6, 19, 20]. Findings in our group of patients with pancreatic mass-forming lesions collected in a single center over 3 years are comparable with previous figures. These findings may contribute to corroborating the value of TUS, with a diagnostic accuracy of up to 87% when the examination was carried out by an experienced sonographer. It is worth mentioning that neither the patients’ characteristics nor the location of the pancreatic mass positively influenced obtaining a definite histological diagnosis.
The current indication for pancreatic tissue acquisition is not only to ascertain the nature of a pancreatic neoplasm, whether benign or malignant, but also to retrieve larger samples with preserved histological architecture, which would allow further characterization of the genetic alterations that underlie tumorigenesis in the pancreas [13, 21, 22]. This goal is difficult to achieve with EUS-FNA because, with this method, sampled tissues allow only cytological evaluation [23]. New technological devices have been developed with the intent to obtain adequate tissue samples for immunohistochemical and biomolecular characterizations. In a recent, observational, multicenter, prospective study by Di Leo et al., the diagnostic accuracy of the newly designed fork-tip needle amounted to 93%, but a tissue core was retrieved in only 67% of patients [24]. An important finding of the current study is that TUS-guided sampling of the pancreatic mass provided a biopsy core in 90 of the 118 patients (76%) in whom the procedure was attempted. These encouraging results should prompt a reappreciation of the TUS-guided approach. In all the recently published consensus reports, EUS-guided FNA or FNB is recommended as the first-line procedure when a pathological diagnosis is required [2, 25,26,27], whereas percutaneous sampling is either not even mentioned or considered only in metastatic disease. Unfortunately, these authoritative statements dismiss experimental data showing that EUS and TUS sampling of pancreatic tissue have an equal diagnostic accuracy [17, 28]. Consonant with these data, both EUS and TUS should be advocated in the initial investigation of a pancreatic mass, the choice between the two being dictated by local expertise and availability. However, in the current medical environment, costs weigh heavily on clinical decision-making. Based on this premise, TUS-assisted biopsy merits endorsement as the first-line investigation for patients with a pancreatic mass, as it does not require the assistance of an anesthesiologist for deep sedation and is not so technically demanding as EUS. In addition, the contemporary presence of an on-site pathologist to assess the adequacy of the retrieved specimen is no longer necessary, as we established that a tissue core is sampled in the vast majority of TUS-guided bioptic attempts. Finally, as a single pass of the needle into the pancreatic lesion allowed us to retrieve an adequate tissue core, the known rate of post-procedural complications, such as inflammation, hemorrhage, and seeding of tumor cells, should be lower than when multiple passes are required.
A novel result of the current study is the evaluation of the effectiveness of sampling a pancreatic lesion under TUS guidance. The available literature on pancreatic tissue sampling reports a high sensitivity, specificity, and diagnostic accuracy, whether the procedure is carried out with EUS [18] or TUS [6]. However, the performance (efficacy) of an intervention is commonly evaluated under ideal and strictly controlled circumstances, whereas the effectiveness evaluates its performance under routine clinical practice. From a clinical standpoint, it is more useful to establish in how many patients with a pancreatic biopsy indication the intended procedure (whether EUS-FNA, EUS-FNB, or TUS-guided biopsy) is eventually carried out. Different conditions may have an impact on the diagnosis of the required procedure. Indeed, abundant abdominal fat deposition or intestinal gas content could mask the visualization of the pancreas at TUS scanning, whereas luminal stenosis or surgically altered anatomy could preclude an optimal positioning of the EUS probe. It is, therefore, not surprising that the effectiveness of TUS-guided pancreatic biopsy has a lower diagnostic accuracy than efficacy. Of the 142 patients with an indication for a biopsy of the pancreatic mass (the effectiveness population), a TUS-guided biopsy was possible in only 118 patients (the efficacy population) because of several anatomic conditions precluding a safe biopsy. Of the 23 patients in whom the sampling could not be done, the success rate did not differ between expert and non-expert sonographers.
A final merit of TUS-guided pancreatic biopsy is the possibility of retrieving a core (> 0.5 cm) sample, which has been achieved in 91% of our patients. The field of pancreatic tissue acquisition is rapidly moving from cytology to histology [5]. Recently, the precision medicine approach in pancreatic cancer allows histological subtypes of pancreatic cancers to be determined, which may be extremely useful clinically and could facilitate the optimization of existing therapies.
In conclusion, a tissue core biopsy from a pancreatic lesion can be accomplished via EUS-FNB or under TUS guidance; these two procedures should be considered complementary and not contradictory. In the present study, the diagnostic performance and safety of the TUS approach are similar to the performance and safety reported in the literature for the EUS-FNB approach, with the former approach being less demanding and costly. We suggest that an ideal protocol for the evaluation of a pancreatic mass should first consider tissue biopsy under TUS guidance and reserve the more sophisticated EUS option for cases with suboptimal US localization of the lesion or with an inconclusive diagnosis.
References
Polkowski M, Jenssen C, Kaye P et al (2017) Technical aspects of endoscopic ultrasound (EUS)-guided sampling in gastroenterology. European Society for Gastrointestinal Endoscopy (ESGE) Technical Guideline – March 2017. Endoscopy 49:989–1006
Tempero MA, Malafa MP, Al-Hawary M et al (2017) Pancreatic Adenocarcinoma, Version 2.2017. Clinical Practice Guidelines in oncology. J Natl Compr Canc Netw 15:1028–1061
Hewitt MJ, McPhail MJ, Possamai L et al (2012) EUS-guided FNA for diagnosis of solid pancreatic neoplasms: a meta-analysis. GastrointestEndosc 75:319–331
Erickson RA, Sayage-Rabie L, Beissner RS et al (2000) Factors predicting the number of EUS-guided fine-needle passes for diagnosis of pancreatic malignancies. GastrointestEndosc 51:184–190
Rimbas M, Crino Sf, Gasbarrini A et al (2018) EUS-guided fine-needle tissue acquisition for solid pancreatic lesions: finally moving from fine-needle aspiration to fine-needle biopsy. Endosc Ultrasound 7:137–40
Huang Y, Hi J, Chen YY et al (2018) Ultrasound-guided percutaneous core needle biopsy for the diagnosis of pancreatic disease. Ultrasound Med Biol 44:1145–1154
Horwhat KD, Paulson EK, McGrath K et al (2006) A randomized comparison of EUS-guided FNA versus CT or US-guided FNA for the evaluation of pancreatic mass lesions. GastrointestEndosc 63:966–975
Volmar KE, Vollmer RT, Jowell PS et al (2005) Pancreatic FNA in 1000 cases: a comparison of imaging modalities. GastrointestEndosc 61:854–861
Erturk SM, Mortelé KJ, Tuncall K et al (2006) Fine-needle aspiration biopsy of solid pancreatic masses: comparison of CT and endoscopic sonographic guidance. Am J Roentgenol 187:1531–1535
Mallery JS, Centeno BA, Hahn PF et al (2002) Pancreatic tissue sampling guided by EUS, CT/US, and surgery: a comparison of sensitivity and specificity. GastrointestEndosc 56:218–224
Matsuyama M, Ishii H, Kuraoka K et al (2013) Ultrasound-guided vs endoscopic ultrasound-guided fine-needle aspiration for pancreatic cancer diagnosis. World J Gastroenterol 19:2368–2373
Okasha H, El-Kassas M, El-Gemele E et al (2013) Endoscopic ultrasound-guided fine-needle aspiration versus percutaneous ultrasound-guided fine needle aspiration in diagnosis of focal pancreatic masses. Endosc Ultrasound 2:190–193
Rajid NU, Peng XL, Jin C et al (2020) Purity independent subtyping of tumors (PurIST), a clinically robust, ingle-sample classifier for tumor subtyping in pancreatic cancer. Clin Cancer Res 26(1):82–92
Jhala NC, Jhala DN, Chieng DC et al (2003) Endoscopic ultrasound-guided fine needle aspiration. A cytopathologist’s perspective. Am J Clin Pathol 120:351–367
Eloubeidi MA, Gress FG, Savides TJ et al (2004) Acute pancreatitis after EUS-guided of solid pancreatic masses: a pooled analysis from EUS centers in the United States. GastrointestEndosc 60:385–389
Roberto DM, Rimbaş M, Attili F et al (2018) Performance of a new needle for endoscopic ultrasound-guided fine-needle biopsy in patients with pancreatic solid lesions: a retrospective multicenter study. Endosc Ultrasound 7:329–334
Yang RY, Ng D, Jaskoiska JD et al (2015) Evaluation of percutaneous ultrasound-guided biopsies of solid mass lesions of the pancreas: a center’s 10-year experience. Clin Imaging 19:62–65
Dumonceau JM, Deprez PH, Jenssen C et al (2017) Indications, results, and clinical impact of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline - Updated January 2017. Endoscopy 49:695–714
Puli SR, Bechtold ML, Buxbaum JL et al (2013) How good is endoscopic ultrasound fine-needle aspiration in diagnosing the correct etiology for a solid pancreatic mass? A meta-analysis and systematic review. Pancreas 42:20–26
Hebert-Magee S, Bae S, Varadarajulu S et al (2003) The presence of a cytopathologist increases the diagnostic accuracy of endoscopic ultrasound-guided fine needle aspiration cytology for pancreatic adenocarcinoma: a meta-analysis. Cytopathology 24:159–171
Waddell N, Pajic M, Patch AM et al (2015) Whole genomes redefine the mutational landscape of pancreatic cancer. Nature 518:495–501
Bailey P, Chang DK, Nones K et al (2016) Genomic analyses identify molecular subtypes of pancreatic cancer. Nature 531:47–52
Sjoquist KM, Chin VT, Chantrill LA et al (2014) Personalizing pancreas cancer treatment: when tissue is the issue. World J Gastroenterol 20:7849–7863
Di Leo M, Crinò SF, Bernardoni L et al (2019) EUS-guided core biopsies of pancreatic solid masses using a new fork-tip needle: a multicenter prospective study. Dig Liver Dis 51:1275–1280
Martin-Richard M, Ginès A, Ayuso JR et al (2016) Comité multidisciplinar para la actualización de las recomendaciones para el manejo de las lesiones pre-malignas y el adenocarcinoma de páncreas. [Recommendations for the diagnosis, staging and treatment of pre-malignant lesions and pancreatic adenocarcinoma]. Med Clin (Barc) 147:465.e1–465
Cascinu S, Falconi M, Valentini V et al (2010) ESMO Guidelines Working Group. Pancreatic cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 21 (Suppl 5):v55–8
Sidhu PS, Brabrand K, Cantisani V et al (2015) EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part II. Diagnostic Ultrasound-Guided Interventional Procedures. Ultraschall in Med 36:E15–E35
Yang JY, Hebert-Magee S, Trevino J et al (2012) Randomized trial comparing the 22-gauge aspiration and 22-gauge biopsy needles for EUS-guided sampling of solid pancreatic mass lesion. GastrointestEndosc 76:321–327
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Contributions
FT, IA, B: performed ultrasound; SK, AA, MA: collected datas; PP, GP: histological analysis; MRV: statistical analysis; AA: writer.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical statement and informed consent
All subjects gave written informed consent to the treatment of personal data in anonymous form and in accordance with the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Terracciano, F., Marra, A., Ippolito, A.M. et al. Transabdominal ultrasound-guided pancreatic biopsy: a neglected but safe, effective and inexpensive procedure that needs to be re-juvinalized. J Ultrasound 24, 175–182 (2021). https://doi.org/10.1007/s40477-020-00542-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-020-00542-y