Abstract
There is an increasing incidence of cesarean scar defect. This article will discuss and show different and variable sonographic presentations of scar niches and uterine postpartum ultrasonography with vaginal birth after cesarean section that can be confusing and many should be unaware of. This brief review aims to help practitioners to avoid confusion and be aware and acquainted with the different sonographic findings encountered in practice related to cesarean scar. It can lead to uterine rupture I labour, dehiscence in pregnancy and placenta accreta in the future pregnancy, but this is not evidence-based and not even a contraindication for pregnancy. It is neither an indication of repair for the presenting patient nor an indication to screen these patients for such complications. It is treated if associated with infertility or bleeding and not in asymptomatic ones.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
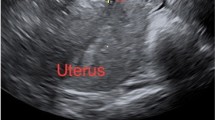
Cesarean section (CS) niche describes the presence of a hypoechoic area within the myometrium in the isthmus, with the discontinuation of the myometrium at the site of a previous CS. Uterine scar defects or scar niches are relatively common after cesarean delivery. Uterine scar imaging with ultrasound and hysterosonography has gained popularity in the last decade. This article aims to present different pictures of scar niches and post-VBAC findings that can be confusing [1, 2].
Cesarean section cases have increased in the recent years. The presence of a niche in the cesarean scar in the uterus has also increased. It can lead to uterine rupture in labour, dehiscence in pregnancy and placenta accreta in the future pregnancy, but this is not evidence-based and not even a contraindication for pregnancy. It is neither an indication of repair for the presenting patient nor an indication to screen these patients for such complications. In transvaginal ultrasound (TVS), the prevalence of niche varies between 42 and 70% in women with one or more previous cesarean sections. Alternative terms, such as cesarean scar defect, deficient cesarean scar, scar diverticulum, scar pouch, and isthmocele, were reported. There was no gold standard for the detection and measurement of a niche, but recently, a consensus among niche experts was achieved regarding ultrasonographic niche evaluation and it will be discussed below [1].
Scar niche
A niche is defined as a triangular anechoic space (with or without fluid) at least 2 mm deep at the presumed site of the cesarean section scar. This should not be confused with the cesarean section scar itself that appears as an echogenic line at the presumed site or similar echogenicity of the surrounding myometrium, and it is not hypoechoic unless pathological. Postmenstrual bleeding is the commonest complaint because of the retention of menstrual blood in the niche, which is intermittently expelled after the majority of the menstruation has passed. This may be related to the poor contractility of the uterine muscle around the scar and the presence of fibrotic tissue below the niche, which impair the drainage of menstrual flow. Postmenstrual bleeding is also because of the newly formed fragile vessels in the niche. This represents a rationale of the hysteroscopic resection aiming not only to facilitate the drainage of menstrual blood, but also to coagulate the niche vessels and to reduce blood production in situ. Postmenstrual spotting is defined as more than 2 days of brownish discharge at the end of menstruation (including spotting) with a total length of more than 7 days or as an intermenstrual bleeding, which starts within 5 days after the end of menstruation for 2 or more days. It is more prevalent in women with a residual myometrial thickness of less than 50% [2]. Scar ectopic pregnancy may develop in a niche.
Regarding assessment by ultrasound, the endometrium should be ignored, as measurements are based only on the myometrium. In case of niches with one or more branches, the thinnest remaining residual myometrium (RMT) is used. Transverse plane is used only for the third dimension of the niche (width), not for depth or RMT. The best method is by starting in the midsagittal plane, with good visualization of the cervical canal, then moving the transvaginal probe laterally to both sides. To visualize the niche in the transverse plane, the best method is to start in the sagittal plane, keeping the visualization of the niche while rotating the probe from the sagittal to the transverse plane. The best method to detect possible branches is in the transverse plane and screening the entire lower uterine segment from cervix to corpus. To measure the uterine niche, there should be a visualization of only the lower uterine segment in all uterine positions. The use of Doppler imaging is not mandatory, but can be useful to differentiate between uterine niche and hematomas, adenomyomas, and fibrotic tissue. Contrast sonography has added value. There is no preference for either gel or saline or the type of catheter used. The best location of the catheter used is just in front of the niche (caudal to its most distal part) or, if possible, cranial to its most proximal part, at start of gel/saline contrast infusion, and then, the catheter is pulled slowly backwards towards the base of the niche. While performing ultrasound following saline infusion, the catheter can be left in front of the niche. However, while performing ultrasound following gel infusion, there is no preference whether to remove catheter or leave it in front of the niche. In case of intrauterine fluid accumulation, gel or saline infusion is not of value [1].
The depth of the niche (the vertical distance between the base and the apex of the defect) and residual myometrium (from the echogenic serosal surface of the uterus to the hypoechoic apex of the niche) can be measured, and the niche shape should be reported. In patients with multiple niches, the largest is measured. The niche shape could be semicircle, triangle, droplet, inclusion cyst(s), circular, rectangular, or others as shown below. These sonographic findings cannot be diagnosed easily by inexperienced trained eyes and may be confusing or missed, so the different pictures shown below aim to provide simple recognition of them.
Postpartum ultrasound after VBAC is not routinely indicated unless there is active bleeding. A normal appearance after VBAC on ultrasound could be a thinned hypoechoic scar in an area with a small rim of fluid in the uterovesical pouch. This can be observed in case of incidental ultrasound findings after delivery, and it does not mandate an extra management other than the routine care (Figs. 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11).
LUS by TVUS after VBAC, a thin rim of fluid in uterovesical pouch and a hypoechoic scar site of cribriform shape of infiltrating blood by stretch of scar in labor and retraction of the LUS that appears as a dehiscent scar, for follow-up as long as no vaginal bleeding or deterioration in general condition. No role of vaginal scar examination or ultrasound in the absence of suspicious vaginal bleeding or clinical findings. A dehiscence after delivery with no clinical findings on ultrasound or examination of 1cm or a finger width can be managed conservatively
Low echogenicity at CS scar site, which is different from, surrounding the myometrium. It is related to fluid retention. (Hematoma niche with myometrial discontinuation affecting full thickness of myometrium with fibrosed retracted ends in the second photo and the first photo (hypoechoic) should be differentiated from Adenomyosis by Doppler signal)
Echogenic appearance of the uterine scar at the usual site of the section with nearly same thickness related to the upper and lower segment. We can claim that this scar characters can sustain labour pains with minimal dehiscence in opposite to others seen before which are thinner and nearly absent in some cases where dehiscence can occur even in pregnancy. A dehiscence especially of more than 50% of the thickness of the uterine wall can lead to silent dehiscence in pregnancy
It was reported that a wedge defect in scar niche was present in 21%, inward protrusion (internal surface of the scar bulging toward the uterine cavity) in 6%, outward protrusion (external surface bulging toward the bladder or abdominal cavity) in 15%, hematoma in 4%, and inward retraction (external surface of the scar dimpled toward the myometrial layer) in 4%. When a niche penetrates to a depth of at least 50% of the myometrium or the remaining myometrial thickness is ≤ 2.2 mm on TVS, it is considered as a large niche. Hysterosalpingogram can show contrast extension into defect in the myometrium with the ballooning of the lower uterine segment (LUS) [3]. Hysteroscopy can show a dome, bulging pouch, or wedge on the anterior aspect of the lower uterine wall or cervical canal.
The risk factors proposed for niches are the number of C-sections, uterine positions (retroversion provides more risk), surgical techniques of closure (one-layer closure), and labor before section. It is more appropriate to use double-layer closure. A thinner myometrium is less well vascularized, which may lead to insufficient wound healing and niche development as in an incision in the cervical part of the uterus in active labor. The most recent systematic review and meta-analysis on uterine closure to reduce niche development after cesarean section shows as follows: double-layer unlocked closure is preferable to single-layer and locked closure, and it results in less dysmenorrhea. Inclusion of the decidua seems to be optimal in terms of healing ratio and niche development. The results of meta-analysis point to better scar healing on ultrasound after double-layer unlocked uterine closure including the decidual which might be related to better full thickness closure [4]. One study has demonstrated that women with large scar defects detected by TVS present a higher risk of uterine rupture or dehiscence in subsequent pregnancy than those with small defects. However, this is a retrospective study with a small sample size [5, 6].
It is important to treat symptomatic isthmocele because of the proposed postmenstrual abnormal uterine spotting, either spontaneously or after coitus, which disrupts the quality of cervical mucus and is harmful for sperm survival and motility, or because of a reflux to the endometrial cavity resulting in chronic endometritis, implantation failure, and pelvic pain. No surgery is required for asymptomatic women, and those who have no (future) desire to conceive. They can also use a levonorgestrel intrauterine device or combined pills or undergo a hysterectomy [7]. The residual myometrium is a limiting factor for hysteroscopic niche resections. Most publications report a desired residual myometrium of 2–3 mm to avoid perforation or bladder injury. In a multicenter randomized controlled trial conducted among women with a niche with a residual myometrium of ≥ 3 mm (52 patients subjected to hysteroscopy versus 51 patients subjected to expectant management), it was found that hysteroscopic niche resection reduced postmenstrual spotting and spotting-related discomfort [8]. A laparoscopic niche resection can be considered for large niches with a residual myometrium of less than 2–3 mm in those desiring conception. Contraceptives should be used for 6 months after the intervention to allow the uterine scar to heal properly, and cesarean section shows better to be recommended at term on next pregnancy [9]. Transvaginal repair for cesarean section scar diverticulum can be performed, where an incision is made at the anterior cervicovaginal junction, and the bladder was dissected away until the anterior peritoneal reflection is identified. Afterward, the defect is located in the previous cesarean incision, where the residual myometrium was thin. With the guidance of a probe in the uterus, a small hollow or depression is identified in the anterior wall of the lower uterus below the internal orifice of the cervix. A transverse incision is made at the most prominent area of the bulge, which usually presented with blood clots. The defect was removed, and the edges of the incision are trimmed to repair the defect [10]. In case of incidental diagnosis in asymptomatic women, surgery is not recommended, but asymptomatic women who wish to conceive in the future may also require surgical repair owing to the high risk of uterine rupture especially if affecting more than 50% of the myometrium [11,12,13].
References
Jordans IPM, de Leeuw RA, Stegwee SI, Amso NN, Barri-Soldevila PN, van den Bosch T, Bourne T, Brolmann HAM, Donnez O, Dueholm M et al (2019) Sonographic examination of uterine niche in non-pregnant women: a modified Delphi procedure. Ultrasound Obstet Gynecol 53(1):107–115
van der Voet LF, Vervoort AJ, Veersema S, BijdeVaate AJ, Brölmann HA, Huirne JA (2014) Minimally invasive therapy for gynaecological symptoms related to a niche in the caesarean scar: a systematic review. BJOG 121(2):145–156
de Vaate AJB, van der Voet LF, Naji O, Witmer M, Veersema S, Brölmann HA, Bourne T, Huirne JA (2014) Prevalence, potential risk factors for development and symptoms related to the presence of uterine niches following Cesarean section: systematic review. Ultrasound Obstet Gynecol 43(4):372–382
Stegwee SI, Jordans I, van der Voet LF, van de Ven PM, Ket J, Lambalk CB, de Groot C, Hehenkamp W, Huirne J (2018) Uterine caesarean closure techniques affect ultrasound findings and maternal outcomes: a systematic review and meta-analysis. BJOG 125(9):1097–1108
Stegwee SI, Jordans IP, Van Der Voet LF, Bongers MY, De Groot CJ, Lambalk CB, De Leeuw RA, Hehenkamp WJ, Van De Ven PM, Bosmans JE, Pajkrt E (2019) Single-versus double-layer closure of the caesarean (uterine) scar in the prevention of gynaecological symptoms in relation to niche development—the 2close study: a multicentre randomised controlled trial. BMC Pregnancy Childbirth 19(1):85
Vikhareva Osser O, Valentin L (2011) Clinical importance of appearance of cesarean hysterotomy scar at transvaginal ultrasonography in nonpregnant women. Obstet Gynecol 117:525–532
de Vacate AJB, van der Voet LF, Naji O, Witmer M, Veersema S, Brölmann HA, Bourne T, Huirne JA (2014) Reply: Niche risk factor for uterine rupture? Ultrasound Obstet Gynecol 44(3):371–372
Vervoort A, van der Voet LF, Hehenkamp W et al (2017) Hysteroscopic resection of a uterine caesarean scar defect (niche) in women with postmenstrual spotting: a randomised controlled trial. BJOG 125(3):326–334. https://doi.org/10.1111/1471-0528.14733
de Vaate AJMB, Linskens IH, van der Voet LF, Twisk JW, Brölmann HA, Huirne JA (2015) Reproducibility of three-dimensional ultrasound for the measurement of a niche in a caesarean scar and assessment of its shape. Eur J Obstet Gynecol Reprod Biol 188:39–44
Chen Y, Chang Y, Yao S (2014) Transvaginal management of cesarean scar section diverticulum: a novel surgical treatment. Med Sci Monit 20:1395–1399. https://doi.org/10.12659/msm.890642(Published 2014 Aug 8)
Donnez O, Donnez J, Orellana R, Dolmans MM (2017) Gynecological and obstetrical outcomes after laparoscopic repair of a cesarean scar defect in a series of 38 women. Fertil Steril. 107(1):289–296.e2. https://doi.org/10.1016/j.fertnstert.2016.09.033
Rheinboldt M, Osborn D, Delproposto Z (2015) Cesarean section scar ectopic pregnancy: a clinical case series. J Ultrasound 18:191. https://doi.org/10.1007/s40477-015-0162-5
Singh N, Tripathi R, Mala YM et al (2015) Scar thickness measurement by transvaginal sonography in late second trimester and third trimester in pregnant patients with previous cesarean section: does sequential change in scar thickness with gestational age correlate with mode of delivery? J Ultrasound 18:173. https://doi.org/10.1007/s40477-014-0116-3
Funding
This study was not funded.
Author information
Authors and Affiliations
Contributions
Elagwany was the only contributor in the conception, planning, carrying out, analyzing and writing up of the work.
Corresponding author
Ethics declarations
Conflict of interest
The author has nothing to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the patients included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
El Agwany, A.S. Gynecological and postpartum ultrasonography of cesarean uterine scar defects: a pictorial essay. J Ultrasound 23, 613–619 (2020). https://doi.org/10.1007/s40477-019-00403-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-019-00403-3