Abstract
Calcific tendinopathy is a condition that is related to the deposition of calcium, mostly hydroxyapatite crystals, within the tendons. The shoulder and the hip are commonly affected joints, but calcific tendinopathy may occur in any tendon of the body. While there is an extensive literature on the ultrasound diagnosis of calcific tendinopathy of the shoulder, there are only sporadic reports on other sites. This review combines the experience of our centers and a thorough analysis of the literature from the last 45 years (1972–2017) in order to highlight the localizations beyond the rotator cuff, their ultrasound characteristics and therapeutic possibilities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcific tendinopathy is a common condition related to deposition of calcium, mostly hydroxyapatite crystals, within the tendons. More rarely the pathology can affect also other anatomical structures as the ligaments. The condition is unique and distinct from degenerative tendons disease, and indeed calcium deposition in degenerative tendinopathy has a different chemical composition than in calcific tendinitis. The shoulder and the hip are the most commonly affected joints [1], but calcific tendinitis may occur in any tendons of the body [2, 3]. In many cases asymptomatic, it can sometimes be a cause of severe pain. The pathogenesis is not completely understood, but it seems related to areas of hypoxia in tendons, which lead to fibrocartilaginous metaplasia, followed by the formation of a calcium deposit, typically in healthy tendons with no pathologic findings.
Calcific tendinopathy is a dynamic process that evolves through successive stages, characterized by distinct imaging, pathologic and clinical features. Four stages of disease are described in the Uhthoff Cycle [4]: pre-calcific, in which fibrocartilaginous transformation occurs within tendon fibers, usually asymptomatic (Stage 1); formative, in which calcifications are formed, usually poorly symptomatic and including sub-acute low-grade pain, increasing at night (Stage 2); resorptive, in which the tendon develops increased vasculature and calcium deposits are usually removed by phagocytes, but calcifications may migrate into the adjacent structures (Stage 3); and post-calcific, in which there is self-healing and repair of the tendon fibers over several months, which may be associated with pain and restricted function (Stage 4).
While there is an extensive literature on the ultrasound diagnosis of the calcific tendinopathy of the shoulder and its therapies [5,6,7,8,9,10], there are only sporadic reports on the other sites. This article aims to provide a systematic review of the literature to highlight the localizations of calcific tendinopathy beyond the rotator cuff, its ultrasound characteristics and the therapeutic possibilities.
This review is generated from the combined experience of our centers, as indicated by the references in the text, and a thorough analysis of the literature from the last 45 years (1972–2017). A systematic search of the literature was performed in PubMed and included original studies and review articles. Case reports and case series were selected according to clinical relevance. Of the 192 selected articles on PubMed animal and cadaver studies were excluded (8 articles), so 184 articles were evaluated (Tables 1, 2, 3).
Neck
The neck, despite being a rare site of calcific tendinopathy, is the most frequently reported site in the literature, with 157 patients in 79 different articles. Calcific deposits tend to occur anteriorly to C1 and C2, near the insertion of the longus colli muscle, in two cases anteriorly to C4–C5 and, only in one, to C5–C6. Calcific tendinopathy may manifest with cervical and shoulder pain [75], neck stiffness, dysphagia or odynophagia, sore throat, fever and mild leukocytosis. Clinical findings of calcific retropharyngeal tendonitis are similar to the retropharyngeal abscess that represents a medical emergency [46]. Other conditions, like meningitis, pharyngitis, epiglottitis, infectious spondylitis, traumatic injury, cervical disk herniation, muscle spasm, foreign body aspiration and neoplasm, must be excluded [23, 39].
Standard latero-lateral radiographs of the cervical spine, showing calcification at the insertion of the longus colli muscle, are usually adequate for a diagnosis. Computed tomography may be useful for a differential diagnosis with retropharyngeal abscess. Magnetic resonance imaging can identify prevertebral edema [77]. There are no descriptions of ultrasound evaluations of calcific tendinopathy of the neck muscles, most likely because they are rarely examined using ultrasound.
Shoulder and arm
The shoulder is the joint most commonly affected by calcific tendinopathy, mostly the rotator cuff tendons [3, 10, 187], rarely the other tendons (pectoralis major, trapezius, biceps brachii) (Fig. 1). Pectoralis major calcific tendinopathy was described in four articles. Radiographs all showed a lithic area of the lateral humeral cortex with periosteal reaction. Second-level examinations (computed tomography and magnetic resonance imaging) and, in one case biopsy, were necessary for the aspecific findings of the radiographs. A single case of calcific tendinopathy is reported in the trapezius tendon. Biceps brachii calcific tendinopathy has been reported in both the proximal and the distal insertions (Fig. 2), except of the brief head. Calcific tendinopathy was also reported concomitant in the biceps tendon and in the rotator cuff tendon [98]. One of the five cases of calcific distal biceps tendinitis affected a 3-year-old boy [114]. Physical examination shows pain, tenderness, swelling and functional limitation, without a history of traumatic events. The differential diagnoses of extra-articular calcific tendinopathy are with calcific bursitis and loose bodies in the biceps tendon recess and synovial osteochondromatosis [98]. Radiography and ultrasound are sufficient for diagnosis.
Elbow and forearm
Two cases of calcific tendinopathy of the common extensor tendon of the elbow were described in two young women exhibiting pain, swelling and functional limitation. Radiograph and ultrasound showed soft-fluid calcification near the muscle insertion [90]. To our knowledge, the common flexor tendon has not been reported in the literature as affected.
Hand and wrist
Tendons of the hand and wrist [188, 189] are rarely reported as affected by calcific tendinopathy (incidence of 2%) [116], but more often the flexor tendons than the extensors (flexor carpi ulnaris four cases, flexor digitorum profundus two cases, flexor digitorum superficialis two cases, abductor pollicis brevis 2). Authors have described calcific tendinopathy in the flexor carpi radialis, abductor digiti minimi, extensor pollicis longus, abductor pollicis longus, flexor pollicis longus and the tendons of the intrinsic muscles. Two cases of calcific tendinopathy of the carpal tunnel tendons have been reported in literature, both with carpal tunnel syndrome.
The differential diagnosis includes soft-tissue infection, bone fracture, metabolic disorder (hyperparathyroidism, gout, pseudogout, hypervitaminosis D, hypercalcemia), degenerative or inflammatory or autoimmune conditions. Clinical presentation, ultrasound and radiographs can differentiate calcific tendinopathy from other etiologies [121].
Hip
The hip [190] is the second most common site of calcific tendinopathy, after the shoulder [158]. The tendons of the rectus femoris are the most commonly involved (Fig. 3) described in 56 patients in 14 different articles. Both direct and indirect tendon components may be affected by this pathology, with prevalence, in our experience, of the direct tendon. But it is also necessary to distinguish the tendinous calcifications from calcifications of their insertional bursae, just beneath the direct and indirect tendon, that may occur quite frequently. The second most common group are the gluteal tendons (42 cases of the gluteus medius and 36 cases of the gluteus maximus reported). Adductor magnus, adductor longus and adductor brevis calcific tendinopathy have been described in six cases (1 magnus, 1 brevis and 4 unknown). Other rare sites are the piriformis (2 cases), the iliopsoas (2 cases), the ischiococcygeus (1 case) and the sartorius (1 case).
Usually occurring in middle-age, patients have functional limitation, tenderness, pain and a positive Patrick’s test [183]. Depending on the affected tendon, the differential diagnosis includes infection [124, 180], arthritis, lumbar radiculopathy [126, 140, 168], os acetabuli, avulsion fracture, insertional calcified bursitis, sesamoid bones, myositis ossificans and chondrosarcoma [146]. Sonography and standard radiographs can be used for diagnosis, showing the calcification. Sometimes computed tomography is useful for bone evaluation, and MRIs to show soft-tissue edema and bone marrow edema.
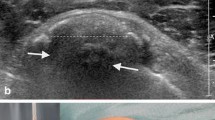
Thigh, knee and leg
Thigh, knee and leg are rarely affected by calcific tendinopathy, and only a few cases involving the quadriceps tendon, patellar tendon (Fig. 4) and iliotibial band (Fig. 5) [191] are described. In many articles [125, 162] there is no distinction between calcific tendinopathy and calcifications of tendinous tendons, but the majority are calcifications in tendinous tendons. As usual, patients have functional limitations, tenderness and pain. The articles confirm the main role of ultrasound in the diagnosis and in the management of calcific tendinopathy, even of the less common ones.
Foot and ankle
Calcific tendinopathy of the ankle [192] and foot is frequently misdiagnosed because of its rare occurrence and a clinical presentation that is similar to other entities. Achilles tendon calcific tendinopathy was described in eight articles, in both sexes, but more commonly in males. The second most commonly involved tendons are the peroneus longus (3 cases) and the flexor hallucis brevis (2 cases). Single cases have been described in other tendons (extensor hallucis longus, tibialis posterior and flexor of the forefoot).
Motion restriction secondary to pain, erythema, swelling and tenderness are the most frequent symptoms, in the absence of acute trauma [108]. The differential diagnosis is broad and includes gout or pseudogout, avulsion fractures, sesamoid bones, myositis ossificans and infection [156]. Ultrasonography and radiography can be used to make a diagnosis of calcific tendinopathy of the ankle and the foot, while computed tomography and MRI have few indications [136].
Ligaments
Calcifications of the ligaments, that can produce an important pain symptomatology like the calcific tendinopathy of the rotator cuff, are more frequent in the medial collateral ligament (proximal insertion) of the knee, where they can also become of considerable size [193, 194]. Other ligaments less frequently affected by the pathology are the lateral collateral ligament, the anterior or posterior cruciate ligament of the knee and sometimes Wrisberg ligament [195, 196].
Differential diagnosis
Depending on the affected tendon the differential diagnosis includes many diseases. Among the idiopathic ones the most known is the diffuse idiopathic skeletal hyperostosis (DISH) which predominantly affects the spine while ligaments and tendons of the appendicular skeleton are rarely involved [197]. In these cases, the US differential diagnosis is not possible and is generally related to the distribution and site of the calcifications.
The differential diagnosis with the calcification in a degenerative tendinopathy is more easy even with the ultrasound because the affected tendon appear as normal in calcific tendinopathy while shows diffuse signs of degeneration (e.g., hypoechogenicity, loss of the fibrillar aspect) around the calcification in a degenerative tendinopathy. In the most challenging cases, CT and MRI may be necessary.
Non-surgical treatment (or conservative, or minimally invasive treatments)
Calcific tendinopathy is usually a self-limited condition, so the initial management of pain is conservative, with physical therapy and oral administration of NSAIDs. If these treatments fail, other non-surgical therapeutic options may be considered: extra-corporeal shock wave therapy (ESWT), steroid injection (ultrasound-guided or unguided) and US-guided percutaneous aspiration of calcific tendinopathy (US-PICT). ESWT is based on the application of repetitive pulses over the affected site. The results are variable and the exact underlying mechanism of the therapeutic effect on calcific tendinopathy is still debated. It seems to be related to the phagocytosis of calcium deposition induced by the neovascularization response and leukocyte chemotaxis [198]; ESWT therapy is painful, expensive and not widely available. The use of conservative treatment or ESWT in patients with acute pain from calcific tendinopathy in resorption seems to be suboptimal, and often fails. The symptoms in this phase significantly impact quality of life [9, 199]. Minimally invasive interventional techniques (steroid injection of calcific tendinitis) may be used in these cases (US-guided or unguided) and/or US-guided percutaneous aspiration of calcific tendinopathy (US-PICT) [200]. A study by de Witta et al. reports that US-PICT is a superior method compared to steroid injection in the calcific tendinitis of the rotator cuff [201]. In cases of hard calcifications in mildly symptomatic patients, elective treatments should be considered [202]. Percutaneous treatment is not indicated when patients are asymptomatic, and calcification is very small (≤ 5 mm) [203]. Different approaches have been reported in recent studies and all include the use of a fluid: local anesthetic or saline solution to dissolve calcium deposits; one needle or two needles are used to inject and retrieve the fluid to dissolve calcium deposits. Recent evidence has suggested that a double-needle approach might be more appropriate for treating harder deposits, while one needle may be more useful in treating fluid calcifications. Some advantages of US-PICT are that the procedure does not require any hospitalization, is performed under local anesthesia, the patient can return home about 30 min after the procedure is complete, there is no need for post-procedural immobilization, and the patient can return to work sooner [10].
Surgical treatment
Arthroscopic treatment of calcific tendinitis involves selected cases in which conservative or less invasive approaches have failed. Calcification removal techniques vary according to the type of tendon incision and the instrumentation used to remove the calcium deposit. The surgery allows the removal of calcification and a thorough cleaning of the joint of interest. Surgery requires hospitalization, general anesthesia or sedation, however, and a relatively long rehabilitation period after treatment.
Conclusion
Calcific tendinopathy is commonly found in non-rotator cuff tendons. It is easily diagnosed using ultrasound, although ultrasound is rarely used in some anatomic sites, such as neck muscles. Depending on the affected tendon the differential diagnosis includes many diseases, and CT and MRI may be necessary. Usually occurring in middle-age, it can however affect patients of all ages, and a case was reported in a 3-year-old boy. Patients with calcific tendinopathy have functional limitation, tenderness and pain.
Resorption of deposits generally occurs spontaneously, although some patients show persistent clinical symptoms and require therapy. Various therapies can be used, although ultrasonographic guided therapeutic procedures (steroid injection or percutaneous aspiration) seem to be the most effective, particularly for calcific tendinopathy in resorption. Surgery remains an option in cases where other approaches have failed.
References
Hayes CW, Conway WF (1990) Calcium hydroxyapatite deposition disease. RadioGraphics 10(6):1031–1048
Faure G, Daculsi G (1983) Calcified tendinitis: a review. Ann Rheum Dis 42(Suppl 1):49–53
Siegal DS, Wu JS, Newman JS et al (2009) Calcific tendinitis: a pictorial review. Can Assoc Radiol J J Assoc Can Radiol 60(5):263–272
Uhthoff HK, Sarkar K (1989) Calcifying tendinitis. Baillieres Clin Rheumatol 3(3):567–581
Messina C, Banfi G, Orlandi D et al (2016) Ultrasound-guided interventional procedures around the shoulder. Br J Radiol 89(1057):20150372
Lanza E, Banfi G, Serafini G et al (2015) Ultrasound-guided percutaneous irrigation in rotator cuff calcific tendinopathy: what is the evidence? A systematic review with proposals for future reporting. Eur Radiol 25(7):2176–2183
Tagliafico A, Russo G, Boccalini S et al (2014) Ultrasound-guided interventional procedures around the shoulder. Radiol Med (Torino) 119(5):318–326
Draghi F, Scudeller L, Draghi AG et al (2015) Prevalence of subacromial-subdeltoid bursitis in shoulder pain: an ultrasonographic study. J Ultrasound 18(2):151–158
Robotti G, Canepa MG, Bortolotto C et al (2013) Interventional musculoskeletal US: an update on materials and methods. J Ultrasound 16(2):45–55
Draghi F, Robotti G, Jacob D et al (2010) Interventional musculoskeletal ultrasonography: precautions and contraindications. J Ultrasound 13(3):126–133
Abdelbaki A, Abdelbaki S, Bhatt N et al (2017) Acute calcific tendinitis of the longus colli muscle: report of two cases and review of the literature. Cureus 9(8):e1597
Ahmed OH, German MA, Handwerker J et al (2012) Radiology quiz case 2. Acute calcific tendinitis of the longus colli (also known as calcific retropharyngeal/prevertebral tendinitis). Arch Otolaryngol Head Neck Surg 138(6):599–600
Alamoudi U, Al-Sayed AA, AlSallumi Y et al (2017) Acute calcific tendinitis of the longus colli muscle masquerading as a retropharyngeal abscess: a case report and review of the literature. Int J Surg Case Rep 41:343–346
Andrade CS, Peixoto CAR, Cevasco FKI et al (2015) Longus colli calcific acute tendinitis: typical features with distinct imaging modalities. Arq Neuropsiquiatr 73(1):69–70
Bailey CW, Connolly BD, Sterner K et al (2015) Acute calcific longus colli tendonitis. W V Med J 111(2):10–12
Benanti JC, Gramling P, Bulat PI et al (1986) Retropharyngeal calcific tendinitis: report of five cases and review of the literature. J Emerg Med 4(1):15–24
Bladt O, Vanhoenacker R, Bevernage C et al (2008) Acute calcific prevertebral tendinitis. JBR-BTR Organe Soc R Belge Radiol SRBR Orgaan Van K Belg Ver Voor Radiol KBVR 91(4):158–159
Blome SA (1987) Retropharyngeal calcific tendinitis. Australas Radiol 31(2):142–143
Boikov AS, Griffith B, Stemer M et al (2012) Acute calcific longus colli tendinitis: an unusual location and presentation. Arch Otolaryngol Head Neck Surg 138(7):676–679
Borrmann A, Niedermeyer HP, Arnold W (2008) Retropharyngeal tendinitis–a rare differential diagnosis of retropharyngeal abscess. Laryngorhinootologie 87(3):186–189
Chen C-H, Lu Y-C, Wong T-Y (2015) Acute calcific prevertebral tendinitis: rare cause of neck pain. Acute Med Surg 2(3):199–201
Chung T, Rebello R, Gooden EA (2005) Retropharyngeal calcific tendinitis: case report and review of literature. Emerg Radiol 11(6):375–380
Colella DM, Calderón Sandoval F et al (2016) A rare cause of dysphagia to remember: calcific tendinitis of the longus colli muscle. Case Rep Gastroenterol 10(3):755–759
Coulier B, Macsim M, Desgain O (2011) Retropharyngeal calcific tendinitis–longus colli tendinitis–an unusual cause of acute dysphagia. Emerg Radiol 18(5):449–451
De Maeseneer M, Vreugde S, Laureys S et al (1997) Calcific tendinitis of the longus colli muscle. Head Neck 19(6):545–548
De Temmerman G, Marcelis S, Beeckman P (2007) Acute calcific retropharyngeal tendonitis. JBR-BTR Organe Soc R Belge Radiol SRBR Orgaan Van K Belg Ver Voor Radiol KBVR 90(3):184–185
Desmots F, Derkenne R, Couppey N (2013) Calcific retropharyngeal tendinitis of the longus colli muscle Answer to the e-quid. ‘Acute cervical pain and dysphagia in a 43 year-old man’. Diagn Interv Imaging 94(4):470
Eastwood JD, Hudgins PA, Malone D (1998) Retropharyngeal effusion in acute calcific prevertebral tendinitis: diagnosis with CT and MR imaging. AJNR Am J Neuroradiol 19(9):1789–1792
Ellika SK, Payne SC, Patel SC et al (2008) Acute calcific tendinitis of the longus colli: an imaging diagnosis. Dento Maxillo Facial Radiol 37(2):121–124
Estimable K, Rizk C, Pujalte GGA (2015) A rare case of neck pain: acute longus colli calcific tendinitis in a possibly immunocompromised individual. J Am Board Fam Med JABFM 28(1):146–150
Fahlgren H (1986) Retropharyngeal tendinitis. Cephalalgia Int J Headache 6(3):169–174
Figler T (1993) Radiologic case study Calcific tendonitis of the longissimus colli muscle. Orthopedics 16(12):1365
Gabra N, Belair M, Ayad T (2013) Retropharyngeal calcific tendinitis mimicking a retropharyngeal phlegmon. Case Rep Otolaryngol 2013:912628
Hall FM, Docken WP, Curtis HW (1986) Calcific tendinitis of the longus coli: diagnosis by CT. AJR Am J Roentgenol 147(4):742–743
Haun CL (1978) Retropharyngeal tendinitis. AJR Am J Roentgenol 130(6):1137–1140
Horowitz G, Ben-Ari O, Brenner A et al (2013) Incidence of retropharyngeal calcific tendinitis (longus colli tendinitis) in the general population. Otolaryngol-Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg 148(6):955–958
Jiménez S, Millán JM (2007) Calcific retropharyngeal tendinitis: a frequently missed diagnosis. Case report. J Neurosurg Spine 6(1):77–80
Joshi GS, Fomin DA, Joshi GS et al (2016) Unusual case of acute neck pain: acute calcific longus colli tendinitis. BMJ Case Rep 2:2016
Kanzaria H, Stein JC (2011) A severe sore throat in a middle-aged man: calcific tendonitis of the longus colli tendon. J Emerg Med 41(2):151–153
Kaplan MJ, Eavey RD (1984) Calcific tendinitis of the longus colli muscle. Ann Otol Rhinol Laryngol 93(3 Pt 1):215–219
Karasick D, Karasick S (1981) Calcific retropharyngeal tendinitis. Skeletal Radiol 7(3):203–205
Kenzaka T, Kumabe A (2017) Acute calcific prevertebral tendinitis. Intern Med Tokyo Jpn 56(12):1611
Khurana B (2012) Calcific tendinitis mimicking acute prevertebral abscess. J Emerg Med 42(1):e15–e16
Kim Y-J, Park J-Y, Choi K-Y et al (2017) Case reports about an overlooked cause of neck pain: calcific tendinitis of the longus colli: case reports. Medicine (Baltimore) 96(46):e8343
Kupferman TA, Rice CH, Gage-White L (2007) Acute prevertebral calcific tendinitis: a nonsurgical cause of prevertebral fluid collection. Ear Nose Throat J 86(3):164–166
Kusunoki T, Muramoto D, Murata K (2006) A case of calcific retropharyngeal tendinitis suspected to be a retropharyngeal abscess upon the first medical examination. Auris Nasus Larynx 33(3):329–331
Lee S, Joo KB, Lee KH et al (2011) Acute retropharyngeal calcific tendinitis in an unusual location: a case report in a patient with rheumatoid arthritis and atlantoaxial subluxation. Korean J Radiol 12(4):504–509
Leep Hunderfund AN, Robertson CE, Bell ML et al (2008) Calcific retropharyngeal tendinitis: unusual cause of acute neck pain with nuchal rigidity. Neurology 71(10):778
Mannoji C, Koda M, Furuya T et al (2015) Calcific tendinitis of the longus colli. Intern Med 54(12):1573
Martindale JL, Senecal EL (2012) Atraumatic neck pain and rigidity: a case of calcific retropharyngeal tendonitis. Am J Emerg Med 30(4):636.e1–636.e2
Mihmanli I, Karaarslan E, Kanberoglu K (2001) Inflammation of vertebral bone associated with acute calcific tendinitis of the longus colli muscle. Neuroradiology 43(12):1098–1101
Naqshabandi AM, Srinivasan J (2011) Teaching neuroimages: acute calcific tendinitis of longus colli mimicking meningismus. Neurology 76(17):e81
Newmark H, Forrester DM, Brown JC et al (1978) Calcific tendinitis of the neck. Radiology 128(2):355–358
Newmark H, Zee CS, Frankel P et al (1981) Chronic calcific tendinitis of the neck. Skeletal Radiol 7(3):207–208
Newmark H, Blackford D, Roberts D et al (1986) Computed tomography of acute cervical spine tendinitis. J Comput Tomogr 10(4):373–375
Nozu T, Kumei S, Ohhira M et al (2015) Retropharyngeal calcific tendinitis. Intern Med Tokyo Jpn 54(17):2277
Nunes C, Casimiro C, Carreiro I (2012) Imagiology of the acute calcific tendinitis of the longus colli. Acta Med Port 25(Suppl 1):51–55
Offiah CE, Hall E (2009) Acute calcific tendinitis of the longus colli muscle: spectrum of CT appearances and anatomical correlation. Br J Radiol 82(978):e117–e121
Oh JY, Lim JH, Kim YS et al (2016) Misconceived retropharyngeal calcific tendinitis during management of myofascial neck pain syndrome. Korean J Pain 29(1):48–52
Omezzine SJ, Hafsa C, Lahmar I et al (2008) Calcific tendinitis of the longus colli: diagnosis by CT. Jt Bone Spine Rev Rhum 75(1):90–91
Park R, Halpert DE, Baer A et al (2010) Retropharyngeal calcific tendinitis: case report and review of the literature. Semin Arthritis Rheum 39(6):504–509
Park SY, Jin W, Lee SH et al (2010) Acute retropharyngeal calcific tendinitis: a case report with unusual location of calcification. Skeletal Radiol 39(8):817–820
Pellicer García V, Pérez Moya C, Magán Martín A (2012) Acute calcific prevertebral tendinitis: case report and literature review. Rev Espanola Cirugia Ortop Traumatol 56(5):389–392
Queinnec S, Petrover D, Guigui P et al (2011) Benign febrile cervicalgia due to calcific retropharyngeal tendinitis: case study. Orthop Traumatol Surg Res OTSR 97(3):341–344
Razon RVB, Nasir A, Wu GS et al (2009) Retropharyngeal calcific tendonitis: report of two cases. J Am Board Fam Med JABFM 22(1):84–88
Sanghvi DA, Jankharia BG, Purandare NC et al (2006) Radiologic case study Acute calcific retropharyngeal tendinitis. Orthopedics 29(7):561
Sarkozi J, Fam AG (1984) Acute calcific retropharyngeal tendinitis: an unusual cause of neck pain. Arthritis Rheum 27(6):708–710
Shibuki T, Goto H, Fukushima K et al (2017) Acute prevertebral calcific tendinitis. Intern Med Tokyo Jpn 56(10):1275
Shin D-E, Ahn C-S, Choi J-P (2010) The acute calcific prevertebral tendinitis: report of two cases. Asian Spine J 4(2):123–127
Silva CF, Soffia PS, Pruzzo E (2014) Acute prevertebral calcific tendinitis: a source of non-surgical acute cervical pain. Acta Radiol Stockh Swed 55(1):91
Siwiec RM, Kushner DJ, Morrison JL (2009) Retropharyngeal calcific tendinitis. J Rheumatol 36(7):1546–1547
Sokolov M, Yaffe D, Ophir D (2009) Retropharyngeal calcific tendinitis. Isr Med Assoc J IMAJ 11(11):701–702
Sierra Solís A, Fernández Prudencio L (2017) Acute calcific tendinitis of the longus colli muscle. Acta Otorrinolaringol Esp 68(4):244–245
Southwell K, Hornibrook J, O’Neill-Kerr D (2008) Acute longus colli calcific tendonitis causing neck pain and dysphagia. Otolaryngol-Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg 138(3):405–406
Suyama Y, Kishimoto M, Nozaki T et al (2015) Acute calcific tendinitis of the longus colli muscle. Arthritis Rheumatol Hoboken NJ 67(9):2446
Szelei N, Tassart M, Le Breton C et al (2001) Calcific retropharyngeal tendinitis: unusual diagnosis. J Radiol 82(9 Pt 1):1001–1004
Tagashira Y, Watanuki S (2015) Acute calcific retropharyngeal tendonitis. CMAJ Can Med Assoc J J Assoc Medicale Can 187(13):995
Tamm A, Jeffery CC, Ansari K et al (2015) Acute prevertebral calcific tendinitis. J Radiol Case Rep 9(11):1–5
Tezuka F, Sakai T, Miyagi R et al (2014) Complete resolution of a case of calcific tendinitis of the longus colli with conservative treatment. Asian Spine J 8(5):675–679
Torbati SS, Vos EM, Bral D et al (2014) Calcific tendinitis of the longus colli muscle. Ear Nose Throat J 93(12):492–493
Uchiyama D, Nakamura K, Yoshida S et al (2016) Calcific tendinitis of the longus colli. Intern Med Tokyo Jpn 55(5):553
Ulusoy OL, Tutar S, Ozturk E et al (2016) Calcific tendinitis of the longus colli muscle: a rare cause of neck pain. Neurol India 64(5):1085–1086
Van Kerkhove F, Geusens E, Knockaert D (2007) Retropharyngeal calcific tendonitis. Eur J Emerg Med Off J Eur Soc Emerg Med 14(5):269–271
Wakabayashi Y, Hori Y, Kondoh Y et al (2012) Acute calcific prevertebral tendonitis mimicking tension-type headache. Neurol Med Chir (Tokyo) 52(9):631–633
Widlus DM (1985) Calcific tendonitis of the longus colli muscle: a cause of atraumatic neck pain. Ann Emerg Med 14(10):1014–1017
Wolzak H, van de Rest M, Geurts M et al (2010) Acute calcific tendinitis of the longus colli muscle: an often unrecognized cause of severe neck pain. J Clin Rheumatol Pract Rep Rheum Musculoskelet Dis 16(5):240–241
Yaylacı S, Öztürk TC, Aksoy E et al (2015) Retropharyngeal calcific tendinitis: report of two cases. J Emerg Trauma Shock 8(2):119–120
Zapolsky N, Heller M, Felberbaum M et al (2017) Calcific tendonitis of the longus colli: an uncommon but benign cause of throat pain that closely mimics retropharyngeal abscess. J Emerg Med 52(3):358–360
Zibis AH, Giannis D, Malizos KN et al (2013) Acute calcific tendinitis of the longus colli muscle: case report and review of the literature. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 22(Suppl 3):S434–S438
Abate M, Salini V, Schiavone C (2016) Ultrasound-guided percutaneous lavage in the treatment of calcific tendinopathy of elbow extensor tendons: a case report. Malays Orthop J 10(2):53–55
Ali SN, Kelly JL (2004) Acute calcific tendinitis of the finger–a case report. Hand Surg Int J Devoted Hand Up Limb Surg Relat Res J Asia-Pac Fed Soc Surg Hand 9(1):105–107
Cahir J, Saifuddin A (2005) Calcific tendonitis of pectoralis major: CT and MRI findings. Skeletal Radiol 34(4):234–238
Dilley DF, Tonkin MA (1991) Acute calcific tendinitis in the hand and wrist. J Hand Surg Edinb Scotl 16(2):215–216
Dürr HR, Lienemann A, Silbernagl H et al (1997) Acute calcific tendinitis of the pectoralis major insertion associated with cortical bone erosion. Eur Radiol 7(8):1215–1217
El-Essawy MT, Vanhoenacker FM (2012) Calcific tendinopathy of the pectoralis major insertion with intracortical protrusion of calcification. JBR-BTR Organe Soc R Belge Radiol SRBR Orgaan Van K Belg Ver Voor Radiol KBVR 95(6):374
Galliani I, Columbaro M, Ferri S et al (1998) A case of calcific lateral epicondylitis: a histological and ultrastructural study. Br J Rheumatol 37(2):235–236
Garayoa SA, Romero-Muñoz LM, Pons-Villanueva J (2010) Acute compartment syndrome of the forearm caused by calcific tendinitis of the distal biceps. Musculoskelet Surg 94(3):137–139
Goldman AB (1989) Calcific tendinitis of the long head of the biceps brachii distal to the glenohumeral joint: plain film radiographic findings. AJR Am J Roentgenol 153(5):1011–1016
Gossner J (2018) Large bone erosion due to calcific tendinitis of the distal biceps tendon. Jt Bone Spine Rev Rhum 85(2):247
Greene TL, Louis DS (1980) Calcifying tendinitis in the hand. Ann Emerg Med 9(8):438–440
Hakozaki M, Iwabuchi M, Konno S et al (2007) Acute calcific tendinitis of the thumb in a child: a case report. Clin Rheumatol 26(5):841–844
Harris AR, McNamara TR, Brault JS et al (2009) An unusual presentation of acute calcific tendinitis in the hand. Hand N Y N 4(1):81–83
Huntley JS (2003) Dougall TW Mistaken identity: calcific tendinitis in the finger. Hosp Med Lond Engl 64(12):747
Ikegawa S (1996) Calcific tendinitis of the pectoralis major insertion. A report of two cases. Arch Orthop Trauma Surg 115(2):118
Kheterpal A, Zoga A, McClure K (2014) Acute calcific tendinitis of the flexor pollicis longus in an 8-year-old boy. Skeletal Radiol 43(10):1471–1475
Kim JH, Lee JH, Park JU et al (2016) Acute calcific tendinitis in the distal interphalangeal joint. Arch Plast Surg 43(3):301–303
Kim KC, Rhee KJ, Shin HD et al (2007) A SLAP lesion associated with calcific tendinitis of the long head of the biceps brachii at its origin. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 15(12):1478–1481
Lee HO, Lee YH, Mun SH et al (2012) Calcific tendinitis of the hand and foot: a report of four cases. J Korean Soc Magn Reson Med 16(2):177
Munjal A, Munjal P, Mahajan A (2013) Diagnostic dilemma: acute calcific tendinitis of flexor digitorum profundus. Hand N Y N 8(3):352–353
Murase T, Tsuyuguchi Y, Hidaka N et al (1994) Calcific tendinitis at the biceps insertion causing rotatory limitation of the forearm: a case report. J Hand Surg 19(2):266–268
Nofsinger CC, Williams GR, Iannotti JP (1999) Calcific tendinitis of the trapezius insertion. J Shoulder Elbow Surg 8(2):162–164
Park J-Y, Gupta A, Park H-K (2008) Calcific tendinitis at the radial insertion of the biceps brachii: a case report. J Shoulder Elbow Surg 17(6):e19–e21
Ryan WG (1993) Calcific tendinitis of flexor carpi ulnaris: an easy misdiagnosis. Arch Emerg Med 10(4):321–323
Sakamoto K, Kozuki K (2002) Calcific tendinitis at the biceps brachii insertion of a child: a case report. J Shoulder Elbow Surg 11(1):88–91
Saleh WR, Yajima H, Nakanishi A (2008) Acute carpal tunnel syndrome secondary to calcific tendinitis: case report. Hand Surg Int J Devoted Hand Up Limb Surg Relat Res J Asia-Pac Fed Soc Surg Hand 13(3):197–200
Schneider D, Hirsch M (2017) Acute calcific tendonitis of dorsal interosseous muscles of the hand: uncommon site of a frequent disease. Reumatismo 69(1):43–46
Seiler JG, Kerwin GA (1995) Adolescent trigger finger secondary to post-traumatic chronic calcific tendinitis. J Hand Surg 20(3):425–427
Selby CL (1984) Acute calcific tendinitis of the hand: an infrequently recognized and frequently misdiagnosed form of periarthritis. Arthritis Rheum 27(3):337–340
Shields JS, Chhabra AB, Pannunzio ME (2007) Acute calcific tendinitis of the hand: 2 case reports involving the abductor pollicis brevis. Am J Orthop Belle Mead NJ 36(11):605–607
Torbati SS, Bral D, Geiderman JM (2013) Acute calcific tendinitis of the wrist. J Emerg Med 44(2):352–354
Walocko FM, Sando IC, Haase SC et al (2017) Acute calcific tendinitis of the index finger in a child. Hand N Y N 12(5):NP84
Yasen S (2012) Acute calcific tendinitis of the flexor carpi ulnaris causing acute compressive neuropathy of the ulnar nerve: a case report. J Orthop Surg Hong Kong 20(3):414–416
Abram SGF, Sharma AD, Arvind C (2012) Atraumatic quadriceps tendon tear associated with calcific tendonitis. BMJ Case Rep 27:2012
Almedghio S, Garneti N (2014) The acute and chronic presentation of gluteus medius calcific tendinitis—a case report of two. J Orthop Case Rep. 4(4):48–50
Beebe JA, Cross PS (2013) Patellar tendinopathy: preliminary surgical results. Sports Health 5(3):220–224
Berney JW (1972) Calcifying peritendinitis of the gluteus maximus tendon. Radiology 102(3):517–518
Braun-Moscovici Y, Schapira D, Nahir AM (2006) Calcific tendinitis of the rectus femoris. J Clin Rheumatol Pract Rep Rheum Musculoskelet Dis 12(6):298–300
Choudur HN, Munk PL (2006) Image-guided corticosteroid injection of calcific tendonitis of gluteus maximus. J Clin Rheumatol Pract Rep Rheum Musculoskelet Dis 12(4):176–178
Cox D, Paterson FW (1991) Acute calcific tendinitis of peroneus longus. J Bone Jt Surg Br 73(2):342
Gillis CT, Lin JS (2016) Use of a central splitting approach and near complete detachment for insertional calcific achilles tendinopathy repaired with an achilles bridging suture. J Foot Ankle Surg Off Publ Am Coll Foot Ankle Surg 55(2):235–239
Doucet C, Gotra A, Reddy SMV et al (2017) Acute calcific tendinopathy of the popliteus tendon: a rare case diagnosed using a multimodality imaging approach and treated conservatively. Skeletal Radiol 46(7):1003–1006
Tennent TD, Goradia VK (2003) Arthroscopic management of calcific tendinitis of the popliteus tendon. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 19(4):E35
Durst HB, Kuster MS (2006) Extracorporeal shock-wave lithotripsy for the treatment of calcific tendonitis of the glutaeus maximus tendon. Z Orthop Ihre Grenzgeb 144(5):516–518
Ferraro A, Mercuri M, Ruggieri P et al (1995) Calcific tendinitis of the gluteus maximus. Chir Organi Mov 80(3):335–340
Garner HW, Whalen JL (2013) Acute calcific tendinosis of the flexor hallucis brevis: case report. Foot Ankle Int 34(10):1451–1455
Harries L, Kempson S, Watura R (2011) Calcific tendonitis of the tibialis posterior tendon at the navicular attachment. J Radiol Case Rep 5(6):25–30
Hottat N, Fumière E, Delcour C (1999) Calcific tendinitis of the gluteus maximus tendon: CT findings. Eur Radiol 9(6):1104–1106
Howell MA, Catanzariti AR (2016) Flexor hallucis longus tendon transfer for calcific insertional achilles tendinopathy. Clin Podiatr Med Surg 33(1):113–123
Huang K, Murphy D, Dehghan N (2017) Calcific tendinitis of the gluteus maximus of a 53-year-old woman. CMAJ Can Med Assoc J J Assoc Medicale Can 189(50):E1561
Jo H, Kim G, Baek S et al (2016) Calcific tendinopathy of the gluteus medius mimicking lumbar radicular pain successfully treated with barbotage: a case report. Ann Rehabil Med 40(2):368–372
Johnson KW, Zalavras C, Thordarson DB (2006) Surgical management of insertional calcific achilles tendinosis with a central tendon splitting approach. Foot Ankle Int 27(4):245–250
Kandemir U, Bharam S, Philippon MJ et al (2003) Endoscopic treatment of calcific tendinitis of gluteus medius and minimus. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 19(1):E4
Karakida O, Aoki J, Fujioka F et al (1995) Radiological and anatomical investigation of calcific tendinitis of the gluteus maximus tendon. Nihon Igaku Hoshasen Gakkai Zasshi Nippon Acta Radiol 55(7):483–487
Kim YS, Lee HM, Kim JP (2013) Acute calcific tendinitis of the rectus femoris associated with intraosseous involvement: a case report with serial CT and MRI findings. Eur J Orthop Surg Traumatol Orthop Traumatol 23(Suppl 2):S233–S239
Klammer G, Iselin LD, Bonel HM et al (2011) Calcific tendinitis of the peroneus longus: case report. Foot Ankle Int 32(6):638–640
Kobayashi H, Kaneko H, Homma Y et al (2015) Acute calcific tendinitis of the rectus femoris: a case series. J Orthop Case Rep 5(3):32–34
Johansson KJJ, Sarimo JJ, Lempainen LL et al (2013) Calcific spurs at the insertion of the Achilles tendon: a clinical and histological study. Muscles Ligaments Tendons J 2(4):273–277
Kurtoğlu S, Akın L, Kendirci M et al (2015) An unusual presentation of parathyroid adenoma in an adolescent: calcific achilles tendinitis. J Clin Res Pediatr Endocrinol 7(4):333–335
Lesavre A, Miquel A, Menu Y (2006) Misleading paradiaphyseal calcifications: calcific tendonitis. Presse Medicale Paris Fr 35(9 Pt 1):1273
Lim CH, Lin C-T, Chen Y-H (2017) Acute calcific tendinitis of gluteus maximus tendon due to tumoral calcium pyrophosphate dihydrate deposition disease. Int J Rheum Dis 20(12):2249–2252
Lin T-C, Lin C-Y, Chou C-L et al (2012) Achilles tendon tear following shock wave therapy for calcific tendinopathy of the Achilles tendon: a case report. Phys Ther Sport Off J Assoc Chart Physiother Sports Med 13(3):189–192
Maffulli N, Testa V, Capasso G et al (2004) Calcific insertional Achilles tendinopathy: reattachment with bone anchors. Am J Sports Med 32(1):174–182
Miao X-D, Jiang H, Wu Y-P et al (2016) Treatment of calcified insertional achilles tendinopathy by the posterior midline approach. J Foot Ankle Surg Off Publ Am Coll Foot Ankle Surg 55(3):529–534
Mizutani H, Ohba S, Mizutani M et al (1994) Calcific tendinitis of the gluteus maximus tendon with cortical bone erosion: CT findings. J Comput Assist Tomogr 18(2):310–312
Moon SG, Kim NR, Choi JW et al (2012) Acute coccydynia related to precoccygeal calcific tendinitis. Skeletal Radiol 41(4):473–476
Mouzopoulos G, Lasanianos N, Nikolaras G et al (2009) Peroneus longus acute calcific tendinitis: a case report. Cases J 1(2):7453
Paik NC (2014) Acute calcific tendinitis of the gluteus medius: an uncommon source for back, buttock, and thigh pain. Semin Arthritis Rheum 43(6):824–829
Park S-M, Baek J-H, Ko Y-B et al (2014) Management of acute calcific tendinitis around the hip joint. Am J Sports Med 42(11):2659–2665
Peng X, Feng Y, Chen G et al (2013) Arthroscopic treatment of chronically painful calcific tendinitis of the rectus femoris. Eur J Med Res 23(18):49
Pierannunzii L, Tramontana F, Gallazzi M (2010) Case report: calcific tendinitis of the rectus femoris: a rare cause of snapping hip. Clin Orthop 468(10):2814–2818
Pope TL, Keats TE (1992) Case report 733. Calcific tendinitis of the origin of the medial and lateral heads of the rectus femoris muscle and the anterior iliac spin (AIIS). Skeletal Radiol 21(4):271
Ramon FA, Degryse HR, De Schepper AM et al (1991) Calcific tendinitis of the vastus lateralis muscle. A report of three cases. Skeletal Radiol 20(1):21
Rhodes RA, Stelling CB (1986) Calcific tendinitis of the flexors of the forefoot. Ann Emerg Med 15(6):751–753
Rozenbaum M, Slobodin G, Boulman N et al (2008) Calcific tendonitis of the rectus femoris. J Clin Rheumatol Pract Rep Rheum Musculoskelet Dis 14(1):57
Sakai T, Shimaoka Y, Sugimoto M et al (2004) Acute calcific tendinitis of the gluteus medius: a case report with serial magnetic resonance imaging findings. J Orthop Sci Off J Jpn Orthop Assoc 9(4):404–407
Sarkar JS, Haddad FS, Crean SV et al (1996) Acute calcific tendinitis of the rectus femoris. J Bone Jt Surg Br 78(5):814–816
Shenoy PM, Kim DH, Wang KH et al (2009) Calcific tendinitis of popliteus tendon: arthroscopic excision and biopsy. Orthopedics 32(2):127
Singh JR, Yip K (2015) Gluteus maximus calcific tendonosis: a rare cause of sciatic pain. Am J Phys Med Rehabil 94(2):165–167
Stark P, Hildebrandt-Stark HE (1983) Calcific tendinitis of the piriform muscle. ROFO Fortschr Geb Rontgenstr Nuklearmed 138(1):111–112
Tamangani J, Davies AM, James SLJ et al (2009) Calcific tendonitis of the adductor brevis insertion. Clin Radiol 64(9):940–943
Thomason HC, Bos GD, Renner JB (2001) Calcifying tendinitis of the gluteus maximus. Am J Orthop Belle Mead NJ 30(10):757–758
Thornton MJ, Harries SR, Hughes PM et al (1998) Calcific tendinitis of the gluteus maximus tendon with abnormalities of cortical bone. Clin Radiol 53(4):296–301
Tibrewal SB (2002) Acute calcific tendinitis of the popliteus tendon–an unusual site and clinical syndrome. Ann R Coll Surg Engl 84(5):338–341
Tomlinson MP, Williams LA (2006) Extensor hallucis longus calcific tendonitis: a case report. Foot Ankle Int 27(2):144–145
Trujeque L, Spohn P, Bankhurst A et al (1977) Patellar whiskers and acute calcific quadriceps tendinitis in a general hospital population. Arthritis Rheum 20(7):1409–1412
Van Damme K, De Coster L, Mermuys K et al (2017) Bone scan findings in calcific tendinitis at the gluteus maximus insertion: some illustrative cases. Radiol Case Rep 12(1):168–174
Varghese B, Radcliffe GS (2006) Groves C Calcific tendonitis of the quadriceps. Br J Sports Med 40(7):652 (Discussion 654)
Watanabe H, Sano K, Shinozaki T et al (1998) Calcific tendinitis in the posterior proximal thigh as a self-limited condition: pathogenic role of inflammatory responses. J Rheumatol 25(5):970–974
Wepfer JF, Reed JG, Cullen GM et al (1983) Calcific tendinitis of the gluteus maximus tendon (gluteus maximus tendinitis). Skeletal Radiol 9(3):198–200
Williams AA, Stang TS, Fritz J et al (2016) Calcific tendinitis of the gluteus maximus in a golfer. Orthopedics 39(5):e997–e1000
Yang I, Hayes CW, Biermann JS (2002) Calcific tendinitis of the gluteus medius tendon with bone marrow edema mimicking metastatic disease. Skeletal Radiol 31(6):359–361
Yang J-H, Oh K-J (2013) Endoscopic treatment of calcific tendinitis of the rectus femoris in a patient with intractable pain. J Orthop Sci Off J Jpn Orthop Assoc 18(6):1046–1049
Yi SR, Lee MH, Yang BK et al (2015) Characterizing the progression of varying types of calcific tendinitis around hip. Hip Pelvis 27(4):265–272
Yun HH, Park JH, Park JW et al (2009) Calcific tendinitis of the rectus femoris. Orthopedics 32(7):490
Zajonz D, Moche M, Tiepold S et al (2013) Acute hip pseudoparalysis with calcific tendinitis at the insertion of the psoas muscle. Case report and first description of an atypical location. Z Rheumatol 72(2):178–183
Zini R, Panascì M, Papalia R et al (2014) Rectus femoris tendon calcification: arthroscopic excision in 6 top amateur athletes. Orthop J Sports Med 2(12):2325967114561585
Precerutti M, Garioni E, Madonia L et al (2010) US anatomy of the shoulder: pictorial essay. J Ultrasound 13(4):179–187
Normal Sonographic Anatomy of the Wrist With Emphasis on Assessment of Tendons, Nerves, and Ligaments—Gitto—2016–Journal of Ultrasound in Medicine–Wiley Online Library [Internet]. [cited 2018 Sep 5]. Available from: https://onlinelibrary.wiley.com/doi/full/10.7863/ultra.15.06105. Accessed 5 June 2019
Presazzi A, Bortolotto C, Zacchino M et al (2011) Carpal tunnel: normal anatomy, anatomical variants and ultrasound technique. J Ultrasound 14(1):40–46
Molini L, Precerutti M, Gervasio A et al (2011) Hip: anatomy and US technique. J Ultrasound 14(2):99–108
Cocco G, Draghi F, Schiavone C Ultrasonographic diagnosis and percutaneous treatment of insertional calcific tendinopathy of iliotibial band: case report [Internet]. https://doi.org/10.1594/EURORAD/CASE.15881
Precerutti M, Bonardi M, Ferrozzi G et al (2014) Sonographic anatomy of the ankle. J Ultrasound 17(2):79–87
Vampertzis T, Agathangelidis F, Gkouliopoulou E, Papastergiou S (2016) Massive non-traumatic calcification of the medial collateral ligament of the knee. BMJ Case Rep. https://doi.org/10.1136/bcr-2016-217743
Jang EC, Lee HJ, Kim SH, Kwak YH (2017) Arthroscopic treatment of symptomatic calcific periarthritis on the medial side of the knee after posterior cruciate ligament reconstruction: case report and literature review. Acta Orthop Traumatol Turc 51(6):495–498
Hayashi H, Fischer H (2016) Incidental anterior cruciate ligament calcification: case report. J Radiol Case Rep. 10(3):20–27
Koukoulias NE, Papastergiou SE (2011) Isolated posterior cruciate ligament calcification. BMJ Case Rep. https://doi.org/10.1136/bcr.10.2011.4916
Mader R, Novofastovski I, Iervolino S et al (2015) Ultrasonography of peripheral entheses in the diagnosis and understanding of diffuse idiopathic skeletal hyperostosis (DISH). Rheumatol Int 35:493–497
Kim Y-S, Lee H-J, Kim Y et al (2014) Which method is more effective in treatment of calcific tendinitis in the shoulder? Prospective randomized comparison between ultrasound-guided needling and extracorporeal shock wave therapy. J Shoulder Elbow Surg 23(11):1640–1646
del Cura JL, Torre I, Zabala R et al (2007) Sonographically guided percutaneous needle lavage in calcific tendinitis of the shoulder: short- and long-term results. AJR Am J Roentgenol 189(3):W128–W134
De Zordo T, Ahmad N, Ødegaard F et al (1980) US-guided therapy of calcific tendinopathy: clinical and radiological outcome assessment in shoulder and non-shoulder tendons. Ultraschall Med Stuttg Ger 2011(32 Suppl 1):S117–S123
de Witte PB, Selten JW, Navas A et al (2013) Calcific tendinitis of the rotator cuff: a randomized controlled trial of ultrasound-guided needling and lavage versus subacromial corticosteroids. Am J Sports Med 41(7):1665–1673
Serafini G, Sconfienza LM, Lacelli F et al (2009) Rotator cuff calcific tendonitis: short-term and 10-year outcomes after two-needle us-guided percutaneous treatment–nonrandomized controlled trial. Radiology 252(1):157–164
Sconfienza LM, Albano D, Messina C et al (2018) How, when, why in magnetic resonance arthrography: an international survey by the european society of musculoskeletal radiology (ESSR). Eur Radiol 28(6):2356–2368
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C.B. is a consultant for Bracco Imaging and Doc. Congress; the other authors have nothing to disclose.
Ethical standards
Exams have been performed in accordance with the ethical standards laid down in the Helsinki Declaration of 1975 and its late amendments. Additional informed consent was obtained from all patients for whom identifying information was not included in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Draghi, F., Cocco, G., Lomoro, P. et al. Non-rotator cuff calcific tendinopathy: ultrasonographic diagnosis and treatment. J Ultrasound 23, 301–315 (2020). https://doi.org/10.1007/s40477-019-00393-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-019-00393-2