Abstract
Purpose of Review
Mycobacterial infections may affect any human organ and produce disseminated disease in immunocompromised individuals. Their most common clinical presentations include pulmonary, cutaneous (skin and soft tissues), and disseminated forms. The skin and soft tissues are frequent targets of affection by mycobacterial pathogens manifesting as localized or diffuse disease.
Recent Findings
Overall, infections due to Mycobacterium leprae, Mycobacterium ulcerans, and Mycobacterium tuberculosis are the most frequently recognized mycobacterial pathogens involving the skin and soft tissues. Additionally, all mycobacterial species of the nontuberculous group may also produce cutaneous disease. Of these, the most commonly identified organisms causing localized infections of the skin and subcutaneous tissues are the rapidly growing species (Mycobacterium fortuitum, Mycobacterium chelonae, and Mycobacterium abscessus complex), Mycobacterium marinum, and M. ulcerans. Since the skin and soft tissues are important protective barriers for environmental pathogens, their disruption often represents the portal of entry of nontuberculous environmental mycobacteria (soil, natural water systems, engineered water networks, etc.). Additionally, some mycobacterial diseases affecting cutaneous structures occur after exposure to infected animals or their products (i.e., Mycobacterium bovis). Mycobacterial infections of the skin and soft tissues may manifest with a broad range of clinical phenotypes such as cellulitis, single or multiple abscesses, subacute or chronic nodular lesions, macules, superficial lymphadenitis, plaques, nonhealing ulcers, necrotic plaques, verrucous lesions, and many other dermatologic manifestations.
Summary
Geography and environmental exposure play an important role in the epidemiology of cutaneous mycobacterial infections. Mycobacterial infection of the skin and subcutaneous tissue is an important cause of human suffering in terms of morbidity, deformity, dysfunction, and stigma. The diagnosis of cutaneous mycobacterial infections is challenging requiring a low threshold of clinical suspicion for obtaining skin biopsies of cutaneous lesions for acid-fast staining and cultures, and molecular probe assays to detect the presence of mycobacterial pathogens. The choice of antibacterial therapy combinations and length of therapy for cutaneous mycobacterial infections is species-specific.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The family Mycobacteriaceae belongs to the order Actinomyetales and the phylum Actinobacteria [1•]. To date, there are more than 150 mycobacterial species identified with the availability of modern molecular techniques including the 16s ribosomal DNA sequencing, polymerase chain reaction (PCR) analysis employing restriction length polymorphisms, and high-performance liquid chromatography [2••]. Most mycobacterial species are harmless saprophytes often found in soils or aquatic environments [1•]. However, many mycobacterial species evolved to cause animal and human disease from a plethora of ecological matrixes (soils, natural water reservoirs, or engineered water systems) [3]. In other cases, human infections represent zoonosis such as in the case of Mycobacterium bovis [4,5,6] or Mycobacterium leprae [7,8,9], or infection occurs through the person-to-person transmission route such as in the case of Mycobacterium tuberculosis [5, 6]. Mycobacterial infections may affect any organ of the human host, but most common sites of involvement include pulmonary, cutaneous (skin and soft tissues including superficial lymphadenitis), and disseminated clinical forms [10••, 11••].
Skin and soft tissue infections caused by nontuberculous mycobacteria groups (NTMs) are usually the result of direct inoculation of these pathogens linked to specific environmental exposures [10••, 11••]. Cutaneous mycobacterial infections are emerging diseases of increasing medical concern because of cohabitation of environmental habitats with mycobacteria [10••]. Indeed, humans venture with increasing frequency into habitats where environmental mycobacteria are highly prevalent [12]. For example, growing human incursion into aquatic environments has been frequently associated with infection caused by Mycobacterium marinum, Mycobacterium ulcerans, and Mycobacterium haemophilum [13,14,15]. Cutaneous mycobacterial infections are also transmitted in the hospital setting through contaminated medical products, indwelling catheters, and surgical procedures [11••, 16]. There is also evidence that nontuberculous mycobacteria are emerging pathogens among immunosuppressed hosts such as those with HIV/AIDS or among those receiving immunosuppressive therapies including biological therapies for immune-mediated inflammatory disease, solid organ transplantation, hematologic malignancies, and hematopoietic stem cell or solid organ transplantation [17].
Clinical Manifestations of Cutaneous Mycobacterial Infections
Mycobacterial infections of the skin and subcutaneous tissues are important causes of human disease. M. leprae, M. ulcerans, and M. tuberculosis are the most frequently recognized mycobacterial pathogens causing diseases involving the skin and soft tissues. Additionally, all environmental mycobacterial species of the nontuberculous group may also produce cutaneous disease. They may manifest as localized or disseminated forms and the spectrum of clinical manifestations ranges from nodules, plaques, sporotrichoid lesions, chronic nonhealing ulcers, single or multiple abscesses, chronic draining sinuses, superficial lymphadenitis (scrofula), and cellulitis (Table 1) [11••]. Local spread of cutaneous mycobacterial diseases into deeper tissues may also be associated with tenosynovitis, septic arthritis, and osteomyelitis [10••, 11••]. Leprosy, the prototype of the cutaneous mycobacterial infections, has inflicted incalculable suffering for millennia by causing deforming cutaneous lesions and peripheral nerve damage resulting in neurologic dysfunction, deformity, and limb loss [10••]. Despite major gains in controlling this ancient plague, leprosy remains an important cutaneous mycobacterial infection in many areas of the world [18, 19]. In fact, since 2000, there have been approximately 3 million new cases of leprosy [20]. In susceptible human hosts, M. leprae may produce a broad spectrum of clinical phenotypes with different degrees of clinical severity and risk of leprosy reactions (Table 1). Similarly, the wide range of clinical forms of cutaneous tuberculosis depends on the mode of acquisition of the infection (exogenous versus endogenous spread), host immune status, and history of previous exposure to the tuberculous bacilli [21••]. Tuberculosis of the skin and soft tissues represents only 1–2% of all combined clinical forms of pulmonary and extrapulmonary tuberculosis [21••]. Infection due to M. ulcerans produces a cutaneous infection that ranges from a localized painless nodule or ulceration to diffuse cutaneous ulcerative or non-ulcerative forms with bone involvement [22, 23]. The disease is termed Buruli ulcer or Bairnsdale ulcer. In 2015, more than 2000 cases were reported to the World Health Organization with most cases reported in Africa. Individuals may acquire M. ulcerans infection through mild skin injuries and subsequent exposure to contaminated water or soils leading to the entry of M. ulcerans into the subcutaneous tissue, or insect vectors may play a role in its transmission [22, 23]. The disease is produced by the production of a potent macrolide toxin, mycolatone which is capable of subcutaneous tissue destruction, modulate pain locally, and that is immunosuppressive [22, 23]. Buruli ulcer is an important neglected tropical disease that can produce important physical impairment, functional sequelae, deformity, and dysfunction [24].
The NTM constitutes mycobacterial species other than those causing tuberculosis, leprosy, and Buruli ulcer and includes two major groups defined by their ability to grow in solid culture media (rapid or slow growers) [25•]. In the USA and other countries, recent reports have suggested that the prevalence of nontuberculous mycobacteria disease is increasing especially among older adults [26]. The NTM pulmonary diseases in patients with chronic pulmonary diseases are those with bronchiectasis, chronic obstructive pulmonary disease, cystic fibrosis, and others, or those with some degree of esophageal dysfunction or gastroesophageal reflux disease, and disseminated disease in immunocompromised hosts [27]. Additionally, NTMs may cause skin and soft tissue infections after trauma or surgery, or as part of disseminated forms of the disease [10••, 11••]. Of the NTMs, the rapidly growing mycobacteria Mycobacterium fortuitum, Mycobacterium chelonae, and Mycobacterium abscessus complex frequently manifest as skin and soft tissue infections (Table 1).
Diagnosis of Cutaneous Mycobacterial Infections
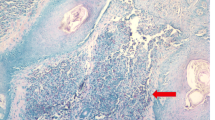
Diagnosing mycobacterial infections of the skin and soft tissues is challenging due to the broad spectrum of clinical manifestations and non-specific histopathologic findings on tissue biopsy. Nonetheless, assessing skin biopsy specimens for acid-fast bacilli staining and mycobacterial cultures or from draining material is crucial in order to confirm the diagnosis of cutaneous mycobacterial infections. Mycobacteria may be identified on direct smear and tissue or recovered in Lowenstein-Jensen agar, BACTEC broth, and Middlebrook 7H10 agar [2••]. Some mycobacterial species have specific growth requirement such as M. haemophilum, which requires iron or hemin supplementation and incubation at 30 °C. Additionally, molecular detection methods including direct probe or sequencing can detect mycobacterial species may assist in confirming the diagnosis. Modern molecular techniques such as the16s ribosomal DNA sequencing, polymerase chain reaction (PCR) analysis employing restriction length polymorphisms, and high-performance liquid chromatography aid in defining the specific mycobacterial species involved in skin and soft tissue infections [2••]. The diagnosis of leprosy is a clinical diagnosis based on characteristic plaques, macules, or nodules associated with sensory loss (hypoesthesia or anesthesia), thickened peripheral nerves. Biopsy confirmation of a skin lesion demonstrates acid-fast bacilli (Fite-Faraco staining) inside peripheral nerves (endoneurium). Buruli ulcer is often diagnosed based on the presence of characteristic nodules or ulcers, ecological risk factors, and at risk age groups (often identified in individuals younger than 15 years) residing in endemic settings. M. ulcerans requires a temperature between 29 and 33 °C and a low-oxygen concentration (2.5%). Due to these limitations, molecular techniques such as qPCR are preferred for confirming a diagnosis of M. ulcerans, and point-of-care testing is underdevelopment [2••].
Performing susceptibility testing of mycobacterial isolates is important to decide on optimal antimycobacterial therapies since the MIC to specific antimicrobials correlate clinically with in vivo response to therapy (i.e., rifampin in the case of Mycobacterium kansasii). M. marinum requires microdilution broth MIC at 30 °C as the preferred susceptibility method. It is recommended that rapidly growing mycobacteria be tested against selected antibacterial drugs such as clarithromycin, cefoxitin, imipenem, amikacin, tobramycin (in the case of M. chelonae), fluoroquinolones, and others [10••]. Since M. leprae is not cultivable, susceptibility testing for M. leprae requires assessments of genetic markers of resistance [28].
Treatment of Cutaneous Mycobacterial Infections
The choice of antibacterial therapy and length of treatment for cutaneous mycobacterial infections is species-specific. Antimycobacterial therapy of M. leprae involves the use of multidrug therapy with a combination of dapsone, rifampin, and clofazimine with length of therapy depending on the clinical staging of the disease. Treatment of cutaneous tuberculosis follows the treatment guidelines for extrapulmonary disease with standard multidrug therapy with length of treatment depending upon the type of cutaneous tuberculosis. Antimycobacterial treatment of M. ulcerans is effective in early limited disease with an 8 week combination of streptomycin, rifampin, and clarithromycin [24].The most frequently encountered members of the rapidly growing mycobacteria group (M. abscessus complex, M. fortuitum, or M. chelonae) are intrinsically resistant to antituberculosis drugs such as isoniazid, rifampin, and ethambutol. The treatment of RGM is species-specific often requiring multidrug therapy with agents such as imipenem, cefoxitin, doxycycline, trimethoprim-sulfamethoxazole, amikacin or tobramycin, linezolid, fluoroquinolones, and other agents [10••, 11••]. M. abscessus and M. chelonae are resistant to doxycycline and trimethoprim-sulfamethoxazole [10••]. Some subspecies of M. abscessus and M. fortuitum possess an erm (41) gene (which produces a 23S RNA methylase) confers inducible resistance to macrolides, and therefore this is an important therapeutic consideration in deciding the specific antimycobacterial drug combination [16].
Conclusions
Cutaneous mycobacterial infections are important causes of human suffering and that manifest with localized or diffuse involvement of skin and soft tissues. The mode of acquisition of cutaneous mycobacterial infections differs among mycobacterial species and ranges from specific environmental exposures, zoonotic transmission, or through the person-to-person route. Leprosy remains an important disease in many areas of the world, while cutaneous tuberculosis represents approximately 1–2% of cases of all clinical forms of tuberculosis. In many settings, particularly in some areas in Africa, infection due to M. ulcerans is an important cause of limb deformity and dysfunction. Skin and soft tissue infection caused by many species of the nontuberculous mycobacteria is usually the result of direct inoculation via trauma followed by exposure to natural aquatic environments, manufactured water networks, soils, or in the hospital setting. Disseminated mycobacterial infections spreading from an either a pulmonary foci or through lymphatic spread may also manifest with diffuse or localized cutaneous involvement.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Bottai D, Stinear TP, Supply P, Brosch R. Mycobacterial pathogenomics and evolution. Microbiol Spectr. 2014;2(1) MGM2–0025-2013. https://doi.org/10.1128/microbiolspec.MGM2-0025-2013. This article describes the evolution and pathogenomics of many mycobacterial species.
•• Forbes BY, Hall GS, Miller MB, Sm N, Rowlinson MC, Salfinger M, et al. Practice guidelines for clinical microbiology laboratories: mycobacteria. Clin Microbiol Rev. 2018;31(2):e00038–17. In-depth discussion of microbiological techniques that assist clinicians in caring for individuals with cutaneous mycobacterial infections.
Falkinham JO. Surrounded by mycobacteria: nontuberculous mycobacteria in the human environment. J Appl Microbiol. 2009;107:356–67.
Behr MA. Mycobacterium du jour: what’s on tomorrow’s menu? Microbes Infect. 2008;10:968–72.
Behr MA, Gordon SV. Why doesn’t Mycobacterium tuberculosis spread in animals? Trends Microbiol. 2015;23(1):1–2.
Mostowy S, Behr MA. The origin and evolution of Mycobacterium tuberculosis. Clin Chest Med. 2005;26:207–16.
Avanzi C, Del-Pozo J, Benjak A, Stevenson K, Sipson VR, Busso P, et al. Red squirrels in the British Isles are infected with leprosy bacilli. Science. 2016;354(6313):744–474.
Balamayooran G, Pena M, Sharma R, Truman RW. The armadillo as an animal model and reservoir host for Mycobacterium leprae. Clin Dermatol. 2015;33:108–15.
Franco-Paredes C, Rodriguez-Morales AJ. Unsolved matters in leprosy: a descriptive review and call for further research. Ann Clin Microbiol Antimicrob. 2016;15:33.
•• Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175:367–416. This is the most important clinical guidelines for the diagnosis and management of non-tuberculous mycobacteria.
•• Wang SH, Pancholi P. Mycobacterial skin and soft tissue infection. Curr Infect Dis Rep. 2014;16:438. https://doi.org/10.1007/s11908-014-0438-5. This is an important publication that summarizes the clinical spectrum of disease caused by mycobacterial infections of the skin and soft tissues.
Falkinham JO 3rd. Environmental sources of nontuberculous mycobacteria. Clin Chest Med. 2015;36:35–41.
Merritt RW, Walker ED, Small PLC, Wallace JR, Johnson PDR, Benbow ME, et al. Ecology and transmission of Buruli ulcer disease: a systematic review. PLoS Negl Trop Dis. 2010;4(12):e911.
Marsollier L, Stinear T, Aubry J, Saint Andre JP, Robert R, Legras P, et al. Aquatic plants stimulate the growth of and biofilm formation by Mycobacterium ulcerans in axenic culture and harbor these bacteria in the environment. Appl Environ Microbiol. 2004;70(2):1097–103.
Smith S, Taylor GD, Fanning EA. Chronic cutaneous Mycobacterium haemophilum infection acquired from coral injury. Clin Infect Dis. 2003;37(7):e100–1.
Mougari F, Guglielmetti L, Raskine L, Sermet-Gaudelus I, Veziris N, Cambau E. Infections caused by Mycobacterium abscessus: epidemiology, diagnostic tools and treatment. Expert Rev Anti-Infect Ther. 2016;14(120):1139–54.
Henkle E, Winthrop KL. Nontuberculous mycobacteria infections in immunosuppressed hosts. Clin Chest Med. 2015;36:91–6.
Smith WC, van Brakel W, Gillis T, Saunderson P, Richardus JH. The missing millions: a threat to the elimination of leprosy. PLoS Negl Trop Dis. 2015;9(4):e0003658.
Stone AC, Wilbur AK, Buikstra JE, Roberts CA. Tuberculosis and leprosy in perspective. Am J Phys Anthropol. 2009;52:66–94.
White C, Franco-Paredes C. Leprosy in the 21st century. Clin Microbiol Rev. 2015;28(1):80–94.
•• Scollard DM, Dacso MM, Abad-Venida ML. Tuberculosis and leprosy: classical granulomatous diseases in the twenty-first century. Dermatol Clin. 2015;33:541–62. Provides important clinical information on the diagnosis and management of leprosy and cutaneous tuberculosis.
Röltgen K, Stinear TP, Pluschke G. The genome, evolution and diversity of Mycobacterium ulcerans. Infect Genet Evol. 2012;12(3):522–9.
Doig KD, Holt KE, Fyfe JAM, Lavender CJ, Eddyani M, Portaels F, et al. On the origin of Mycobacterium ulcerans, the causative agent of Buruli ulcer. BMC Genomics. 2012;13:258.
Nienhuis WA, Stienstra Y, Thompson WA, Awuah PC, Abass MK, Tuah W, et al. Antimycobacterial treatment for early, limited Mycobacterium ulcerans infection: a randomized controlled trial. Lancet. 2010;37:664–72.
• Brown-Elliott BA, Wallace RJ Jr. Clinical and taxonomic status of pathogenic non-pigmented or late-pigmenting rapidly growing mycobacteria. Clin Microbiol Rev. 2002;15(4):716–46. This article reports the clinical and taxonomic status of non-tuberculous mycobacteria.
Adjemian J, Olivier KN, Seitz AE, Holland SM, Prevots DR. Prevalence of nontuberculous mycobacterial lung disease in U.S. Medicare beneficiaries. Am J Respir Crit Care Med. 2012;185(8):881–6.
Wu U, Holland SM. Host susceptibility to non-tuberculous mycobacterial infections. Lancet Infect Dis. 2015;15:968–80.
Williams DL, Gillis TP. Drug-resistant leprosy: monitoring and current status. Lepr Rev. 2012;83(3):269–81.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Cutaneous Mycobacterial Diseases of the Skin and Soft Tissues
Rights and permissions
About this article
Cite this article
Franco-Paredes, C., Chastain, D.B., Allen, L. et al. Overview of Cutaneous Mycobacterial Infections. Curr Trop Med Rep 5, 228–232 (2018). https://doi.org/10.1007/s40475-018-0161-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40475-018-0161-7