Abstract
Purpose of Review
Leptospirosis is a zoonotic disease caused by pathogenic spirochetes of the genus Leptospira. In Central America, Leptospira is endemic, and almost all countries experience frequent outbreaks. Diagnosis of leptospirosis is primarily based on serology. More technologically advanced methods, such as polymerase chain reaction (PCR), are used in only a few laboratories, although it can identify genes specific to pathogenic species. New techniques, such as isothermal reactions and molecular typing could also contribute to disease surveillance in humans, animals, and the environment.
Recent Findings
Advanced techniques, including molecular characterization methods, have been used only rarely up until now. In Nicaragua, we have used phenotypic analysis to characterize pathogenic Leptospira species and multiple locus sequence typing (MLST) to facilitate the identification of a completely new serovar in Costa Rica.
Summary
Improved technology and expertise for molecular typing of Leptospira are needed in order to improve surveillance and provide the basis for epidemiologic studies. Current MLST characterization schemes include representative strains known to be circulating in Central America, and a more widespread implementation of this technique could enrich information about the epidemiology of Leptospira and enable identification of novel strains emerging in the region.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Leptospirosis is considered to be one of the most widespread zoonoses, and it is a serious public health problem throughout the world. The disease is caused by pathogenic spirochetes of the genus Leptospira. It typically affects the most vulnerable populations, is mainly associated with poverty and flooding, and primarily occurs in tropical countries [1•].
In Central America, one of the most vulnerable regions in the Americas for natural disasters, outbreaks of leptospirosis have been reported in almost all countries [2,3,4]. One study, in which the local Ministries of Health compared data to the published literature, found that Costa Rica and Nicaragua ranked 5th and 12th, respectively, in relation to the highest incidence of leptospirosis in the world [5]. Although efforts have been made in recent years to increase awareness of and knowledge about the disease in these countries, it is doubtful this is responsible for the high incidence these authors found in the region, since underreporting is a handicap to all surveillance systems in developing countries like those in Central America.
In Nicaragua, human leptospirosis was recorded for the first time in 1995, with significant outbreaks in that year, as well as in 1998 and 2007 [4, 6•, 7]. Although there have been fatal cases of pulmonary hemorrhage in the late stage of the disease, generally the case fatality rate is low [8]. In Nicaragua, as in other countries of Central America, leptospirosis has an endemic nature and is observed in all regions—urban, suburban, and rural areas. The majority of cases are associated with intense rains, with an average of two cases reported weekly in the rainy season (October and November). However, in hyper-endemic areas, such as the western region, as many as eight cases per week are reported during the frequent epidemic events [1•].
The difficulties that surround making a specific clinical diagnosis, combined with a lack of diagnostic laboratory resources in most low- and middle-income countries, result in an underestimation of disease in sites where leptospirosis has the biggest impact. In Central America, as in the rest of the world, the gold standard for leptospirosis diagnosis is the microscopic agglutination technique (MAT), but disadvantages of the test limit absolute reliance on it. Real-time polymerase chain reaction (PCR) is analytically superior, but lack of equipment and expertise on the technique in laboratories with limited resources has led to the design of isothermal PCR reactions (loop mediated isothermal amplification [LAMP]), a diagnostic technique that has been successfully used for human, animal, and environmental samples. LAMP, however, does not accomplish molecular characterization, which is still necessary for specific identification. Here, we detail the laboratory methods, their strengths and weaknesses, and provide examples of their direct application in a real-world setting.
Phenotypic and Serological Classification
The genus Leptospira contains two phenotypically derived species; their classification is based on the antigenicity of their lipopolysaccharide (LPS) molecules. These species are (1) L. interrogans (sensu lato), the group of pathogenic Leptospira, and (2) L. biflexa (sensu lato), which are free-living leptospires present mainly in water and are neither associated with human or animal infections nor virulent in laboratory-infected animals. Both L. interrogans and L. biflexa are classified further into serogroups, according to their serological characteristics. More than 60 serovars of L. biflexa are known, and L. interrogans includes more than 200 serovars; more serovars have been isolated, but remain to be published and verified. Serovars that are antigenically related to each other are traditionally grouped into larger serogroups. However, neither serovar nor serogroup are taxonomic classifications in the sense of phylogenetic determination [9•].
The distinction between serovars is essential to understand the epidemiology of Leptospira, but in most cases, distinction relies on the availability of monoclonal antibodies to identify the serovar quickly and is only possible after first succeeding in isolating and purifying the bacteria. For example, in Nicaragua, the phenotypes of clinical isolates have been characterized following growth tests at 13 ° C, growth in medium supplemented with 8-azaguanine, conversion to spherical forms in 1 M NaCl, with the result that 8 of the analyzed isolates were classified as pathogenic species [10].
Genotypic Classification
Within the Leptospiraceae family, phylum Spirochaetes, Leptospira consists of a unique genus, which is very heterogeneous and divided into different subgroups, according to their genetic classification. Reference strains are available from the World Health Organization (WHO) Collaboration Centers in Amsterdam (The Netherlands) and Brisbane (Australia) [11]. There is a discordance between phenotypic and genetic classification systems so that there are species that include both pathogenic and non-pathogenic serovars, and some of them are also included in more than one genetically-determined species. Accordingly, the genetic species is typical of the strain, but no serogroup or serovar predicts the genetic species to which a strain in question belongs [9•, 12].
Microscopic Agglutination (MAT)
MAT is the technique commonly used in reference laboratories and can be used to identify immune response to Leptospira according to serogroup, but it detects only antibodies present in serum, without specificity for infection-induced antibodies (versus vaccine-induced). It also requires maintaining both clean cultures and local specific reference strains [13]. In Nicaragua, MAT is performed only in two laboratories. One laboratory is located within the National Diagnostic and Reference Center (NDRC) and is responsible for the diagnosis of leptospirosis in humans. The other laboratory is in the Veterinary Diagnostic and Research Center (CEVEDI), School of Agrarian and Veterinary Sciences of Universidad Nacional Autónoma de Nicaragua (UNAN-León), the laboratory specializing in the diagnosis of leptospirosis in animals. Both centers form part of the National Commission of Zoonoses and the “Inter-institutional work plan for a comprehensive approach to the prevention and control of leptospirosis” [14]. In Costa Rica, diagnostics are performed at the Laboratory of Leptospirosis Diagnosis of the National Reference Center of Virology and Leptospirosis (CNRVL), in the Costa Rican Institute for Research and Teaching in Nutrition and Health (INCIENSA) [15].
Real-time Polymerase Chain Reaction (qPCR)
Real-time PCR is a more sensitive and specific test for the detection of Leptospira. Besides providing faster results than conventional PCR, qPCR, either using SYBR green or TaqMan technology, allows quantification of bacterial loads by comparing cycle thresholds (CTs) to a standard curve of known bacterial concentrations. However, it has been shown that the quantification of leptospiremia in serum or whole blood does not correlate directly with clinical manifestations in patients [16]. While the specificity of the TaqMan qPCR probes is higher than the one obtained with SYBR green, the analysis of the dissociation curve may reveal additional information, such as differentiating L. interrogans from other species [17].
Despite the advantages of qPCR, the technique must be carefully standardized because of several considerations in its applicability. For example, the diagnostic and analytical sensitivity depends largely on the type of sample and the process of DNA extraction; in part, it is due to potential reaction inhibitors present in the sample. Another important factor is proper design of the primers, which in most cases are not capable of binding to target genes of different serovars with the same affinity. Therefore, a detailed analysis of the target gene sequences of the circulating and suspected strains is necessary for the design of probes and primers that yield the highest sensitivity.
It is most appropriate to design primers that detect the largest possible number of serovars, mainly aimed at the species known to be present in the region, with contextual knowledge of the specific geographical area of interest. Some studies have evaluated the usefulness of different qPCR protocols for detection of Leptospira in cultures, blood, plasma, and serum samples. Table 1 details some PCR parameters that have been developed for the diagnosis of leptospirosis. One finding is that the SYBR green amplification targeting the SecY gene detects the L. interrogans species with good analytical sensitivity, but is not able to amplify the same gene in L. borgpetersenii [21].
Loop-Mediated Isothermal Amplification (LAMP)
LAMP is a technique, designed and described in the year 2000, to amplify thousands of copies of DNA (up to 109 times) in 1 h under isothermal conditions (between 60 and 65 °C), due to the capacity of the Bst polymerase enzyme of DNA. Four primers are designed to recognize 6 different sequences in the DNA to be studied (Fig. 1): an internal forward primer (FIP), an internal reverse primer (BIP), an external forward primer (F3), and an external reverse primer (B3). In the cases of FIP and BIP, each is formed by two sequences with different sense, a sequence of nucleotides 5′ 3′ (sense, F2 or B2) and another 3′ 5′ (antisense, F1 or B1), in two proximal regions in the template DNA, such that the F2 region of the IFP binds to the complementary sequence of template DNA (F2C) and the enzyme synthesizes the remainder of the complementary strand, including the F1 complementary region (F1C). Subsequently, F3 binds to the template DNA in the area outside the FIP, releasing the amplification product and allowing F1 to bind to F1C, previously synthesized. The same process occurs with BIP and B3 at the other end so that successive cycles give rise to the formation of loops of different sizes that can be visualized in 2% agarose gel or using other development techniques [26]. A variant has been developed that incorporates two more primers, called forward loop (FL) and backward loop (BL) that accelerate the reaction of the LAMP [27].
Although amplification has proved to be efficient in LAMP, it remains necessary to improve on these techniques. For example, the electrophoresis procedure requires specific equipment, and elimination of this element has been studied using systems of direct development, such as turbidimetry with magnesium sulfate (MgSO4), which forms a visible precipitate when it reacts with the pyrophosphate that is released by dNTPs during DNA polymerization [28, 29]. However, turbidity is not an entirely stable property, and calcium chloride (CaCl2) could be used in order to lend greater stability [30]. Colorimetric techniques, such as with hydroxynaphthol blue (HNB) have also been tested as a pH indicator in monitoring the concentration of Mg2+, providing a violet color in positive samples and light blue in negative samples [31]. Calcein is a molecule that is bound to Mg2+ and inhibits fluorescence, producing an orange color during the reaction. In the amplification of the LAMP, the Mg2+ is released for the formation of pyrophosphates recovering the fluorescence, and the residual Mg2 + ions bind to the calcein, increasing fluorescence [24]. Other fluorophores, such as SYBR green I [32], Quant-iT PicoGreen [33], and GeneFinder TM [34] have also been tested.
The two essential advantages of LAMP, compared to conventional and real-time PCR, are that sensitivity is not affected by the presence of non-specific DNA and there is less inhibition by factors in the sample [35]. Furthermore, the use of 4 primers to recognize 6 sequences in the template DNA provides high specificity [27]. These advantages are important because the technique can be used in developing countries, which are largely affected by leptospirosis and which typically do not have thermocyclers or other equipment necessary for a conventional PCR, let alone for qPCR. In addition, it is a technique that requires little training and, in the case of the Central America, could be utilized by various laboratories for decentralized diagnosis and surveillance of both human and animal disease in endemic regions.
Molecular characterization
Insertion Sequences (SI)
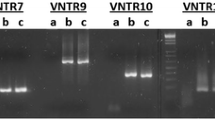
Bacterial typing is of immense value for epidemiological studies. Insertion sequences can be used to accomplish this, and in Leptospira, three different types of IS are described: 1500, 1502, and 1533 [36]. The number of copies of SI varies between the different serovars and also between isolates of a given serogroup. In a study by Zuerner and Bolin, a typing method was developed for L. interrogans (sensu stricto) using SI1500, which was applied to identify and characterize strains isolated from a specific region of Nicaragua. Hybridization analysis showed that SI1500 was present in polymorphic fragments and that differences in these patterns could be used for serovars identification [37]. Interestingly, another element, the SI1502, was undetectable in some strains, suggesting its recent introduction into the genus Leptospira [38]. This method of typing is simple and easy to implement in laboratories, and it is useful for the correct identification of strains, making it ideal for epidemiological studies. However, interpretation of the results can be difficult and requires some expertise, since a correct reading of molecular weight must be done in order to ascertain the number of repeats that are the product of amplification [39].
Multi-Locus Sequencing Typing (MLST)
MLST is promising for the characterization of Leptospira and is easy to standardize because of widely available internet databases (http://leptospira.mlst.net/) and ensure a uniform nomenclature. This technique offers an unambiguous procedure for characterizing isolates of bacterial species using the sequence of 7 internal fragments of conserved regions of approximately 450–650 base pairs (bp). Differences in the sequences within each locus are designated as alleles, and each isolated allele at each locus define the allelic profile or sequence type (ST). Each species is characterized by corresponding numbers of the alleles of the 7 loci with conserved regions [40, 41]. It has been observed that the sequence of a single gene or locus is not sufficient to identify among the more than 200 pathogenic serovars, but MLST provides a way to accomplish this.
The sequences of the loci have different numbers of alleles, differing by a single nucleotide or several different nucleotides (since a simple genetic change can result in a new allele, either by a point mutation or by replacement). Characterizing the differences in the number of nucleotides between the alleles, one can infer which alleles differ most from the original allele in spite of mutations over time. Most bacterial species exhibit sufficient variations in their genes, with conserved regions, to provide many alleles per locus, thus allowing billions of allelic profiles using 7 loci. For example, an average of 30 alleles per locus enables a resolution of 20 billion genotypes [42]. Currently, three schemes of MLST, using different loci, are recognized [41,42,43]. The scheme presented in 2006 includes strains from Central America (2 from Nicaragua, 3 from Panama, and 10 from Costa Rica), and the possibility of a new serovar was identified in Costa Rica [41], later confirmed as novel and named “Arenal” [44].
This sequencing technique has gained attention for its usefulness, and several formats have been described, which utilize different loci. One of the most widely used is that described by Boonsilp et al., in 2013 [42], which is a modification of the one designed in 2007 by Thaipadungpanit et al. [45]. There is even a website with sequences of for the 7 recommended loci for 7 pathogenic Leptospira species, which facilitates the comparison of isolates with 327 strains obtained in different parts of the world, including Nicaragua. In a study carried out by the team in Nicaragua, applying the scheme recommended by Boonsilp et al., difficulties were encountered with sequencing products, most likely due to poor DNA quality. Importantly, this has been reported by other authors who found that at least 4.9 × 104 Leptospira/ml were required to obtain good products using MLST [46]. As an alternative, simpler schemes, such as the one proposed by Merien [18] and the one by Perez [47], have proved yield good results.
The current MLST database contains information on more than 300 isolates belonging to 7 species of pathogenic Leptospira, including L. interrogans, L. borgpetersenii, L. kirschneri, L. weilii, L. santarosai, L. nogouchii, and L. alexanderi. The rapid increase in utilization and reduction of costs of nucleotide sequence determination, together with the development and availability of the databases, leads to a projection of high application of this technique. However, in some countries, particularly in Central America, it is still difficult to register with sequencing services, and sample shipments to other countries are prohibitively expensive.
Conclusion
Leptospirosis in Central America is a serious problem, with outbreaks occurring in practically all countries in the region. High incidence rates are reported throughout the region, although accurate rates are likely to be even higher, since lack of availability and resources for laboratory diagnosis is a major cause of underreporting. The gold standard test for leptospirosis diagnosis is MAT, which may detect antibodies in serum, cannot detect pathogen directly or be used on other sample types, and in reality is carried out only in a few laboratories. The implementation of molecular tests that allow a more accurate identification of specific types and also permit detection in a diversity of sample types—such as urine from animal carriers and environmental specimens like river samples—is essential for adequate surveillance and identification of important maintenance reservoirs. Ultimately, this will guide disease prevention.
Due to antigenic and genetic complexity of Leptospira, it is important to complement diagnosis of disease with characterization of the infecting strain by molecular techniques in order to understand its epidemiology. By applying these new, molecular techniques as a means of classification, Leptospira isolated from clinical samples have been phenotypically characterized in Nicaragua, and a completely novel serovar was even identified and described in Costa Rica. In spite of this, the technology remains scarce and only a few studies have been done for the molecular characterization of Leptospira circulating in Central America. Good alternatives, such as MLST, a standardized technique that produces internationally comparable results and already has proved to be the most useful method for epidemiologic studies in recent years, remain a possibility for the future.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Schneider MC, Nájera P, Aldighieri S, et al. Leptospirosis outbreaks in Nicaragua: identifying critical areas and exploring drivers for evidence-based planning. Int J Environ Res Public Health. 2012;9:3883–910. This is a complete epidemiological study, carried out in Nicaragua with data obtained from the health system and other institutions of the country.
Naranjo M, Suárez M, Fernández C, Amador N, González M, Batista N, et al. Study of a leptospirosis outbreak in Honduras following hurricane Mitch and prophylactic protection of the vax-SPIRAL® vaccine. MEDICC Rev. 2008;10:38–42.
Centers for Disease Control and Prevention (CDC). Outbreak of leptospirosis among white-water rafters--Costa Rica, 1996. MMWR Morb Mortal Wkly Rep. 1997;46:577–9.
Zaki SR, Shieh WJ. Leptospirosis associated with outbreak of acute febrile illness and pulmonary haemorrhage, Nicaragua, 1995. The Epidemic Working Group at Ministry of Health in Nicaragua. Lancet Lond Engl. 1996;347:535–6.
Pappas G, Papadimitriou P, Siozopoulou V, Christou L, Akritidis N. The globalization of leptospirosis: worldwide incidence trends. Int J Infect Dis. 2008;12:351–7.
Trevejo RT, Rigau-Pérez JG, Ashford DA, et al. Epidemic leptospirosis associated with pulmonary hemorrhage—Nicaragua, 1995. J Infect Dis. 1998;178:1457–63. This is the first study to describe pulmonary hemorrhagic fever in the American continent.
Ashford DA, Kaiser RM, Spiegel RA, Perkins BA, Weyant RS, Bragg SL, et al. Asymptomatic infection and risk factors for leptospirosis in Nicaragua. Am J Trop Med Hyg. 2000;63:249–54.
Costa F, Martinez-Silveira MS, Hagan JE, Hartskeerl RA, dos Reis MG, Ko AI. Surveillance for leptospirosis in the Americas, 1996–2005: a review of data from ministries of health. Rev Panam Salud Publica Pan Am J Public Health. 2012;32:169–77.
Levett PN. Leptospirosis. Clin Microbiol Rev. 2001;14:296–326. A review by one of the most prestigious investigators on the subject of leptospirosis describes the diagnosis and classification of leptopires.
Rosario LA, Arencibia DF, Batista N, Jirón W, Suárez YE, Infante JF. Caracterización de aislamientos clínicos de Leptospira por métodos fenotípicos y moleculares en la República de Nicaragua. VacciMonitor. 2012;21:6–12.
Smythe L, Adler B, Hartskeerl RA, Galloway RL, Turenne CY, Levett PN, et al. Classification of Leptospira genomospecies 1, 3, 4 and 5 as Leptospira alstonii sp. nov., Leptospira vanthielii sp. nov., Leptospira terpstrae sp. nov. and Leptospira yanagawae sp. nov., respectively. Int J Syst Evol Microbiol. 2013;63:1859–62.
Brenner DJ, Kaufmann AF, Sulzer KR, Steigerwalt AG, Rogers FC, Weyant RS. Further determination of DNA relatedness between serogroups and serovars in the family Leptospiraceae with a proposal for Leptospira alexanderi sp. nov. and four new Leptospira genomospecies. Int J Syst Bacteriol. 1999;49(Pt 2):839–58.
Levett PN. Usefulness of serologic analysis as a predictor of the infecting serovar in patients with severe leptospirosis. Clin Infect Dis. 2003;36:447–52.
Ortiz E (2011) Elaboración del Plan de Trabajo Interinstitucional para el abordaje de la Leptospirosis. http://www.paho.org/nic/index.php?option=com_content&view=article&id=335%3Aelaboracin-del-plan-de-trabajo-interinstitucional-para-el-abordaje-de-la-leptospirosis&catid=735%3Aarchivo-de-noticias&Itemid=244. Accessed 1 Dec 2016
Rodríguez-Moreno V, Romero-Zúñiga JJ. Definiciones operativas para la prevención y control de la leptospirosis en Costa Rica Operative Definitions for Prevention and Control of Leptospirosis in Costa Rica. Acta Méd Costarric. 2010;52:232–9.
Agampodi SB, Matthias MA, Moreno AC, Vinetz JM. Utility of quantitative polymerase chain reaction in leptospirosis diagnosis: association of level of leptospiremia and clinical manifestations in Sri Lanka. Clin Infect Dis Off Publ Infect Dis Soc Am. 2012;54:1249–55.
Levett PN, Morey RE, Galloway RL, Turner DE, Steigerwalt AG, Mayer LW. Detection of pathogenic leptospires by real-time quantitative PCR. J Med Microbiol. 2005;54:45–9.
Merien F, Portnoi D, Bourhy P, Charavay F, Berlioz-Arthaud A, Baranton G. A rapid and quantitative method for the detection of Leptospira species in human leptospirosis. FEMS Microbiol Lett. 2005;249:139–47.
Ahmed A, Engelberts MFM, Boer KR, Ahmed N, Hartskeerl RA. Development and validation of a real-time PCR for detection of pathogenic Leptospira species in clinical materials. PLoS ONE. 2009. doi:10.1371/journal.pone.0007093.
Boonsilp S, Thaipadungpanit J, Amornchai P, Wuthiekanun V, Chierakul W, Limmathurotsakul D, et al. Molecular detection and speciation of pathogenic Leptospira spp. in blood from patients with culture-negative leptospirosis. BMC Infect Dis. 2011;11:338.
Bourhy P, Bremont S, Zinini F, Giry C, Picardeau M. Comparison of real-time PCR assays for detection of pathogenic Leptospira spp. in blood and identification of variations in target sequences. J Clin Microbiol. 2011;49:2154–60.
Rawlins J, Portanova A, Zuckerman I, Loftis A, Ceccato P, Willingham AL, et al. Molecular detection of leptospiral DNA in environmental water on St. Kitts. Int J Environ Res Public Health. 2014;11:7953–60.
Xu C, Loftis A, Ahluwalia SK, Gao D, Verma A, Wang C, et al. Diagnosis of canine leptospirosis by a highly sensitive FRET-PCR targeting the lig genes. PLoS ONE. 2014. doi:10.1371/journal.pone.0089507.
Suwancharoe D, Sittiwicheanwong B, Wiratsudakul A. Evaluation of loop-mediated isothermal amplification method (LAMP) for pathogenic Leptospira spp. detection with leptospires isolation and real-time PCR. J Vet Med Sci. 2016;78:1299–302.
Chen H-W, Weissenberger G, Atkins E, Chao C-C, Suputtamongkol Y, Ching W-M. Highly sensitive loop-mediated isothermal amplification for the detection of Leptospira. Int J Bacteriol. 2015;2015:147173.
Notomi T, Okayama H, Masubuchi H, Yonekawa T, Watanabe K, Amino N, et al. Loop-mediated isothermal amplification of DNA. Nucleic Acids Res. 2000;28:E63.
Mori Y, Notomi T. Loop-mediated isothermal amplification (LAMP): a rapid, accurate, and cost-effective diagnostic method for infectious diseases. J Infect Chemother Off J Jpn Soc Chemother. 2009;15:62–9.
Mori Y, Nagamine K, Tomita N, Notomi T. Detection of loop-mediated isothermal amplification reaction by turbidity derived from magnesium pyrophosphate formation. Biochem Biophys Res Commun. 2001;289:150–4.
Mori Y, Kitao M, Tomita N, Notomi T. Real-time turbidimetry of LAMP reaction for quantifying template DNA. J Biochem Biophys Methods. 2004;59:145–57.
Almasi MA, Hosseyni-Dehabadi SM, Aghapour-ojaghkandi M. Comparison and evaluation of three diagnostic methods for detection of beet curly top virus in sugar beet using different visualizing systems. Appl Biochem Biotechnol. 2014;173:1836–48.
Inoshima Y, Takasu M, Ishiguro N. Establishment of an on-site diagnostic procedure for detection of orf virus from oral lesions of Japanese serows (Capricornis crispus) by loop-mediated isothermal amplification. J Vet Med Sci. 2016. doi:10.1292/jvms.16-0268.
Lin X, Chen Y, Lu Y, Yan J, Yan J. Application of a loop-mediated isothermal amplification method for the detection of pathogenic Leptospira. Diagn Microbiol Infect Dis. 2009;63:237–42.
Wastling SL, Picozzi K, Kakembo ASL, Welburn SC. LAMP for human African trypanosomiasis: a comparative study of detection formats. PLoS Negl Trop Dis. 2010;4:e865.
Almasi MA, Erfan Manesh M, Jafary H, Dehabadi SMH. Visual detection of Potato Leafroll virus by loop-mediated isothermal amplification of DNA with the GeneFinderTM dye. J Virol Methods. 2013;192:51–4.
Zhang X, Lowe SB, Gooding JJ. Brief review of monitoring methods for loop-mediated isothermal amplification (LAMP). Biosens Bioelectron. 2014;61:491–9.
Zuerner RL. Nucleotide sequence analysis of IS1533 from Leptospira borgpetersenii: identification and expression of two IS-encoded proteins. Plasmid. 1994;31:1–11.
Zuerner RL, Bolin CA. Differentiation of Leptospira interrogans isolates by IS1500 hybridization and PCR assays. J Clin Microbiol. 1997;35:2612–7.
Zuerner RL, Huang WM. Analysis of a Leptospira interrogans locus containing DNA replication genes and a new IS, IS1502. FEMS Microbiol Lett. 2002;215:175–82.
Pavan ME, Brihuega B, Pettinari MJ, Cairó F. Multiple-locus variable-number tandem repeat analysis of reference strains used for the diagnosis of leptospirosis in Argentina. Rev Argent Microbiol. 2011;43:251–5.
Ahmed A, Thaipadungpanit J, Boonsilp S, et al. Comparison of two multilocus sequence based genotyping schemes for Leptospira species. PLoS Negl Trop Dis. 2011;5:e1374.
Ahmed N, Devi SM, Mde Valverde L, Vijayachari P, Machang’u RS, Ellis WA, et al. Multilocus sequence typing method for identification and genotypic classification of pathogenic Leptospira species. Ann Clin Microbiol Antimicrob. 2006;5:28.
Boonsilp S, Thaipadungpanit J, Amornchai P, et al. A single multilocus sequence typing (MLST) scheme for seven pathogenic Leptospira species. PLoS Negl Trop Dis. 2013;7:e1954.
Varni V, Ruybal P, Lauthier JJ, Tomasini N, Brihuega B, Koval A, et al. Reassessment of MLST schemes for Leptospira spp. typing worldwide. Infect Genet Evol. 2014;22:216–22.
Valverde Mde L, Ramírez JM, de Oca LG M, Goris MGA, Ahmed N, Hartskeerl RA. Arenal, a new Leptospira serovar of serogroup Javanica, isolated from a patient in Costa Rica. Infect Genet Evol J Mol Epidemiol Evol Genet Infect Dis. 2008;8:529–33.
Thaipadungpanit J, Wuthiekanun V, Chierakul W, et al. A dominant clone of Leptospira interrogans associated with an outbreak of human leptospirosis in Thailand. PLoS Negl Trop Dis. 2007. doi:10.1371/journal.pntd.0000056.
Agampodi SB, Moreno AC, Vinetz JM, Matthias MA. Utility and limitations of direct multi-locus sequence typing on qPCR-positive blood to determine infecting Leptospira strain. Am J Trop Med Hyg. 2013;88:184–5.
Perez J, Goarant C. Rapid Leptospira identification by direct sequencing of the diagnostic PCR products in New Caledonia. BMC Microbiol. 2010;10:325.
Acknowledgements
We would like to thank Rodion Gorchakov in the Laboratory for Zoonotic and Vectorborne Diseases at Baylor College of Medicine for lending his expertise, when needed, on sequencing methods of Leptospira employed in his laboratory and for his encouragement of our ongoing work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Byron Flores Somarriba, Jessica Sheleby-Elías, Rebecca S.B. Fischer, William Jirón, and Christiane Duttmann declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Leptospirosis in Mesoamerica
Rights and permissions
About this article
Cite this article
Flores Somarriba, B., Sheleby-Elías, J., Fischer, R.S.B. et al. Leptospirosis in Central America: Techniques for Diagnosis and Molecular Characterization. Curr Trop Med Rep 4, 70–76 (2017). https://doi.org/10.1007/s40475-017-0106-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40475-017-0106-6